Protective Effect of Ethanolic Extract of Djulis Hull on Indomethacin-Induced Gastric Injury
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemical Reagents
2.2. Material Preparation
2.3. Animals and Treatment
2.4. Evaluation of Ulcer Area and Protective Index
2.5. Histopathological Assessment
2.6. Gastric GSH Determination
2.7. Determination of Gastric SOD and CAT Activities
2.8. Analysis of Gastric Protein Expression
2.9. Statistical Analysis
3. Results
3.1. Effects of EEDH Pretreatment on IND-Induced Gastric Mucosal Damage in Mice
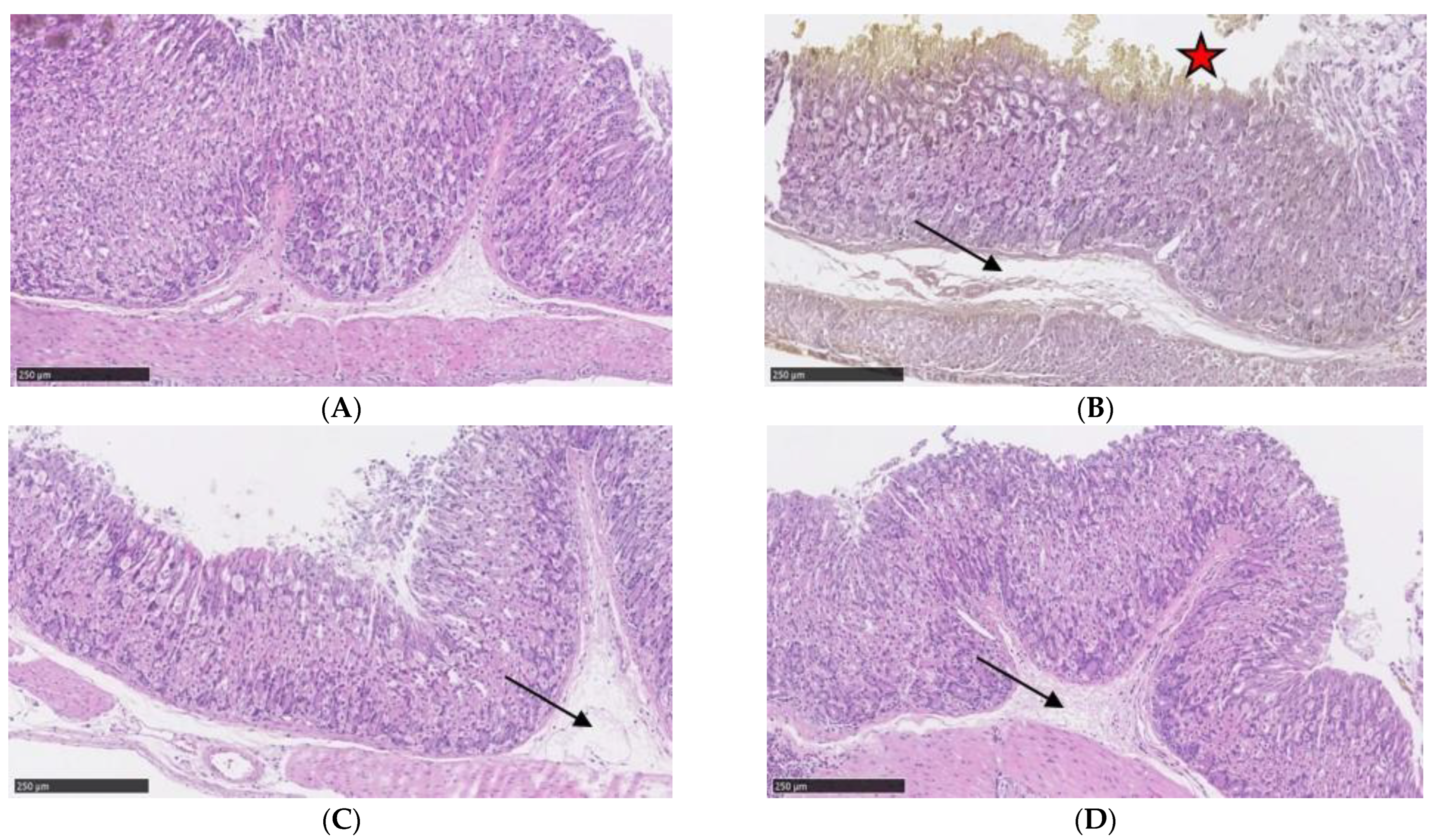
3.2. Effects of EEDH Pretreatment on IND-Induced Changes in Gastric Mucosal Histopathology
3.3. Effects of EEDH on Gastric Levels of GSH and Activities of SOD and CAT in Mice
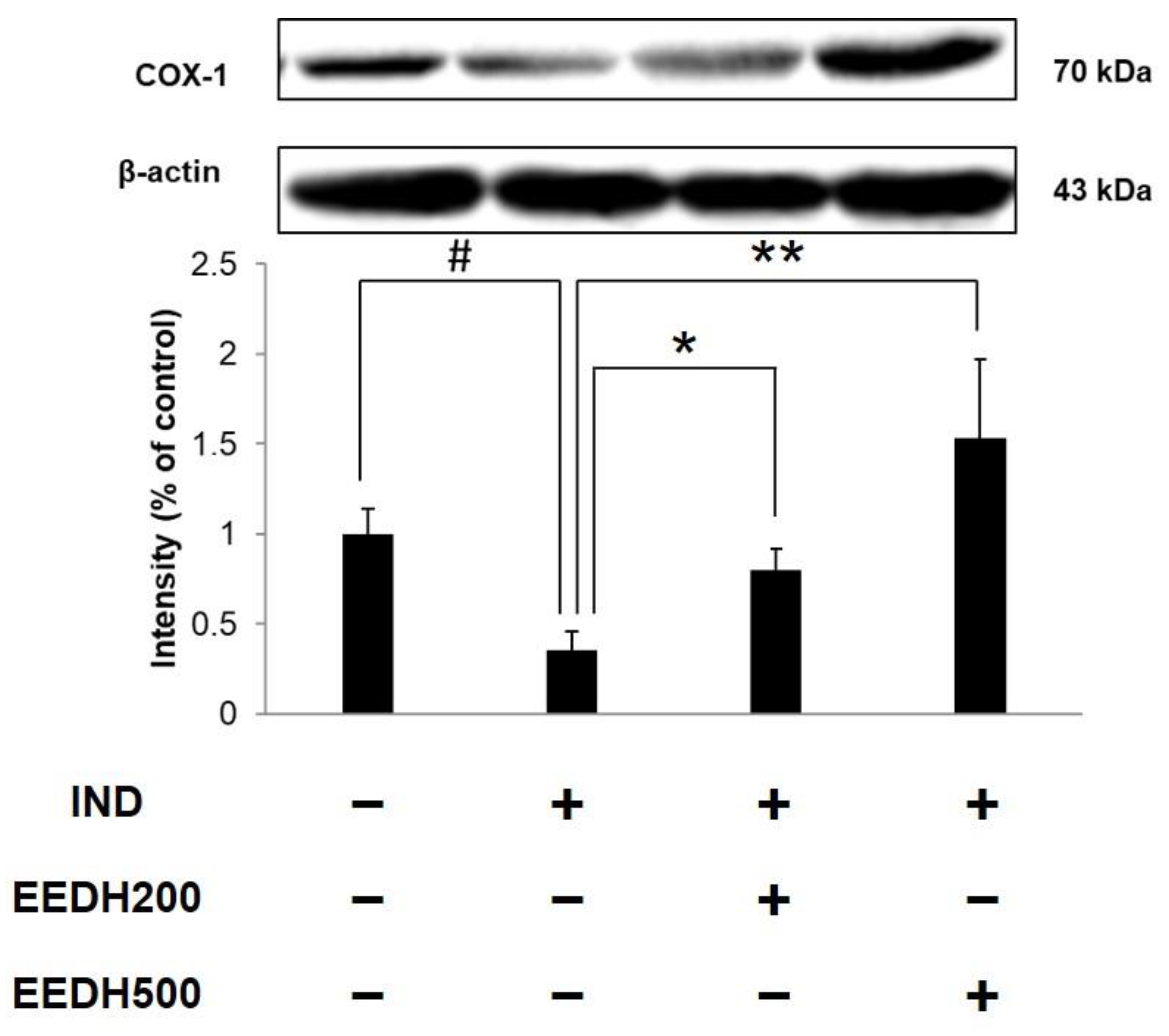
3.4. Effects of EEDH on Gastric COX-1 Protein Expression in Mice
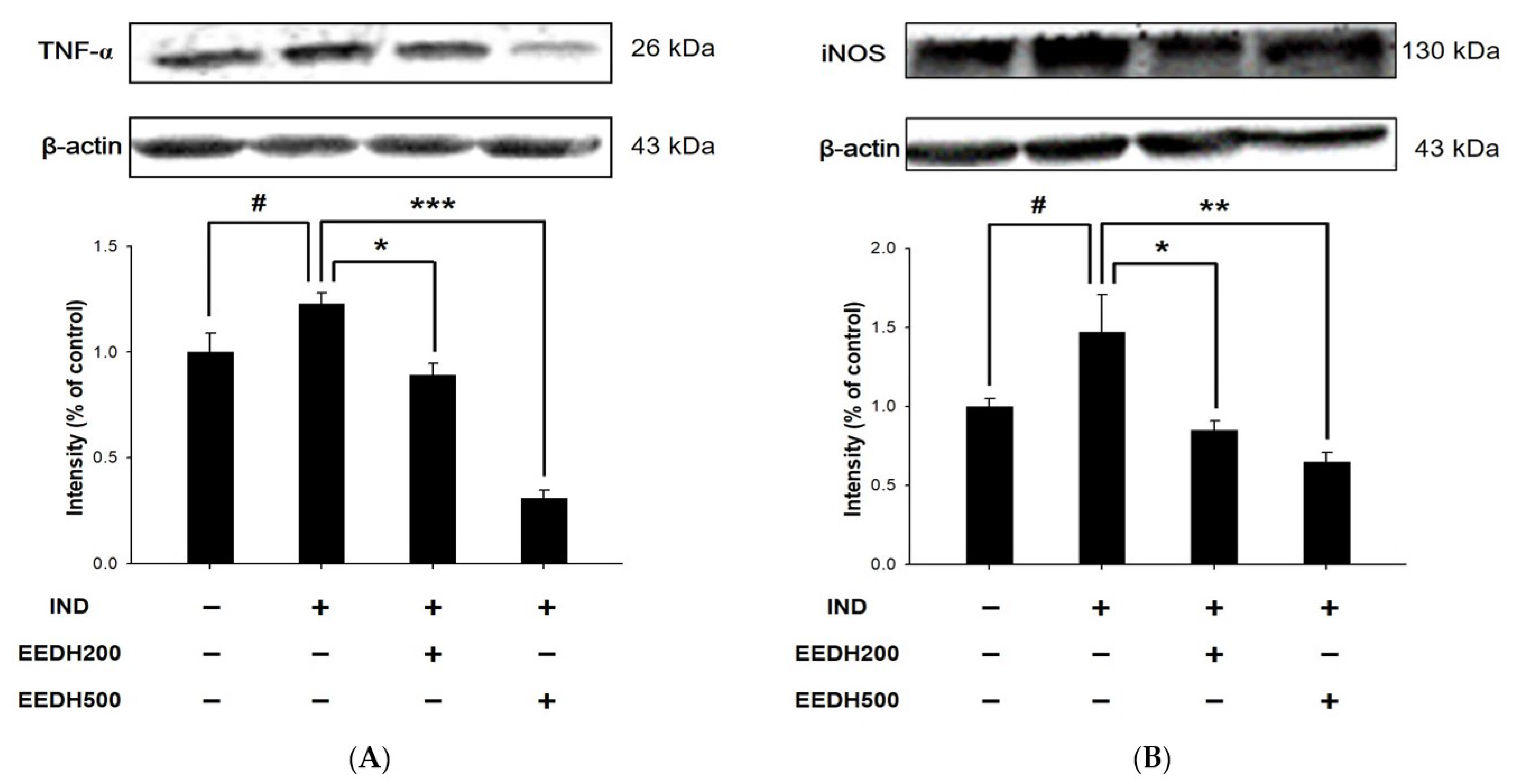
3.5. Effects of EEDH on Gastric Expression of TNF-α and iNOS Proteins in Mice
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hafez, A.A.; Tavassoli, E.; Hasanzadeh, A.; Reisi, M.; Javadzade, S.H.; Imanzad, M. Quality of life in peptic ulcer patients referring to Al-Zahra hospital of Isfahan, Iran. Gastroenterol. Hepatol. Bed Bench 2013, 6, S87–S92. [Google Scholar] [PubMed]
- Wasman, S.; Mahmood, A.A.; Salehhuddin, H.; Zahra, A.A.; Salmah, I. Cytoprotective activities of Polygonum minus aqueous leaf extract on ethanol-induced gastric ulcer in rats. J. Med. Plants Res. 2010, 4, 2658–2665. [Google Scholar]
- Lu, S.Y.; Guo, S.; Chai, S.B.; Yang, J.Q.; Yue, Y.; Li, H.; Sun, P.M.; Zhang, T.; Sun, H.W.; Zhou, J.L.; et al. Autophagy in gastric mucosa: The dual role and potential therapeutic target. Biomed. Res. Int. 2021, 2021, 2648065. [Google Scholar] [CrossRef] [PubMed]
- Jang, T.J.; Kim, J.R. Proliferation and apoptosis in gastric antral epithelial cells of patients infected with Helicobacter pylori. J. Gastroenterol. 2000, 35, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Shareef, S.H.; Al-Medhtiy, M.H.; Ibrahim, I.A.A.; Alzahrani, A.R.; Jabbar, A.A.; Galali, Y.; Agha, N.F.S.; Aziz, P.Y.; Thabit, M.A.; Agha, D.N.F.; et al. Gastroprophylactic effects of p-cymene in ethanol-induced gastric ulcer in rats. Processes 2022, 10, 1314. [Google Scholar] [CrossRef]
- Rawla, P.; Barsouk, A. Epidemiology of gastric cancer: Global trends, risk factors and prevention. Prz. Gastroenterol. 2019, 14, 26–38. [Google Scholar] [CrossRef]
- Maddirevula, S.; Abanemai, M.; Alkuraya, F.S. Human knockouts of PLA2G4A phenocopy NSAID-induced gastrointestinal and renal toxicity. Gut 2016, 65, 1575–1577. [Google Scholar] [CrossRef]
- Wolfe, M.M.; Lichtenstein, D.R.; Singh, G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N. Engl. J. Med. 1999, 340, 1888–1899. [Google Scholar] [CrossRef]
- Wong, R.S.Y. Role of Nonsteroidal anti-inflammatory drugs (NSAIDs) in cancer prevention and cancer promotion. Adv. Pharmacol. Sci. 2019, 2019, 3418975. [Google Scholar] [CrossRef]
- Atchison, J.W.; Herndon, C.M.; Rusie, E. NSAIDs for musculoskeletal pain management:current perspectives and novel strategies to improve safety. J. Manag. Care Pharm. 2013, 19, S3–S19. [Google Scholar]
- Griffin, M.R.; Scheiman, J.M. Prospects for changing the burden of nonsteroidal anti-inflammatory drug toxicity. Am. J. Med. 2001, 110, 33S–37S. [Google Scholar] [CrossRef] [PubMed]
- Andrews, F.J.; Malcontenti-Wilson, C.; O’Brien, P.E. Effect of nonsteroidal anti-inflammatory drugs on LFA-1 and ICAM-1 expression in gastric mucosa. Am. J. Physiol. 1994, 266, G657–G664. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, T.; Naito, Y. The role of neutrophils and inflammation in gastric mucosal injury. Free. Radic. Res. 2000, 33, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Hussain, T.; Tan, B.; Yin, Y.; Blachier, F.; Tossou, M.C.; Rahu, N. Oxidative stress and inflammation: What polyphenols can do for us? Oxid. Med. Cell. Longev. 2016, 2016, 7432797. [Google Scholar] [CrossRef] [PubMed]
- Nandi, J.; Saud, B.; Zinkievich, J.M.; Yang, Z.J.; Levine, R.A. TNF-α modulates iNOS expression in an experimental rat model of indomethacin-induced jejunoileitis. Mol. Cell. Biochem. 2010, 336, 17–24. [Google Scholar] [CrossRef]
- Küçükler, S.; Kandemir, F.M.; Yıldırım, S. Protective effect of chrysin on indomethacin induced gastric ulcer in rats: Role of multi-pathway regulation. Biotech. Histochem. 2022, 97, 490–503. [Google Scholar] [CrossRef]
- Chyau, C.C.; Chu, C.C.; Chen, S.Y.; Duh, P.D. The inhibitory effects of djulis (Chenopodium formosanum) and its bioactive compounds on adipogenesis in 3T3-L1 adipocytes. Molecules 2018, 23, 1780. [Google Scholar] [CrossRef]
- Hsu, B.Y.; Pan, S.Y.; Wu, L.Y.; Ho, C.T.; Hwang, L.S. Hypoglycemic activity of Chenopodium formosanum Koidz. components using a glucose uptake assay with 3T3-L1 adipocytes. Food Biosci. 2018, 24, 9–16. [Google Scholar] [CrossRef]
- Lee, C.W.; Chen, H.J.; Xie, G.R.; Shih, C.K. Djulis (Chenopodium formosanum) prevents colon carcinogenesis via regulating antioxidative and apoptotic pathways in rats. Nutrients 2019, 11, 2168. [Google Scholar] [CrossRef]
- Chen, S.Y.; Chu, C.C.; Chyau, C.C.; Yang, J.W.; Duh, P.D. Djulis (Chenopodium formosanum) and its bioactive compounds affect vasodilation, angiotensin converting enzyme activity, and hypertension. Food Biosci. 2019, 32, 100469. [Google Scholar] [CrossRef]
- Chu, C.C.; Chen, S.Y.; Chyau, C.C.; Wang, S.C.; Chu, H.L.; Duh, P.D. Djulis (Chenopodium formosanum) and its bioactive compounds protect human lung epithelial A549 cells from oxidative injury induced by particulate matter via Nrf2 signaling pathway. Molecules 2021, 27, 253. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.Y.; Chu, Y.L.; Sridhar, K.; Tsai, P.J. Analysis and determination of phytosterols and triterpenes in different inbred lines of djulis (Chenopodium formosanum Koidz.) hull: A potential source of novel bioactive ingredients. Food Chem. 2019, 297, 124948. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.Y.; Sridhar, K.; Tsai, P.J. Anti-glycation and inhibition of starch hydrolyzing enzymes by enzymatically hydrolysed djulis (Chenopodium formosanum Koidz.) hull, leaf and seedling. Int. J. Food Sci. Technol. 2021, 56, 6601–6610. [Google Scholar] [CrossRef]
- Tung, Y.T.; Zeng, J.L.; Ho, S.T.; Xu, J.W.; Lin, I.H.; Wu, J.H. Djulis hull improves insulin resistance and modulates the gut microbiota in high-fat diet (HFD)-induced hyperglycaemia. Antioxidants 2022, 11, 45. [Google Scholar] [CrossRef]
- Tung, Y.T.; Zeng, J.L.; Ho, S.T.; Xu, J.W.; Li, S.; Wu, J.H. Anti-NAFLD effect of djulis hull and its major compound, rutin, in mice with high-fat diet (HFD)-induced obesity. Antioxidants 2021, 10, 1694. [Google Scholar] [CrossRef]
- Zhou, D.; Yang, Q.; Tian, T.; Chang, Y.; Li, Y.; Duan, L.-R.; Li, H.; Wang, S.-W. Gastroprotective effect of gallic acid against ethanol-induced gastric ulcer in rats: Involvement of the Nrf2/HO-1 signaling and anti-apoptosis role. Biomed. Pharmacother. 2020, 126, 110075. [Google Scholar] [CrossRef] [PubMed]
- Beck, P.L.; Xavier, R.; Lu, N.; Nanda, N.N.; Dinauer, M.; Podolsky, D.K.; Seed, B. Mechanisms of NSAID-induced gastrointestinal injury defined using mutant mice. Gastroenterology 2000, 119, 699–705. [Google Scholar] [CrossRef]
- Tsai, H.Y.; Yang, J.F.; Chen, H.H.; You, F.N.; Zhao, Y.J.; Lin, Y.H.; Hsu, J.L.; Chang, C.I.; Chen, Y.K. The effect of hot water extract of tilapia on exercise capacity in mice. Appl. Sci. 2022, 12, 2601. [Google Scholar] [CrossRef]
- Tsai, H.Y.; Shih, Y.Y.; Yeh, Y.T.; Huang, C.H.; Liao, C.A.; Hu, C.Y.; Nagabhushanam, K.; Ho, C.T.; Chen, Y.K. Pterostilbene and its derivative 3′-hydroxypterostilbene ameliorated nonalcoholic fatty liver disease through synergistic modulation of the gut microbiota and SIRT1/AMPK signaling pathway. J. Agric. Food Chem. 2022, 70, 4966–4980. [Google Scholar] [CrossRef]
- Sinha, M.; Gautam, L.; Shukla, P.K.; Kaur, P.; Sharma, S.; Singh, T.P. Current perspectives in NSAID-induced gastropathy. Mediat. Inflamm. 2013, 2013, 258209. [Google Scholar] [CrossRef]
- Wallace, J.L. Prostaglandins, NSAIDs, and gastric mucosal protection: Why doesn’t the stomach digest itself? Physiol. Rev. 2008, 88, 1547–1565. [Google Scholar] [CrossRef] [PubMed]
- Nemmani, K.V.; Mali, S.V.; Borhade, N.; Pathan, A.R.; Karwa, M.; Pamidiboina, V.; Senthilkumar, S.P.; Gund, M.; Jain, A.K.; Mangu, N.K.; et al. NO-NSAIDs: Gastric-sparing nitric oxide-releasable prodrugs of non-steroidal anti-inflammatory drugs. Bioorg. Med. Chem. Lett. 2009, 19, 5297–5301. [Google Scholar] [CrossRef] [PubMed]
- Oren, R.; Ligumsky, M. Indomethacin-induced colonic ulceration and bleeding. Ann. Pharmacother. 1994, 28, 883–885. [Google Scholar] [CrossRef] [PubMed]
- Suleyman, H.; Albayrak, A.; Bilici, M.; Cadirci, E.; Halici, Z. Different mechanisms in formation and prevention of indomethacin-induced gastric ulcers. Inflammation 2010, 33, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Hamauzu, Y.; Irie, M.; Kondo, M.; Fujita, T. Antiulcerative properties of crude polyphenols and juice of apple, and Chinese quince extracts. Food Chem. 2008, 108, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; He, F.; Wu, C.; Li, P.; Li, N.; Deng, J.; Zhu, G.; Ren, W.; Peng, Y. Betaine in inflammation: Mechanistic aspects and applications. Front. Immunol. 2018, 9, 1070. [Google Scholar] [CrossRef]
- Svajger, U.; Jeras, M. Anti-inflammatory effects of resveratrol and its potential use in therapy of immune-mediated diseases. Int. Rev. Immunol. 2012, 31, 202–222. [Google Scholar] [CrossRef]
- Tsai, P.J.; Chen, Y.S.; Sheu, C.H.; Chen, C.Y. Effect of nanogrinding on the pigment and bioactivity of djulis (Chenopodium formosanum Koidz.). J. Agric. Food Chem. 2011, 59, 1814–1820. [Google Scholar] [CrossRef]
- Huang, H.W.; Cheng, M.C.; Chen, B.Y.; Wang, C.Y. Effects of high pressure extraction on the extraction yield, phenolic compounds, antioxidant and anti-tyrosinase activity of djulis hull. J. Food Sci. Technol. 2019, 56, 4016–4024. [Google Scholar] [CrossRef]
- Tanaka, A.; Hase, S.; Miyazawa, T.; Ohno, R.; Takeuchi, K. Role of cyclooxygenase (COX)-1 and COX-2 inhibition in nonsteroidal anti-inflammatory drug-induced intestinal damage in rats: Relation to various pathogenic events. J. Pharmacol. Exp. Ther. 2002, 303, 1248–1254. [Google Scholar] [CrossRef]
- Santucci, L.; Fiorucci, S.; Giansanti, M.; Brunori, P.M.; Di Matteo, F.M.; Morelli, A. Pentoxifylline prevents indomethacin induced acute gastric mucosal damage in rats: Role of tumour necrosis factor alpha. Gut 1994, 35, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Vivatvakin, S.; Werawatganon, D.; Somanawat, K.; Klaikeaw, N.; Siriviriyakul, P. Genistein-attenuated gastric injury on indomethacin-induced gastropathy in rats. Pharmacogn. Mag. 2017, 13, S306–S310. [Google Scholar] [CrossRef] [PubMed]
- Odabasoglu, F.; Cakir, A.; Suleyman, H.; Aslan, A.; Bayir, Y.; Halici, M.; Kazaz, C. Gastroprotective and antioxidant effects of usnic acid on indomethacin-induced gastric ulcer in rats. J. Ethnopharmacol. 2006, 103, 59–65. [Google Scholar] [CrossRef] [PubMed]


| Group | Ulcer Area (mm2) | Protective Index (%) |
|---|---|---|
| Control | 0 | ─ |
| IND | 2.7 ± 0.9 # | ─ |
| EEDH200 + IND | 0.9 ± 0.3 * | 67 |
| EEDH500 + IND | 0.5 ± 0.3 ** | 80 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Isnain, F.S.; Liao, N.-C.; Tsai, H.-Y.; Hsu, J.-L.; Tsai, P.-J.; Wardani, A.K.; Chen, Y.-K. Protective Effect of Ethanolic Extract of Djulis Hull on Indomethacin-Induced Gastric Injury. Appl. Sci. 2023, 13, 594. https://doi.org/10.3390/app13010594
Isnain FS, Liao N-C, Tsai H-Y, Hsu J-L, Tsai P-J, Wardani AK, Chen Y-K. Protective Effect of Ethanolic Extract of Djulis Hull on Indomethacin-Induced Gastric Injury. Applied Sciences. 2023; 13(1):594. https://doi.org/10.3390/app13010594
Chicago/Turabian StyleIsnain, Fuad Sauqi, Nai-Chen Liao, Hui-Yun Tsai, Jue-Liang Hsu, Pi-Jen Tsai, Agustin Krisna Wardani, and Yu-Kuo Chen. 2023. "Protective Effect of Ethanolic Extract of Djulis Hull on Indomethacin-Induced Gastric Injury" Applied Sciences 13, no. 1: 594. https://doi.org/10.3390/app13010594
APA StyleIsnain, F. S., Liao, N.-C., Tsai, H.-Y., Hsu, J.-L., Tsai, P.-J., Wardani, A. K., & Chen, Y.-K. (2023). Protective Effect of Ethanolic Extract of Djulis Hull on Indomethacin-Induced Gastric Injury. Applied Sciences, 13(1), 594. https://doi.org/10.3390/app13010594











