Abstract
Physical activity and exercise participation among older adults have decreased dramatically because of the physical distancing measures implemented to prevent the spread of COVID-19. However, even in the face of unforeseen environmental changes, physical activity and exercise for older adults must be sustainable. This study aimed to identify the influencing physical activity and exercise participation among older adults in 2020 when varying levels of quarantine were in place as a protective measure against the COVID-19 pandemic to build a foundation for sustainable older adult health strategies. We utilized a large-scale dataset from the 2020 National Survey of Older Koreans conducted in 2020. Twenty survey questions were used as predictors, and logistic regression and decision tree analyses were utilized to identify influencing factors. Through a logistic regression analysis, 16 factors influencing exercise participation were identified. Additionally, through a decision tree analysis, 7 factors that influence exercise participation and 8 rules were derived through a combination of these factors. According to the results of this study, the use of ICT technologies, such as ‘smartphone or tablet PC’, can be a useful tool to maintain or promote physical activity and exercise by older adults in a situation like the COVID-19 pandemic. In conclusion, physical activity and exercise intervention strategies should be developed with comprehensive consideration of the influencing factors to ensure that physical activity and exercise among older adults can be sustained uninterrupted in the face of unforeseen circumstances, such as the COVID-19 pandemic.
1. Introduction
Coronavirus disease (COVID-19), which began to spread in December 2019, reached Korea on 20 January 2020 and had spread across the country by 23 February 2020. On 11 March 2020, the World Health Organization (WHO) officially declared COVID-19 to be a global pandemic [1]. Shortly thereafter, several countries, including Korea, enacted mitigation strategies such as physical distancing, stay-at-home orders, and the closing of nonessential businesses to reduce the spread of virus [2]. Consequently, in almost all countries, nonessential government and private services were closed, and efforts to keep people at home intensified [3]. The implementation of these strategies reduced the transmission of COVID-19 but also changed daily life significantly, affecting normal activities such as PAEXP [4]. South Korea announced its first physical distancing policy to limit the operation of religious and sporting events, sports facilities, and entertainment facilities on 22 March 2020. It shifted to a more relaxed policy on 6 May 2020, before strengthening to a level 2.5 quarantine on 30 August. On 14 September 2020, the restrictions eased to a level 2 quarantine, and for six weeks, from 12 October to 22 November, restrictions eased to a level 1 quarantine, the lowest level [5]. In Korea, the level of social activity restrictions varied depending on the stage of physical distancing measures, but there were no national lockdown measures, and outdoor activities were requested to be restrained [6]. The policy was based on a distance of 2 m between people. Additionally, infected people were forced to stay at home for 14 days by stay-at-home orders. This policy lasted until 15 April 2022.
While physical distancing measures to prevent the spread of COVID-19 have mitigated the spread of the virus [4], activity restrictions due to long-term home stays have resulted in a sharp decline in ‘physical activity and exercise participation’ (PAEXP) [7]. The decline in PAEXP has been particularly remarkable among older adults. In South Korea, the PXEXP rate of adults aged 65 years and older decreased significantly from 68% in 2017 (n = 10,299) to 53.7% in 2020 (n = 10,097) [8,9]. Japan also reported that the level of physical activity in older adults aged 65–84 years (n = 1600) decreased by approximately 65 min per week compared to that before the COVID-19 pandemic [10]. In France, during the COVID-19 confinement period, 39.2% of individuals aged 65 years and older (n = 1178) reported a decrease in their level of physical activity [11]. In a multinational (14 countries) study investigating the effects of pandemic-related confinement on physical activity levels, adults aged 70 years and older showed greater decreases in physical activity compared to other age groups [12]. Considering that PAEXP and a lack of opportunities to engage in PAEXP are important factors in the development of chronic diseases and all-cause deaths in older adults [13], restricting activities due to confinement measures will negatively affect the health of older individuals moving forward [14].
The benefits of PAEXP in the older adult population are indisputable. PAEXP in older adults helps them to not only properly respond to negative changes related to aging by maintaining and improving physical abilities [15] but also to slow the deterioration of mental health, which is a concern in the older adult population [16]. It also has a positive effect in that it provides opportunities for social contact or the maintenance of continuous social contact [17] and is highly effective in preventing the onset, or reducing the severity of, many chronic diseases that are prevalent among older adults [18]. In other words, PAEXP is essential for maintaining the physiological, psychological, and social health of older adults and improving their quality of life [19]. Despite restrictions due to COVID-19 measures, there is a need for effective intervention strategies to promote and maintain an active state among older adults.
A basic and important task is to identify the factors influencing the preparation of effective intervention strategies to promote PAEXP in older adults. Accordingly, numerous studies have explored the factors affecting PAEXP in older adults. Previous research has reported various factors impacting PAEXP in older adults, including sociodemographic characteristics, health-related factors, functional status, economic status, social factors, and physical environments. The following factors were reported to affect PAEXP in older adults: age [13], gender [20], residence [21] marital status [22], and educational level [23] for sociodemographic characteristics; chronic diseases [24], smoking [25], nutritional status [26], body mass index [27], depression [28], and health status [29] for health-related factors; functional limitations [30] and physical function [31] for functional status; working status [25] and household income [32] for economic status; family support [33], support from friends and neighbors [34], social participation [29], and social network contacts [17] for social factors; and proximity to parks and trails [35] and accessibility of pedestrian infrastructure and facilities [36] for physical environments.
The spread of COVID-19 and subsequent confinement measures have dramatically altered the environment for PAEXP. Factors influencing PAEXP may have changed during the COVID-19 pandemic, and these changes can aggravate the prevalent lack of physical activity and motivation to exercise among older adults. Information on the factors influencing PAEXP in older adults should be updated based on the COVID-19 pandemic. However, studies on the factors influencing PAEXP in older adults during the COVID-19 pandemic have not been actively conducted. Although a study analyzing the correlation between physical activity and household variables in children aged under 13 years [37] and another analyzing the effects of components of the COM (capability, opportunity, and motivation)-B (changing behavior) model on physical activity in adults aged 18 years and older [14] have been conducted, there have been no studies involving older adults, who are known to be the most vulnerable to quarantine measures due to COVID-19. To devise a public health strategy that allows older adults to participate in PAEXP continuously without interruption, it is necessary to systematize their knowledge of the determinants of PAEXP during the COVID-19 period.
Therefore, this study aimed to identify factors related to PAEXP participation in older adults during a COVID-19 lockdown. In addition, given that COVID-19 is ongoing and that unpredictable circumstances, such as other pandemics, may occur frequently in the future, discussions on PAEXP in older adults in the COVID-19 environment are essential to devise a sustainable older adult health strategy. Therefore, this study set 2020, the COVID-19 pandemic period, as the time range and utilized large quantities of data from the 2020 National Survey of Older Koreans. Moreover, 18 variables related to PAEXP in older adults, which are well known through previous studies, and two new variables (the number of rooms and smartphone or tablet PC using), which are expected to affect PAEXP considering the COVID-19 pandemic environment were set as predictors, and logistic regression and decision tree analyses were performed.
2. Related Works
The COVID-19 lockdown led to a decrease in PAEXP, not only among older adults in Korea, but among all age groups. The rate of decrease in PAEXP in adults in their 30s was the highest at 11.7%, followed by 8.9% for those in their 40s, 8.2% for those in their 20s, and 6.9% for those in their 60s. On the other hand, in teenagers, PAEXP increased by 2% [38]. PAEXP showed the largest decrease in those aged in their 20s, 30s, and 40s, which are the age groups who are most active in social activities. These results are in line with Meyer et al. [39]’s findings that PAEXP in young adults (ages 18–34) in the United States decreased and sitting time increased significantly compared to that of older adults (Figure 1).
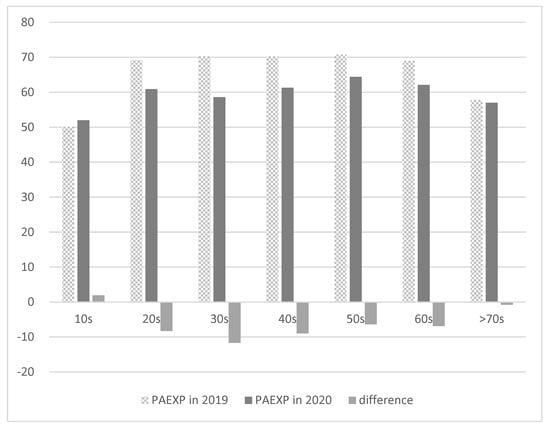
Figure 1.
Decrease in PAEXP by age group in Korea due to the COVID-19 lockdown.
Wilke et al. [12] surveyed 13,503 people in 14 countries about the decline in PAEXP. Their finding was that the amount of habitual movement declined by 41% and 42% for moderate-to-vigorous PAEXP and vigorous PAEXP, respectively [12]. Maugeri et al. [40], who surveyed 2524 Italians about their reduction in PAEXP before and after COVID-19 confinement, showed a significant reduction in total energy expenditure through weekly PAEXP by older adults in Italy. Qin et al. [41] reported a decrease in PAEXP in nearly 60% of the subjects in a study of 12,107 Chinese people aged 18 to 80. Although there have been cases of increased PAEXP despite COVID-19 lockdowns in certain groups, many studies have shown a decrease in PAEXP in all age groups in general.
Did the PAEXP of older adults decrease during the COVID-19 lockdown? In addition, it is important to review the results of previous studies on factors that promote PAEXP in older adults. Previous studies on this show conflicting results. Several previous studies [42] have reported that the PAEXP of older adults decreased during the first three months of the COVID-19 lockdown. Lefferts et al. [42] studied the effect of the COVID-19 pandemic on PAEXP and sedentary behavior in 387 older adults. The study reported that aerobic exercise, muscle-strengthening physical activities, and walking decreased in the older adults, and time spent sitting at home increased during the first three months of the pandemic, although sitting time at home and both physical activity and sedentary behaviors returned to prepandemic levels after a year. According to a survey by Yang and Koenigstorfer [43], US residents’ PAEXP levels decreased by 18.2% during the COVID-19 lockdown, and PAEXP decreased less when apps were used frequently. Pombo et al. (2020) [3] reported that children’s PAEXP decreased during the COVID-19 lockdown. Additionally, it was reported that having at least one adult who was free from working, other children in the household, and a big outdoor space were significant positive factors for the PAEXP level.
In contrast, Spence et al. [14] surveyed 1521 UK adults on the effects of demographic information and psychological factors on PAEXP, and 57% of the subjects answered that they maintained or increased their PAEXP level during the COVID-19 lockdown. The study concluded that UK adults would be willing to engage in PAEXP during lockdown if they had physical opportunities and motivation.
3. Methods
3.1. Data
This study was a secondary data analysis of the 2020 National Survey of Older Koreans (NSOK) conducted by the Ministry of Health and Welfare and the Korea Institute for Health and Social Affairs of South Korea. The 2020 NSOK is a large-scale survey that has been conducted every three years since 2008 to provide the basic data necessary for the establishment of policies for older adults in South Korea [9]. As of 2020, the target population of the 2020 NSOK has included people aged 65 years and older living in standard residential facilities or premises in 17 metropolitan cities and provinces across South Korea. Sampling framing was based on the 2018 population and housing census; samples were extracted according to stratified cluster random sampling and distributed according to the square root proportion according to the number of older adults in each region [9]. The survey was conducted as face-to-face interviews using the TAPI (tablet PC assisted personal interview) method during the 14 September–20 November 2020 period, and a total of 10,097 older adults aged 65 or older participated. According to NSOK 2020, the same face-to-face survey was conducted despite the COVID-19 pandemic due to the vastness of the survey volume, considering the health and literacy of older adults, and the connection with the previous survey. In consideration of COVID-19 quarantine rules, surveyors and subjects observed safety conditions. All 169 surveyors were required to wear sanitary caps on masks before the survey (double quarantine), spray disinfectant during home visits, and carry out tablet PC disinfection before the survey [9]. The 2020 NSOK included 186 questions covering ten survey items to gain a better understanding of the various characteristics of older adults. The survey items were as follows: general characteristics, financial status, family and social relations, exchange of help between family members, health condition and health behavior, functional status and nursing care, cognitive function, economic activities, leisure and social activities, living environment, and life in old age [9].
3.2. Subjects
The participants of this study were 9920 out of the total of 10,097 participants in the NSOK 2020, excluding 177 participants who responded by proxy. The reason for the proxy responses was when an older adult’s family responded on behalf of the older adult due to mental instability, senility, or illness of the older adult. Proxy responses were excluded from this study, because the accuracy of these responses was not certain. The age ranges of the subjects were 65–69 years old (35.4%), 70–74 years old (24.9%), 75–79 years old (19.7%), 80–84 years old (13.9%), and 85 years of age or older (6.1%). Older female adults accounted for 60% of the total, and older adults living in urban areas made up 71.5% of the total. Approximately 59% of the surveyed older adults were married. Regarding the educational level, elementary school graduation was the highest at 33.4%, followed by high school at 26.8%, middle school at 23.5%, uneducated at 11.3%, and beyond college at 5.1%.
3.3. Measurement
Physical activity and exercise are terms that describe different concepts; however, their meanings are often confused and used interchangeably [44]. In South Korea, these terms are used academically as different concepts and have similar meanings without a clear distinction. However, in everyday language, the term “exercise” is used interchangeably with physical activity [45]. The questionnaire used in this study also asked whether the participants exercised daily as one of the health type categories. However, it is difficult to clearly define the concept to be measured because it does not provide criteria that can clearly distinguish between physical activity and exercise. It is also difficult to find strong evidence of differences in the factors influencing PAEXP. Therefore, in the present study, PAEXP was operationally defined using similar concepts and the discussion proceeded.
The target variable was PAEXP, and this was based on the following survey question: “Do you PAEXP regularly?” PAEXP refers to all movement, including sports, exercise and brisk walking, wheeling, cycling, active recreation, and play and can be done at any level of skill. There were two possible responses: yes and no. The recommended level of PAEXP by the Ministry of Health and Welfare in Korea is a total of more than 150 min per week.
The predictor variables included sociodemographic, economic, and health-related factors, functional status, social factors, physical environments, and other variables expected to influence PAEXP during the COVID-19 lockdown. Under COVID-19 quarantine conditions, the presence of large spaces in the home has been related to PAEXP [3,46]. Therefore, we used the number of rooms as a measure of household variables. In addition, the demand for home training via wireless devices or internet technology increased during the COVID-19 pandemic when contactless living became the norm [47]. Thus, we measured smartphone or tablet PC using as a technology variable, assuming that older adults’ use of wireless devices or Internet technology affected their PAEXP.
The sociodemographic factors included age, gender, marital status, educational level, and residential area. Age was categorized into groups of 65–69, 70–74, 75–79, 80–84, and 85 years or more. Marital status was dichotomized into married and nonmarried (never married, widowed, divorced, or separated), and educational level was categorized into uneducated, elementary school, middle school, high school, and beyond college. The participants were male and female, and the residential areas were urban and rural.
The economic factors included paid work and household income. Paid work was based on the following question in the survey: “Do you currently have a job that pays you?” The response options were yes or no. Household income was categorized into three categories: ≤9.03 million won (~6800 US dollars), ≤27.08 million won (~20,400 US dollars), and >27.08 million won. The cutoff point for the category was the income corresponding to 50% and 150% of the median income, and the income class was divided based on this [48].
Health-related factors included the number of chronic diseases, smoking status, nutritional status, body mass index, depression, and health status. The number of chronic diseases was based on a question asking respondents to identify any disease that had lasted three months or more and had been diagnosed by a doctor from a list of 32 diseases. The total number of chronic diseases was categorized into three or more, one to two, and zero. Smoking was based on a question asking whether the individual currently smoked, and the response options were yes or no. Nutritional status was measured using the “Determine Your Nutritional Health Checklist” developed by the Nutrition Screening Initiative [49]. This checklist contains ten items (response options: yes or no) that inquire about the state of nutritional management in the past month. Scores were summed by weighting according to the response value, and based on this, they were categorized into good (0–2 points), moderate risk (3–5 points), and high risk (more than 6 points). Body mass index (BMI; kg/m2) was calculated using self-reported height and weight values, and participants were then categorized as underweight (BMI < 18.5 kg/m2), normal weight (BMI between 18.5 and 24.9 kg/m2), overweight (BMI between 25.0 and 29.9 kg/m2), or obese (BMI ≥ 30 kg/m2) [50]. Depression was measured using the Korean version of the short form of the geriatric depression scale [51,52]. This scale has 15 questions (response options: yes or no), and scores range from 0 to 15 according to the response values. A score of 8 or higher was classified as depression and categorized as yes or no. Health status was based on the following survey question: “How do you feel about your health in general?” The responses were categorized into three groups: unhealthy, neither healthy nor unhealthy, and healthy.
Functional status included functional limitations and physical function. Functional limitations were measured using the Korean versions of the activities of daily living (ADL) and instrumental activities of daily living (IADL) scales [53]. The Korean version of the ADL assesses whether the participant has needed help with each of the following seven activities in the past week: dressing, washing face, brushing teeth and washing hair, taking a bath, eating food, getting up and walking across the room, using the toilet, and holding bowel movements and bladder. The Korean version of the IADL assesses whether the participant has needed help with each of the following ten activities in the past week: personal grooming, performing household chores, preparing meals, doing laundry, purchasing goods, making and receiving calls, taking medications on time, managing money, going out for a short walk, and using transportation. Through the evaluation of ADL and IADL, if help was needed for any one activity, the participant was categorized as having a functional limitation (yes); if no help was needed, the participant was classified as having no functional limitation (no). Physical function was measured using the mobility scale as part of the physical functioning scale [54], which assesses the degree of difficulty in accomplishing each of the following five upper and lower body tasks: walking 400 m; walking up 10 steps without resting; stooping, crouching, or kneeling; reaching one’s head; lifting; or carrying a bag of rice (8 kg). The items were scored from 0 to 3, corresponding to the degree of difficulty in performing individual tasks (response options: not difficult at all = 0, 1 = a lot of difficulty, 2 = some difficulty, and 3 = none). The total score was obtained by adding the points collected for each item divided by 5 and then dividing the score by 3 and multiplying it by 100 to obtain a total score of 100, with higher scores indicating better mobility. This variable was categorized as Level 1 (≤60), Level 2 (≤86.67), or Level 3 (≤100) with respect to the total score.
Social factors included social participation and social network contact. Social participation was based on the survey question, “Have you been involved in club activities (club activities), social groups (class reunions, mutual aid meetings, etc.), or political and social groups in the last year?” The response options were yes or no. Social network contact was based on the survey question, “During the past year, how often have you communicated with friends, neighbors, or acquaintances (via phone calls, cell phone texts and instant messages, email, etc.)?” This variable was categorized as less than once per month, more than once per month, or more than once per week.
Physical environment was measured as the individual’s proximity to parks and trails based on the survey question, “How long does it take to go from the house where you live to the park where you can go for a walk or exercise?” This variable was categorized as within 10 min, 10–20 min, and more than 20 min.
The number of rooms and smartphone or tablet PC using are variables that reflect the quarantine situation due to COVID-19. We predicted that the presence of a room in which PAEXP could be performed while outside access was restricted would influence PAEXP. This assumption was based on the results of a previous study which showed that the larger the interior space, the higher the PAEXP [55]. We also predicted that the use of a virtual exercise program that uses new technology would influence PAEXP in the COVID-19 lockdown, during which virtual interactions became commonplace. This assumption was based on a previous study that reported a positive correlation between ICT use and PAEXP in the context of physical distancing caused by the COVID-19 pandemic [56,57]. The number of rooms was reported by participants, and this variable was categorized as one room, two rooms, three rooms, or more than three rooms. Smartphone or tablet PC using was based on a question asking whether the individual was currently using these devices, and the response options were yes and no.
3.4. Statistical Analysis
Chi-squared tests were used to explore participants’ characteristics and test the bivariate relationships between PAEXP and the independent variables. Statistical significance was set at a p-value of <0.05. Logistic regression and decision tree analyses were used to identify factors influencing PAEXP. Such analyses are widely used to identify predictors of dichotomous dependent variables [58].
Logistic regression is similar to linear regression, but it linearizes the model by performing a logit transformation on a dichotomous dependent variable [59]. This is an effective method for analyzing the effects of a set of independent variables on a response variable by quantifying the unique contribution of each independent variable [60].
A decision tree analyses the hierarchical influences of multiple independent variables on a response variable and displays them as a visual model [61]. Decision trees are composed of nodes and branches through splitting, stopping, and pruning steps. Algorithms such as chi-squared automatic interaction detection (CHAID), classification and regression tree (CART), and quick, unbiased, efficient, statistical tree (QUEST) are used to build tree models [62].
Logistic regression analysis is useful for determining how each independent variable affects the dependent variable, whereas the decision tree analysis is useful for determining relationships in the data by showing how important variables interact with each other [63].
In this study, we used a combination of both methods to effectively identify factors that influence PAEXP. For the logistic regression analysis, we used the “enter” variable selection method to enter all variables in the block at once. The goodness-of-fit of the model was assessed using the Hosmer–Lemeshow goodness-of-fit test, which is a popular method for assessing the goodness-of-fit of a logistic regression model, with a p-value > 0.05. interpreted as being a good fit. Statistical significance was set at a p-value of <0.05. The decision tree analysis was employed to build a tree model using the chi-squared automatic interaction detector (CHAID) algorithm, which performs multiple splits with a chi-squared test with a significance level of p = 0.05. This model was validated using split-sample validation, which randomized the ratio of training and validation data to 50:50.
For model estimation, the maximum number of iterations was set to 100, and the minimum change in the expected cell frequency was set to 0.05. The maximum tree depth was set to 3, with 100 minimum cases in the parent node and 50 minimum cases in the child node. Data analyses were performed using SPSS version 22 (IBM Corporation, Armonk, NY, USA).
4. Results
4.1. Subject Characteristics
The chi-squared test was conducted to confirm the difference in PAEXP according to sociodemographic information, and the results are shown in Table 1 below. The difference verification was conducted with a 95% confidence level (p < 0.05). The chi-squared test results shown in Table 1 show that 20 predictors (p < 0.05), excluding smoking (p > 0.05), had significant effects on PAEXP.

Table 1.
Subject characteristics (N = 9920).
A total of 9920 subjects aged 65 years and older were included in the study, 4733 (47.7%) in the nonexercise group and 5187 (52.3%) in the exercise group, with a 4.6% difference in favor of the exercise group.
Regarding the predictors, both the exercise and nonexercise groups had higher percentages in the following categories: 65–69, female, married, urban area, paid work (yes), household income (≤2708.25), number of chronic diseases (1–2), smoking (no), nutritional status (good), BMI (normal weight), depression (no), healthy, functional limitations (no), social network contact (≥once a week), proximity to parks and trails (≤10 min), and 3 rooms or more.
In terms of educational level, the elementary school category (37%) had the highest rate in the nonexercise group, and the high school category (30.2%) had the highest rate in the exercise group.
In terms of physical ability, Level 1 (the lowest level of physical ability, 61.8%) had the highest rate in the nonexercise group, and Level 3 (the highest level of physical ability, 63%) had the highest rate in the exercise group.
In terms of social participation, the nonexercise group had a higher percentage of “no” responses (55.2%), and the exercise group had a higher percentage of “yes” responses (62.8%).
In terms of using a smartphone or tablet PC, the nonexercise group had a higher percentage of “no” responses (58.5%), and the exercise group had a higher percentage of “yes” responses (60.1%).
4.2. Results of the Logistic Regression Analysis
Table 2 shows the results of the logistic regression analysis. The model fit was adequate, with p = 0.133 in the Hosmer–Lemeshow tests.

Table 2.
Logistic regression model of exercise participation by older adults.
Age, gender, educational level, residential area, paid work, household income, number of chronic diseases, smoking, nutritional status, depression, health status, functional limitation, physical function, social participation, social network contact, and smartphone and tablet PC use were significantly associated with PAEXP in the logistic regression analysis.
The effects of marital status, BMI, and proximity to parks and trails on PAEXP were insignificant in the 95% confidence interval. Although not shown here, the results of the backward stepwise regression were also consistent with the logistic regression results, showing insignificant (p > 0.05) effects of marital status, BMI, and proximity to parks and trails on PAEXP.
Compared to the 65–69-year-old group, the 70–74- and 75–79-year-old groups had 1.178 times and 1.201 times higher PAEXP levels, respectively. On the other hand, in the case of the group aged over 85 years, the PAEXP level was lower than that of the 65–59-year-old group. In other words, increased age does not simply decrease the PAEXP level. Many previous studies [64,65] have reported that the older group of older adults showed a lower PAEXP level than the younger group of older adults. Yasunaga et al. [64] investigated the association between age and the PAEXP level in 95 Japanese people. They showed a significant negative association between age and PAEXP. Their results were significantly greater in the 65–74-year-old group than in the 75–83-year-old group. Lohne-Seiler et al. [65] showed that PAEXP level differed considerably between the age groups, whereby the oldest adults (80–85 years) displayed a 50% lower PAEXP level compared to those in the youngest group (65–70 years).
Males had higher odds of participating in PAEXP than females. The odds ratio, for individuals with a level of education above college level participating in PAEXP was 1.731 times higher than that of the uneducated. However, an increase in educational level did not mean an increase in PAEXP.
Living in an urban area (OR = 1.408), not smoking (OR = 1.408), not having depression (OR = 1.347), being healthy (OR = 1.164), having no functional limitations (OR = 1.706), social participation (OR = 1.453), and smartphone or tablet use (OR = 1.484) were all associated with higher odds for participating in PAEXP.
When the housing income increased up to 27.08 M, the PAEXP also increased, but when the housing income was higher than that level, an increase in the household income did not increase the PAEXP.
As the level of physical function increased, the odds ratio for PAXEP participation increased by 1.454 times and 1.948 times, respectively. This increase in the odds ratio is the highest increase among all factors, and it means that physical function one of the most important factors in determining participation in PAXEP.
The impact on PAEXP increases when social contact occurs more than once per month, but above that, increasing social contact did not increase PAEXP further.
The odds ratio of people with ≥3 chronic diseases participating in PAEXP decreased compared to that in those with no chronic diseases. This result is in contrast to results from previous studies [24,66]. Ashe et al. [24]’s study showed that for older adults with no chronic diseases, 30% reported meeting the guidelines for leisure-time physical activity (LTPA), while only 23% met the recommendations if they had one or more chronic diseases. However, this result might be interpreted as meaning that if the number of chronic diseases increases to more than three, the older adults increase their health awareness and increase their willingness to participate in PAEXP. In Barker et al. [66]’s study, the experimental group with chronic diseases had 9% lower rates of moderate activity and completed 11% less vigorous activity per week than the comparison group without chronic diseases.
Individuals with a better nutritional status had lower PAEXP, which is a different result than expected.
4.3. Results of the Decision Tree Analysis
Figure 2 shows the results of a decision tree analysis. A decision tree was built with test data from 4992 of the 9920 subjects (training data: 4928).
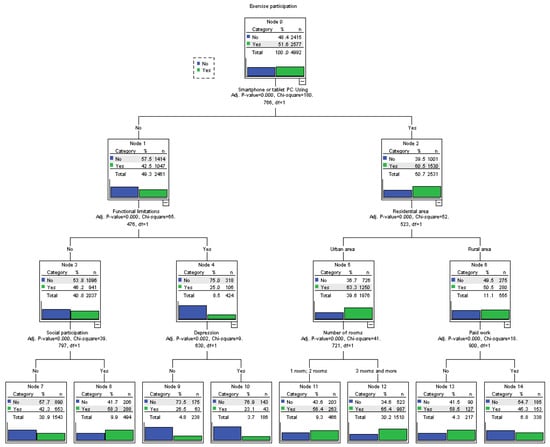
Figure 2.
Decision tree model of exercise participation by older adults.
This model included 15 nodes with seven predictors: smartphone or tablet PC use, functional limitations, residential area, social participation, depression, number of rooms, and paid work. The seven predictors were the final variables that influenced exercise participation and were derived from the decision tree analysis.
Node 0 at the top is the root node, representing the state in which no predictors are input, and it represents the baseline. At the root node, the exercise participation rate (51.6%) was higher than that of the nonexercise participation rate (48.4%). The most important predictor of exercise participation was smartphone or tablet PC use, which was associated with higher exercise participation rates. Based on the terminal node, there were a total of eight profiles.
In the case of using a smartphone or tablet PC in an urban area with three rooms and more, the exercise participation rate was 65.4% (Node 12). Under the same conditions, in the case of having fewer than three rooms (one or two), the exercise participation rate was 56.4%. (Node 11). In the group that used smartphones or tablet PCs in urban areas, the number of available rooms was the most powerful predictor (chi-square = 41.721, p < 0.001). Specifically, a higher number of rooms was associated with a higher rate of exercise participation.
In the case of using a smartphone or tablet PC while living in a rural area, the rate of exercise participation varied greatly depending on whether paid work was involved. In the case of not having paid work, the rate of exercise participation (58.5%) was higher than the rate of not participating in exercise, while in the case of having paid work, the rate of not participating in exercise (54.7%) was higher than the rate of exercise participation (nodes 13–14). This means that paid work was the most powerful predictor in the group that used a smartphone or tablet PC while living in a rural area (chi-square = 18.900, p < 0.001).
In the case of those not using a smartphone or tablet PC in individuals with functional limitations and depression, the rate of not participating in exercise was 76.9% (Node 10). Under the same conditions, for the case of individuals without depression, the rate of not participating in exercise was 73.5% (Node 9). In the group who did not use a smartphone or tablet PC, having functional limitations and depression were significant predictors (chi-square = 9.630, p < 0.01) of not participating in exercise.
In the case of not using a smartphone or tablet PC and having no functional limitations, the rate of exercise participation varied greatly depending on whether individuals had social participation. This means that social participation was the most powerful predictor in the group of individuals using a smartphone or tablet PC who had no functional limitations (chi-square = 39.797, p < 0.001). In the case of social participation, the rate of exercise participation (58.3%) was higher than the rate of not exercising (Node 8), and in the case of not having social participation, the rate of not participating in exercise (57.7%) was higher than the rate of exercise participation (Node 7).
5. Discussion
This study aimed to identify factors influencing physical activity and exercise participation in older adults during the physical distancing period implemented as a measure to prevent the spread of COVID-19. Large quantities of data from surveys conducted on older adult Korean individuals in the 2020 NSOK (n = 9920) were used, and logistic regression and decision tree analyses were performed.
At baseline, only 52.3% of participants reported exercise participation, which is a significant drop compared with the results of the 2017 NSOK survey conducted before the outbreak of COVID-19 (68%) [8]. Considering that older adults are not sufficiently engaged [67] and that inactive lifestyles negatively impact their health [11], more continuous active measures must be established to promote PAEXP in older adults in preparation for unexpected environmental changes, such as the COVID-19 pandemic.
Logistic regression analysis was used to identify the following factors influencing PAEXP: age, gender, educational level, residential area, paid work, household income, number of chronic diseases, smoking, nutritional status, depression, health status, functional limitations, physical function, social participation, social network contact, and smartphone or tablet PC using.
Consistent with previous studies [17,21,23,25,26,28,29,30,31], the following factors were identified as causing higher PAEXP: being male, having a high educational level, living in urban areas, having a high household income, not smoking, having a good nutritional status, the absence of depression, having a high health status, having low functional limitations, having high physical functions, engagement in social participation, and engagement with many social network contacts.
The influences of most variables were similar to those identified in the previous studies mentioned above but with some different characteristics. It is generally known that PAEXP decreases with age. However, this study found different PAEXP rates in each age group. Specifically, the PAEXP rate was higher in the 70–74- and 75–79-year age groups than in the 65–69-year age group, and the PAEXP rate was lower in the 85 years and older age group [68], in which the rapid deterioration of physical function is known to occur. This indicates that the effect of age on PAEXP in the older adult generation is limited under the quarantine conditions caused by the outbreak of COVID-19. This finding suggests that promotional strategies for PAEXP in the older adult population need to be further refined.
According to previous studies [32] which reported that a high household income has a positive effect on PAEXP, paid work is predicted to increase PAEXP, and job losses are associated with a reduced PAEXP [23]. The results of this study also show that having an appropriate household income has a positive effect on PAEXP. This suggests that a cost-free PAEXP program needs to be supported in consideration of the economic aspects of the older adults.
PAEXP prescriptions are the most widely used interventions for the prevention of chronic diseases. By reporting that exercise guidelines are met when chronic diseases are absent but are not met when one or more chronic diseases are present, previous studies [24] have shown that the number of chronic diseases is associated with a lower PAEXP. However, contrary to previous studies, our results show that the number of chronic diseases is associated with a higher PAEXP. This can be interpreted [69] as the fact that older adults with chronic diseases have greater health motivation and participated in exercise more under the quarantine conditions caused by the outbreak of COVID-19. However, further evidence is needed to support this claim. It is not desirable to maintain a low level of PAEXP just because one has no chronic diseases. The incidence of chronic disease tends to increase with age [70], because a decrease in PAEXP can be a direct cause of disease [66]. Therefore, the promotion of PAEXP is necessary for all older adults, regardless of the presence or absence of chronic diseases.
Smartphone or tablet PC using has been identified as a new and important variable that influences higher PAEXP, although its influence was not well known in relation to older adults’ PAEXP. Smartphone or tablet PC using is an important approach that can promote PAEXP in quarantine conditions, and attention was drawn mainly to home training during the actual COVID-19 period [47]. Before the COVID-19 outbreak, previous studies [71] reported that mHealth and eHealth interventions based on the use of smartphones or tablet PC use increase PAEXP in older adults. In addition, there are studies showing that the use of ICT devices was significantly associated with PAEXP during COVID-19 confinement [56,57]. Our results support the results of these previous studies [56,57] and simultaneously extend the validity of results showing the factors influencing PAEXP during the COVID-19 lockdown. Therefore, in order to maintain and promote the PAEXP of older adults, it is necessary to continue to pay attention to the application of ICT devices such as smartphones or tablet PCs. These results highlight the importance of introducing new empirical data to understand PAEXP among older adults in a changing environment.
Through the decision tree analysis, seven factors that influence exercise participation (smartphone or tablet PC using, functional limitations, residential area, social participation, depression, number of rooms, and paid work) and eight rules were derived through a combination of these factors. Smartphone or tablet PC using turned out to be the strongest predictor for classifying exercise participation in the decision tree analysis, and a series of rules were derived based on these factors.
For smartphone or tablet PC using, four terminal nodes were built based on the residential area. Paid work is a strong classification criterion for those living in rural areas who use smartphones or tablet PC, and those who do not have paid work show higher PAEXP rates than those who do. The result showing that the PAEXP ratio was lower in older adults who had paid work compared with those did not can be explained as follows: The work of older adults, whose residential area is rural, generally involves physical labor, such as farming. In this case, it can be seen that older adults living in rural areas equate physical labor with PAEXP or avoid PAEXP due to physical exhaustion [72]. Additionally, the number of rooms was a strong classification criterion for those living in urban areas who used a smartphone or tablet PC, with a large number of rooms being correlated with a higher PAEXP rate. While the number of rooms was a statistically insignificant variable in exercise participation in the logistic regression analysis, it acted as an important variable in the decision tree analysis for determining PAEXP in the case of living in urban areas and using a smartphone or tablet PC. In a situation where PAEXP has spread to home-based indoor exercise due to the COVID-19 lockdown [73], having indoor space is associated with (urban) older adults’ participation in PAEXP. The presence of a wider interior space, evaluated by the number of rooms, has been shown to act as a variable that predicts a higher PAEXP, which is supported by previous studies [55].
For individuals not using a smartphone or tablet PC, four terminal nodes were built based on functional limitations. Depression is a classification criterion for those with functional limitations who do not use smartphones or tablet PC, but it is difficult to interpret depression as a strong classification criterion, because there is little difference in the exercise participation rate between the two classified nodes (Nodes 9 and 10). Social participation is a strong classification criterion for those without functional limitations who do not use a smartphone or tablet PC, and those who engaged in social participation showed a higher PAEXP rate than those who did not. This result supports the results of previous studies [74] that reported the association between social participation and PAEXP during the physical distancing period caused by the COVID-19 pandemic, and it suggests that social activities are an important factor in maintaining PAEXP for older adults who do not have functional restrictions, regardless of the use of smartphones or tablet PCs.
Our results verify the influences of various variables on PAEXP in the social isolation environment caused by the COVID-19 pandemic and show that ‘smartphone or table PC use’ is an important factor in participation in PAEXP among various variables. The ‘smartphone or tablet PC use’ variable was found to be an important variable affecting PAEXP in both the logistic regression analysis and the decision tree analysis. This suggests that the use of ICT devices during times of unexpected environmental changes, such as the COVID-19 lockdown, can be an approach to effectively promote PAEXP in older adults. In addition, the application of ICT technology has the potential to be applied to various environments, such as by providing customized physical activity [75], for free use [76], for the management of chronic diseases [77], by rural distribution [78], and in home-based exercise applications [79]. However, there is an important problem that needs to be solved in order to promote PAEXP through smartphone or table PC use. It is the ability of older adults to use digital information devices. In Korea, the number of older adults using digital devices, such as smartphones or tablet PCs, has steadily increased to a smart device ownership rate of 77.1%. However, the level of digital device utilization by older adults is 34.9%, which is only half that of the general public (64.9%) [80]. Therefore, in order to ensure the continuation of older adult’s PAEXP in response to unexpected environmental changes, such as COVID-19, efforts should be continued to promote older adults’ ICT utilization capabilities. To this end, governments and nonprofit organizations need to provide educational services to improve the digital literacy of older adults and community organizations, and community volunteers should also seek ways to participate in efforts to improve ICT education for older adults living in the region [76].
In addition, policymakers should consider the following: In a quarantine situation, due to measures to prevent the spread of COVID-19 transmission, we confirmed that the older age groups and older adults who work to maintain their livelihoods are exposed to health risks because they do not participate in PAEXP. Thus, a strategy to promote PAEXP for underprivileged older adults should first be prepared. The strategy of increasing PAEXP via ICT can be effective, as outlined above. Offering low-cost internet-based PAEXP access, free online PAEXP resources, and even customized e-devices may be strategically supported at the public level.
6. Conclusions
This study aimed to establish the basic data needed to prepare a sustainable health strategy for older adults by identifying factors that affect exercise participation using the 2020 NSOK data on the Korean older adults (n = 9920) in 2020, where social confinement has become common due to the COVID-19 pandemic. Based on previous studies, 20 independent variables and questions regarding exercise participation were set as dependent variables. Logistic regression and decision tree analyses were performed to identify the factors affecting physical activity and exercise participation through the influences of individual variables and combinations of variables. Logistic regression analysis was used to identify the following factors influencing exercise participation: age, sex, educational level, residential area, paid work, household income, number of chronic diseases, smoking, nutritional status, depression, health status, functional limitations, physical function, social participation, social network contact, and smartphone or tablet PC using. Through a decision tree analysis, seven factors that influence exercise participation (smartphone or tablet PC using, functional limitations, residential area, social participation, depression, number of rooms, and paid work) were identified, and eight rules were derived through a combination of these factors.
The results of this study show that various influencing factors, rather than a single factor, affect physical activity and exercise participation in older adults through individual and combined effects in the context of COVID-19. Above all, ‘smartphone or table PC using’, which has not been well known previously, was identified as a factor that has a significant effect on PAEXP in older adults.
PAEXP has been reported to help prevent depression and dementia in older adults. Therefore, PAEXP, which has no side effects and a low cost, is quite important for older adults. However, in lockdown situations, such as during periods of physical distancing in the COVID-19 pandemic, older adults are significantly restricted from PAEXP. Since the world is closely connected, if a situation such as the COVID-19 pandemic occurs in one country, it is likely to spread rapidly around the world. Korea is an aging society. In Korea, where the older adult population is increasing, knowing the factors that affect the older adults’ PAEXP can be actively used for counseling the older adults and can be used as basic data for the older adults’ PAEXP programs.
The strengths of this study are as follows: First, it identified the factors influencing PAEXP in older adults based on the temporal background of COVID-19, which had not previously been ascertained. In addition, a large sample size and wide range of variables were input into both the logistic regression and decision tree models to secure a high explanatory power for factors influencing PAEXP in older adults. There was also a progressive attempt to consider a new variable (smartphone or tablet PC using) that had not been dealt with in previous studies.
The limitations of this study are as follows: NSOK was designed and investigated with a wide range of variables. For this reason, there was a limit to the analysis of data to verify in-depth and diverse causality in terms of PAEXP. The investigator’s subjectivity could not be completely removed from data preprocessing, and the rationale for the recategorization of some variables in the recategorization process was weak due to the complexity of the raw data. Gender differences may exist, but in this study, gender was not considered in the decision tree analysis. In future studies, a decision tree analysis should be conducted by dividing gender to identify how predictors differ between men and women. In addition, the explanation of the causal relationships among variables are limited because data based on the collection of cross-sectional data were used. More in-depth research seems to be needed through longitudinal studies with at least two points in time. Additionally, the generalization of these data is not free from bias, since the analyzed research data only cover South Korea.
Author Contributions
Conceptualization, K.J. and Y.C.; methodology, K.J. and Y.C.; formal analysis, K.J. and Y.C.; data curation, K.J. and Y.C.; writing—original draft preparation, K.J. and Y.C.; writing—review and editing, K.J. and Y.C.; visualization, K.J. and Y.C.; supervision, K.J. and Y.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The use of the 2020 NSOK data in this study was approved by the National Statistical Office (Approval No. 117071) and the Institutional Review Board of the Korea Institute for Health and Social Affairs (IRB No. 20-029-00). The researcher received these data without personally identifiable information after receiving approval from the Korea Institute for Health and Social Affairs. Exemption from approval (IRB No. P01-202212-01-038) was also obtained to conduct this research from the Public Institutional Review Board Designated by the Ministry of Health and Welfare.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors have no authority over the data, which were provided upon request from the Korea Institute for Health and Social Affairs. (https://data.kihasa.re.kr/kihasa/kor/contents/ContentsList.html (accessed on 11 October 2022)).
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. Title of Site. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 1 December 2022).
- Sun, P.; Lu, X.; Xu, C.; Sun, W.; Pan, B. Understanding of COVID-19 based on current evidence. J. Med. Virol. 2020, 92, 548–551. [Google Scholar] [CrossRef] [PubMed]
- Pombo, A.; Luz, C.; Rodrigues, L.P.; Ferreira, C.; Cordovil, R. Correlates of children’s physical activity during the COVID-19 confinement in Portugal. Public Health 2020, 189, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M.; Bovo, C.; Sanchis-Gomar, F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis 2020, 7, 85–90. [Google Scholar] [CrossRef] [PubMed]
- You, M.H.; Choi, Y.J.; Kim, J.Y. Impact of the COVID-19 social distancing policy on the exit and entry of stores in South Korea. Korea World Econ. 2022, 23, 57–75. [Google Scholar] [CrossRef]
- Lim, B.; Kyoungseo Hong, E.; Mou, J.; Cheong, I. COVID-19 in Korea: Success based on past failure. Asian Econ. Pap. 2021, 20, 41–62. [Google Scholar] [CrossRef]
- Park, A.H.; Zhong, S.; Yang, H.; Jeong, J.; Lee, C. Impact of COVID-19 on physical activity: A rapid review. J. Glob. Health 2022, 12, 05003. [Google Scholar] [CrossRef]
- Chung, K.J.; Kang, E.N.; Kim, K.R.; Oh, Y.H.; Oh, M.A.; Lee, Y.K.; Hwang, N.H.; Kim, S.J.; Lee, S.H.; Lee, S.; et al. 2017 National Survey of Older Koreans; Ministry of Health and Welfare and Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2017. [Google Scholar]
- Lee, Y.K.; Kim, S.J.; Hwang, N.H.; Lim, J.M.; Joo, B.H.; Namgung, E.H.; Lee, S.H.; Jeong, K.H.; Kang, E.N.; Kim, K.R. 2020 National Survey of Older Koreans; Ministry of Health and Welfare and Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2020. [Google Scholar]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: A cross-sectional online survey. J. Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef]
- Chambonniere, C.; Lambert, C.; Tardieu, M.; Fillon, A.; Genin, P.; Larras, B.; Melsens, P.; Baker, J.; Pereira, B.; Tremblay, A. Physical activity and sedentary behavior of elderly populations during confinement: Results from the FRENCH COVID-19 ONAPS survey. Exp. Aging Res. 2021, 47, 401–413. [Google Scholar] [CrossRef]
- Wilke, J.; Mohr, L.; Tenforde, A.S.; Edouard, P.; Fossati, C.; González-Gross, M.; Sánchez Ramírez, C.; Laiño, F.; Tan, B.; Pillay, J.D. A pandemic within the pandemic? Physical activity levels substantially decreased in countries affected by COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2235. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major noncommunicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Spence, J.C.; Rhodes, R.E.; McCurdy, A.; Mangan, A.; Hopkins, D.; Mummery, W.K. Determinants of physical activity among adults in the United Kingdom during the COVID-19 pandemic: The DUK-COVID study. Br. J. Health Psychol. 2021, 26, 588–605. [Google Scholar] [CrossRef] [PubMed]
- Hollmann, W.; Strüder, H.K.; Tagarakis, C.V.; King, G. Physical activity and the elderly. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 730–739. [Google Scholar] [CrossRef] [PubMed]
- Yao, L.; Fang, H.; Leng, W.; Li, J.; Chang, J. Effect of aerobic exercise on mental health in older adults: A meta-analysis of randomized controlled trials. Front. Psychiatry 2021, 12, 748257. [Google Scholar] [CrossRef] [PubMed]
- Bertera, E.M. Physical Activity and Social Network Contacts in Community Dwelling Older Adults. Act. Adapt. Aging 2003, 27, 113–127. [Google Scholar] [CrossRef]
- Schutzer, K.A.; Graves, B.S. Barriers and motivations to exercise in older adults. Prev. Med. 2004, 39, 1056–1061. [Google Scholar] [CrossRef]
- Park, C.H. Experience of sport stacking in Korean older adults. J. Exerc. Rehabil. 2017, 13, 43–47. [Google Scholar] [CrossRef]
- Booth, M.L.; Owen, N.; Bauman, A.; Clavisi, O.; Leslie, E. Social–cognitive and perceived environment influences associated with physical activity in older Australians. Prev. Med. 2000, 31, 15–22. [Google Scholar] [CrossRef]
- Park, S.; Park, Y.H. Predictors of Physical Activity in Korean Older Adults: Distinction between Urban and Rural Areas. J. Korean Acad. Nurs. 2010, 40, 191–201. [Google Scholar] [CrossRef]
- Pettee, K.K.; Brach, J.S.; Kriska, A.M.; Boudreau, R.; Richardson, C.R.; Colbert, L.H.; Satterfield, S.; Visser, M.; Harris, T.B.; Ayonayon, H.N. Influence of marital status on physical activity levels among older adults. Med. Sci. Sports Exerc. 2006, 38, 541–546. [Google Scholar] [CrossRef]
- Shaw, B.A.; Spokane, L.S. Examining the association between education level and physical activity changes during early old age. J. Aging Health 2008, 20, 767–787. [Google Scholar] [CrossRef]
- Ashe, M.C.; Miller, W.C.; Eng, J.J.; Noreau, L. Older adults, chronic disease and leisure-time physical activity. Gerontology 2009, 55, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Stiggelbout, M.; Hopman-Rock, M.; Crone, M.; Lechner, L.; Van Mechelen, W. Predicting older adults’ maintenance in exercise participation using an integrated social psychological model. Health Educ. Res. 2006, 21, 1–14. [Google Scholar] [CrossRef] [PubMed]
- da Silva, L.S.L.; de Freitas Batalhão, D.; Dos Santos Carvalho, A.; Bohn, L.; Ramos, N.C.; Abdalla, P.P. Nutritional status, health risk behaviors, and eating habits are correlated with physical activity and exercise of brazilian older hypertensive adults: A cross-sectional study. BMC Public Health 2022, 22, 2382. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas Fuentes, G.; Bawaked, R.A.; Martínez González, M.Á.; Corella, D.; Subirana Cachinero, I.; Salas-Salvadó, J.; Estruch, R.; Serra-Majem, L.; Ros, E.; Lapetra Peralta, J. Association of physical activity with body mass index, waist circumference and incidence of obesity in older adults. Eur. J. Public Health 2018, 28, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Marx, M.S.; Guralnik, J.M. Motivators and barriers to exercise in an older community-dwelling population. J. Aging Phys. Act. 2003, 11, 242–253. [Google Scholar] [CrossRef]
- Souza, A.M.; Fillenbaum, G.G.; Blay, S.L. Prevalence and correlates of physical inactivity among older adults in Rio Grande do Sul, Brazil. PLoS ONE 2015, 10, e0117060. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, M.S.; Newsom, J.T.; McFarland, B.H.; Lu, L. Demographic and psychosocial correlates of physical activity in late life. Am. J. Prev. Med. 2001, 21, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.; Taylor, L. Factors associated with physical activity among older people—a population-based study. Prev. Med. 2005, 40, 33–40. [Google Scholar] [CrossRef]
- Lee, Y.S.; Levy, S.S. Gender and income associations in physical activity and blood pressure among older adults. J. Phys. Act. Health 2011, 8, 1–9. [Google Scholar] [CrossRef]
- Eyler, A.A.; Brownson, R.C.; Donatelle, R.J.; King, A.C.; Brown, D.; Sallis, J.F. Physical activity social support and middle-and older-aged minority women: Results from a US survey. Soc. Sci. Med. 1999, 49, 781–789. [Google Scholar] [CrossRef]
- Chaudhury, H.; Campo, M.; Michael, Y.; Mahmood, A. Neighbourhood environment and physical activity in older adults. Soc. Sci. Med. 2016, 149, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Michael, Y.C.; Perdue, L.A.; Orwoll, E.S.; Stefanick, M.L.; Marshall, L.M. Physical activity resources and changes in walking in a cohort of older men. Am. J. Public Health 2010, 100, 654–660. [Google Scholar] [CrossRef] [PubMed]
- Moran, M.; Van Cauwenberg, J.; Hercky-Linnewiel, R.; Cerin, E.; Deforche, B.; Plaut, P. Understanding the relationships between the physical environment and physical activity in older adults: A systematic review of qualitative studies. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Goethals, L.; Barth, N.; Guyot, J.; Hupin, D.; Celarier, T.; Bongue, B. Impact of Home Quarantine on Physical Activity Among Older Adults Living at Home During the COVID-19 Pandemic: Qualitative Interview Study. JMIR Aging 2020, 3, e19007. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Culture, Sports and Tourism. 2020 Korea National Sports Participation Survey; Ministry of Culture, Sports and Tourism: Sejong, Republic of Korea, 2020. [Google Scholar]
- Meyer, J.; Herring, M.; McDowell, C.; Lansing, J.; Brower, C.; Schuch, F.; Smith, L.; Tully, M.; Martin, J.; Caswell, S. Joint prevalence of physical activity and sitting time during COVID-19 among US adults in April 2020. Prev. Med. Rep. 2020, 20, 101256. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
- Qin, F.; Song, Y.; Nassis, G.P.; Zhao, L.; Dong, Y.; Zhao, C.; Feng, Y.; Zhao, J. Physical activity, screen time, and emotional well-being during the 2019 novel coronavirus outbreak in China. Int. J. Environ. Res. Public Health 2020, 17, 5170. [Google Scholar] [CrossRef]
- Lefferts, E.C.; Saavedra, J.M.; Song, B.K.; Lee, D.C. Effect of the COVID-19 pandemic on physical activity and sedentary behavior in older adults. J. Clin. Med. 2022, 11, 1568. [Google Scholar] [CrossRef]
- Yang, Y.; Koenigstorfer, J. Determinants of physical activity maintenance during the Covid-19 pandemic: A focus on fitness apps. Transl. Behav. Med. 2020, 10, 835–842. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Ahn, Y.K.; Kim, D.K.; Kwon, O.R.; Song, H.S.; Kim, H.S. Redefinition of Terms in Physical Education and Sport. J. Korean Soc. Philos. Sport Danc. Martial Arts 2011, 19, 33–60. [Google Scholar]
- Yomoda, K.; Kurita, S. Influence of social distancing during the COVID-19 pandemic on physical activity in children: A scoping review of the literature. J. Exerc. Sci. Fit. 2021, 19, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.Y.; Nam, S.B. How Has the Home Training Trend Changed before and after the COVID-19 Pandemic? J. Sport Leis. Stud. 2022, 90, 279–293. [Google Scholar] [CrossRef]
- Methods and Significance of Income Distribution Indicators. Available online: http://kostat.go.kr/incomeNcpi/income/income_dg/4/4/index.action (accessed on 1 January 2023).
- Posner, B.M.; Jette, A.M.; Smith, K.W.; Miller, D.R. Nutrition and health risks in the elderly: The nutrition screening initiative. Am. J. Public Health 1993, 83, 972–978. [Google Scholar] [CrossRef] [PubMed]
- National Heart, L.; Institute, B. Obesity Education Initiative: The Evidence Report; National Institutes of Health: Bethesda, MD, USA, 1998. [Google Scholar]
- Bae, J.N.; Cho, M.J. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J. Psychosom. Res. 2004, 57, 297–305. [Google Scholar] [CrossRef]
- Sheikh, J.; JA, Y. Brink TL. Geriatric Depression Scale (GDS): Recent Evidence and Development of a Shorter Version. Clinical Gerontology: A Guide to Assessment and Intervention; Haworth Press: New York, NY, USA, 1986. [Google Scholar]
- Won, C.W.; Yang, K.Y.; Rho, Y.G.; Kim, S.Y.; Lee, E.J.; Yoon, J.L.; Cho, K.J.; Shin, H.C.; Cho, B.R.; Oh, J.R. The development of Korean activities of daily living (K-ADL) and Korean instrumental activities of daily living (K-IADL) scale. J. Korean Geriatr. Soc. 2002, 6, 107–120. [Google Scholar]
- Lee, K.-J.; Han, G.-S.; Yoon, S.-J.; Lee, Y.-K.; Kim, C.-H.; Kim, J.-L.; Lee, Y.-H. The development of physical functioning scale for community-dwelling older persons. J. Prev. Med. Public Health 2002, 35, 359–374. [Google Scholar]
- Cress, M.E.; Orini, S.; Kinsler, L. Living environment and mobility of older adults. Gerontology 2011, 57, 287–294. [Google Scholar] [CrossRef]
- Satake, S.; Kinoshita, K.; Arai, H. More active participation in voluntary exercise of older users of information and communicative technology even during the COVID-19 pandemic, independent of frailty status. J. Nutr. Health Aging 2021, 25, 516–519. [Google Scholar] [CrossRef]
- Sasaki, S.; Sato, A.; Tanabe, Y.; Matsuoka, S.; Adachi, A.; Kayano, T.; Yamazaki, H.; Matsuno, Y.; Nakano, A.; Watanabe, T. Internet use and physical activity of older adults during the COVID-19 pandemic: A cross-sectional study in a northern Japanese City. BMC Geriatr. 2022, 22, 1–9. [Google Scholar] [CrossRef]
- Kim, Y.S.; An, H.G. Analysis of Stressful Life Event Factors Related to Suicidal Ideation in Specialized and Academic High School Female Students. J. Korean Data Anal. Soc. 2011, 13, 1293–1309. [Google Scholar]
- Antipov, E.; Pokryshevskaya, E. Applying CHAID for logistic regression diagnostics and classification accuracy improvement. J. Target. Meas. Anal. Mark. 2010, 18, 109–117. [Google Scholar] [CrossRef]
- Stoltzfus, J.C. Logistic regression: A brief primer. Acad. Emerg. Med. 2011, 18, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Kweon, Y.R.; Kim, S.Y. Predictors of Protective Factors for Internet Game Addiction in Middle School Students using Data Mining Decision Tree Analysis. J. Korean Acad. Psychiatr. Ment. Health Nurs. 2014, 23, 12–20. [Google Scholar] [CrossRef]
- Song, Y.-Y.; Ying, L. Decision tree methods: Applications for classification and prediction. Shanghai Arch. Psychiatry 2015, 27, 130. [Google Scholar]
- Fiskin, R.; Cakir, E.; Sevgili, C. Decision tree and logistic regression analysis to explore factors contributing to harbour tugboat accidents. J. Navig. 2021, 74, 79–104. [Google Scholar] [CrossRef]
- Yasunaga, A.; Togo, F.; Watanabe, E.; Park, H.; Park, S.; Shephard, R.J.; Aoyagi, Y. Sex, age, season, and habitual physical activity of older Japanese: The Nakanojo study. J. Aging Phys. Act. 2008, 16, 3–13. [Google Scholar] [CrossRef]
- Lohne-Seiler, H.; Hansen, B.H.; Kolle, E.; Anderssen, S.A. Accelerometer-determined physical activity and self-reported health in a population of older adults (65–85 years): A cross-sectional study. BMC Public Health 2014, 14, 1–10. [Google Scholar] [CrossRef]
- Barker, J.; Smith Byrne, K.; Doherty, A.; Foster, C.; Rahimi, K.; Ramakrishnan, R.; Woodward, M.; Dwyer, T. Physical activity of UK adults with chronic disease: Cross-sectional analysis of accelerometer-measured physical activity in 96 706 UK Biobank participants. Int. J. Epidemiol. 2019, 48, 1167–1174. [Google Scholar] [CrossRef]
- Park, C.-H.; Elavsky, S.; Koo, K.-M. Factors influencing physical activity in older adults. J. Exerc. Rehabil. 2014, 10, 45. [Google Scholar] [CrossRef]
- Guay, M.; Dubois, M.-F.; Corrada, M.; Lapointe-Garant, M.-P.; Kawas, C. Exponential increases in the prevalence of disability in the oldest old: A Canadian national survey. Gerontology 2014, 60, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.J.; Lee, H.N. Concept Analysis of Health Motivation in Patients with Chronic Disease. J. Korea Contents Assoc. 2021, 21, 575–586. [Google Scholar]
- Bloom, D.E.; Chen, S.; Kuhn, M.; McGovern, M.E.; Oxley, L.; Prettner, K. The economic burden of chronic diseases: Estimates and projections for China, Japan, and South Korea. J. Econ. Ageing 2020, 17, 100163. [Google Scholar] [CrossRef]
- McGarrigle, L.; Todd, C. Promotion of Physical Activity in Older People Using mHealth and eHealth Technologies: Rapid Review of Reviews. J. Med. Internet Res. 2020, 22, e22201. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Park, B. Exploration on the Health-related Factors of the Elderly in Rural Village based on the Social Ecological Model. J. Korean Public Health Nurs. 2021, 35, 415–429. [Google Scholar]
- De Maio, M.; Bratta, C.; Iannaccone, A.; Castellani, L.; Foster, C.; Cortis, C.; Fusco, A. Home-based physical activity as a healthy aging booster before and during COVID-19 outbreak. Int. J. Environ. Res. Public Health 2022, 19, 4317. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, S.; Sato, A.; Tanabe, Y.; Matsuoka, S.; Adachi, A.; Kayano, T.; Yamazaki, H.; Matsuno, Y.; Miyake, A.; Watanabe, T. Associations between socioeconomic status, social participation, and physical activity in older people during the COVID-19 pandemic: A cross-sectional study in a northern Japanese city. Int. J. Environ. Res. Public Health 2021, 18, 1477. [Google Scholar] [CrossRef] [PubMed]
- Niemiec, S.L.S.; Wagas, R.; Vigen, C.L.; Blanchard, J.; Barber, S.J.; Schoenhals, A. Preliminary User Evaluation of a Physical Activity Smartphone App for Older Adults. Health Policy Technol. 2022, 11, 100639. [Google Scholar] [CrossRef]
- Son, J.S.; Nimrod, G.; West, S.T.; Janke, M.C.; Liechty, T.; Naar, J.J. Promoting older adults’ physical activity and social well-being during COVID-19. Leis. Sci. 2021, 43, 287–294. [Google Scholar] [CrossRef]
- Vathsangam, H.; Sukhatme, G.S. Using phone-based activity monitors to promote physical activity in older adults: A pilot study. Proceedings of 2014 IEEE Healthcare Innovation Conference (HIC), Seattle, WA, USA, 8–10 October 2014; pp. 42–47. [Google Scholar]
- Kurti, A.N.; Logan, H.; Manini, T.; Dallery, J. Physical activity behavior, barriers to activity, and opinions about a smartphone-based physical activity intervention among rural residents. Telemed. E-Health 2015, 21, 16–23. [Google Scholar] [CrossRef]
- Ghram, A.; Briki, W.; Mansoor, H.; Al-Mohannadi, A.S.; Lavie, C.J.; Chamari, K. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgrad. Med. 2021, 133, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Science and ICT.; National Information Society Agency. The Report on the Digital Divide 2020; National Information Society Agency: Daegu, Republic of Korea, 2020. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).