Phimosis in Adults: Narrative Review of the New Available Devices and the Standard Treatments
Abstract
1. Introduction
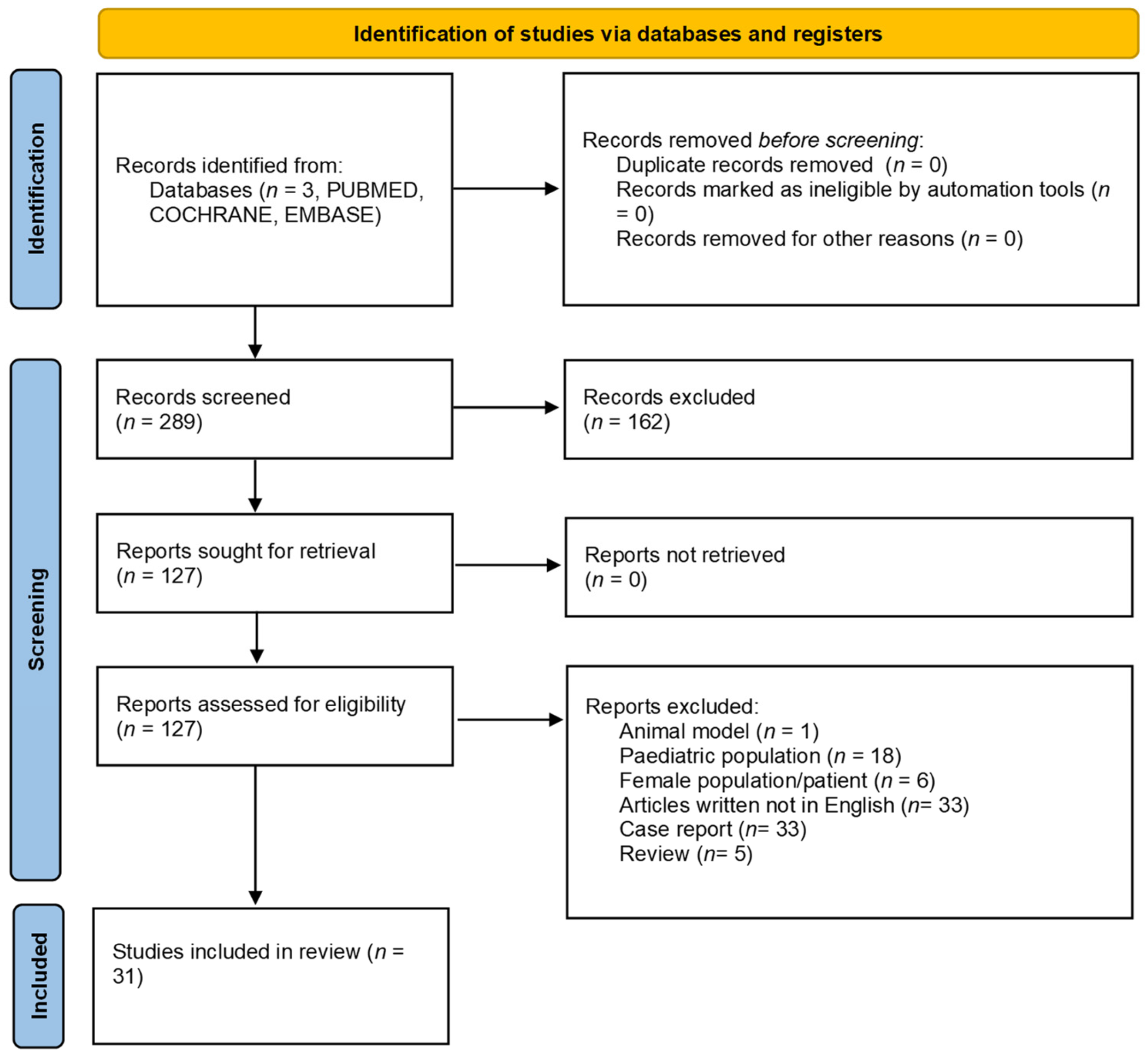
2. Materials and Methods
3. Results
3.1. Conservative Treatments
3.1.1. Topical Corticosteroids
3.1.2. The Platelet-Rich Plasma (PRP) for Lichen Sclerosus (LS)
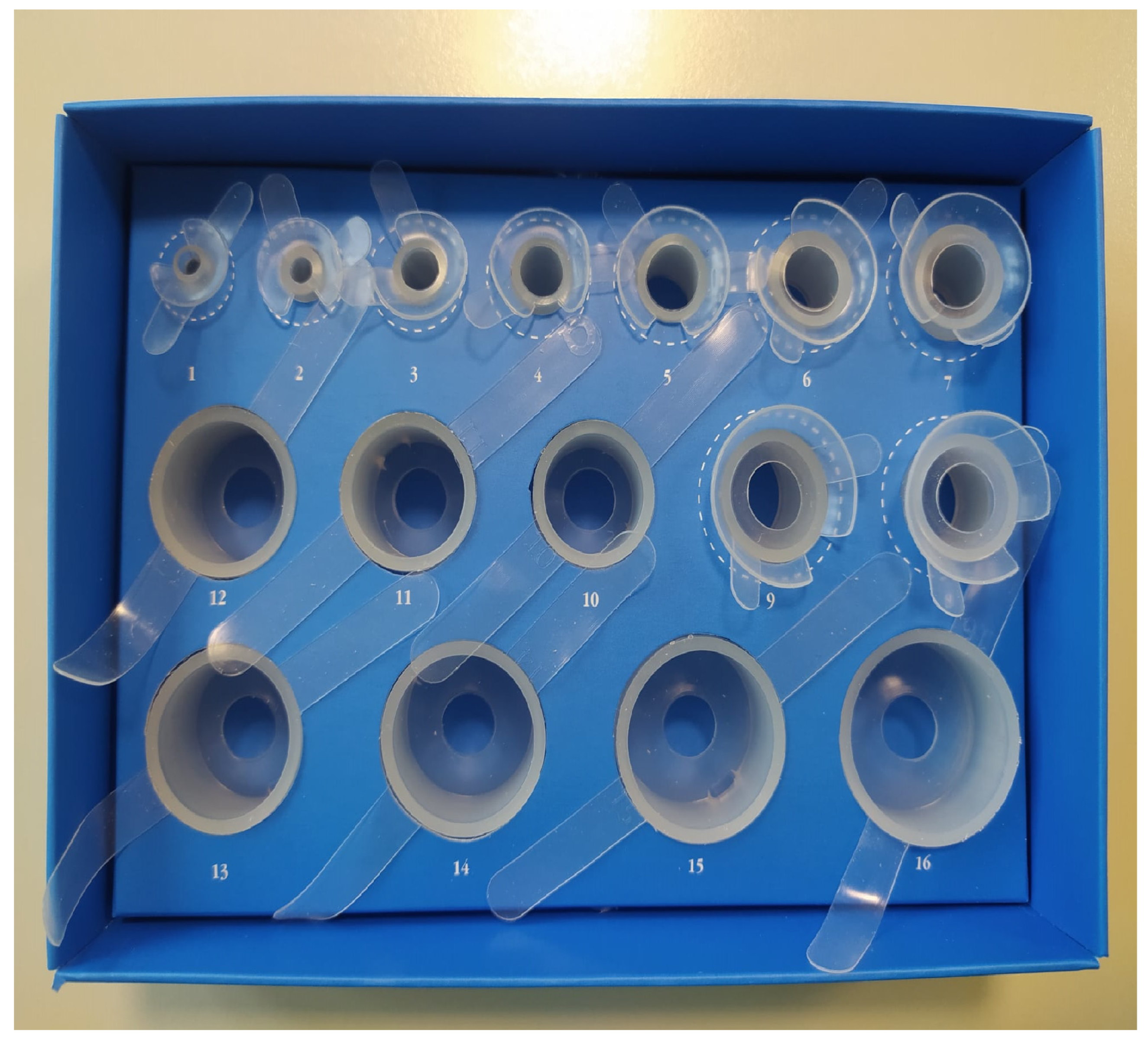
3.1.3. PhimoStop™
3.2. Surgical Treatment
3.2.1. Circumcision
Techniques of Circumcision (Figure 3)
Alternative Devices for Suture
Laser Circumcision
3.2.2. Circumcision in Elderly Patients
3.2.3. Effect of Circumcision on Sexual Function
3.3. Preputial Sparing Techniques
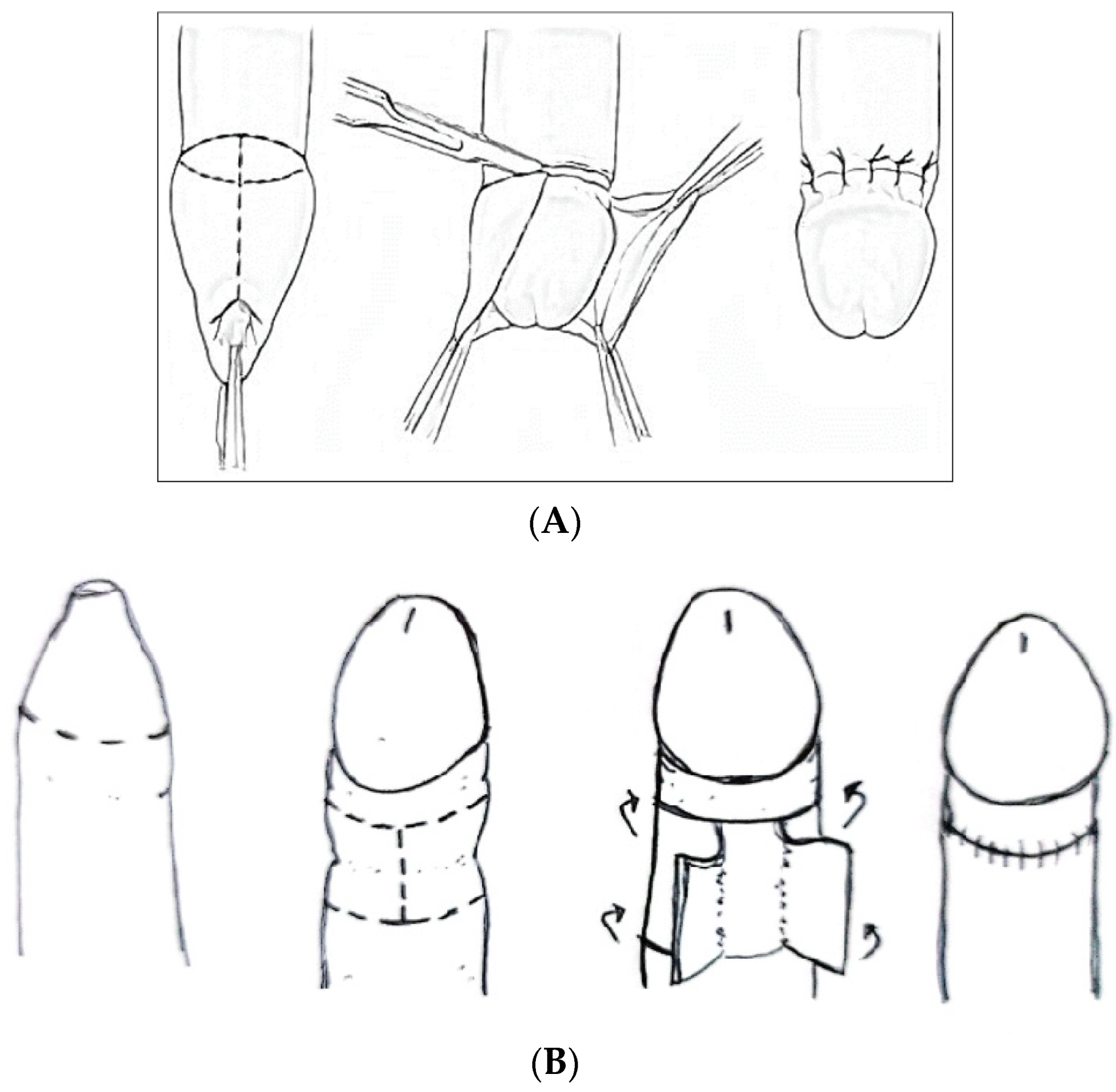
3.3.1. Prepuce-Sparing Plasty and Simple Running Suture (Figure 4)

3.3.2. Y-V Preputioplasty (Figure 4)
3.3.3. Heineke-Mikulicz Preputioplasty (Figure 5)

3.4. In Situ Devices
3.4.1. The Gomco Clamp
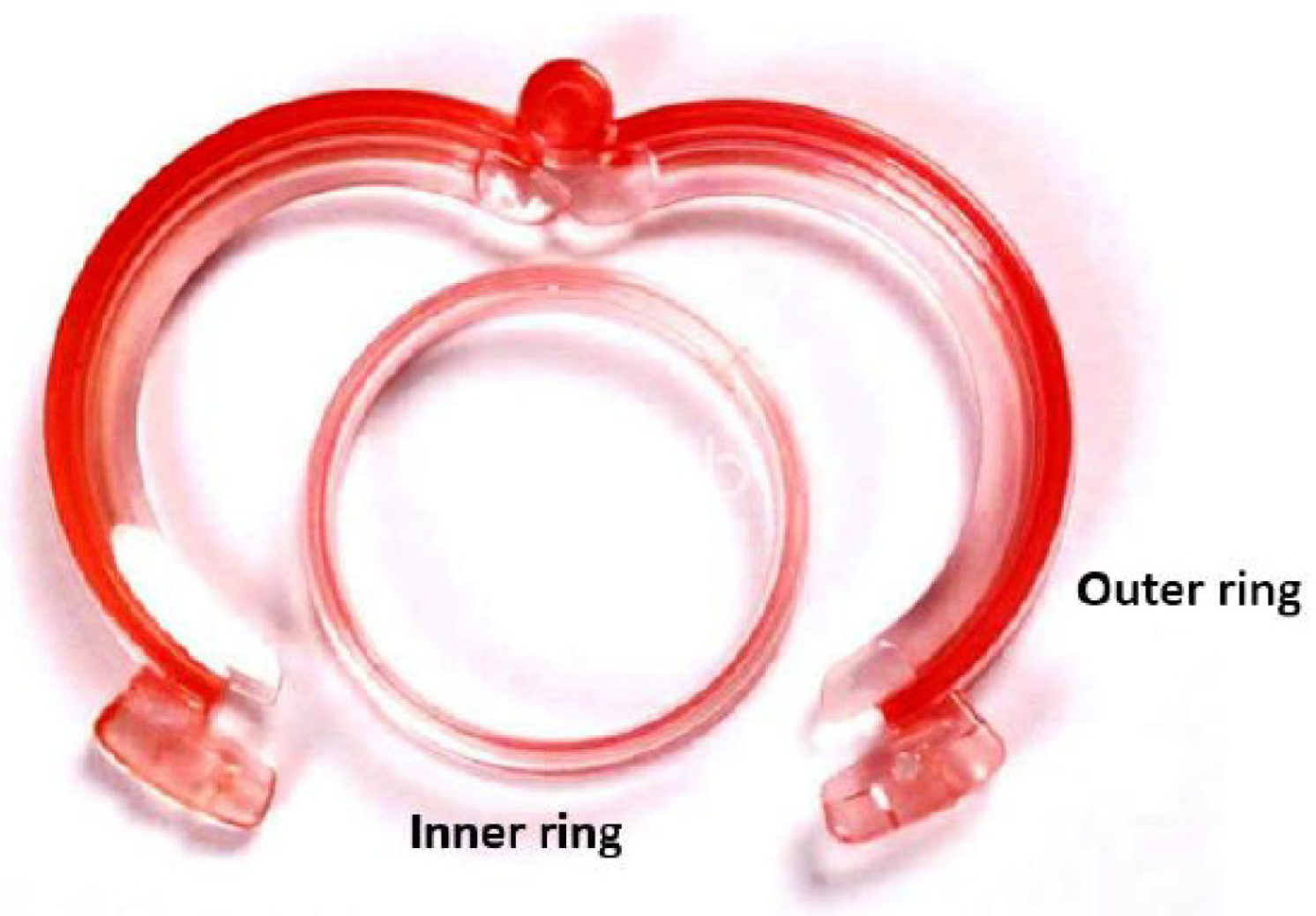
3.4.2. The PrePex Device (Figure 6)
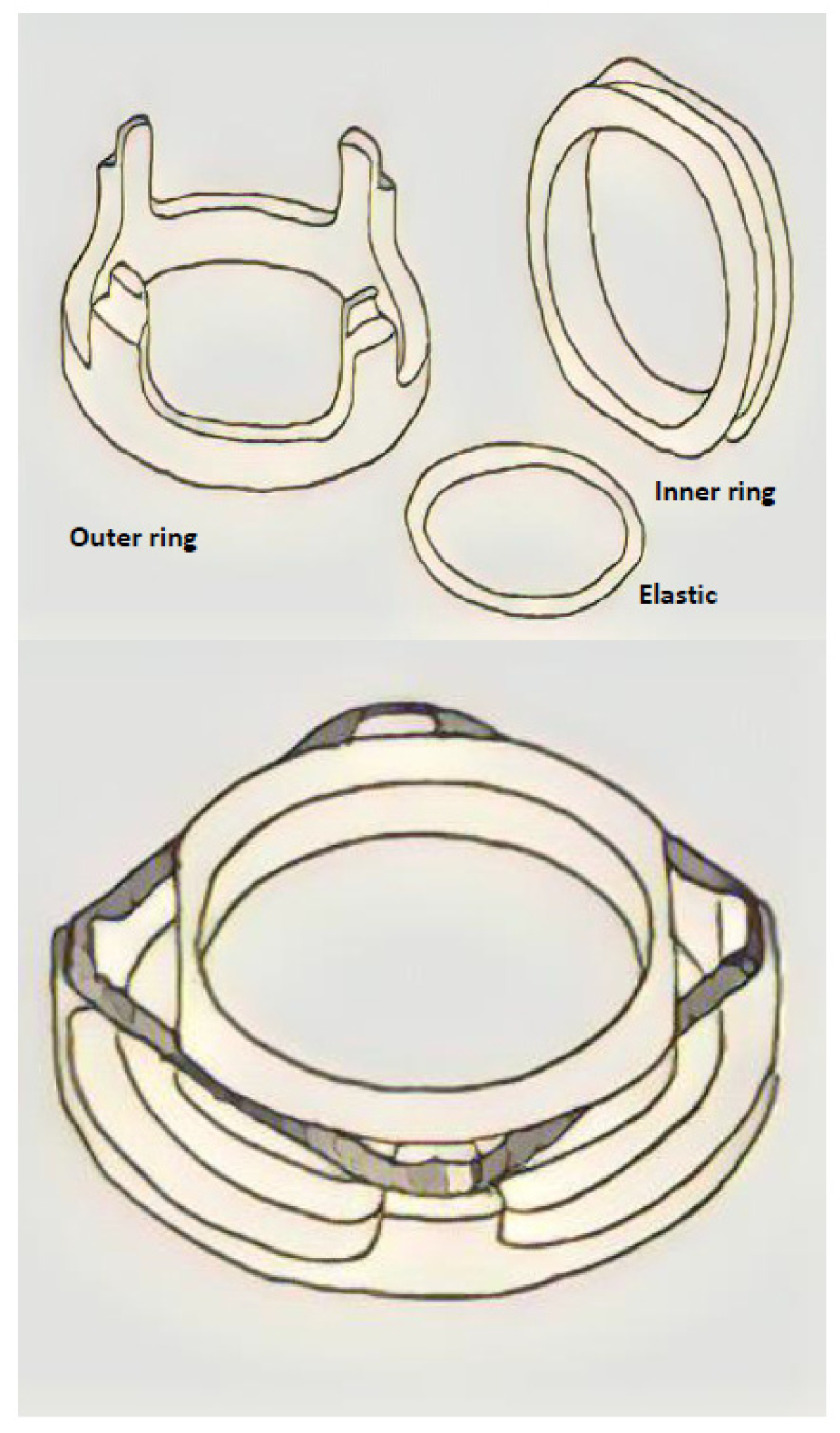
3.4.3. The Shang Ring™ Device (Figure 7)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Palmer, L.S.; Palmer, J.S. Management of abnormalities of the external genitalia in boys. In CampbellWalsh Urology, 11th ed.; Elsevier: Philadelphia, PA, USA, 2016; Volume 4. [Google Scholar]
- Gairdner, D. The fate of the foreskin, a study of circumcision. Br. Med. J. 1949, 2, 1433–1437. [Google Scholar] [CrossRef]
- Czajkowski, M.; Żawrocki, A.; Czajkowska, K.; Kłącz, J.; Sokołowska-Wojdyło, M.; Biernat, W.; Matuszewski, M. Lichen Sclerosus and Phimosis—Discrepancies between Clinical and Pathological Diagnosis and Its Consequences. Urology 2021, 148, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Korkes, F.; Silva, J.L.; Pompeo, A.C.L. Circumcisions for medical reasons in the Brazilian public health system: Epidemiology and trends. Einstein 2012, 10, 342–346. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Radmayr, C.; Bogaert, G.; Burgu, B.; Castagnetti, M.; O’Kelly, F.; Quaedackers, J.S.L.T.; Rawashdeh, Y.F.; Silay, M.S.; ‘t Hoen, L.A.; Gnech, M.; et al. EAU guidelines on paediatric urology. Eur. Urol. 2022, 40, 589–599. [Google Scholar]
- Carilli, M.; Asimakopoulos, A.D.; Pastore, S.; Germani, S.; Orecchia, L.; Agrò, E.F.; Miano, R. Can circumcision be avoided in adult male with phimosis? Results of the PhimoStop™ prospective trial. Transl. Androl. Urol. 2021, 10, 4152–4160. [Google Scholar] [CrossRef] [PubMed]
- Shabanzadeh, D.M.; Clausen, S.; Maigaard, K.; Fode, M. Male Circumcision Complications—A Systematic Review, Meta-Analysis and Meta-Regression. Urology 2021, 152, 25–34. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Iorio, B.; Vespasiani, G.; Cervelli, V.; Spera, E. Autologous split-thickness skin graft for penile coverage in the treatment of buried (trapped) penis after radical circumcision. BJU Int. 2012, 110, 602–606. [Google Scholar] [CrossRef] [PubMed]
- Krill, A.J.; Palmer, L.S.; Palmer, J.S. Complications of circumcision. Sci. World J. 2011, 11, 2458–2468. [Google Scholar] [CrossRef] [PubMed]
- Abdulwahab-Ahmed, A.; Mungadi, I.A. Techniques of male circumcision. J. Surg. Tech. Case Rep. 2013, 5, 1–7. [Google Scholar] [CrossRef]
- Tsen, H.F.; Morgenstern, H.; Mack, T.; Peters, R.K. Risk factors for penile cancer: Results of a population-based case-control study in Los Angeles County (United States). Cancer Causes Control 2001, 12, 267–277. [Google Scholar] [CrossRef]
- Pedersini, P.; Parolini, F.; Bulotta, A.L.; Alberti, D. ‘Trident’ preputial plasty for phimosis in childhood. J. Pediatr. Urol. 2017, 13, 278.e1–278.e4. [Google Scholar] [CrossRef]
- Benson, M.; Hanna, M.K. Prepuce sparing: Use of Z-plasty for treatment of phimosis and scarred foreskin. J. Pediatr. Urol. 2018, 14, 545.e1–545.e4. [Google Scholar] [CrossRef]
- Peterson, A.C.; Joyner, B.D.; Allen, R.C. Plastibell template circumcision: A new technique. Urology 2001, 58, 603–604. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Xu, A.J.; Mishra, K.; Zhao, L.C. Heineke-Mikulicz Preputioplasty: Surgical Technique and Outcomes. Urology 2022, 166, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Nabavizadeh, B.; Li, K.D.; Hakam, N.; Shaw, N.M.; Leapman, M.S.; Breyer, B.N. Incidence of circumcision among insured adults in the United States. PLoS ONE 2022, 17, e0275207. [Google Scholar] [CrossRef]
- Monarca, C.; Rizzo, M.I.; Quadrini, L.; Sanese, G.; Prezzemoli, G.; Scuderi, N. Prepuce-sparing plasty and simple running suture for phimosis. G. Chir. J. Ital. Surg. Assoc. 2013, 34, 38–41. [Google Scholar]
- Siev, M.; Keheila, M.; Motamedinia, P.; Smith, A. Indications for adult circumcision: A contemporary analysis. Can. J. Urol. 2016, 23, 8204–8208. [Google Scholar]
- Carmine, P.; Mario, F.; Antonio, G.; Vincenzo, M.; Elisa, G.; Angelo, C.; Gorizio, P.; Sara, I. Circumferential dissection of deep fascia as ancillary technique in circumcision: Is it possible to correct phimosis increasing penis size? BMC Urol. 2021, 21, 15. [Google Scholar] [CrossRef]
- Rajan, P.; McNeill, S.A.; Turner, K.J. Is frenuloplasty worthwhile? A 12-year experience. Ann. R. Coll. Surg. Engl. 2006, 88, 583–584. [Google Scholar] [CrossRef]
- Casabona, F.; Gambelli, I.; Casabona, F.; Santi, P.; Santori, G.; Baldelli, I. Autologous platelet-rich plasma (PRP) in chronic penile lichen sclerosus: The impact on tissue repair and patient quality of life. Int. Urol. Nephrol. 2017, 49, 573–580. [Google Scholar] [CrossRef]
- D’Arcy, F.T.; Jaffry, S.Q. A review of 100 consecutive sutureless child and adult circumcisions. Ir. J. Med. Sci. 2011, 180, 51–53. [Google Scholar] [CrossRef]
- Fink, K.S.; Carson, C.C.; DeVellis, R.F. Adult circumcision outcomes study: Effect on erectile function, penile sensitivity, sexual activity and satisfaction. J. Urol. 2002, 167, 2113–2116. [Google Scholar] [CrossRef]
- Munro, N.P.; Khan, H.; Shaikh, N.A.; Appleyard, I.; Koenig, P. Y-V preputioplasty for adult phimosis: A review of 89 cases. Urology 2008, 72, 918–920. [Google Scholar] [CrossRef] [PubMed]
- Barone, M.; Li, P.; Lee, R.; Ouma, D.; Oundo, M.; Barasa, M.; Oketch, J.; Otiende, P.; Nyangweso, N.; Maina, M.; et al. Simplifying the ShangRing technique for circumcision in boys and men: Use of the no-flip technique with randomization to removal at 7 days versus spontaneous detachment. Asian J. Androl. 2019, 21, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Tian, F.; Jia, Z.; Li, G.; Meng, Z.; Xing, W.; Ding, Y.; Jin, Z.; Kan, Q.; Yang, J. Introducing the QuillTM device for modified sleeve circumcision with subcutaneous suture: A retrospective study of 70 cases. Urol. Int. 2015, 94, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Kigozi, G.; Musoke, R.; Watya, S.; Kighoma, N.; Nkale, J.; Nakafeero, M.; Namuguzi, D.; Serwada, D.; Nalugoda, F.; Sewankambo, N.; et al. The safety and acceptance of the PrePex device for non-surgical adult male circumcision in Rakai, Uganda. A non-randomized observational study. PLoS ONE 2014, 9, e100008. [Google Scholar] [CrossRef] [PubMed]
- Su, Q.; Gao, S.; Chen, J.; Lu, C.; Mao, W.; Wu, X.; Zhang, L.; Zuo, L.; Su, Q.; Gao, S.; et al. A Comparative Study on the Clinical Efficacy of Modified Circumcision and Two Other Types of Circumcision. Urol. J. 2020, 18, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Jasaitienė, D.; Valiukevičienė, S.; Vaitkienė, D.; Jievaltas, M.; Barauskas, V.; Gudinavičienė, I.; Franke, I.; Gollnick, H. Lichen sclerosus et atrophicus in pediatric and adult male patients with congenital and acquired phimosis. Medicina 2008, 44, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wang, Y.; Zheng, J.; Shen, W.; Yan, J.-A.; Ji, H.; Li, X.; Zhang, H.; Zhou, Z. A report of 918 cases of circumcision with the Shang Ring: Comparison between children and adults. Urology 2013, 81, 1058–1063. [Google Scholar] [CrossRef]
- Mu, J.; Fan, L.; Liu, D.; Zhu, D. A Comparative Study on the Efficacy of Four Types of Circumcision for Elderly Males with Redundant Prepuce. Urol. J. 2020, 17, 301–305. [Google Scholar] [CrossRef]
- Shen, J.; Shi, J.; Gao, J.; Wang, N.; Tang, J.; Yu, B.; Wang, W.; Wang, R. A Comparative Study on the Clinical Efficacy of Two Different Disposable Circumcision Suture Devices in Adult Males. Urol. J. 2017, 14, 5013–5017. [Google Scholar] [PubMed]
- Ronchi, P.; Manno, S.; Dell’Atti, L. Technology Meets Tradition: CO2 Laser Circumcision versus Conventional Surgical Technique. Res. Rep. Urol. 2020, 12, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.-L.; Sun, C.-W.; Sun, J.; Shi, G.-F.; Li, H. Subcutaneous tissue-sparing dorsal slit with new marking technique: A novel circumcision method. Medicine 2019, 98, e15322. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Chen, Z.-D.; Lv, B.-D.; Zhang, S.-G.; Zhu, X.-W.; Chen, G.; Chen, M.-F.; Shen, H.-L.; Pei, Z.-J. Disposable circumcision suture device: Clinical effect and patient satisfaction. Asian J. Androl. 2014, 16, 453–456. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Yang, B.; Yu, W.; Han, Y.; Xu, Z.; Chen, H.; Chen, Y.; Dai, Y. Application of a novel disposable suture device in circumcision: A prospective non-randomized controlled study. Int. Urol. Nephrol. 2016, 48, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Xie, D.-W.; Zhou, X.-G.; Zhang, X.-D. Novel penile circumcision suturing devices versus the shang ring for adult male circumcision: A prospective study. Int. Braz. J. Urol. 2017, 43, 736–745. [Google Scholar] [CrossRef]
- Wei, Q.; Zhu, Y.-C.; Lei, J.-H.; Liu, L.-R.; Xue, W.-B.; Song, T.-R.; Yan, S.-B.; Yang, L.; Han, P. Circumcision with ‘no-flip Shang Ring’ and ‘Dorsal Slit’ methods for adult males: A single-centered, prospective, clinical study. Asian J. Androl. 2016, 18, 798–802. [Google Scholar] [CrossRef]
- Jiang, M.; Wang, J.; Zhou, Y.; Xia, S.; Zhu, Z.; Jia, L.; Liu, Y. Safety and efficacy of a novel disposable circumcision device: A pilot randomized controlled clinical trial at 2 centers. Med. Sci. Monit. 2014, 20, 454–462. [Google Scholar] [CrossRef]
- Malone, P.; Steinbrecher, H. Medical aspects of male circumcision. BMJ 2007, 335, 1206–1290. [Google Scholar] [CrossRef]
- Chi, C.-C.; Kirtschig, G.; Baldo, M.; Brackenbury, F.; Lewis, F.; Wojnarowska, F. Topical interventions for genital lichen sclerosus. Cochrane Database Syst. Rev. 2011, 2011, CD008240. [Google Scholar] [CrossRef]
- Xu, Y.; Li, F.; Li, Z.; Guan, W.; Wu, Y.; Ouyang, Y.; Zhao, Y.; Liu, C. A Prospective, Randomized Controlled Trial of Circumcision in Adult Males Using the CO2 Laser: Modified Technique Compared with the Conventional Dorsal-Slit Technique. Photomed. Laser Surg. 2013, 31, 422–427. [Google Scholar] [CrossRef]
- Millard, P.S.; Wilson, H.R.; Veldkamp, P.J.; Sitoe, N. Rapid, minimally invasive adult voluntary male circumcision: A randomised trial. S. Afr. Med. J. 2013, 103, 736. [Google Scholar] [CrossRef] [PubMed]
- Neill, S.M.; Lewis, F.M.; Tatnall, F.M.; Cox, N.H.; British Association of Dermatologists. British Association of Dermatologists’ guidelines for the management of lichen sclerosus 2010. Br. J. Dermatol. 2010, 163, 672–682. [Google Scholar] [CrossRef]
- Moreno, G.; Corbalán, J.; Peñaloza, B.; Pantoja, T. Topical corticosteroids for treating phimosis in boys. Cochrane Database Syst. Rev. 2014, 2014, CD008973. [Google Scholar] [CrossRef]
- Liu, J.; Yang, J.; Chen, Y.; Cheng, S.; Xia, C.; Deng, T. Is steroids therapy effective in treating phimosis? A meta-analysis. Int. Urol. Nephrol. 2016, 48, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Kikiros, C.S.; Beasley, S.W.; Woodward, A.A. The response of phimosis to local steroid application. Pediatr. Surg. Int. 1993, 8, 329–332. [Google Scholar] [CrossRef]
- Totaro, A.; Volpe, A.; Racioppi, M.; Pinto, F.; Sacco, E.; Bassi, P.F. Circumcision: History, religion and law. Urologia 2011, 78, 1–9. [Google Scholar] [CrossRef]
- Hohlfeld, A.; Ebrahim, S.; Shaik, M.Z.; Kredo, T. Circumcision devices versus standard surgical techniques in adolescent and adult male circumcisions. Cochrane Database Syst. Rev. 2021, 31, CD012250. [Google Scholar] [CrossRef]
- Shikanov, S.; Wille, M.; Large, M.; Lifshitz, D.A.; Zorn, K.C.; Shalhav, A.L.; Eggener, S.E. Knotless Closure of the Collecting System and Renal Parenchyma with a Novel Barbed Suture during Laparoscopic Porcine Partial Nephrectomy. J. Endourol. 2009, 23, 1157–1160. [Google Scholar] [CrossRef]
- Elmasalme, F.N.; Matbouli, S.A.; Zuberi, M.S. Use of tissue adhesive in the closure of small incisions and lacerations. J. Pediatr. Surg. 1995, 30, 837–838. [Google Scholar] [CrossRef] [PubMed]
- Morris, B.J.; Krieger, J.N. The Contrasting Evidence Concerning the Effect of Male Circumcision on Sexual Function, Sensation, and Pleasure: A Systematic Review. Sex. Med. 2020, 8, 577–598. [Google Scholar] [CrossRef] [PubMed]
- Czajkowski, M.; Czajkowska, K.; Zarańska, K.; Giemza, A.; Kłącz, J.; Sokołowska-Wojdyło, M.; Matuszewski, M. Male Circumcision Due to Phimosis as the Procedure That Is Not Only Relieving Clinical Symptoms of Phimosis But Also Improves the Quality of Sexual Life. Sex. Med. 2021, 9, 100315. [Google Scholar] [CrossRef] [PubMed]
- Osmonov, D.; Hamann, C.; Eraky, A.; Kalz, A.; Melchior, D.; Bergholz, R.; Romero-Otero, J. Preputioplasty as a surgical alternative in treatment of phimosis. Int. J. Impot. Res. 2022, 34, 353–358. [Google Scholar] [CrossRef]
- Harahap, M.; Siregar, A.S. Circumcision: A review and a new technique. J. Dermatol. Surg. Oncol. 1988, 14, 383–386. [Google Scholar] [CrossRef]
- Mutabazi, V.; Kaplan, S.A.; Rwamasirabo, E.; Bitega, J.P.; Ngeruka, M.L.; Savio, D.; Karema, C.; Binagwaho, A. One-arm, open-label, prospective, cohort field study to assess the safety and efficacy of the PrePex device for scale-up of nonsurgical circumcision when performed by nurses in resource-limited settings for HIV prevention. J. Acquir. Immune Defic. Syndr. 2013, 63, 315–322. [Google Scholar] [CrossRef]

| Treatment | Advantage/Disadvantage | Side Effects |
|---|---|---|
| Phimostop™ [6] | Shaped silicone tuboids of increasing size to obtain a non-forced dilation of the prepuce | Scarce: discomfort with larger tuboid size |
| Platelet-rich plasma (PRP) [22] | Reduction/disappearance of symptoms and/or of lichen sclerosus | Risk of malignant disease (actually no study demonstrates that PRP promotes hyperplasia, carcinogenesis, or tumor growth) |
| Topical corticosteroids [47] | Complete or partial clinical resolution of phimosis (long-term follow-up not available) | These drugs could induce skin atrophy, telangiectasia and immunosuppression (increasing the risk of malignancy) |
| Potency | Topical Corticosteroids |
|---|---|
| Very potent | Clobetasol propionate 0.05% Diflucortolone valerate 0.3% |
| Potent | Bethametasone dipropionate 0.05% to 0.064% Bethametasone valerate 0.1% to 0.12% Diflucortolone valerato 0.1% Hydrocortisone butyrate 0.1% Mometasone furoate 0.1% Triamcinolone acetonide 0.1% |
| Moderate | Betamethasone valerate 0.025% Clobetasone butyrate 0.05% |
| Mild | Hydrocortisone 0.1% to 2.5% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosato, E.; Miano, R.; Germani, S.; Asimakopoulos, A.D. Phimosis in Adults: Narrative Review of the New Available Devices and the Standard Treatments. Clin. Pract. 2024, 14, 361-376. https://doi.org/10.3390/clinpract14010028
Rosato E, Miano R, Germani S, Asimakopoulos AD. Phimosis in Adults: Narrative Review of the New Available Devices and the Standard Treatments. Clinics and Practice. 2024; 14(1):361-376. https://doi.org/10.3390/clinpract14010028
Chicago/Turabian StyleRosato, Eleonora, Roberto Miano, Stefano Germani, and Anastasios D. Asimakopoulos. 2024. "Phimosis in Adults: Narrative Review of the New Available Devices and the Standard Treatments" Clinics and Practice 14, no. 1: 361-376. https://doi.org/10.3390/clinpract14010028
APA StyleRosato, E., Miano, R., Germani, S., & Asimakopoulos, A. D. (2024). Phimosis in Adults: Narrative Review of the New Available Devices and the Standard Treatments. Clinics and Practice, 14(1), 361-376. https://doi.org/10.3390/clinpract14010028






