Extreme Weather Conditions and Cardiovascular Hospitalizations in Southern Brazil
Abstract
1. Introduction
- (1)
- To understand whether the seasonality of hospitalizations for CVDs is correlated with extreme weather conditions (CWs and HWs);
- (2)
- To determine the worst thermal comfort classes in southern Brazil for CVD hospitalizations.
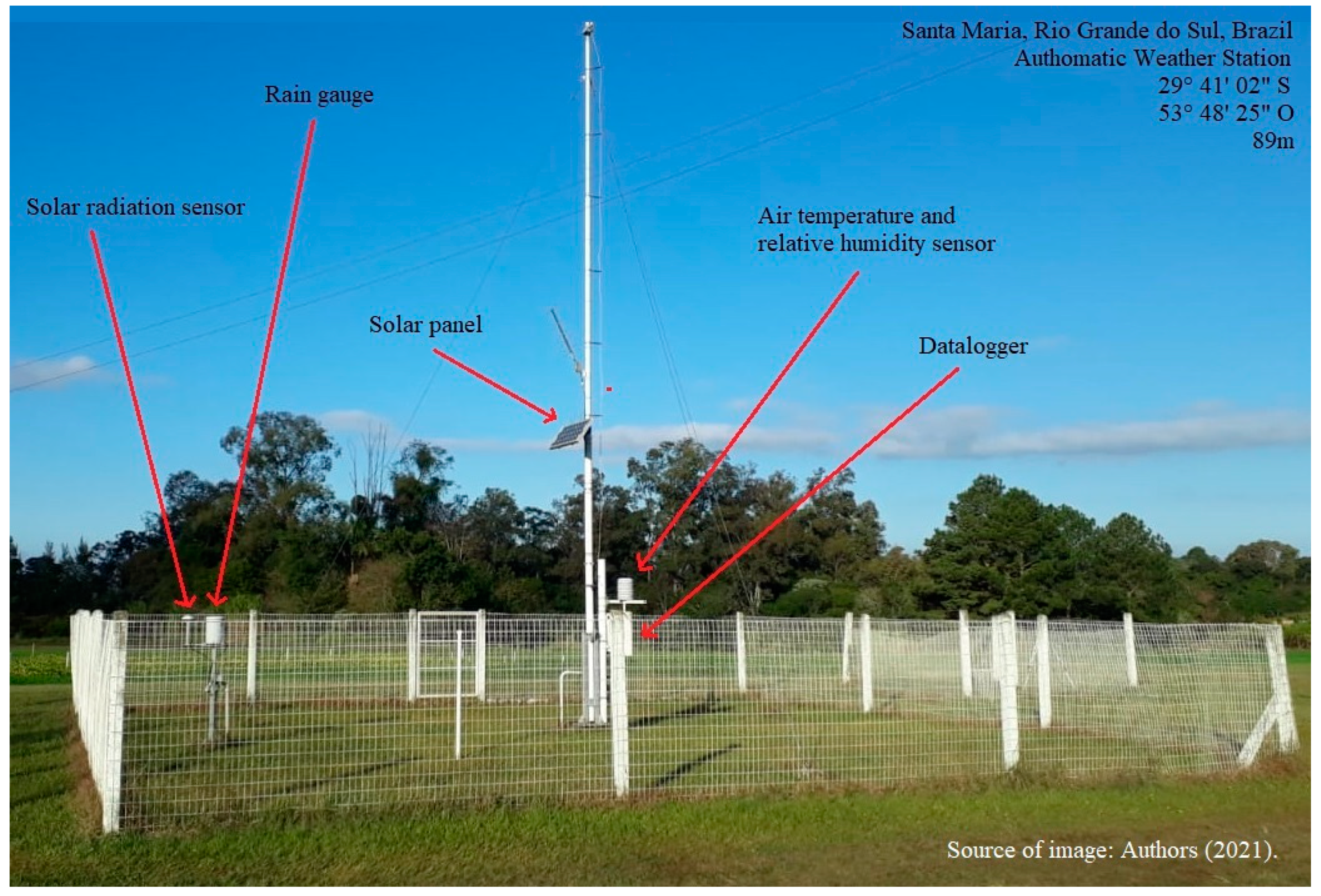
2. Materials and Methods
3. Results
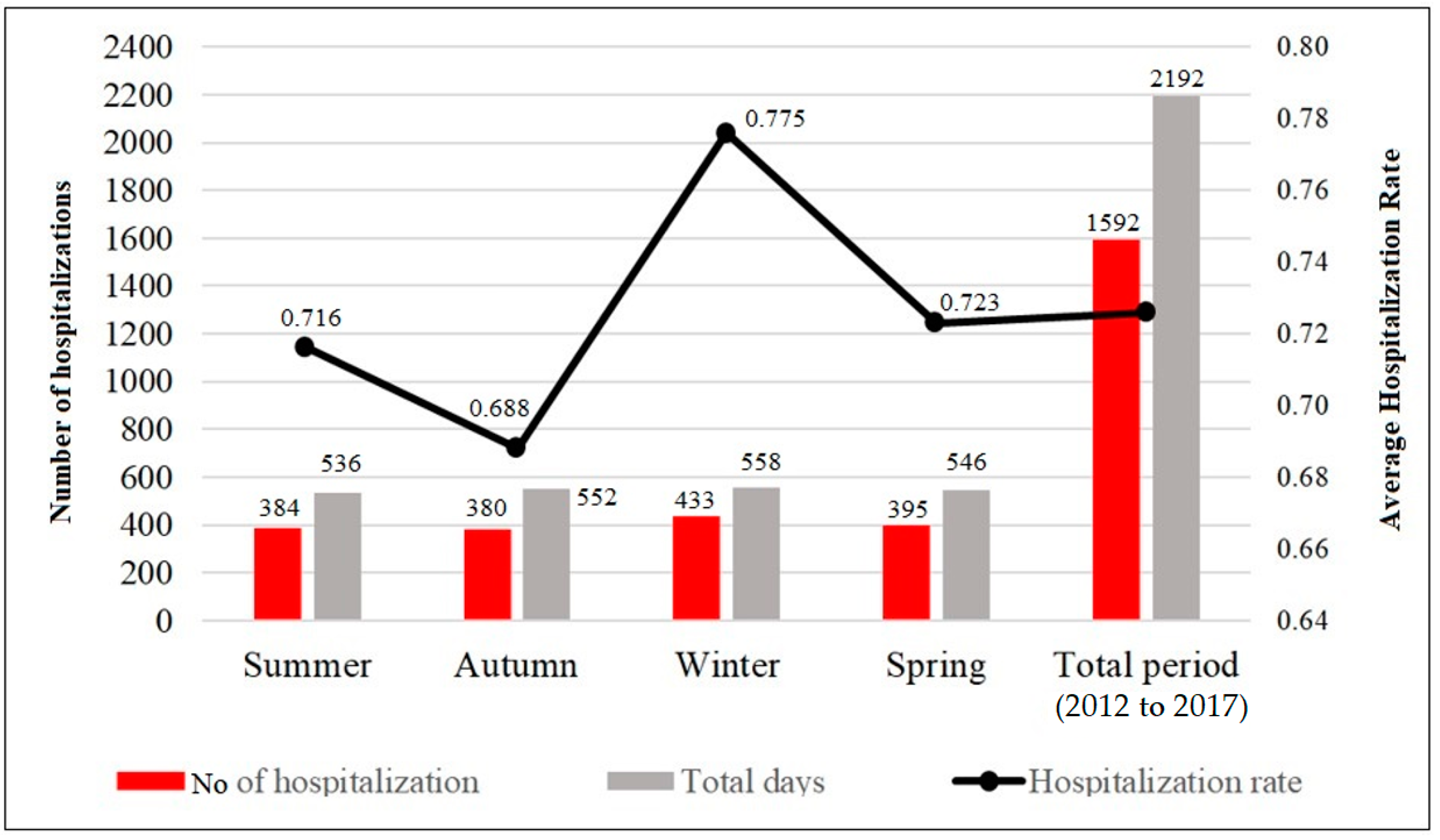
3.1. Seasonal Hospitalizations
3.2. Hospitalizations during Cold and Heat Waves
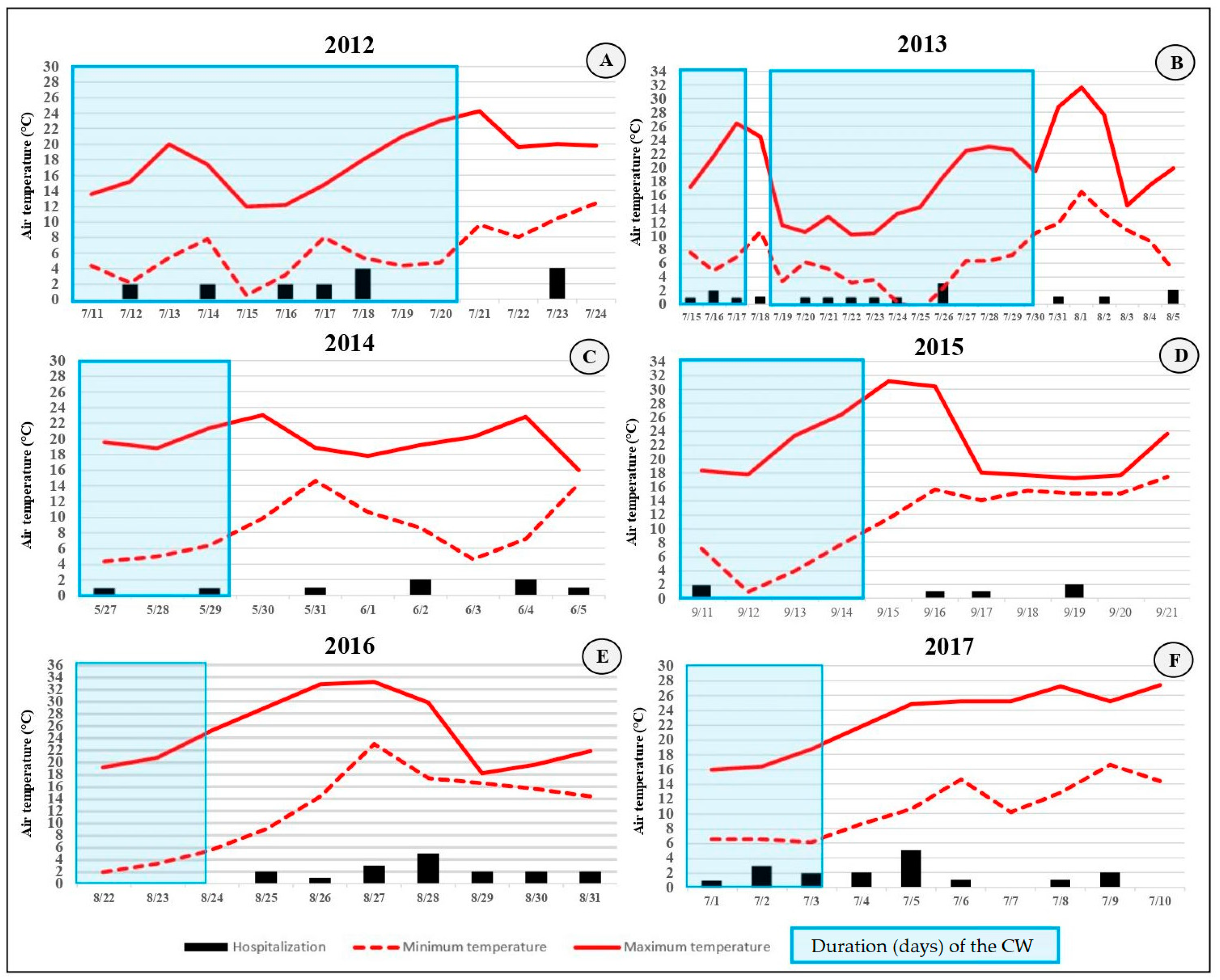
3.3. Hospitalizations during Representative Cold Waves
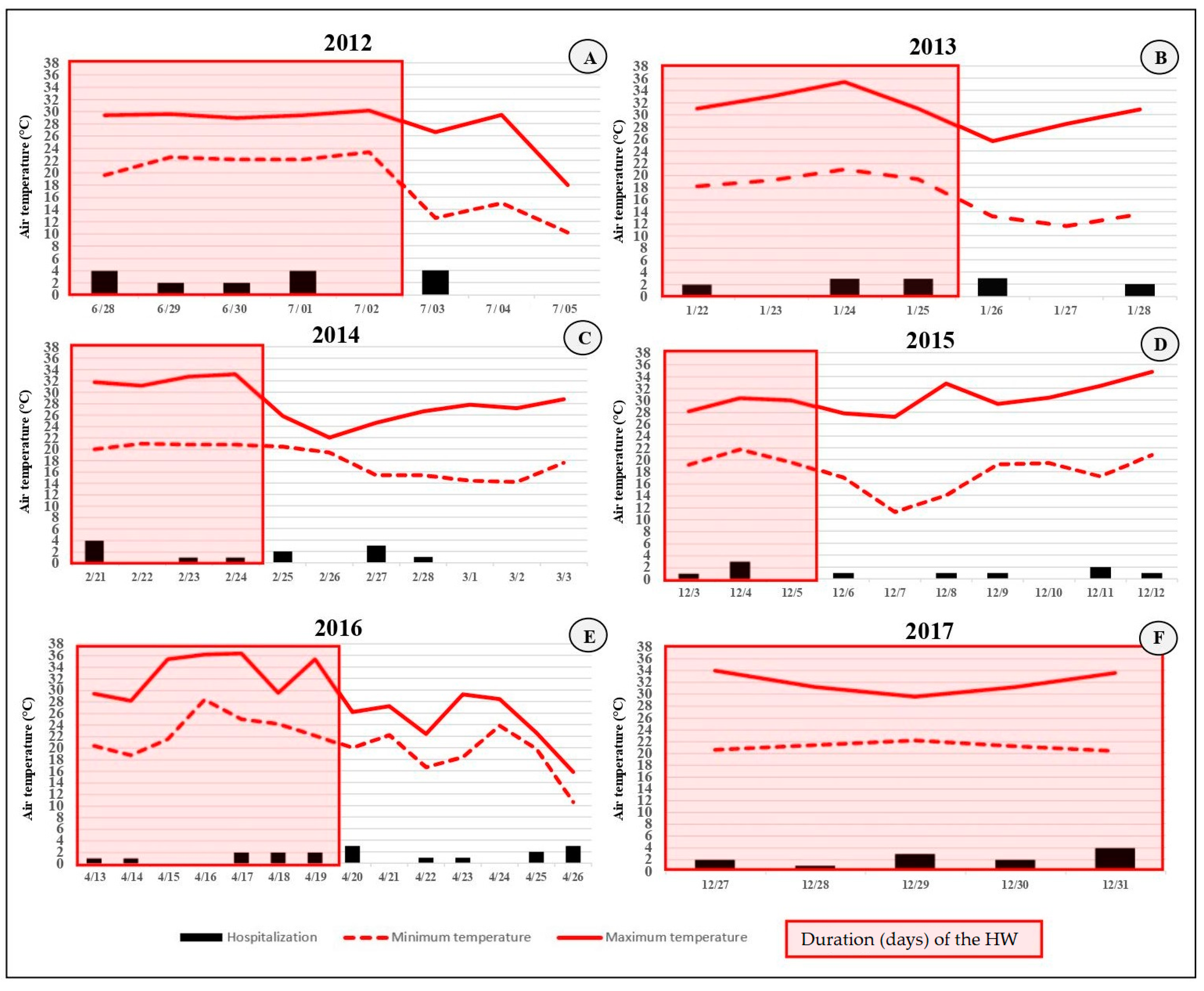
3.4. Hospitalizations during Representative Heat Waves
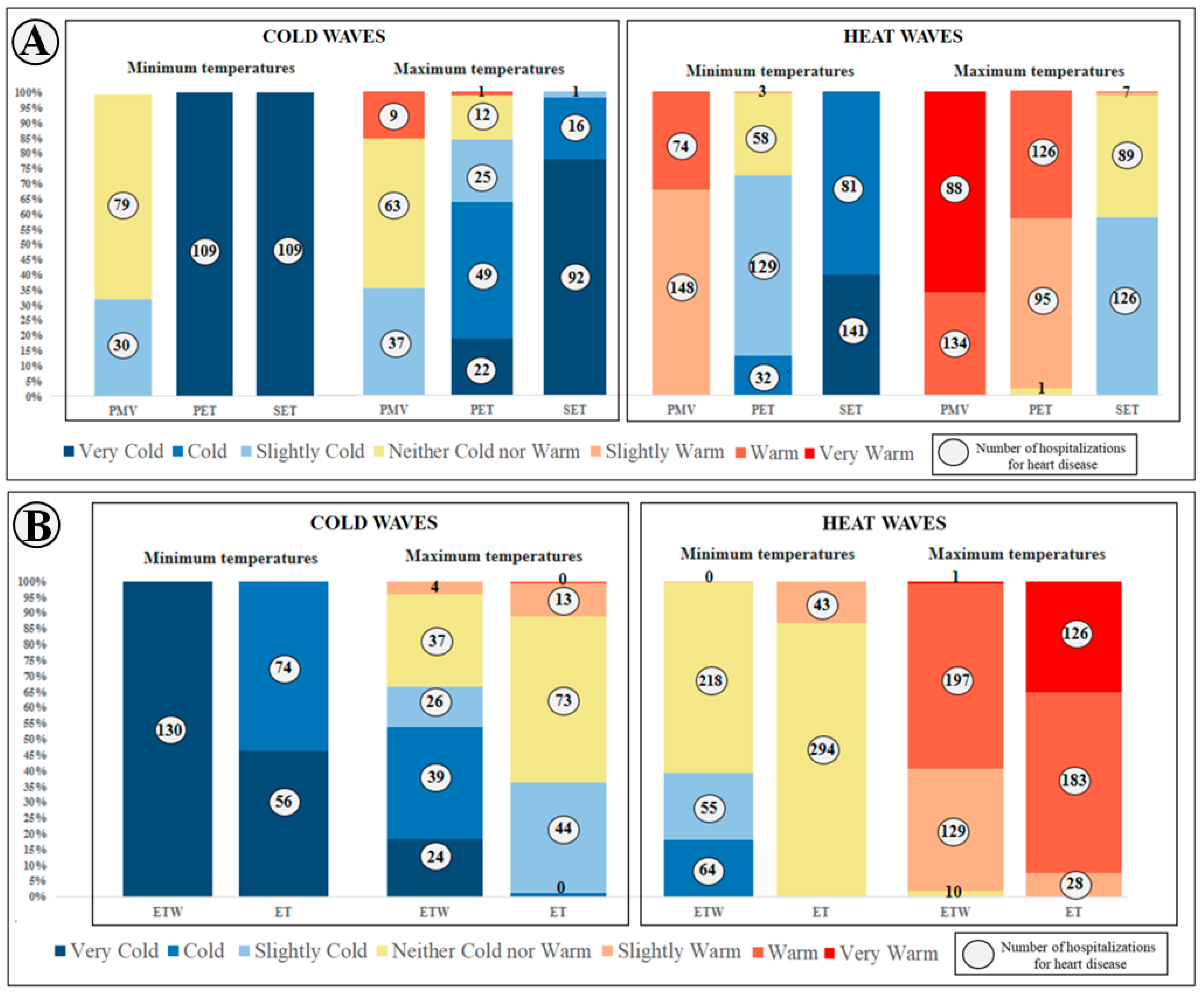
3.5. Hospitalizations and Human Thermal Comfort Indices during Cold and Heat Waves
3.6. Distributed Nonlinear Lag Models Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schlegel, I.; Muthers, S.; Mücke, H.G.; Matzarakis, A. Comparison of Respiratory and Ischemic Heart Mortalities and their Relationship to the Thermal Environment. Atmosphere 2020, 11, 826. [Google Scholar] [CrossRef]
- Mendis, S.; Puska, P.; Norrving, B. Global Atlas on Cardiovascular Disease Prevention and Control; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Marques, L.P.; Confortin, S.C. Doenças do aparelho circulatório: Principal causa de internações de idosos no Brasil entre 2003 e 2012. Rev. Bras. Ciênc. Saúde 2015, 19, 83–90. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Ornato, J.P.; Peberdy, M.A.; Chandra, N.C.; Bush, D.E. Seasonal pattern of acute myocardial infarction in the National Registry of Myocardial Infarction. J. Am. Coll. Cardiol. 1996, 28, 1684–1688. [Google Scholar] [CrossRef]
- Manfredini, R.; Manfredini, F.; Boari, B.; Bergami, E.; Mari, E.; Gamberini, S.; Gallerani, M. Seasonal and weekly patterns of hospital admissions for nonfatal and fatal myocardial infarction. Am. J. Emerg. Med. 2009, 27, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Abrignani, M.G.; Corrao, S.; Biondo, G.B.; Renda, N.; Braschi, A.; Novo, G. Influence of climatic variables on acute myocardial infarction hospital admissions. Int. J. Cardiol. 2009, 137, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Conlon, K.C.; Rajkovich, N.B.; White-Newsome, J.L.; Larsen, L.; O’Neill, M.S. Preventing cold-related morbidity and mortality in a changing climate. Maturitas 2011, 69, 197–202. [Google Scholar] [CrossRef]
- Urban, A.; Kyselý, J. Comparison of UTCI with other thermal indices in the assessment of heat and cold effects on cardiovascular mortality in the Czech Republic. Int. J. Environ. Res. Public Health 2014, 11, 952–967. [Google Scholar] [CrossRef] [PubMed]
- Gronlund, C.J.; Sullivan, K.P.; Kefelegn, Y.; Cameron, L.; O’Neill, M.S. Climate change and temperature extremes: A review of heat-and cold-related morbidity and mortality concerns of municipalities. Maturitas 2018, 14, 54–59. [Google Scholar] [CrossRef]
- Santurtún, A.; Almendra, R.; Fdez-Arroyabe, P.; Sanchez-Lorenzo, A.; Royé, D.; Zarrabeitia, M.T.; Santana, P. Predictive value of three thermal comfort indices in low temperatures on cardiovascular morbidity in the Iberian peninsula. Sci. Total Environ. 2020, 729, 138969. [Google Scholar] [CrossRef]
- Fares, A. Winter cardiovascular diseases phenomenon. N. Am. J. Med. Sci. 2013, 5, 266. [Google Scholar] [CrossRef]
- Group, T.E. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet 1997, 349, 1341–1346. [Google Scholar]
- Barnett, A.G.; Dobson, A.J.; McElduff, P.; Salomaa, V.; Kuulasmaa, K.; Sans, S. Cold periods and coronary events: An analysis of populations worldwide. J. Epidemiol. Community Health 2005, 59, 551–557. [Google Scholar] [CrossRef]
- Fischer, T.; Lundbye-Christensen, S.; Johnsen, S.P.; Schønheyder, H.C.; Sørensen, H.T. Secular trends and seasonality in first-time hospitalization for acute myocardial infarction—A Danish population-based study. Int. J. Cardiol. 2004, 97, 425–431. [Google Scholar] [CrossRef]
- Achebak, H.; Devolder, D.; Ingole, V.; Ballester, J. Reversal of the seasonality of temperature-attributable mortality from respiratory diseases in Spain. Nat. Commun. 2020, 11, 2457. [Google Scholar] [CrossRef]
- Pimentel, M.; Grüdtner, L.; Zimerman, L.I. Seasonal variation of ventricular tachycardia registered in 24-hour Holter monitoring. Arq. Bras. Cardiol. 2006, 87, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Jorge, J.E.L.; Cagy, M.; Mesquita, E.T.; Da Costa, T.L.; Moscavitch, S.D.; Rosa, M.L.G. Seasonal variation in hospitalizations due to heart failure in Niterói city, Southeastern Brazil. Rev. Saude Publica 2009, 43, 555–557. [Google Scholar] [CrossRef]
- Godoy, H.L.; Silveira, J.A.; Segalla, E.; Almeida, D.R. Hospitalization and mortality rates for heart failure in public hospitals in São Paulo. Arq. Bras. Cardiol. 2011, 97, 402–407. [Google Scholar] [CrossRef]
- Ikefuti, P.V.; Barrozo, L.V.; Braga, A.L. Mean air temperature as a risk factor for stroke mortality in São Paulo, Brazil. Int. J. Biometeorol. 2018, 62, 1535–1542. [Google Scholar] [CrossRef] [PubMed]
- Kovats, R.S.; Kristie, L.E. Heatwaves and public health in Europe. Eur. J. Public Health 2006, 16, 592–599. [Google Scholar] [CrossRef]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health 2009, 8, 40. [Google Scholar] [CrossRef]
- Shevchenko, O.; Lee, H.; Snizhko, S.; Mayer, H. Long-term analysis of heat waves in Ukraine. Int. J. Climatol. 2014, 34, 1642–1650. [Google Scholar] [CrossRef]
- Anthes, R.A.; Panofsky, H.A.; Cahir, J.J.; Rango, A. The Atmosphere; Charles, E., Ed.; Merrill Publishing Company: Columbus, OH, USA, 1975. [Google Scholar]
- Kim, Y.M.; Kim, S.; Cheong, H.K.; Kim, E.H. Comparison of temperature indices for the impact assessment of heat stress on heat-related mortality. Environ. Health Toxicol. 2011, 26, e2011009. [Google Scholar] [CrossRef]
- Royé, D.; Zarrabeitia, M.T.; Riancho, J.; Santurtún, A. A time series analysis of the relationship between apparent temperature, air pollutants and ischemic stroke in Madrid, Spain. Environ. Res. 2019, 173, 349–358. [Google Scholar] [CrossRef]
- Machado, F. P Contribuição ao Estudo do Clima do Rio Grande do Sul; Serviço Geográfico do IBGE: Rio de Janeiro, Brazil, 1950. [Google Scholar]
- Sartori, M.D.G.B. A dinâmica do clima do Rio Grande do Sul: Indução empírica e conhecimento científico. Terra Livre 2003, 20, 27–50. [Google Scholar]
- Bitencourt, D.P.; Fuentes, M.V.; Franke, A.E.; Silveira, R.B.; Alves, M.P. The climatology of cold and heat waves in Brazil from 1961 to 2016. Int. J. Climatol. 2020, 40, 2464–2478. [Google Scholar] [CrossRef]
- Folkerts, M.A.; Bröde, P.; Botzen, W.J.; Martinius, M.L.; Gerrett, N.; Harmsen, C.N.; Daanen, H.A. Long term adaptation to heat stress: Shifts in the minimum mortality temperature in the Netherlands. Front. Physiol. 2020, 11, 225. [Google Scholar] [CrossRef] [PubMed]
- ASHRAE. American Society for Heating Ventilating and Air-Conditioning Engineers; ASHRAE Fundamentals Handbook: New York, NY, USA, 2017. [Google Scholar]
- Chen, L.; Ng, E. Outdoor thermal comfort and outdoor activities: A review of research in the past decade. Cities 2012, 29, 118–125. [Google Scholar] [CrossRef]
- Fong, C.S.; Aghamohammadi, N.; Ramakreshnan, L.; Sulaiman, N. Holistic recommendations for future outdoor thermal comfort assessment in tropical Southeast Asia: A critical appraisal. Sustain. Cities Soc. 2019, 46, 101428. [Google Scholar] [CrossRef]
- Golden, J.S.; Hartz, D.; Brazel, A.; Luber, G.; Phelan, P. A biometeorology study of climate and heat-related morbidity in Phoenix from 2001 to 2006. Int. J. Biometeorol. 2008, 52, 471–480. [Google Scholar] [CrossRef]
- Aboubakri, O.; Khanjani, N.; Jahani, Y.; Bakhtiari, B. Thermal comfort and mortality in a dry region of Iran, Kerman; a 12-year time series analysis. Theor. Appl. Climatol. 2020, 139, 403–413. [Google Scholar] [CrossRef]
- Anderson, B.G.; Bell, M.L. Weather-Related Mortality: How Heat, Cold, and Heat Waves Affect Mortality in the United States. Epidemiology 2009, 20, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Matzarakis, A.; Muthers, S.; Graw, K. Thermische Belastung von Bewohnern in Städten bei Hitzewellen am Beispiel von Freiburg (Breisgau). Bundesgesundheitsblatt-Gesundh.-Gesundh. 2020, 63, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Brychkov, D.; Garb, Y.; Pearlmutter, D. The influence of climatocultural background on outdoor thermal perception. Int. J. Biometeorol. 2018, 62, 1873–1886. [Google Scholar] [CrossRef] [PubMed]
- Gosling, S.; Bryce, E.; Dixon, P.G.; Gabriel, K.A.; Gosling, E.; Hanes, J.; Hondula, D.L.; Liang, P.; Bustos, M.S.; Nascimento, S.; et al. A glossary for biometeorology. Int. J. Biometeorol. 2014, 58, 277–308. [Google Scholar] [CrossRef]
- Givoni, B.; Noguchi, M.; Saaroni, H.; Pochter, O.; Yaacov, Y.; Feller, N.; Becker, S. Outdoor comfort research issues. Energy Build. 2003, 35, 77–86. [Google Scholar] [CrossRef]
- Nikolopoulou, M.; Lykoudis, S. Thermal comfort in outdoor urban spaces: Analysis across different European countries. Build. Environ. 2006, 41, 1455–1470. [Google Scholar] [CrossRef]
- Lim, Y.-H.; Kim, H.; Hong, Y.-C. Variation in mortality of ischemic and hemorrhagic strokes in relation to high temperature. Int. J. Biometeorol. 2013, 57, 145–153. [Google Scholar] [CrossRef]
- Ormandy, D.; Ezratty, V. Health and thermal comfort: From WHO guidance to housing strategies. Energy Policy 2012, 49, 116–121. [Google Scholar] [CrossRef]
- Martinelli, L.; Matzarakis, A. Andreas. Influence of height/width proportions on the thermal comfort of courtyard typology for Italian climate zones. Sustain. Cities Soc. 2017, 29, 97–106. [Google Scholar] [CrossRef]
- Jowkar, M.; De Dear, R.; Brusey, J. Influence of long-term thermal history on thermal comfort and preference. Energy Build. 2020, 210, 109685. [Google Scholar] [CrossRef]
- Alvares, C.A.; Stape, J.L.; Sentelhas, P.C.; Gonçalves, J.D.M.; Sparovek, G. Köppen’s climate classification map for Brazil. Meteorol. Z. 2013, 22, 711–728. [Google Scholar] [CrossRef]
- Shooshtarian, S.; Rajagopalan, P.; Sagoo, A. comprehensive review of thermal adaptive strategies in outdoor spaces. Sustain. Cities Soc. 2018, 41, 647–665. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Portaria nº 123, de 28 de Fevereiro de 2005. Atualiza as Normas Para Organização das Redes de Atenção em Alta Complexidade Cardiovascular, Assim Como Inclui Procedimentos de Órteses, Próteses e Materiais Referentes À Assistência Cardiovascular na Tabela do SIH/SUS. Brasília, DF. 2005. Available online: http://adcon.rn.gov.br/ACERVO/Suvisa/doc/DOC000000000024879.PDF (accessed on 1 October 2021).
- Köppen, W. Climatologia; Fondo de Cultura Económica: México City, Mexico, 1931; Volume 2. [Google Scholar]
- Sartori, M.G.B.O. Vento Norte, 1st ed.; DR Publicidade: Santa Maria, RS, Brazil, 2016; 256p. [Google Scholar]
- Rossato, P.S.; Sartori, M.G.B.; Missio, L.R. As ondas de calor na região central do RS entre os meses de maio a outubro. In Simpósio Brasileiro de Geografia Física Aplicada; SBGFA: São Paulo, Brazil, 2003; Volume 10. [Google Scholar]
- Gobo, J.P.A.; Galvani, E.; Wollmann, C.A.; Gonçalves, F.L.T. Calibração das Faixas de Conforto Térmico Humano para Espaços Abertos em Clima Subtropical. Rev. Do Dep. Geogr. 2018, 1, 129–139. [Google Scholar] [CrossRef]
- Costa, E.R.; Sartori, M.G.B.; Almeida, A.P. Gênese e ocorrência de ondas de frio na região de Santa Maria-RS: Análise do período de 1968 a 2007. Rev. Geogr. Ensino Pesqui. St. Maria 2008, 12, 811–820. [Google Scholar]
- Brasil. Ministério da Saúde. Secretaria de Assistência à Saúde. Departamento de Sistemas e Redes Assistenciais. In Padronização da Nomenclatura do Censo Hospitalar; Ministério da Saúde: Brasília, Brazil, 2002.
- Mayer, H.; Höppe, P. Thermal comfort of man in different urban environments. Theor. Appl. Climatol. 1987, 38, 43–49. [Google Scholar] [CrossRef]
- Höppe, P. The physiological equivalent temperature–a universal index for the biometeorological assessment of the thermal environment. Int. J. Biometeorol. 1999, 43, 71–75. [Google Scholar] [CrossRef]
- Gagge, A.P.; Stolwijk, J.A.; Nishi, Y. An effective temperature scale based on a simple model of human physiological regulatory response. Mem. Fac. Eng. Hokkaido Univ. 1972, 13, 21–36. [Google Scholar]
- Fanger, P.O. Thermal Comfort; McGraw-Hill Book Company: New York, NY, USA, 1970. [Google Scholar]
- Gobo, J.P.A.; Galvani, E.; Wollmann, C.A. Subjective Human Perception of Open Urban Spaces in the Brazilian Subtropical Climate: A First Approach. Climate 2018, 6, 24. [Google Scholar] [CrossRef]
- Suping, Z.; Guanglin, M.; Yanwen, W.; Ji, L. Study of the relationships between weather conditions and the marathon race, and of meteorotropic effects on distance runners. Int. J. Biometeorol. 1992, 36, 63–68. [Google Scholar] [CrossRef]
- Matzarakis, A. Climate Change: Temporal and spatial dimension of adaptation possibilities at regional and local scale. In Tourism and the Implications of Climate Change: Issues and Actions; Schott, C., Ed.; Emerald Group Publishing: Bingley, UK, 2010; Volume 3, pp. 237–259. [Google Scholar]
- Matzarakis, A.; Rutz, F.; Mayer, H. Modelling radiation fluxes in simple and complex environments—Application of the RayMan model. Int. J. Biometeorol. 2007, 51, 323–334. [Google Scholar] [CrossRef]
- Gasparrini, A. Statistical Methods in Studies on Temperature-Health Associations. Ph.D. Thesis, London School of Hygiene & Tropical Medicine, London, UK, 2011. [Google Scholar] [CrossRef]
- Gao, J.; Sun, Y.; Liu, Q.; Zhou, M.; Lu, Y.; Li, L. Impact of extreme high temperature on mortality and regional level definition of heat wave: A multi-city study in China. Sci. Total Environ. 2015, 505, 535–544. [Google Scholar] [CrossRef]
- Sherbakov, T.; Malig, B.; Guirguis, K.; Gershunov, A.; Basu, R. Ambient temperature and added heat wave effects on hospitalizations in California from 1999 to 2009. Environ. Res. 2018, 160, 83–90. [Google Scholar] [CrossRef]
- Fu, S.H.; Gasparrini, A.; Rodriguez, P.S.; Jha, P. Mortality attributable to hot and cold ambient temperatures in India: A nationally representative case-crossover study. PLoS Med. 2018, 15, e1002619. [Google Scholar] [CrossRef] [PubMed]
- Dang, T.N.; Honda, Y.; Van Do, D.; Pham, A.L.T.; Chu, C.; Huang, C.; Phung, D. Effects of extreme temperatures on mortality and hospitalization in Ho Chi Minh City, Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 432. [Google Scholar] [CrossRef]
- Aklilu, D.; Wang, T.; Amsalu, E.; Feng, W.; Li, Z.; Li, X.; Tao, L.; Luo, Y.; Guo, M.; Liu, X.; et al. Short-term effects of extreme temperatures on cause specific cardiovascular admissions in Beijing, China. Environ. Res. 2020, 186, 109455. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Hansen, A.; Varghese, B.; Liu, Z.; Tong, M.; Qiu, H.; Bi, P. Cause-specific mortality attributable to cold and hot ambient temperatures in Hong Kong: A time-series study, 2006–2016. Sustain. Cities Soc. 2020, 57, 102131. [Google Scholar] [CrossRef]
- Rothwell, P.M.; Wroe, S.J.; Slattery, J.; Warlow, C.P. On behalf of the Oxfordshire Community Stroke Project. Is stroke related to season or temperature. Lancet 1996, 347, 934–936. [Google Scholar] [CrossRef]
- Wang, X.Y.; Barnett, A.G.; Hu, W.; Tong, S. Temperature variation and emergency hospital admissions for stroke in Brisbane, Australia, 1996–2005. Int. J. Biometeorol. 2009, 53, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. USA 2012, 109, 6608–6613. [Google Scholar] [CrossRef]
- Abreu-Harbich, L.V.; Labaki, L.C.; Matzarakis, A. Thermal bioclimate in idealized urban street canyons in Campinas, Brazil. Theor. Appl. Climatol. 2014, 115, 333–340. [Google Scholar] [CrossRef]
- Neder, E.A.; de Araújo Moreira, F.; Dalla Fontana, M.; Torres, R.R.; Lapola, D.M.; da Penha Costa Vasconcellos, M.; Bedran-Martins, A.M.B.; Philippi, A., Jr.; Lemos, M.C.; Di Giulio, G.M. Urban adaptation index: Assessing cities readiness to deal with climate change. Clim. Chang. 2021, 166, 16. [Google Scholar] [CrossRef]
- Linares, C.; Díaz, J.; Negev, M.; Martínez, G.S.; Debono, R.; Paz, S. Impacts of climate change on the public health of the Mediterranean Basin population-current situation, projections, preparedness and adaptation. Environ. Res. 2020, 182, 109107. [Google Scholar] [CrossRef] [PubMed]
- World Meteorological Organization (WMO). Guide to the Global Observing System. 488; WMO: Geneva, Switzerland, 2010; Volume 172. [Google Scholar]


| Gobo et al., 2018 [59] | Categories | Gobo et al., 2018 [51] | |||
|---|---|---|---|---|---|
| PMV | PET | SET | ETW | ET | |
| <−3.6 | <5 | <6 | Cold | <7 | <4 |
| −3.6 to −2.3 | 5 to 11 | 6 to 12 | Cool | 7 to 14 | 4 to 8 |
| −2.3 to −1.0 | 11 to 16 | 12 to 17 | Slightly cool | 14 to 15 | 8 to 15 |
| −1.0 to 0.8 | 16 to 24 | 17 to 23 | Neither cold nor hot | 15 to 22 | 15 to 22 |
| 0.8 to 1.9 | 24 to 30 | 23 to 29 | Slightly warm | 22 to 38 | 22 to 23 |
| 1.9 to 3.5 | 30 to 39 | 29 to 33 | Warm | 38 to 46 | 23 to 26 |
| >3.5 | >39 | >33 | Very warm | >46 | >26 |
| Description | Total Days | No. Hospitalization | Hospitalizations/Day |
|---|---|---|---|
| Days without anomalies | 1575 | 1125 | 0.714 |
| Heat waves | 444 | 337 | 0.759 |
| Cold waves | 173 | 130 | 0.751 |
| Total | 2192 | 1592 | 0.726 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, I.T.; Wollmann, C.A.; Gobo, J.P.A.; Ikefuti, P.V.; Shooshtarian, S.; Matzarakis, A. Extreme Weather Conditions and Cardiovascular Hospitalizations in Southern Brazil. Sustainability 2021, 13, 12194. https://doi.org/10.3390/su132112194
Costa IT, Wollmann CA, Gobo JPA, Ikefuti PV, Shooshtarian S, Matzarakis A. Extreme Weather Conditions and Cardiovascular Hospitalizations in Southern Brazil. Sustainability. 2021; 13(21):12194. https://doi.org/10.3390/su132112194
Chicago/Turabian StyleCosta, Iago Turba, Cassio Arthur Wollmann, João Paulo Assis Gobo, Priscilla Venâncio Ikefuti, Salman Shooshtarian, and Andreas Matzarakis. 2021. "Extreme Weather Conditions and Cardiovascular Hospitalizations in Southern Brazil" Sustainability 13, no. 21: 12194. https://doi.org/10.3390/su132112194
APA StyleCosta, I. T., Wollmann, C. A., Gobo, J. P. A., Ikefuti, P. V., Shooshtarian, S., & Matzarakis, A. (2021). Extreme Weather Conditions and Cardiovascular Hospitalizations in Southern Brazil. Sustainability, 13(21), 12194. https://doi.org/10.3390/su132112194









