Reliability of Compartmental Body Composition Measures in Weight-Stable Adults Using GE iDXA: Implications for Research and Practice
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sample Size
2.3. Procedures
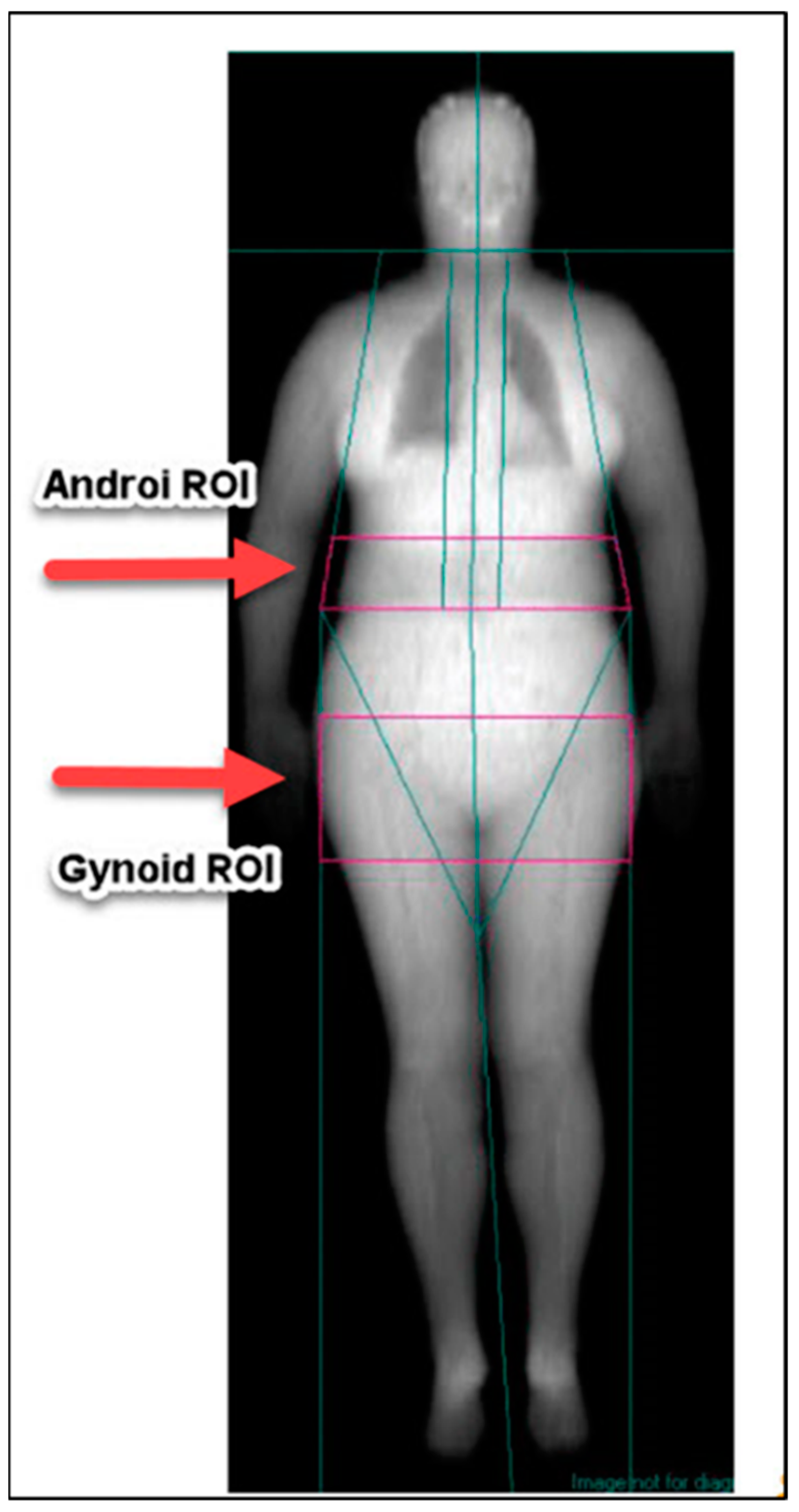
2.4. Scan Analysis Procedures
2.5. Statistical Analysis
3. Results
3.1. Three-Month Reliability Study
3.1.1. Participants’ Baseline Characteristics
3.1.2. Body Composition Variability Over Three Months
3.2. Same-Day Repeated-Scan Precision
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Newton, R.L.; Alfonso, A.; White, M.A.; York-Crowe, E.; Walden, H.; Ryan, D.; Bray, G.A.; Williamson, D. Percent body fat measured by BIA and DEXA in obese, African-American adolescent girls. Int. J. Obes. 2005, 29, 594–602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watts, K.; Naylor, L.H.; Davis, E.A.; Jones, T.W.; Beeson, B.; Bettenay, F.; Siafarikas, A.; Lana, B.; Ackland, T.; Green, D.J. Do skinfolds accurately assess changes in body fat in obese children and adolescents? Med. Sci. Sports Exerc. 2006, 38, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.L.; Wilson, K.E.; Heymsfield, S.B. Dual energy X-Ray absorptiometry body composition reference values from NHANES. PLoS ONE 2009, 4, e7038. [Google Scholar] [CrossRef] [PubMed]
- Steinsbekk, S.; Wichstrom, L.; Odegard, R.; Mehus, I. Change in body fat during a family-based treatment of obesity in children: The relative importance of energy intake and physical activity. Obes. Facts 2013, 5, 515–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manios, Y.; Moschonis, G.; Koutsikas, K.; Papoutsou, S.; Petraki, I.; Bellou, E.; Naoumi, A.; Kostea, S.; Tanagra, S. Changes in body composition following a dietary and lifestyle intervention trial: The postmenopausal health study. Maturitas. 2009, 62, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.; Dempster, D.W.; Recker, R.R.; Lappe, J.M.; Zhou, H.; Zwahlen, A.; Müller, R.; Zhao, B.; Guo, X.; Lang, T. Abdominal fat is associated with lower bone formation and inferior bone quality in healthy premenopausal women: A transiliac bone biopsy study. J. Clin. Endocrinol. Metab. 2013, 98, 2562–2572. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Thornton, J.C.; Mei, Z.; Wang, J.; Dietz, W.H.; Pierson, R.N., Jr.; Horlick, M. Height and adiposity among children. Obes. Res. 2004, 12, 846–853. [Google Scholar] [CrossRef]
- Marinangeli, C.P.; Kassis, A.N. Use of dual X-ray absorptiometry to measure body mass during short- to medium-term trials of nutrition and exercise interventions. Nutr. Rev. 2013, 71, 332–342. [Google Scholar] [CrossRef]
- Millstein, R.A. Measuring outcomes in adult weight loss studies that include diet and physical activity: A systematic review. J. Nutr. Metab. 2014. [Google Scholar] [CrossRef] [PubMed]
- Wensveen, F.M.; Valentic, S.; Sestan, M.; Wensveen, T.T.; Polic, B. The ”Big Bang” in obese fat: Events initiating obesity-induced adipose tissue inflammation. Eur. J. Immunol. 2015, 45, 2446–2456. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Hu, T.; Zhang, S.; Zhou, L. Associations of different adipose tissue depots with insulin resistance: A systematic review and meta-analysis of observational studies. Sci. Rep. 2015, 5, 18495. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Sahakyan, K.R.; Rodriguez-Escudero, J.P.; Bartels, S.J.; Somers, V.K.; Lopez-Jimenez, F. Normal weight obesity and mortality in United States subjects >/=60 years of age (from the Third National Health and Nutrition Examination Survey). Am. J. Cardiol. 2013, 112, 1592–1598. [Google Scholar] [CrossRef] [PubMed]
- Shea, J.L.; King, M.T.; Yi, Y.; Gulliver, W.; Sun, G. Body fat percentage is associated with cardiometabolic dysregulation in BMI-defined normal weight subjects. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 741–747. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Bianchi, A.; Maroni, P.; Iannarelli, A.; Daniele, N.D.; Iacopino, L.; Renzo, L.D. Adiposity rather than BMI determines metabolic risk. Int. J. Cardiol. 2013, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- von Hurst, P.R.; Walsh, D.C.I.; Conlon, C.A.; Ingram, M.; Kruger, R.; Stonehouse, W. Validity and reliability of bioelectrical impedance analysis to estimate body fat percentage against air displacement plethysmography and dual-energy X-ray absorptiometry. Nutr. Diet. 2016, 73, 197–204. [Google Scholar] [CrossRef]
- Kuk, J.L.; Lee, S.; Heymsfield, S.B.; Ross, R. Waist circumference and abdominal adipose tissue distribution: Influence of age and sex. Am. J. Clin. Nutr. 2005, 81, 1330–1334. [Google Scholar] [CrossRef] [PubMed]
- Camhi, S.M.; Bray, G.A.; Bouchard, C.; Greenway, F.L.; Johnson, W.D.; Newton, R.L.; Ravussin, E.; Ryan, D.H.; Smith, S.R.; Katzmarzyk, P.T. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: Sex and race differences. Obesity (Silver Spring) 2011, 19, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Kaul, S.; Rothney, M.P.; Peters, D.M.; Wacker, W.K.; Davis, C.E.; Shapiro, M.D.; Ergun, D.L. Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity (Silver Spring) 2012, 20, 1313–1318. [Google Scholar] [CrossRef] [PubMed]
- Leonard, C.M.; Roza, M.A.; Barr, R.D.; Webber, C.E. Reproducibility of DXA measurements of bone mineral density and body composition in children. Pediatr. Radiol. 2009, 39, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Alwis, G.; Rosengren, B.; Stenevi-Lundgren, S.; Duppe, H.; Sernbo, I.; Karlsson, M.K. Normative dual energy X-ray absorptiometry data in Swedish children and adolescents. Acta. Paediatr. 2013, 99, 1091–1099. [Google Scholar] [CrossRef] [PubMed]
- Mellis, M.G.; Oldroyd, B.; Hind, K. In vivo precision of the GE Lunar iDXA for the measurement of visceral adipose tissue in adults: The influence of body mass index. Eur. J. Clin. Nutr. 2014, 68, 1365–1367. [Google Scholar] [CrossRef] [PubMed]
- Carver, T.E.; Christou, N.V.; Court, O.; Lemke, H.; Andersen, R.E. In vivo precision of the GE lunar iDXA for the assessment of lumbar spine, total hip, femoral neck, and total body bone mineral density in severely obese patients. J. Clin. Densitom. 2014, 17, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Lohman, M.; Tallroth, K.; Kettunen, J.A.; Marttinen, M.T. Reproducibility of dual-energy X-ray absorptiometry total and regional body composition measurements using different scanning positions and definitions of regions. Metabolism 2009, 58, 1663–1668. [Google Scholar] [CrossRef] [PubMed]
- Kaminsky, L.A.; Ozemek, C.; Williams, K.L.; Byun, W. Precision of total and regional body fat estimates from dual-energy X-ray absorptiometer measurements. J. Nutr. Health Aging 2014, 18, 591–594. [Google Scholar] [CrossRef] [PubMed]
- Baim, S.; Wilson, C.R.; Lewiecki, E.M.; Luckey, M.M.; Downs, R.W., Jr.; Lentle, B.C. Precision assessment and radiation safety for dual-energy X-ray absorptiometry: Position paper of the International Society for Clinical Densitometry. J. Clin. Densitom. 2005, 8, 371–378. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gomez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis—Part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef] [PubMed]
- Hind, K.; Oldroyd, B. In-vivo precision of the GE Lunar iDXA densitometer for the measurement of appendicular and trunk lean and fat mass. Eur. J. Clin. Nutr. 2013, 67, 1331–1333. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Bachrach, L.; Brown, J.P.; Hanley, D.A.; Josse, R.G.; Kendler, D.L.; Leib, E.S.; Lentle, B.C.; Leslie, W.D.; Lewiecki, E.M.; et al. Standards and guidelines for performing central dual-energy X-ray absorptiometry in premenopausal women, men, and children. J. Clin. Densitom. 2004, 7, 51–64. [Google Scholar] [CrossRef]
- International Society for Clinical Densiotometry (ISCD). Bone Densitometry Precision Calculating Tool. Available online: http://www.iscd.org/resources/calculators/precision-calculator/faq/ (accessed on 13 March 2017).
- Wing, R.R.; Lang, W.; Wadden, T.A.; Safford, M.; Knowler, W.C.; Bertoni, A.G.; Hill, G.O.; Brancati, F.L.; Peters, A.; Wagenknecht, L.; et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011, 34, 1481–1486. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, G. Effect of degree of weight loss on health benefits. Obes. Res. 1995, 3 (Suppl. S2), 211s–216s. [Google Scholar] [CrossRef] [PubMed]
- Dulloo, A.G.; Jacquet, J.; Solinas, G.; Montani, J.P.; Schutz, Y. Body composition phenotypes in pathways to obesity and the metabolic syndrome. Int. J. Obes. 2010, 34 (Suppl. 2), S4–S17. [Google Scholar] [CrossRef]
- Smith, J.D.; Borel, A.L.; Nazare, J.A.; Haffner, S.M.; Balkau, B.; Ross, R.; Massien, C.; Alméras, N.; Després, J.-P. Visceral adipose tissue indicates the severity of cardiometabolic risk in patients with and without type 2 diabetes: Results from the INSPIRE ME IAA study. J. Clin. Endocrinol. Metab. 2012, 97, 1517–1525. [Google Scholar] [CrossRef] [PubMed]
- Lewiecki, E.M.; Binkley, N.; Morgan, S.L.; Shuhart, C.R.; Camargos, B.M.; Carey, J.J.; Gordon, C.M.; Jankowski, L.G.; Lee, J.-K.; Leslie, W.D.; et al. Best Practices for Dual-Energy X-ray Absorptiometry Measurement and Reporting: International Society for Clinical Densitometry Guidance. J. Clin. Densitom. 2016, 19, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Carver, T.E.; Christou, N.V.; Andersen, R.E. In vivo precision of the GE iDXA for the assessment of total body composition and fat distribution in severely obese patients. Obesity (Silver Spring) 2013, 21, 1367–1369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hind, K.; Oldroyd, B.; Truscott, J.G. In vivo precision of the GE Lunar iDXA densitometer for the measurement of total body composition and fat distribution in adults. Eur. J. Clin. Nutr. 2011, 65, 140–142. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Franks, P.W.; Brookshire, T.; Tataranni, P.A. The intra- and inter-instrument reliability of DXA based on ex vivo soft tissue measurements. Obes. Res. 2004, 12, 1925–1929. [Google Scholar] [CrossRef] [PubMed]
- Borruel, S.; Molto, J.F.; Alpanes, M.; Fernandez-Duran, E.; Alvarez-Blasco, F.; Luque-Ramirez, M.; Escobar-Morreale, H.F. Surrogate markers of visceral adiposity in young adults: Waist circumference and body mass index are more accurate than waist hip ratio, model of adipose distribution and visceral adiposity index. PLoS ONE 2014, 9, e114112. [Google Scholar] [CrossRef] [PubMed]
- Larsson, I.; Lissner, L.; Samuelson, G.; Fors, H.; Lantz, H.; Naslund, I.; Carlsson, L.M.S.; Sjöström, L.; Bosaeus, I. Body composition through adult life: Swedish reference data on body composition. Eur. J. Clin. Nutr. 2015, 69, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Yeung, E.H.; Zhang, C.; Albert, P.S.; Mumford, S.L.; Ye, A.; Perkins, N.J.; Wactawski-Wende, J.; Schisterman, E.F. Adiposity and sex hormones across the menstrual cycle: The BioCycle Study. Int. J. Obes. (Lond.) 2013, 37, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Gleichauf, C.N.; Roe, D.A. The menstrual cycle’s effect on the reliability of bioimpedance measurements for assessing body composition. Am. J. Clin. Nutr. 1989, 50, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Kirchengast, S.; Gartner, M. Changes in fat distribution (WHR) and body weight across the menstrual cycle. Coll. Antropol. 2002, 26, 47–57. [Google Scholar] [PubMed]
- Haddad, L.; Milke, P.; Zapata, L.; de la Fuente, J.R.; Vargas-Vorackova, F.; Lorenzana-Jimenez, M.; Corte, G.; Tamayo, J.; Kaplan, M.; Márquez, M.; et al. Effect of the menstrual cycle in ethanol pharmacokinetics. J. Appl. Toxicol. 1998, 18, 15–18. [Google Scholar] [CrossRef]
- Cheung, A.S.; de Rooy, C.; Hoermann, R.; Gianatti, E.J.; Hamilton, E.J.; Roff, G.; Zajac, J.D.; Grossmann, M. Correlation of visceral adipose tissue measured by Lunar Prodigy dual X-ray absorptiometry with MRI and CT in older men. Int. J. Obes. (Lond.) 2016, 40, 1325–1328. [Google Scholar] [CrossRef] [PubMed]
- Mourier, A.; Gautier, J.F.; De Kerviler, E.; Bigard, A.X.; Villette, J.M.; Garnier, J.P.; Duvallet, A.; Guezennec, C.Y.; Cathelineau, G. Mobilization of visceral adipose tissue related to the improvement in insulin sensitivity in response to physical training in NIDDM. Effects of branched-chain amino acid supplements. Diabetes Care 1997, 20, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Toro-Ramos, T.; Goodpaster, B.H.; Janumala, I.; Lin, S.; Strain, G.W.; Thornton, J.C.; Kang, P.; Courcoulas, A.P.; Pomp, A.; Gallagher, D. Continued loss in visceral and intermuscular adipose tissue in weight-stable women following bariatric surgery. Obesity (Silver Spring) 2015, 23, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Chaston, T.B.; Dixon, J.B. Factors associated with percent change in visceral versus subcutaneous abdominal fat during weight loss: Findings from a systematic review. Int. J. Obes. (Lond.) 2008, 32, 619–628. [Google Scholar] [CrossRef] [PubMed]
| Number of Participants (Male n, (%)) | 51 (6 (12)) | |||||||||
| Total | Visit 1 | Visit 2 | Visit 3 | |||||||
| Height (cm) | 165.0 (149.1–178.5) | 165.3 (148.8–178.7) | 164.9 (148.3–178.3) | |||||||
| Weight (kg) | 59.8 (49.5–83.7) | 60.2 (49.2–83.6) | 59.7 (47.6–84.0) | |||||||
| BMI (kg/m2) | 22.2 (18.6–31.5) | 22.3 (18.3–31.7) | 22.4 (18.2–31.7) | |||||||
| Male | ||||||||||
| Height (cm) | 172.0 (167.5–178.5) | 171.6 (168.1–178.7) | 171.9 (167.8–178.4) | |||||||
| Weight (kg) | 77.6 (69.9–82.5) | 75.5 (69.0–81.6) | 77.5 (69.4–81.9) | |||||||
| BMI (kg/m2) | 25.5 (23.8–28.2) | 25.1 (23.3–27.9) | 25.5 (23.4–27.9) | |||||||
| Female | ||||||||||
| Height (cm) | 164.5 (149.1–176.4) | 164.3 (148.8–176.4) | 164.2 (148.3–176.4) | |||||||
| Weight (kg) | 58.7 (49.5–83.7) | 57.9 (49.2–83.6) | 58.4 (47.6–84.0) | |||||||
| BMI (kg/m2) | 21.8 (18.6–31.5) | 21.9 (18.3–31.7) | 22.0 (18.2–31.7) | |||||||
| Measure (Region of Interest) | Visit 1 | Visit 2 | Visit 3 | CV% | RMSSD (LSC 95% CI) | |||||
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | V1–V2 | V2–V3 | V1–V3 | ||
| A-FM (kg) | 1.33 (0.97) | 0.27–4.81 | 1.33 (0.98) | 0.30–5.01 | 1.32 (0.96) | 0.25–4.89 | 5.9 | 0.10 (0.27) | 0.11 (0.31) | 0.12 (0.34) |
| G-FM (kg) | 3.53 (1.37) | 1.28–7.76 | 3.54 (1.35) | 1.20–7.62 | 3.55 (1.40) | 1.25–8.07 | 2.8 | 0.15 (0.43) | 0.15 (0.40) | 0.19 (0.53) |
| TB-FM (kg) | 18.8 (7.82) | 7.62–47.3 | 18.9 (7.93) | 8.10–47.7 | 18.8 (7.94) | 7.81–47.7 | 2.5 | 0.73 (2.03) | 0.60 (1.67) | 1.00 (2.76) |
| A-LM (kg) | 3.01 (0.54) | 2.18–4.69 | 2.98 (0.56) | 2.16–4.61 | 2.99 (0.58) | 1.91–4.80 | 3.1 | 0.14 (0.39) | 0.16 (0.46) | 0.14 (0.39) |
| G-LM (kg) | 6.60 (1.29) | 4.67–10.2 | 6.58 (1.30) | 4.50–10.2 | 6.60 (1.31) | 4.45–10.1 | 1.6 | 0.15 (0.42) | 0.17 (0.46) | 0.16 (0.43) |
| TB-LM (kg) | 41.0 (7.55) | 30.6–61.3 | 41.1 (7.61) | 30.4–61.4 | 41.1 (7.68) | 29.1–62.0 | 1.2 | 0.77 (2.14) | 0.80 (2.21) | 0.86 (2.37) |
| A-TM (kg) | 4.38 (1.23) | 2.71–8.51 | 4.36 (1.22) | 2.68–8.42 | 4.36 (1.27) | 2.52–8.45 | 2.3 | 0.15 (0.43) | 0.14 (0.40) | 0.16 (0.43) |
| G-TM (kg) | 10.4 (1.92) | 6.81–15.8 | 10.4 (1.87) | 6.86–15.4 | 10.4 (1.95) | 6.65–15.7 | 1.3 | 0.22 (0.62) | 0.22 (0.60) | 0.20 (0.55) |
| TB-TM (kg) | 62.2 (11.9) | 43.1–98.2 | 62.3 (11.9) | 43.9–98.9 | 62.3 (12.1) | 42.7–98.7 | 0.8 | 0.79 (2.20) | 0.67 (1.85) | 0.92 (2.56) |
| A-%Fat | 28 (12) | 9–58 | 28 (12) | 9–60 | 28 (11) | 10–58 | 5.5 | 2.0 (5.5) | 2.3 (6.3) | 2.7 (7.5) |
| G-%Fat | 34 (9) | 16–52 | 34 (9) | 15–51 | 34 (9) | 15–53 | 2.2 | 1.2 (3.3) | 1.1 (3.1) | 1.4 (3.8) |
| TB-%Fat | 30 (8) | 17–50 | 30 (8) | 16–51 | 30 (8) | 16–50 | 2.5 | 1.1 (3.1) | 1.1 (3.1) | 1.6 (4.4) |
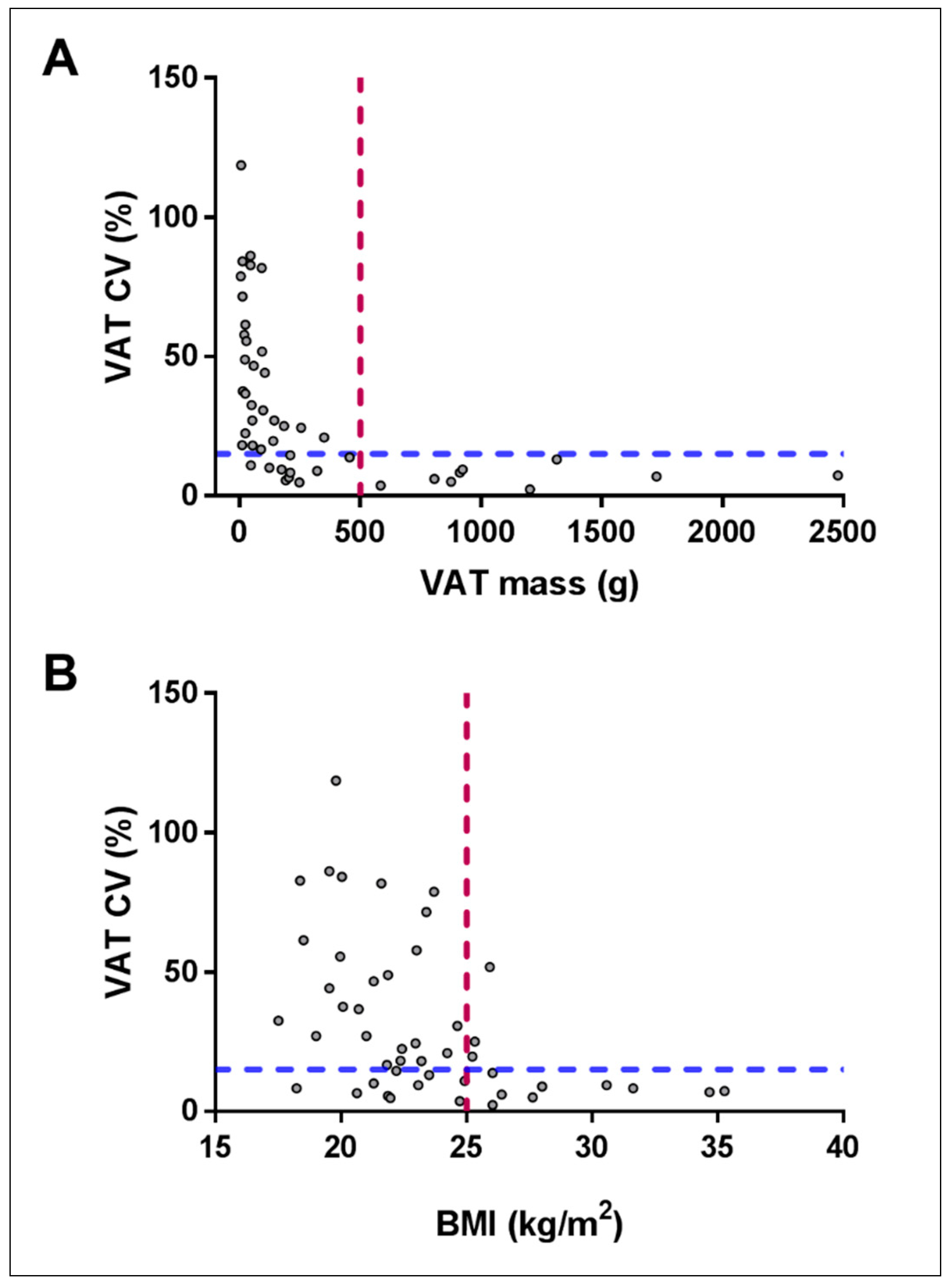
| VAT Mass (g) | 303.7 (504.9) | 0–2540.0 | 301.4 (516.6) | 0–2621.7 | 280.9 (464.1) | 0–2273.1 | 42.2 | 50.8 (140.7) | 82.7 (229.0) | 74.5 (206.3) |
| VAT Vol (cm3) | 322.0 (535.2) | 0–2692.4 | 319.5 (547.6) | 0–2779.0 | 297.7 (491.9) | 0–2409.5 | 42.2 | 66.4 (184.0) | 70.2 (194.5) | 65.4 (181.2) |
| VAT Mass (g) ^ | 350.8 (529.1) | 0.49–2540.0 | 348.3 (542.1) | 0.46–2621.7 | 324.9 (485.8) | 2.18–2273.1 | 29.3 | 54.6 (151.3) | 88.7 (245.8) | 79.6 (220.5) |
| VAT Vol (cm3) ^ | 371.8 (560.8) | 0.51–2692.4 | 369.2 (574.6) | 0.48–2779.0 | 344.4 (514.9) | 2.32–2409.5 | 29.3 | 57.9 (160.4) | 94.0 (260.5) | 84.4 (233.7) |
| Characteristics | ||||||
| Number of participants (Male n, (%)) | 30 (14 (47)) | Men | Women | |||
| Height (cm) Median (5th–95th percentile) | 171.4 (161.9–184.6) | 176.6 (169.7–192.3) | 165.3 (161.9–184.2) | |||
| Weight (kg) Median (5th–95th percentile) | 77.8 (51.7–131.9) | 102.8 (55.8–145.1) | 69.9 (51.7–126.9) | |||
| BMI (kg/m2) Median (5th–95th percentile) | 26.5 (18.9–39.2) | 34.2 (18.9–42.53) | 24.4 (19.0–37.4) | |||
| Measure | Scan 1 Mean (SD) | Range | Scan 2 Mean (SD) | Range | CV% | RMSSD (LSC 95% CI) |
| A-FM (kg) | 2.32 (1.77) | 0.36–6.56 | 2.34 (1.81) | 0.36–6.60 | 1.87 | 0.06 (0.18) |
| G-FM (kg) | 4.75 (2.64) | 1.77–11.96 | 4.79 (2.74) | 1.77–12.43 | 1.28 | 0.15 (0.43) |
| TB-FM (kg) | 26.80 (15.01) | 10.51–60.09 | 26.86 (15.14) | 10.78–60.10 | 0.74 | 0.31 (0.85) |
| A-LM (kg) | 3.82 (0.87) | 2.32–5.93 | 3.82 (0.87) | 2.29–6.01 | 1.11 | 0.08 (0.23) |
| G-LM (kg) | 8.74 (2.21) | 5.12–13.46 | 8.75 (2.23) | 5.01–13.59 | 0.60 | 0.15 (0.43) |
| TB-LM (kg) | 53.67 (12.54) | 32.79–79.23 | 53.69 (12.46) | 32.77–79.93 | 0.48 | 0.48 (1.34) |
| A-TM (kg) | 6.19 (2.44) | 3.33–11.02 | 6.21 (2.48) | 3.25–11.22 | 0.63 | 0.08 (0.21) |
| G-TM (kg) | 13.81 (4.36) | 8.60–23.64 | 13.86 (4.46) | 8.57–24.33 | 0.58 | 0.18 (0.50) |
| TB-TM (kg) | 83.41 (25.29) | 51.58–136.13 | 83.50 (25.42) | 51.60–136.22 | 0.20 | 0.40 (1.10) |
| A-%Fat | 33 (15) | 8–61 | 33 (15) | 8–61 | 1.75 | 0.9 (2.5) |
| G-%Fat | 33 (9) | 16–52 | 33 (10) | 16–53 | 1.02 | 0.6 (1.7) |
| TB-%Fat | 30 (9) | 17–48 | 30 (9) | 17–48 | 0.80 | 0.4 (1.1) |
| VAT Mass (g) | 776.9 (808.8) | 28.0–2978.2 | 766.7 (807.5) | 0.0–2999.2 | 16.2 | 65.5 (181.4) |
| VAT Vol (cm3) | 823.5 (857.4) | 29.7–3156.9 | 812.7 (856.0) | 0.0–3179.1 | 16.2 | 82.2 (227.8) |
| VAT Mass (g) ^ | 802.4 (810.8) | 28.0–2978.2 | 793.2 (808.5) | 23.4–2999.2 | 11.8 | 66.4 (184.0) |
| VAT Vol (cm3) ^ | 850.5 (859.4) | 29.7–3156.9 | 840.7 (857.0) | 24.8–3179.1 | 11.8 | 82.5 (228.6) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dordevic, A.L.; Bonham, M.; Ghasem-Zadeh, A.; Evans, A.; Barber, E.; Day, K.; Kwok, A.; Truby, H. Reliability of Compartmental Body Composition Measures in Weight-Stable Adults Using GE iDXA: Implications for Research and Practice. Nutrients 2018, 10, 1484. https://doi.org/10.3390/nu10101484
Dordevic AL, Bonham M, Ghasem-Zadeh A, Evans A, Barber E, Day K, Kwok A, Truby H. Reliability of Compartmental Body Composition Measures in Weight-Stable Adults Using GE iDXA: Implications for Research and Practice. Nutrients. 2018; 10(10):1484. https://doi.org/10.3390/nu10101484
Chicago/Turabian StyleDordevic, Aimee L., Maxine Bonham, Ali Ghasem-Zadeh, Alison Evans, Elizabeth Barber, Kaitlin Day, Alastair Kwok, and Helen Truby. 2018. "Reliability of Compartmental Body Composition Measures in Weight-Stable Adults Using GE iDXA: Implications for Research and Practice" Nutrients 10, no. 10: 1484. https://doi.org/10.3390/nu10101484
APA StyleDordevic, A. L., Bonham, M., Ghasem-Zadeh, A., Evans, A., Barber, E., Day, K., Kwok, A., & Truby, H. (2018). Reliability of Compartmental Body Composition Measures in Weight-Stable Adults Using GE iDXA: Implications for Research and Practice. Nutrients, 10(10), 1484. https://doi.org/10.3390/nu10101484






