Sustainable Care in a Familialist Regime: Coping with Elderly Care in Slovenia
Abstract
1. Introduction
2. Coping Strategies: Related Literature
3. Materials and Methods
3.1. Design, Setting, and Sample
3.2. Procedures
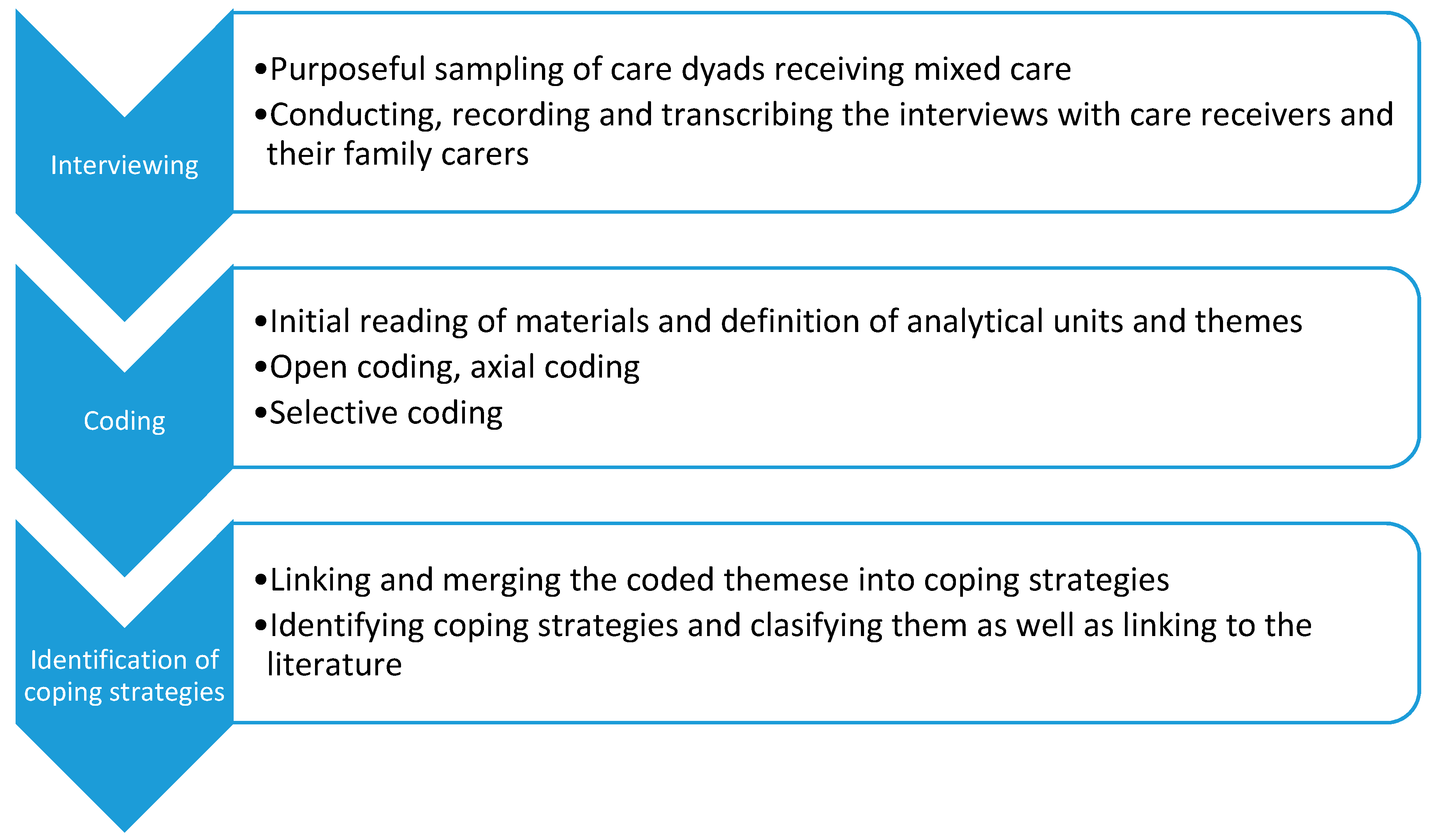
3.3. Data Analysis
4. Results
4.1. Coping Strategies of Family Carers in Slovenia
4.1.1. External Coping Strategies
This situation has lasted already a couple of years. And I started feeling tired. This is why I found help. A doctor gave me advice on using social home help, as I did not know this existed. And I called them up, where they organise this and they helped me. But there is not enough help, as much as one would need….(I55, CG, female)
I called the Centre for Social Home Help and they said ‘No way’ that they could come and help for an hour (…). And then we waited. This was at the end of summer and we waited until March of the next year.(I14, female)
Another thing that is very inconvenient is that they do not do the bandaging of the legs. At the start, they did that. But then it was said that it is too medical and they do not do that. This is most unpractical since you have to be present at the exact time they dress her, to bandage the legs. There is no solution here. You have to be at home.(I16, CG, female)
Only that the hours would change. Not at 7 am, but at 8 in the morning. Only this, nothing else.(I18, CR, female)
The difference is that on the weekends those carers come, who do not know exactly… This transition is not ok. Sometimes the new people come and grandma is very angry since they do not know how to handle her. And they come earlier and are in a hurry, as they have more users.(I5, CG, male)
Well, I have a large family and we have divided this a little. So, it isn’t just me. Not only one person. We are 5, 6 carers in the game, so it is all divided.(I59, CG, female)
Yes, the daughter lives in (city in another country). (…). And the son lives in (city in the country). But he is so busy, so that under no circumstances could he… well, if I need something yes. But to be a large help, then no.(LP1, CG)
We have to go separately, I went on a trip that I would have preferred to take together, if it were possible.(LP31, female)
It is like that, I have a good neighbour. She has sometimes looked over my father, when we had to go to the doctor. And another neighbour is here across, who I can call upon.(Lp4, CG)
When I lived in (a bigger city), I came every week. I had an apartment in a house. When my mother become immobile, I said they should come to leave on the ground floor and I would move in on the upper floor. But they didn’t want to hear about that. So I moved with my son here, to be available to them.(I28, CG)
In 2014, I moved here because I was too tired with that every day. You cannot have one woman and a house and an apartment… managing two households was too much. We decided that I should come here. I slept over a few nights. And we decided this would not be so bad. And so it came that I stayed here.(Intervju14, CG, female)
You see, we built this ramp so that we can go out with a wheelchair. We made a bathroom without a tub, only tiles on the floor. And we bought a wheel chair, for showering.(I 14, CG, female)
4.1.2. Internal Coping Strategies
Recently, I changed my schedule so that I work from 9 am to 1 pm and come home (….) I did this also before, but I worked more hours. Now I have cut my working hours and work from 9 to 1 pm.(I28, CG, female)
Well, I simply forgot a bit about my own life. Now, after 2 years, I wonder if that is really expected and demanded from me, that I neglect my personal life, my personal pleasures. Or that I put my children second. Because I first make sure that they (mother and father in law) are taken care of ….(Intrevju11, female)
What can I say? I am trapped. This is how it is, I cannot go anywhere… mostly at home.(LP18, CG, female)
To tell you honestly, we haven’t been on vacation for 5 years. And if we go somewhere, we need to find a replacement. For example, the mother of my daughter in law died in February and we had to find someone.(LP29, CG, male)
Instead of going for a walk in the evening, I came over to them. I have this in me, I know that dad would take care of…, but I still come and check the medicines, sometimes they are already in bed, I just say hi, sometimes we put pyjamas on and take care of things.(LP11, CG, female)
Everything is upside down. Not bad, you know. If you have people around you and you get what you need, it is fine. Best to say thank you and thank god it is like this.(I12, CR, female)
Well, you need to just accept this change… I cannot say it was easy. But it is like this, life goes as it goes. And you handle every day as it comes. This is not some high philosophy.(LP22, CG)
You have to adjust your way of life. Basically, you have to give up everything.(LP31, CG, female)
Sometimes, I cannot find the strength for everything. What bothers me is guilt that I do not do enough. For mum, for my husband, or for the kids. I am always haunted by guilt.(I55, CG, female)
I sometimes feel I would need professional help, to be educated on how to deal with older people, if they fall, if they vomit… in that sense. How to react….(I30, CG, female)
24 h a day. 24 h a day for me. It is boring, to be like this 24 h a day. I do nothing.(I3, CR, male)
Maybe if someone would come and maybe talk, maybe 1 h maximum. Or play a game xxx, so that she gets distracted.(Lp2, CG)
If it were possible… I recently saw on television something on dementia, on how we should work on with people more. Not only this basic, but for example, with music. So that one would work with the person, as if they are living in the time when they remember everything. And play that music.(I56, CG, female)
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Saraceno, C. Varieties of familialism: Comparing four southern European and East Asian welfare regimes. J. Eur. Soc. Policy 2016, 26, 314–326. [Google Scholar] [CrossRef]
- Osterle, A. Long-term Care in Central and South-Eastern Europe: Challenges and Perspectives in Addressing a New” Social Risk. Soc. Policy Adm. 2010, 44, 461–480. [Google Scholar] [CrossRef]
- Lowenstein, A. Caregiving and Elder Abuse and Neglect—Developing a New Conceptual Perspective. Ageing Int. 2010, 35, 215–227. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2017: OECD Indicators; OECD Publishing: Paris, France, 2017; Available online: https://doi.org/10.1787/health_glance-2017-en (accessed on 15 July 2020).
- Saraceno, C.; Keck, W. Can we identify intergenerational policy regimes in Europe? Eur. Soc. 2010, 12, 675–696. [Google Scholar] [CrossRef]
- Esping-Andersen, G. Social Foundations of Postindustrial Economies; Oxford University Press: Oxford, UK, 1999. [Google Scholar]
- Bettio, F.; Platenga, J. Comparing Care Regimes in Europe. Fem. Econ. 2004, 10, 85–113. [Google Scholar] [CrossRef]
- Leitner, S. Varieties of familialism. Eur. Soc. 2003, 5, 353–375. [Google Scholar] [CrossRef]
- Hlebec, V.; Srakar, A.; Majcen, B. Care for the elderly in Slovenia: A combination of informal and formal care. Rev. Za Soc. Polit. 2016, 23, 159–179. [Google Scholar] [CrossRef]
- Hlebec, V.; Rakar, T. Ageing policies in Slovenia: Before and after austerity. In Selected Contemporary Challenges of Ageing Policy; Tomczyk, Ł., Ed.; Uniwersytet Pedagogiczny w Krakowie: Krakow, Poland, 2017; pp. 27–51. [Google Scholar]
- Filipovič Hrast, M.; Schoyen, M.; Rakar, T. A comparative analysis of people’s views on future policies for older people. Rev. Za Soc. Polit. 2019, 26, 153–169. [Google Scholar] [CrossRef]
- Kovač, N.; Orehek, Š.; Černič, M.; Nagode, M.; Kobal Tomc, B. Analiza Izvajanja Pomoči Na Domu V Letu 2018, Končno Poročilo; IRSSV: Ljubjana, Slovenia, 2019. [Google Scholar]
- De Roit, B.; Naldini, M. Should I Stay or Should I Go? Combining Work and Care for an Older Parent in Italy. South. Eur. Soc. Politics 2010, 15, 531–551. [Google Scholar] [CrossRef]
- Pickard, L.; King, D.; Brimblecombe, N.; Knapp, M. The effectiveness of paid services in supporting unpaid carers’ employment in England: Analysis using large-scale survey data and implications for policy. J. Soc. Policy 2015, 44, 567–590. [Google Scholar] [CrossRef] [PubMed]
- Da Roit, B.; Hoogenboom, M.; Weicht, B. The Gender Informal Care Gap. Eur. Soc. 2015, 17, 199–218. [Google Scholar] [CrossRef]
- Bonsang, E. Does informal care from children to their elderly parents substitute for formal care in Europe? J. Health Econ. 2009, 28, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Haberkern, K.; Schmid, T.; Szydlik, M. Gender differences in intergenerational care in European welfare states. Ageing Soc. 2015, 35, 298–320. [Google Scholar] [CrossRef]
- Schmid, T.; Brandt, M.; Haberkern, K. Gendered support to older parents: Do welfare states matter? Eur. J. Ageing 2012, 9, 39–50. [Google Scholar] [CrossRef]
- Eichler, M.; Pfau-Effinger, B. The ‘Consumer Principle’ in the Care of Elderly People: Free Choice and Actual Choice in the German Welfare State. Soc. Policy Adm. 2009, 43, 617–633. [Google Scholar] [CrossRef]
- Pavolini, E.; Ranci, C. Restructuring the welfare state: Reforms in long-term care in Western European countries. J. Eur. Soc. Policy 2008, 18, 246–259. [Google Scholar] [CrossRef]
- Deusdad, B.A.; Pace, C.; Anttonen, A. Facing the Challenges in the Development of Long-Term Care for Older People in Europe in the Context of an Economic Crisis. J. Soc. Serv. Res. 2016, 42, 144–150. [Google Scholar] [CrossRef]
- Rummery, K.; Fine, M. Care: A Critical Review of Theory, Policy and Practice. Soc. Policy Adm. 2012, 46, 321–343. [Google Scholar] [CrossRef]
- Shutes, I.; Chiatti, C. Migrant labour and the marketisation of care for older people: The employment of migrant care workers by families and service providers. J. Eur. Soc. Policy 2012, 22, 392–405. [Google Scholar] [CrossRef]
- Le Bihan, B. The redefinition of the familialist home care model in France: The complex formalization of care through cash payment. Health Soc. Care Community 2012, 20, 238–246. [Google Scholar] [CrossRef]
- Yeandle, S.; Kröger, T.; Cass, B. Voice and choice for users and carers? Developments in patterns of care for older people in Australia, England and Finland. J. Eur. Soc. Policy 2012, 22, 432–445. [Google Scholar] [CrossRef]
- Da Roit, B.; Le Bihan, B.; Österle, A. Longterm care policies in Italy, Austria and France: Variations in cash-for-care schemes. Soc. Policy Adm. 2007, 41, 653–671. [Google Scholar] [CrossRef]
- Verbakel, E. Informal caregiving and well-being in Europe: What can ease the negative consequences for caregivers? J. Eur. Soc. Policy 2014, 24, 424–441. [Google Scholar] [CrossRef]
- Lazarus, R.S. Psychological Stress and the Coping Process; McGraw-Hill: New York, NY, USA, 1966. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Apraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Schroder-Butterfill, E.; Marianti, R. A framework for understanding old-age vulnerabilities. Ageing Soc. 2006, 26, 9–35. [Google Scholar] [CrossRef]
- Gottlieb, B.H.; Wolfe, J. Coping with family caregiving to persons with dementia: A critical review. Aging Ment. Health 2002, 6, 325–342. [Google Scholar] [CrossRef]
- Monroe, P.; Tiller, V.R.; O’Neil, C.E.; Blalock, L.L. We make our ends meet good: Coping strategies of former welfare reliant women. J. Loss Trauma 2007, 12, 199–221. [Google Scholar] [CrossRef]
- Pratt, C.C.; Schmall, V.L.; Wright, S.; Cleland, M. Burden and coping strategies of caregivers to Alzheimer’s patients. Fam. Relat. Interdiscip. J. Appl. Fam. Stud. 1985, 34, 27–33. [Google Scholar] [CrossRef]
- Sun, F.; Kosberg, J.I.; Kaufman, A.V.; Leeper, J.D. Coping Strategies and Caregiving Outcomes among Rural Dementia Caregivers. J. Gerontol. Soc. Work 2010, 53, 547–567. [Google Scholar] [CrossRef]
- Carandang, R.R.; Asis, E.; Shibanuma, A.; Kiriya, J.; Murayama, H.; Jimba, M. Unmet Needs and Coping Mechanisms Among Community-Dwelling Senior Citizens in the Philippines: A Qualitative Study. Int. J. Environ. Res. Public Health 2019, 16, 3745. [Google Scholar] [CrossRef]
- Haley, W.E.; Levine, E.G.; Brown, S.L.; Bartolucci, A.A. Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychol. Aging 1987, 2, 323–330. [Google Scholar] [CrossRef]
- Sayegh, P.; Knight, B.G. The Effects of Familism and Cultural Justification on the Mental and Physical Health of Family Caregivers. J. Gerontol. Psychol. Sci. 2010, 66B, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Kneebone, I.; Martin, P. Coping and caregivers of people with dementia. Br. J. Health Psychol. 2003, 8, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, J.; Muers, J.; Patterson, T.G.; Marczak, M. Self-Compassion, Coping Strategies, and Caregiver Burden in Caregivers of People with Dementia. Clin. Gerontol. 2019, 42, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Knight, B.G.; Flynn Longmire, C.V. The role of familism values in stress and coping processes among African American and White dementia caregivers: Effects on mental and physical health. Health Psychol. 2007, 26, 564–576. [Google Scholar] [CrossRef]
- Lieberman, M.A.; Fisher, L. The effects of family conflict resolution and decision making on the provision of help for an elder with Alzheimer’s disease. Gerontologist 1999, 39, 159–166. [Google Scholar] [CrossRef]
- Kroger, T.; Puthenparambil, J.M.; Van Aerschot, L. Care poverty:unmet care needs in a Nordic Welfare State. Int. J. Care Caring 2019, 3, 485–500. [Google Scholar] [CrossRef]
- Lowenstein, A.; Katz, R. Living arrangements, family solidarity and life satisfaction of two generations of immigrants. Ageing Soc. 2005, 25, 1–19. [Google Scholar] [CrossRef]
- Eurofound. COVID-19: Policy Responses Across Europe; Publications Office of the European Union: Luxembourg, 2020. [Google Scholar]
- Boeije, H. Analysis in Qualitative Research; Sage: Los Angeles, CA, USA, 2010. [Google Scholar]
- Kavčič, M.; Filipovič Hrast, M.; Hlebec, V. Starejši ljudje in njihove strategije shajanja s tveganji za zdravje = Older people and their strategies for coping with health risks. Zdr. Varst. Slov. J. Public Health 2012, 51, 163–172. [Google Scholar]
- Iacovou, M.; Skew, A. Population and Social Conditions; Eurostat Statistics in Focus: Luxembourg, 2011. [Google Scholar]
- Hank, K. Proximity and Contacts between Older Parents and Their Children: A European Comparison. J. Marriage Fam. 2007, 69, 157–173. [Google Scholar] [CrossRef]
- Jacobs, T.M.; van Broese Groenou, M.I.; de Boer, A.H.; Deeg, D.J.H. Individual determinants of task division in older adults’ mixed care networks. Health Soc. Care Community 2014, 22, 57–66. [Google Scholar] [CrossRef]
- Thompson, E.H.; Futterman, A.M.; Gallagher-Thompson, D.; Rose, M.J.; Lovett, S.B. Social Support and Caregiving Burden in Family Caregivers of Frail Elders. J. Gerontol. 1993, 48, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.; Quesnel-Vallée, A. The Structural Burden of Caregiving: Shared Challenges in the United States and Canada. Gerontologist 2017, 57, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, V. Understanding stress in informal caregiving: Is burden a problem of the individual or of society? Res. Aging 1996, 18, 139–174. [Google Scholar] [CrossRef]
- Pinquart, M.; Sörensen, S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, 112–128. [Google Scholar] [CrossRef] [PubMed]
- Vlachantoni, A. Unmet need for social care among older people. Ageing Soc. 2019, 39, 657–684. [Google Scholar] [CrossRef]
- Srakar, A.; Filipovič Hrast, M.; Hlebec, V.; Majcen, B. Social exclusion, welfare regime and unmet long-term care need: Evidence from SHARE. In Ageing in Europe: Supporting Policies for an Inclusive Society; Börsch-Supan, A., Ed.; W. de Gruyter: Berlin, Germany; Boston, MA, USA, 2015. [Google Scholar] [CrossRef]
- Hlebec, V.; Filipovič Hrast, M. Ovrednotenje dostopa do socialne oskrbe na domu z vidika uporabnikov. Teor. Praksa Rev. Za Družbena Vprašanja 2015, 52, 48–66. [Google Scholar]
- Hlebec, V. Evaluation of access to long-term care services for old people ageing in place in Slovenia = Ovrednotenje dostopa do storitev dolgotrajne oskrbe ljudi, ki se starajo v domačem okolju v Sloveniji. Zdr. Varst. Slov. J. Public Health 2018, 57, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Glaser, K.; Stuchbury, R.; Price, D.; Di Gessa, G.; Ribe, E.; Tinker, A. Trends in the prevalence of grandparents living with grandchild (ren) in selected European countries and the United States. Eur. J. Ageing 2018, 15, 237–250. [Google Scholar] [CrossRef]
- Luciano, A.; Pascale, F.; Polverino, F.; Pooley, A. Measuring Age-Friendly Housing: A Framework. Sustainability 2020, 12, 848. [Google Scholar] [CrossRef]
- Filipovič Hrast, M. Prostorska determiniranost omrežij starejših in vloga sosedov v časovni perspektivi. Teor. Praksa: Rev. Za Družbena Vprašanja 2007, 44, 298–316. [Google Scholar]
- Henning, C.; Lieberg, M. Strong or weak ties? Neighborhood networks in a new perspective. Scand. Hous. Plan. Res. 1996, 13, 3–26. [Google Scholar] [CrossRef]
- Guest, A.M.; Wierzbicki, S.K. Social ties at the neighborhood level, Two decades of GSS evidence. Urban. Aff. Rev. 1999, 35, 92–111. [Google Scholar] [CrossRef]
- Barker, J.C. Neighbors, Friends and other non-kin caregivers of community-living dependent elders. J. Gerontol. 2002, 57b, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Kohli, M.; Karsten, H.; Kunemund, H. The social connectedness of older Europeans: Patterns, dynamics and contexts. J. Eur. Soc. Policy 2009, 19, 327–340. [Google Scholar] [CrossRef]
- Litwin, H. Social networks and well-being: A comparison of older people in Mediterranean and non-Mediterranean countries. J. Gerontol. 2009, Series B 65, 599–608. [Google Scholar] [CrossRef]
- European Commission. Confronting Demographic Change: A New Solidarity between the Generations, Green Paper; European Commission: Brussels, Belgium, 2005. [Google Scholar]
- Nagode, M.; Dolničar, V. Assistive technology for older people and its potential for intergenerational cooperation: Critical review of the present situation and identification of key constraints for wider uptake. Teor. Praksa: Rev. Za Družbena Vprašanja 2010, 47, 1278–1294. [Google Scholar]
- Kerbler, B. Older people and the innovative forms of living and care. Antropol. Časopis Cent. Za Etnološka I Antropološka Istraživanja Filoz. Fak. Univ. U Beogr. 2013, 13, 73–87. [Google Scholar]
- Tingvold, L.; Fagertun, A. Between Privileged and Oppressed? Immigrant Labor Trajectories in Norwegian Long-Term Care. Sustainability 2020, 12, 4777. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
| Government-Supported/-Addressed Strategy | Active/Passive Strategy | |
|---|---|---|
| External coping strategies | ||
| using formal care services | yes | active |
| use of the extended family network | no | active |
| use of a wider social network | no | active |
| cohabitation strategy | no | active |
| home adjustments | no | active |
| Internal coping strategies | ||
| work-related adjustments | partly | active |
| abandoning leisure activities, routines | no | passive |
| abandoning vacations | no | passive |
| keeping and establishing new routines | no | active |
| accepting and finding satisfaction in care | partly | active |
| worries and overburdening linked to care | no | active |
| some needs remain unmet | no | passive |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hrast, M.F.; Hlebec, V.; Rakar, T. Sustainable Care in a Familialist Regime: Coping with Elderly Care in Slovenia. Sustainability 2020, 12, 8498. https://doi.org/10.3390/su12208498
Hrast MF, Hlebec V, Rakar T. Sustainable Care in a Familialist Regime: Coping with Elderly Care in Slovenia. Sustainability. 2020; 12(20):8498. https://doi.org/10.3390/su12208498
Chicago/Turabian StyleHrast, Maša Filipovič, Valentina Hlebec, and Tatjana Rakar. 2020. "Sustainable Care in a Familialist Regime: Coping with Elderly Care in Slovenia" Sustainability 12, no. 20: 8498. https://doi.org/10.3390/su12208498
APA StyleHrast, M. F., Hlebec, V., & Rakar, T. (2020). Sustainable Care in a Familialist Regime: Coping with Elderly Care in Slovenia. Sustainability, 12(20), 8498. https://doi.org/10.3390/su12208498






