Predictors for Poor Outcomes at Six Months on Pain, Disability, Psychological and Health Status in Greek Patients with Chronic Low Back Pain After Receiving Physiotherapy: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
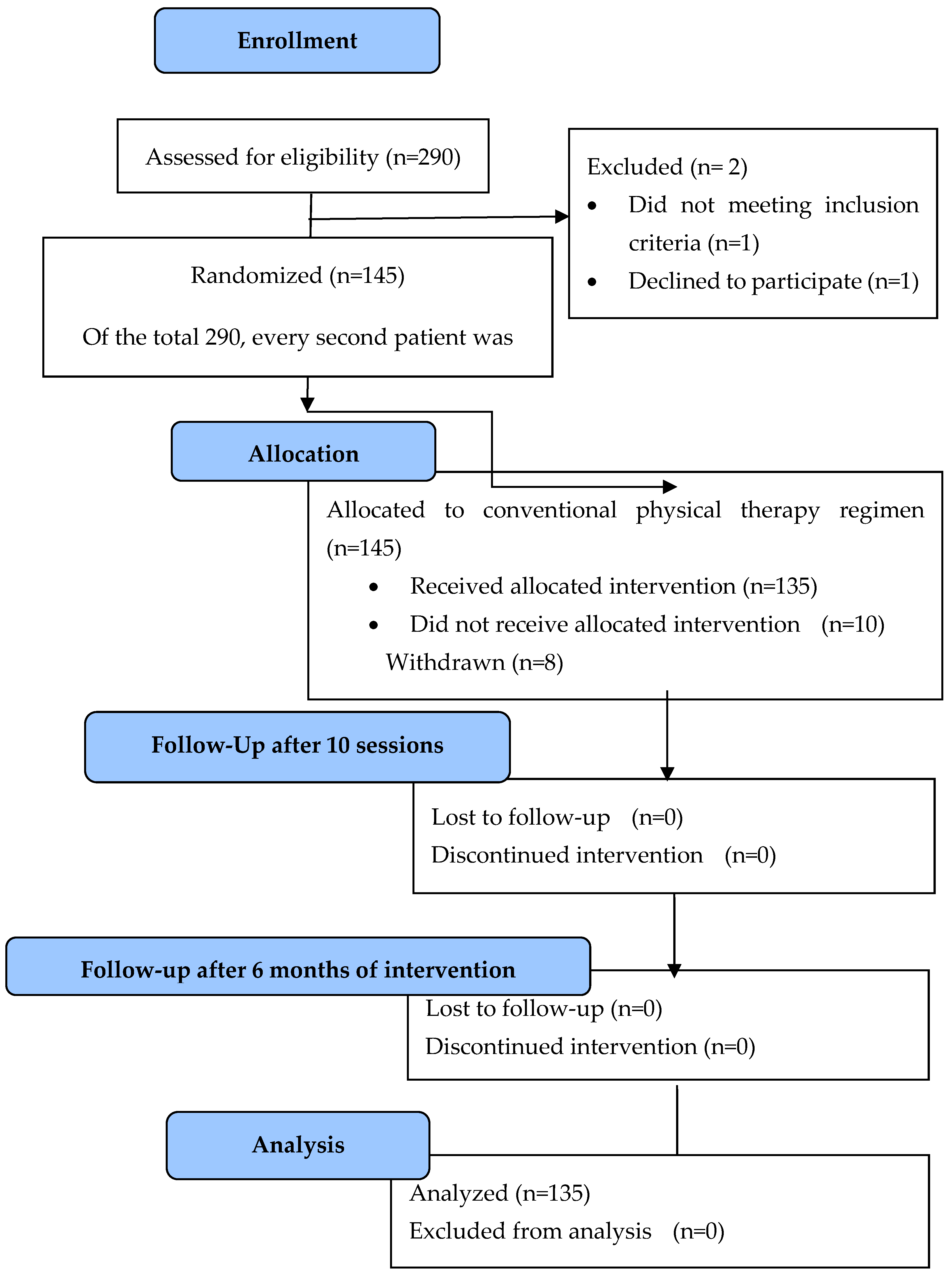
2.1. Study Design and Participants
2.2. Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SSD | Somatic symptom disorders |
| CLBP | Chronic low back pain |
| PNRS | Pain numerical rating scale |
| RMDQ | Roland–Morris Disability Questionnaire |
| EQ-5D-5L | EuroQol-5-dimension-5-level |
| HADS | Hospital Anxiety and Depression Scale |
| SSS-8 | Somatic Symptom Scale-8 |
| HRQoL | Health-related quality of life |
| TENS | Transcutaneous electrical nerve stimulation |
| US | Ultrasound |
| TYPET | Greek acronym for the Mutual Fund of National Bank of Greece Personnel |
| BMI | Body mass index |
References
- Global Burden of Disease 2021: Findings from the GBD 2021 Study | Institute for Health Metrics and Evaluation. Available online: https://www.healthdata.org/research-analysis/library/global-burden-disease-2021-findings-gbd-2021-study (accessed on 27 July 2024).
- Tyrovolas, S.; Kassebaum, N.J.; Stergachis, A.; Abraha, H.N.; Alla, F.; Androudi, S.; Car, M.; Chrepa, V.; Fullman, N.; Fürst, T.; et al. The Burden of Disease in Greece, Health Loss, Risk Factors, and Health Financing, 2000–16: An Analysis of the Global Burden of Disease Study 2016. Lancet Public Health 2018, 3, e395–e406. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What Low Back Pain Is and Why We Need to Pay Attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [PubMed]
- Bener, A.; Verjee, M.; Dafeeah, E.E.; Falah, O.; Aljuhaisi, T.; Schlogl, J.; Sedeeq, A.; Khan, S. Psychological Factors: Anxiety, Depression, and Somatization Symptoms in Low Back Pain Patients. J. Pain Res. 2013, 6, 95–101. [Google Scholar] [CrossRef]
- Alhowimel, A.; AlOtaibi, M.; Radford, K.; Coulson, N. Psychosocial Factors Associated with Change in Pain and Disability Outcomes in Chronic Low Back Pain Patients Treated by Physiotherapist: A Systematic Review. SAGE Open Med. 2018, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tom, A.A.; Rajkumar, E.; John, R.; George, A.J. Determinants of Quality of Life in Individuals with Chronic Low Back Pain: A Systematic Review. Health Psychol. Behav. Med. 2022, 10, 122–144. [Google Scholar] [CrossRef]
- Petrelis, M.; Soultanis, K.; Michopoulos, I.; Nikolaou, V. Associations of Somatic Symptom Disorder with Pain, Disability and Quality of Life in Patients with Chronic Low Back Pain. Psychiatriki 2023, 34, 221–230. [Google Scholar] [CrossRef]
- Artus, M.; Campbell, P.; Mallen, C.D.; Dunn, K.M.; van der Windt, D.A.W. Generic Prognostic Factors for Musculoskeletal Pain in Primary Care: A Systematic Review. BMJ Open 2017, 7, e012901. [Google Scholar] [CrossRef]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann. Intern. Med. 2017, 166, 514. [Google Scholar] [CrossRef]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. Chapter 4: European Guidelines for the Management of Chronic Nonspecific Low Back Pain. Eur. Spine J. 2006, 15, s192–s300. [Google Scholar] [CrossRef]
- Acaroğlu, E.; Nordin, M.; Randhawa, K.; Chou, R.; Côté, P.; Mmopelwa, T.; Haldeman, S. The Global Spine Care Initiative: A Summary of Guidelines on Invasive Interventions for the Management of Persistent and Disabling Spinal Pain in Low- and Middle-Income Communities. Eur. Spine J. 2018, 27, 870–878. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE). Low Back Pain and Sciatica in over 16s: Assessment and Management. NICE Guideline NG59. Available online: https://www.ncbi.nlm.nih.gov/books/NBK562933/ (accessed on 1 April 2021).
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and Treatment of Low Back Pain: Evidence, Challenges, and Promising Directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef] [PubMed]
- Durmus, D.; Alayli, G.; Goktepe, A.S.; Taskaynatan, M.A.; Bilgici, A.; Kuru, O. Is Phonophoresis Effective in the Treatment of Chronic Low Back Pain? A Single-Blind Randomized Controlled Trial. Rheumatol. Int. 2013, 33, 1737–1744. [Google Scholar] [CrossRef]
- Pivovarsky, M.L.F.; Gaideski, F.; de Macedo, R.M.; Korelo, R.I.G.; Guarita-Souza, L.C.; Liebano, R.E.; de Macedo, A.C.B. Immediate Analgesic Effect of Two Modes of Transcutaneous Electrical Nerve Stimulation on Patients with Chronic Low Back Pain: A Randomized Controlled Trial. Einstein (São Paulo) 2021, 19, eAO6027. [Google Scholar] [CrossRef] [PubMed]
- Glazov, G.; Yelland, M.; Emery, J. Low-Level Laser Therapy for Chronic Non-Specific Low Back Pain: A Meta-Analysis of Randomised Controlled Trials. Acupunct. Med. 2016, 34, 328–341. [Google Scholar] [CrossRef]
- Huang, Z.; Ma, J.; Chen, J.; Shen, B.; Pei, F.; Kraus, V.B. The Effectiveness of Low-Level Laser Therapy for Nonspecific Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Arthritis Res. Ther. 2015, 17, 360. [Google Scholar] [CrossRef] [PubMed]
- Rubira, A.P.F.D.A.; Rubira, M.C.; Rubira, L.D.A.; Comachio, J.; Magalhães, M.O.; Marques, A.P. Comparison of the Effects of Low-Level Laser and Pulsed and Continuous Ultrasound on Pain and Physical Disability in Chronic Non-Specific Low Back Pain: A Randomized Controlled Clinical Trial. Adv. Rheumatol. 2019, 59, 57. [Google Scholar] [CrossRef]
- Sahin, N.; Karahan, A.Y.; Albayrak, I. Effectiveness of Physical Therapy and Exercise on Pain and Functional Status in Patients with Chronic Low Back Pain: A Randomized-Controlled Trial. Turk. J. Phys. Med. Rehabil. 2018, 64, 52–58. [Google Scholar] [CrossRef]
- van Middelkoop, M.; Rubinstein, S.M.; Kuijpers, T.; Verhagen, A.P.; Ostelo, R.; Koes, B.W.; van Tulder, M.W. A Systematic Review on the Effectiveness of Physical and Rehabilitation Interventions for Chronic Non-Specific Low Back Pain. Eur. Spine J. 2011, 20, 19–39. [Google Scholar] [CrossRef] [PubMed]
- Ferlito, R.; Blatti, C.; Lucenti, L.; Boscarino, U.; Sapienza, M.; Pavone, V.; Testa, G. Pain Education in the Management of Patients with Chronic Low Back Pain: A Systematic Review. J. Funct. Morphol. Kinesiol. 2022, 7, 74. [Google Scholar] [CrossRef]
- Karstens, S.; Hermann, K.; Froböse, I.; Weiler, S.W. Predictors for Half-Year Outcome of Impairment in Daily Life for Back Pain Patients Referred for Physiotherapy: A Prospective Observational Study. PLoS ONE 2013, 8, e61587. [Google Scholar] [CrossRef]
- Cruz, E.B.; Canhão, H.; Fernandes, R.; Caeiro, C.; Branco, J.C.; Rodrigues, A.M.; Pimentel-Santos, F.; Gomes, L.A.; Paiva, S.; Pinto, I.; et al. Prognostic Indicators for Poor Outcomes in Low Back Pain Patients Consulted in Primary Care. PLoS ONE 2020, 15, e0229265. [Google Scholar] [CrossRef] [PubMed]
- Zografakis-Sfakianakis, M.; Sousamlis, M.; Kounalaki, E.; Skoulikari, K.; Iliaki, A.; Fragiadaki, E. Assessment of the Health Related Quality of Life of Patients with Low Back Pain under Conservative Treatment. Nosileftiki 2010, 49, 182–194. [Google Scholar]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement. Epidemiology 2007, 18, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Kamali, F.; Panahi, F.; Ebrahimi, S.; Abbasi, L. Comparison between Massage and Routine Physical Therapy in Women with Sub Acute and Chronic Nonspecific Low Back Pain. J. Back Musculoskelet. Rehabil. 2014, 27, 475–480. [Google Scholar] [CrossRef]
- Dilekçi, E.; Özkuk, K.; Kaki, B. The Short-Term Effects of Balneotherapy on Pain, Disability and Fatigue in Patients with Chronic Low Back Pain Treated with Physical Therapy: A Randomized Controlled Trial. Complement. Ther. Med. 2020, 54, 102550. [Google Scholar] [CrossRef]
- Köroğlu, F.; Çolak, T.K.; Polat, M.G. The Effect of Kinesio® Taping on Pain, Functionality, Mobility and Endurance in the Treatment of Chronic Low Back Pain: A Randomized Controlled Study. J. Back Musculoskelet. Rehabil. 2017, 30, 1087–1093. [Google Scholar] [CrossRef]
- Nambi, G.; Kamal, W.; Es, S.; Joshi, S.; Trivedi, P. Spinal Manipulation plus Laser Therapy versus Laser Therapy Alone in the Treatment of Chronic Non-Specific Low Back Pain: A Randomized Controlled Study. Eur. J. Phys. Rehabil. Med. 2019, 54, 880–889. [Google Scholar] [CrossRef]
- Koldaş Doğan, Ş.; Ay, S.; Evcik, D. The Effects of Two Different Low Level Laser Therapies in the Treatment of Patients with Chronic Low Back Pain: A Double-Blinded Randomized Clinical Trial. J. Back Musculoskelet. Rehabil. 2017, 30, 235–240. [Google Scholar] [CrossRef]
- Kent, P.; Keating, J.L.; Leboeuf-Yde, C. Research methods for subgrouping low back pain. BMC Med. Res. Methodol. 2010, 10, 62. [Google Scholar] [CrossRef]
- Childs, J.D.; Piva, S.R.; Fritz, J.M. Responsiveness of the Numeric Pain Rating Scale in Patients with Low Back Pain. Spine 2005, 30, 1331–1334. [Google Scholar] [CrossRef] [PubMed]
- Roland, M.; Fairbank, J. The Roland–Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000, 25, 3115–3124. [Google Scholar] [CrossRef]
- Kontodimopoulos, N.; Pappa, E.; Niakas, D.; Yfantopoulos, J.; Dimitrakaki, C.; Tountas, Y. Validity of the EuroQoL (EQ-5D) Instrument in a Greek General Population. Value Health 2008, 11, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Soer, R.; Reneman, M.F.; Speijer, B.L.G.N.; Coppes, M.H.; Vroomen, P.C.A.J. Clinimetric Properties of the EuroQol-5D in Patients with Chronic Low Back Pain. Spine J. 2012, 12, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Gierk, B.; Kohlmann, S.; Kroenke, K.; Spangenberg, L.; Zenger, M.; Brähler, E.; Löwe, B. The Somatic Symptom Scale–8 (SSS-8). JAMA Intern. Med. 2014, 174, 399–407. [Google Scholar] [CrossRef]
- Chapman, J.R.; Norvell, D.C.; Hermsmeyer, J.T.; Bransford, R.J.; DeVine, J.; McGirt, M.J.; Lee, M.J. Evaluating Common Outcomes for Measuring Treatment Success for Chronic Low Back Pain. Spine 2011, 36, S54–S68. [Google Scholar] [CrossRef]
- Michopoulos, I.; Douzenis, A.; Kalkavoura, C.; Christodoulou, C.; Michalopoulou, P.; Kalemi, G.; Fineti, K.; Patapis, P.; Protopapas, K.; Lykouras, L. Hospital Anxiety and Depression Scale (HADS): Validation in a Greek General Hospital Sample. Ann. Gen. Psychiatry 2008, 7, 4. [Google Scholar] [CrossRef]
- Petrelis, M.; Domeyer, P.-R. Translation and Validation of the Greek Version of the Somatic Symptom Scale-8 (SSS-8) in Patients with Chronic Low Back Pain. Disabil. Rehabil. 2021, 44, 4467–4473. [Google Scholar] [CrossRef]
- Yfantopoulos, J.N.; Chantzaras, A.E. Validation and Comparison of the Psychometric Properties of the EQ-5D-3L and EQ-5D-5L Instruments in Greece. The Eur. J. Health Econ. 2017, 18, 519–531. [Google Scholar] [CrossRef]
- Tomczak, M.; Tomczak, E. The Need to Report Effect Size Estimates Revisited. An Overview of Some Recommended Measures of Effect Size; Akademia Wychowania Fizycznego w Poznaniu: Poznań, Poland, 2014; Volume 1. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Keeley, P.; Creed, F.; Tomenson, B.; Todd, C.; Borglin, G.; Dickens, C. Psychosocial Predictors of Health-Related Quality of Life and Health Service Utilisation in People with Chronic Low Back Pain. Pain 2008, 135, 142–150. [Google Scholar] [CrossRef]
- Mutubuki, E.N.; Beljon, Y.; Maas, E.T.; Huygen, F.J.P.M.; Ostelo, R.W.J.G.; van Tulder, M.W.; van Dongen, J.M. The Longitudinal Relationships between Pain Severity and Disability versus Health-Related Quality of Life and Costs among Chronic Low Back Pain Patients. Qual. Life Res. 2020, 29, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Oka, H.; Katsuhira, J.; Tonosu, J.; Kasahara, S.; Tanaka, S.; Matsudaira, K. Association between Somatic Symptom Burden and Health-Related Quality of Life in People with Chronic Low Back Pain. PLoS ONE 2018, 13, e0193208. [Google Scholar] [CrossRef] [PubMed]
- Ailliet, L.; Rubinstein, S.M.; Knol, D.; van Tulder, M.W.; de Vet, H.C.W. Somatization Is Associated with Worse Outcome in a Chiropractic Patient Population with Neck Pain and Low Back Pain. Man. Ther. 2016, 21, 170–176. [Google Scholar] [CrossRef]
- Jegan, N.R.A.; Brugger, M.; Viniol, A.; Strauch, K.; Barth, J.; Baum, E.; Leonhardt, C.; Becker, A. Psychological Risk and Protective Factors for Disability in Chronic Low Back Pain—A Longitudinal Analysis in Primary Care. BMC Musculoskelet. Disord. 2017, 18, 114. [Google Scholar] [CrossRef]
- Alhowimel, A.S.; Alotaibi, M.A.; Alenazi, A.M.; Alqahtani, B.A.; Alshehri, M.A.; Alamam, D.; Alodaibi, F.A. Psychosocial Predictors of Pain and Disability Outcomes in People with Chronic Low Back Pain Treated Conservatively by Guideline-Based Intervention: A Systematic Review. J. Multidiscip. Healthc. 2021, 14, 3549–3559. [Google Scholar] [CrossRef]
- Tomenson, B.; Essau, C.; Jacobi, F.; Ladwig, K.H.; Leiknes, K.A.; Lieb, R.; Meinlschmidt, G.; Mcbeth, J.; Rosmalen, J.; Rief, W.; et al. Total Somatic Symptom Score as a Predictor of Health Outcome in Somatic Symptom Disorders. Br. J. Psychiatry 2013, 203, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Lykouras, L. Psychological Profile of Obese Patients. Dig. Dis. 2007, 26, 36–39. [Google Scholar] [CrossRef]
- Wimmelmann, C.L.; Lund, R.; Christensen, U.; Osler, M.; Mortensen, E.L. Associations between Obesity and Mental Distress in Late Midlife: Results from a Large Danish Community Sample. BMC Obes. 2016, 3, 54. [Google Scholar] [CrossRef]
- Wettstein, M.; Eich, W.; Bieber, C.; Tesarz, J. Pain Intensity, Disability, and Quality of Life in Patients with Chronic Low Back Pain: Does Age Matter? Pain. Med. 2019, 20, 464–475. [Google Scholar] [CrossRef]
- Kohlmann, S.; Gierk, B.; Hilbert, A.; Brähler, E.; Löwe, B. The Overlap of Somatic, Anxious and Depressive Syndromes: A Population-Based Analysis. J. Psychosom. Res. 2016, 90, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.; Hommel, G.; Blettner, M. Linear Regression Analysis: Part 14 of a Series on Evaluation of Scientific Publications. Dtsch. Arztebl. Int. 2010, 107, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, M.O.; Comachio, J.; Ferreira, P.H.; Pappas, E.; Marques, A.P. Effectiveness of Graded Activity versus Physiotherapy in Patients with Chronic Nonspecific Low Back Pain: Midterm Follow up Results of a Randomized Controlled Trial. Braz. J. Phys. Ther. 2018, 22, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Kostadinović, S.; Milovanović, N.; Jovanović, J.; Tomašević-Todorović, S. Efficacy of the Lumbar Stabilization and Thoracic Mobilization Exercise Program on Pain Intensity and Functional Disability Reduction in Chronic Low Back Pain Patients with Lumbar Radiculopathy: A Randomized Controlled Trial. J. Back Musculoskelet. Rehabil. 2020, 33, 897–907. [Google Scholar] [CrossRef]
- Díaz-Arribas, M.J.; Kovacs, F.M.; Royuela, A.; Fernández-Serrano, M.; Gutiérrez-Fernández, L.; San Martín-Pariente, O.; Abraira, V.; Ramos-Sánchez, M.; Llorca-Palomera, R.; Pardo-Hervás, P.; et al. Effectiveness of the Godelieve Denys-Struyf (GDS) Method in People with Low Back Pain: Cluster Randomized Controlled Trial. Phys. Ther. 2015, 95, 319–336. [Google Scholar] [CrossRef]
- Hampel, P.; Tlach, L. Cognitive-Behavioral Management Training of Depressive Symptoms among Inpatient Orthopedic Patients with Chronic Low Back Pain and Depressive Symptoms: A 2-Year Longitudinal Study. J. Back Musculoskelet. Rehabil. 2015, 28, 49–60. [Google Scholar] [CrossRef]
| n = 135 | Mean | SD | |
|---|---|---|---|
| Age | 60.6 | 14.7 | |
| BMI | 27.2 | 5.3 | |
| n | % | ||
| Gender | |||
| Man | 54 | 40.0 | |
| Woman | 81 | 60.0 | |
| BMI | |||
| Normal | 48 | 35.6 | |
| Overweight | 56 | 41.5 | |
| Obese | 31 | 23.0 | |
| Marital status | |||
| Unmarried | 24 | 17.8 | |
| Married | 74 | 54.8 | |
| Divorced | 17 | 12.6 | |
| Widowed | 20 | 14.8 | |
| Educational level | |||
| Primary school | 5 | 3.7 | |
| Secondary school | 8 | 5.9 | |
| High school | 36 | 26.7 | |
| Two years of college | 5 | 3.7 | |
| University | 56 | 41.5 | |
| Postgraduate degree | 25 | 18.5 | |
| Working status | |||
| Employee in the private sector | 33 | 24.4 | |
| Freelancer | 6 | 4.4 | |
| Employee in the public sector | 0 | 0.0 | |
| Pensioner | 83 | 61.5 | |
| Student | 1 | 0.7 | |
| Household labor | 10 | 7.4 | |
| Unemployed | 2 | 1.5 | |
| Unable to work | 0 | 0.0 | |
| Dependent Variable: EQ5D (6 Months) | β + | SE ++ | p |
|---|---|---|---|
| Gender (women vs. men) | 0.001 | 0.026 | 0.975 |
| Age | −0.004 | 0.001 | 0.001 |
| BMI | |||
| Normal vs. obese | −0.036 | 0.036 | 0.328 |
| Overweight vs. obese | 0.042 | 0.033 | 0.211 |
| Educational level | |||
| Primary/secondary/high school vs. postgraduate degree | −0.020 | 0.041 | 0.628 |
| Two years of college/university vs. postgraduate degree | −0.046 | 0.038 | 0.227 |
| Married (yes vs. no) | 0.016 | 0.025 | 0.523 |
| Employed (yes vs. no) | −0.083 | 0.045 | 0.059 |
| SSS-8 (pre) | −0.002 | 0.003 | 0.441 |
| HADS depression (pre) | −0.008 | 0.004 | 0.077 |
| HADS anxiety (pre) | −0.005 | 0.004 | 0.266 |
| PMDQ score (pre) | −0.005 | 0.003 | 0.140 |
| PNRS (pre) | −0.027 | 0.007 | <0.001 |
| Dependent Variable | Independent Variables | β + | SE ++ | p |
|---|---|---|---|---|
| HADS Depression (6 months) | Gender (women vs. men) | 0.039 | 0.052 | 0.450 |
| Age | 0.001 | 0.003 | 0.752 | |
| BMI | ||||
| Normal vs. obese | 0.018 | 0.070 | 0.793 | |
| Overweight vs. obese | −0.071 | 0.064 | 0.272 | |
| Educational level | ||||
| Primary/secondary/high school vs. postgraduate degree | 0.005 | 0.079 | 0.949 | |
| Two years of college/university vs. postgraduate degree | 0.003 | 0.073 | 0.973 | |
| Married (yes vs. no) | 0.008 | 0.049 | 0.869 | |
| Employed (yes vs. no) | −0.047 | 0.081 | 0.562 | |
| SSS-8 (pre) | 0.018 | 0.006 | 0.003 | |
| RMDQ (pre) | 0.004 | 0.006 | 0.558 | |
| PNRS (pre) | −0.008 | 0.013 | 0.540 | |
| HADS Anxiety (6 months) | Gender (women vs. men) | 0.041 | 0.057 | 0.477 |
| Age | −0.002 | 0.003 | 0.562 | |
| BMI | ||||
| Normal vs. obese | 0.068 | 0.077 | 0.375 | |
| Overweight vs. obese | −0.022 | 0.070 | 0.757 | |
| Educational level | ||||
| Primary/secondary/high school vs. postgraduate degree | −0.090 | 0.087 | 0.305 | |
| Two years of college/university vs. postgraduate degree | −0.078 | 0.081 | 0.337 | |
| Married (yes vs. no) | 0.017 | 0.054 | 0.748 | |
| Employed (yes vs. no) | −0.060 | 0.089 | 0.500 | |
| SSS-8 (pre) | 0.017 | 0.006 | 0.008 | |
| RMDQ (pre) | 0.011 | 0.007 | 0.094 | |
| PNRS (pre) | 0.003 | 0.014 | 0.843 |
| Dependent Variable | Independent Variables | β + | SE ++ | p |
|---|---|---|---|---|
| RMDQ Score (6 months) | Gender (women vs. men) | −0.029 | 0.064 | 0.655 |
| Age | 0.009 | 0.003 | 0.006 | |
| BMI | ||||
| Normal vs. obese | −0.060 | 0.087 | 0.492 | |
| Overweight vs. obese | −0.140 | 0.079 | 0.078 | |
| Educational level | ||||
| Primary/secondary/high school vs. postgraduate degree | 0.022 | 0.098 | 0.825 | |
| Two years of college/university vs. postgraduate degree | 0.101 | 0.090 | 0.264 | |
| Married (yes vs. no) | −0.020 | 0.061 | 0.742 | |
| Employed (yes vs. no) | 0.170 | 0.100 | 0.091 | |
| SSS-8 (pre) | 0.016 | 0.007 | 0.025 | |
| PNRS (pre) | 0.036 | 0.016 | 0.024 | |
| PNRS (6 months) | Gender (women vs. men) | −0.002 | 0.047 | 0.963 |
| Age | 0.001 | 0.002 | 0.723 | |
| BMI | ||||
| Normal vs. obese | 0.001 | 0.062 | 0.993 | |
| Overweight vs. obese | 0.007 | 0.057 | 0.905 | |
| Educational level | ||||
| Primary/secondary/high school vs. postgraduate degree | 0.013 | 0.072 | 0.853 | |
| Two years of college/university vs. postgraduate degree | 0.027 | 0.066 | 0.683 | |
| Married (yes vs. no) | 0.000 | 0.045 | 0.993 | |
| Employed (yes vs. no) | −0.082 | 0.073 | 0.262 | |
| SSS-8 (pre) | 0.019 | 0.005 | <0.001 | |
| SSS-8 (6 months) | Gender (women vs. men) | 0.094 | 0.049 | 0.057 |
| Age | 0.001 | 0.002 | 0.703 | |
| BMI | ||||
| Normal vs. obese | −0.113 | 0.064 | 0.082 | |
| Overweight vs. obese | −0.139 | 0.060 | 0.023 | |
| Educational level | ||||
| Primary/secondary/high school vs. postgraduate degree | −0.016 | 0.077 | 0.834 | |
| Two years of college/university vs. postgraduate degree | −0.006 | 0.071 | 0.932 | |
| Married (yes vs. no) | −0.014 | 0.048 | 0.765 | |
| Employed (yes vs. no) | −0.024 | 0.078 | 0.757 |
| Pre 1 | Post 2 | 6 Months 3 | P Friedman Test | Effect Size W | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |||
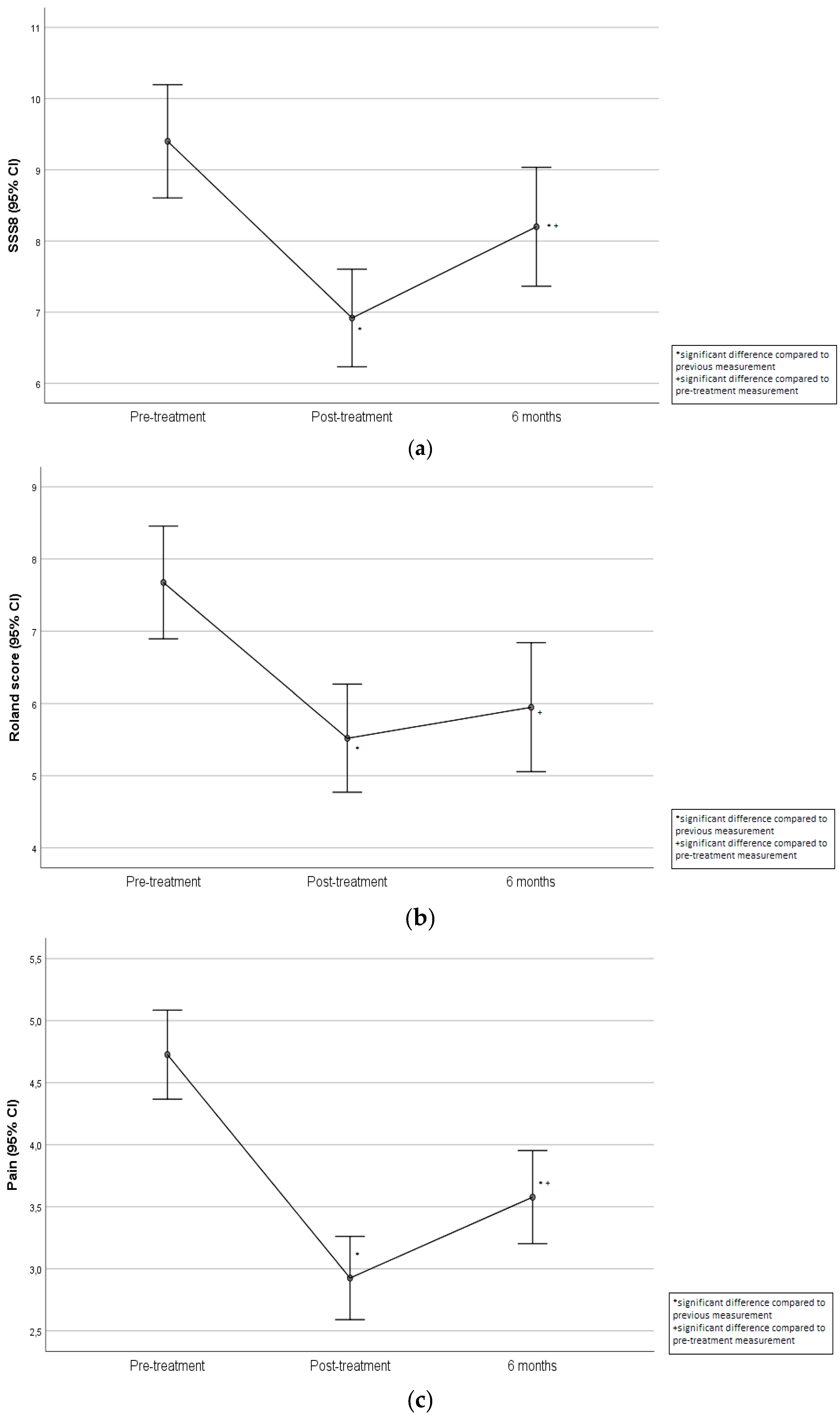
| SSS-8 score | 9.4 (4.67) 2,3 | 9 (6–12) | 6.92 (4.03) 1,3 | 6 (4–10) | 8.2 (4.9) 1,2 | 8 (4–11) | <0.001 | 0.15 |
| HADS depression score | 5.87 (3.3) | 6 (3–8) | 5.44 (3.27) | 5 (3–7) | 5.63 (3.61) | 5 (3–8) | 0.059 | 0.02 |
| HADS anxiety score | 5.41 (3.52) 2 | 6 (2–7) | 4.76 (3.54) 1 | 4 (2–7) | 5.22 (3.6) | 5 (3–7) | 0.002 | 0.05 |
| RMDQ | 7.67 (4.59) 2,3 | 7 (4–10) | 5.52 (4.39) 1 | 5 (2–8) | 5.95 (5.24) 1 | 4 (1–9) | <0.001 | 0.15 |
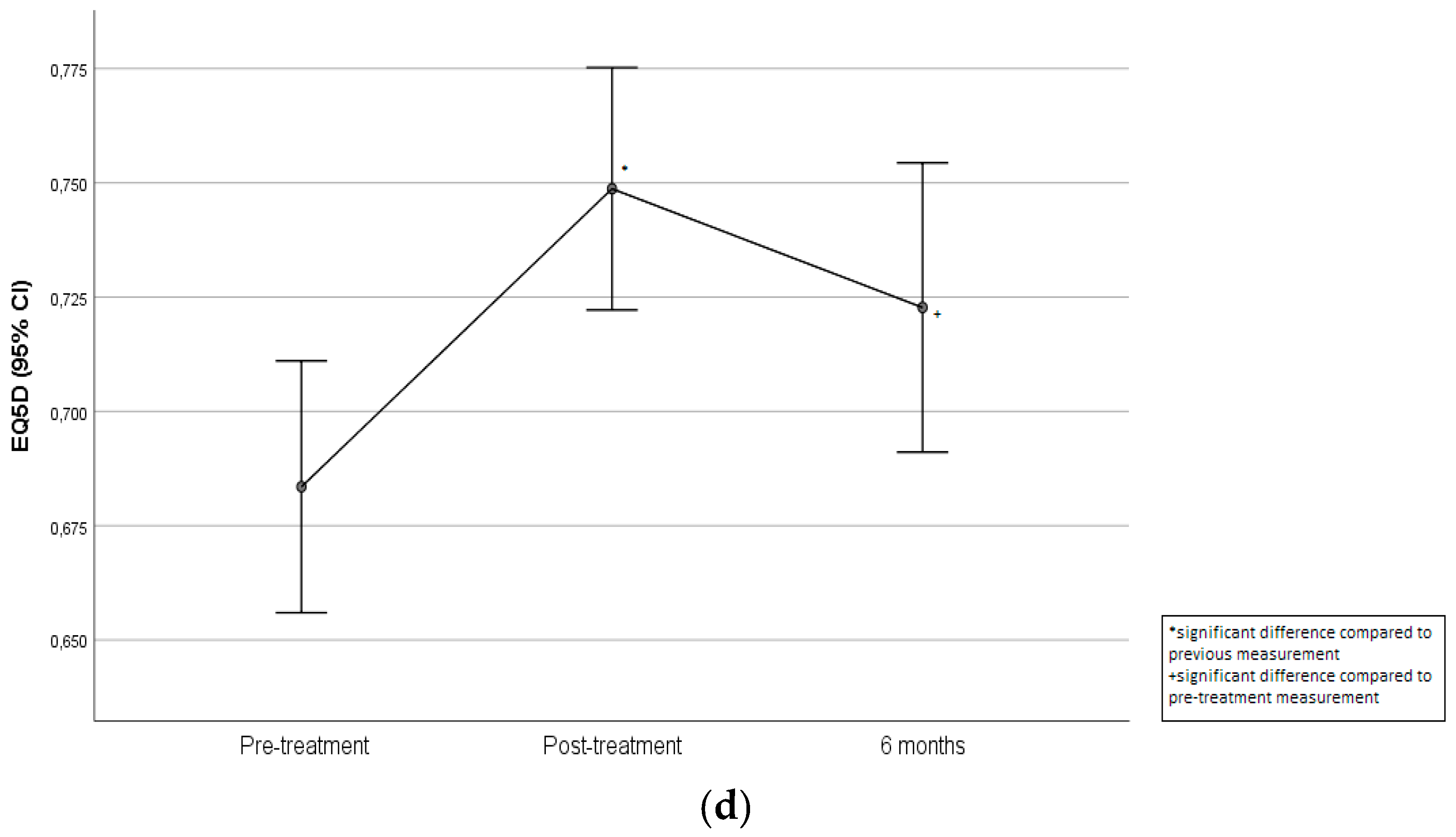
| EQ-5D-5L value | 0.68 (0.16) 2,3 | 0.71 (0.6–0.78) | 0.75 (0.15) 1 | 0.76 (0.68–0.86) | 0.72 (0.18) 1 | 0.76 (0.68–0.83) | <0.001 | 0.20 |
| PNRS (0–10 scale) | 4.73 (2.11) 2,3 | 5 (3–6) | 2.93 (1.97) 1,3 | 3 (2–5) | 3.58 (2.2) 1,2 | 3 (2–5) | <0.001 | 0.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrelis, M.; Krekoukias, G.; Michopoulos, I.; Nikolaou, V.; Soultanis, K. Predictors for Poor Outcomes at Six Months on Pain, Disability, Psychological and Health Status in Greek Patients with Chronic Low Back Pain After Receiving Physiotherapy: A Prospective Cohort Study. Clin. Pract. 2025, 15, 63. https://doi.org/10.3390/clinpract15030063
Petrelis M, Krekoukias G, Michopoulos I, Nikolaou V, Soultanis K. Predictors for Poor Outcomes at Six Months on Pain, Disability, Psychological and Health Status in Greek Patients with Chronic Low Back Pain After Receiving Physiotherapy: A Prospective Cohort Study. Clinics and Practice. 2025; 15(3):63. https://doi.org/10.3390/clinpract15030063
Chicago/Turabian StylePetrelis, Matthaios, Georgios Krekoukias, Ioannis Michopoulos, Vasileios Nikolaou, and Konstantinos Soultanis. 2025. "Predictors for Poor Outcomes at Six Months on Pain, Disability, Psychological and Health Status in Greek Patients with Chronic Low Back Pain After Receiving Physiotherapy: A Prospective Cohort Study" Clinics and Practice 15, no. 3: 63. https://doi.org/10.3390/clinpract15030063
APA StylePetrelis, M., Krekoukias, G., Michopoulos, I., Nikolaou, V., & Soultanis, K. (2025). Predictors for Poor Outcomes at Six Months on Pain, Disability, Psychological and Health Status in Greek Patients with Chronic Low Back Pain After Receiving Physiotherapy: A Prospective Cohort Study. Clinics and Practice, 15(3), 63. https://doi.org/10.3390/clinpract15030063







