Integrated Behavior Therapy for Exclusively Anxious Selective Mutism: A Nonconcurrent Multiple-Baseline Design across Five Participants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.2.1. Recruitment and Consent/Assent Procedures
2.2.2. Baseline Phase
2.2.3. Treatment Phase
2.2.4. Project Personnel
2.3. Measures
2.3.1. Treatment Adherence
2.3.2. Baseline to End-of-Treatment Measures
2.3.3. The Rule-Out Assessment
2.3.4. The Social Anxiety Scale for Children—Revised (SASC-R)
2.3.5. The Selective Mutism Questionnaire
2.3.6. The Anxiety Disorders Interview Schedule (ADIS-P)
2.3.7. The Screen for Child Anxiety Related Disorders (SCARED)
2.4. Multiple-Baseline Measures
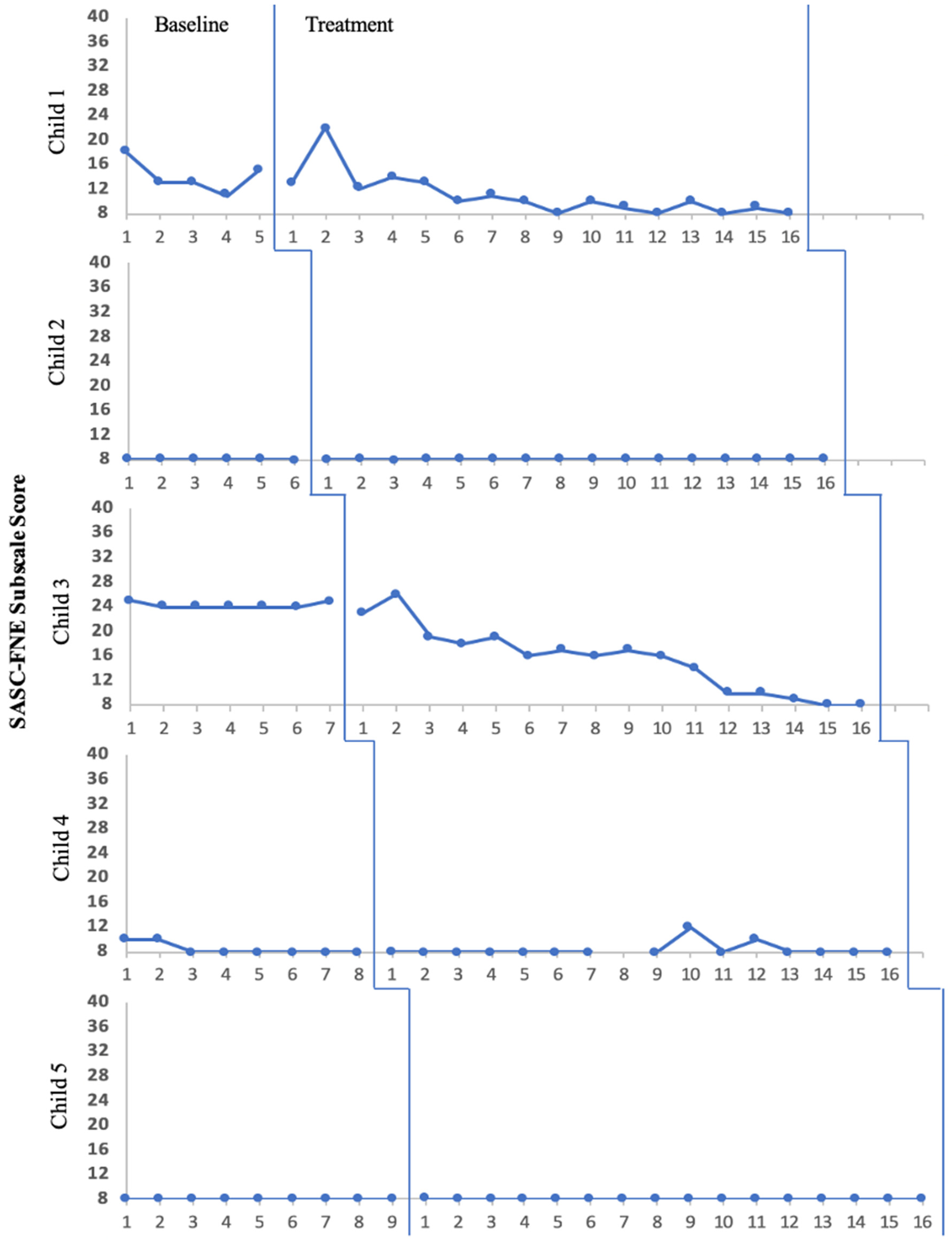
2.4.1. Social Anxiety
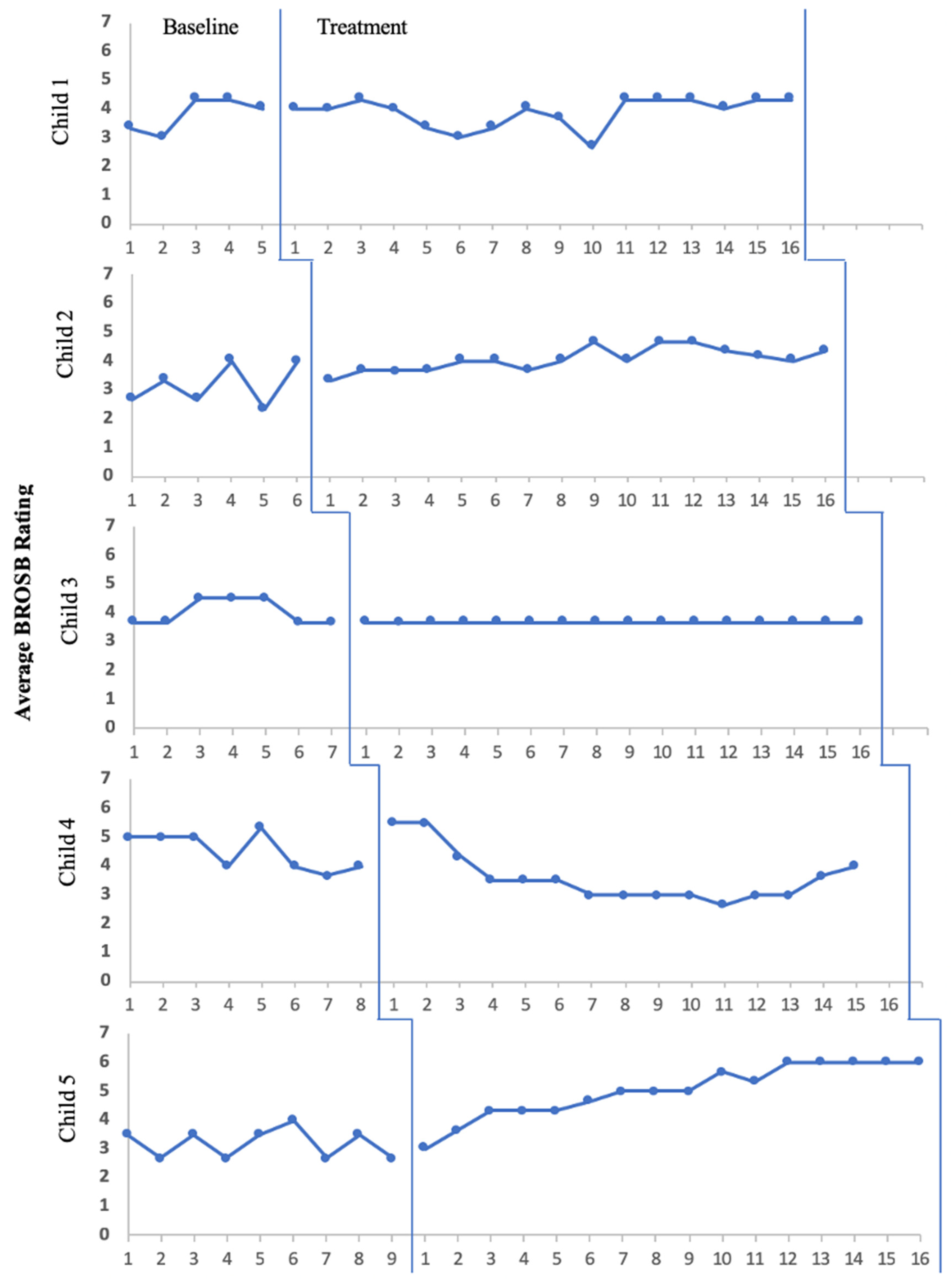
2.4.2. Observed Speaking Behaviors
2.4.3. Treatment Acceptability
2.5. Data Analyses
2.5.1. Treatment Adherence
2.5.2. Treatment Effectiveness
2.5.3. Baseline to End-of-Treatment Measures
2.5.4. Treatment Acceptability
3. Results
3.1. Treatment Adherence
3.2. Treatment Effectiveness
3.2.1. Multiple-Baseline Measures
3.2.2. Baseline to End-of-Treatment Measures
3.3. Treatment Acceptability
4. Discussion
5. Limitations
6. Implications for Research
7. Implications for Practice
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Muris, P.; Ollendick, T.H. Current challenges in the diagnosis and management of selective mutism in children. Psychol. Res. Behav. Manag. 2021, 14, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Ford, M.; Sladeczek, I.; Carlson, J.; Kratochwill, T. Selective mutism: Phenomenological characteristics. Sch. Psychol. Q. 1998, 13, 192–227. [Google Scholar] [CrossRef]
- Steinhausen, H.; Juzi, C. Elective mutism: An analysis of 100 cases. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 606. [Google Scholar] [CrossRef]
- Milic, M.I.; Carl, T.; Rapee, R.M. Similarities and differences between young children with selective mutism and social anxiety disorder. Behav. Res. Ther. 2020; advance online publication. [Google Scholar] [CrossRef]
- Schwenck, C.; Gensthaler, A.; Vogel, F.; Pfeffermann, A.; Laerum, S.; Stahl, J. Characteristics of person, place, and activity that trigger failure to speak in children with selective mutism. Eur. Child Adolesc. Psychiatry, 2021; advance online publication. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Lang, C.; Nir, Z.; Gothelf, A.; Domachevsky, S.; Ginton, L.; Kushnir, J.; Gothelf, D. The outcome of children with selective mutism following cognitive behavioral intervention: A follow-up study. Eur. J. Pediatr. 2016, 175, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Ostergaard, K.R. Treatment of selective mutism based on cognitive behavioural therapy, psychopharmacology and combination therapy: A systematic review. Nord. J. Psychiatry 2018, 72, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Steains, S.Y.; Malouff, J.M.; Schutte, N.S. Efficacy of psychological interventions for selective mutism in children: A meta-analysis of randomized controlled trials. Child Care Health Dev. 2020, 47, 771–781. [Google Scholar] [CrossRef]
- Bergman, R.L. Treatment for Children with Selective Mutism: An Integrative Behavioral Approach; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Kotrba, A. Selective Mutism: An Assessment and Intervention Guide for Therapists, Educators & Parents; PESI Publishing & Media: Eau Claire, WI, USA, 2015. [Google Scholar]
- Zakszeski, B.N.; DuPaul, G.J. Reinforce, shape, expose, and fade: A review of treatments for selective mutism (2005–2015). Sch. Ment. Health 2017, 9, 1–15. [Google Scholar] [CrossRef]
- Kearney, C.A.; Rede, M. The heterogeneity of selective mutism: A primer for a more refined approach. Front. Psychol. 2021, 12, 2251. [Google Scholar] [CrossRef]
- Bergman, R.L.; Gonzalez, A.; Piacentini, J.; Keller, M.L. Integrated Behavior Therapy for Selective Mutism: A randomized controlled pilot study. Behav. Res. Ther. 2013, 51, 680–689. [Google Scholar] [CrossRef]
- Siroky, A.K.; Carlson, J.S.; Kotrba, A. Investigation of Integrated Behavior Therapy for Selective Mutism: A replicated single-case study design. Int. J. Psychol. Stud. 2017, 9, 82–88. [Google Scholar] [CrossRef]
- Khan, M.; Renk, K. Be your own superhero: A case of a young boy with selective mutism and complex comorbidities. Clin. Case Stud. 2018, 17, 348–365. [Google Scholar] [CrossRef]
- Cohan, S.L.; Chavira, D.A.; Shipon-Blum, E.; Hitchcock, C.; Roesch, S.C.; Stein, M.B. Refining the classification of children with selective mutism: A latent profile analysis. J. Clin. Child Adolesc. Psychol. 2008, 37, 770–784. [Google Scholar] [CrossRef] [PubMed]
- Chorpita, B.F.; Daleiden, E.L.; Weisz, J.R. Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Ment. Health Serv. Res. 2005, 7, 5–20. [Google Scholar] [CrossRef] [PubMed]
- Chorpita, B.F.; Daleiden, E.L.; Ebesutani, C.; Young, J.; Becker, K.D.; Nakamura, B.J.; Phillips, L.; Ward, A.; Lynch, R.; Trent, L.; et al. Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clin. Psychol. Sci. Pract. 2011, 18, 154–172. [Google Scholar] [CrossRef]
- Bergman, R.L.; Keller, M.L.; Piacentini, J.; Bergman, A.J. The development and psychometric properties of the selective mutism questionnaire. J. Clin. Child Adolesc. Psychol. 2008, 37, 456–464. [Google Scholar] [CrossRef] [PubMed]
- La Greca, A.M.; Stone, W.L. The social anxiety scale for children-revised: Factor structure and concurrent validity. J. Clin. Child Psychol. 1993, 22, 17–27. [Google Scholar] [CrossRef]
- La Greca, A.M. Social Anxiety Scales for Children and Adolescents: Manual and Instructions for the SASC, SASC-R, SAS-S (Adolescents), and Parent Versions of the Scales; University of Miami: Miami, FL, USA, 1999. [Google Scholar]
- Silverman, W.K.; Albano, A.M. Anxiety Disorders Interview Schedule for DSM-IV: Parent Interview Schedule; Oxford University Press: Oxford, UK, 1996; Volume 1. [Google Scholar]
- Silverman, W.K.; Saavedra, L.M.; Pina, A.A. Test-retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: Child and parent versions. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 937–944. [Google Scholar] [CrossRef] [PubMed]
- Wood, J.J.; Piacentini, J.C.; Bergman, R.L.; McCracken, J.; Barrios, V. Concurrent validity of the anxiety disorders section of the anxiety disorders interview schedule for DSM-IV: Child and parent versions. J. Clin. Child Adolesc. Psychol. 2002, 31, 335–342. [Google Scholar] [CrossRef]
- Birmaher, B.; Brent, D.A.; Chiappetta, L.; Bridge, J.; Monga, S.; Baugher, M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 1230–1236. [Google Scholar] [CrossRef]
- Ginsburg, G.S.; La Greca, A.M.; Silverman, S.K. Social anxiety in children with anxiety disorders: Relation with social and emotional functioning. J. Abnorm. Child Psychol. 1998, 26, 175–185. [Google Scholar] [CrossRef]
- Chafouleas, S.; Riley-Tillman, T.; Christ, T. Direct behavior rating (DBR): An emerging method for assessing social behavior within a tiered intervention system. Assess. Eff. Instr. 2009, 34, 195–200. [Google Scholar] [CrossRef]
- Kelley, M.L.; Heffer, R.W.; Gresham, F.M.; Elliott, S.N. Development of a modified treatment evaluation inventory. J. Psychopathol. Behav. Assess. 1989, 11, 235–247. [Google Scholar] [CrossRef]
- Kazdin, A.E. Acceptability of alternative treatments for deviant child behavior. J. Appl. Behav. Anal. 1980, 13, 259–273. [Google Scholar] [CrossRef]
- Kratochwill, T.R.; Hitchcock, J.H.; Horner, R.H.; Levin, J.R.; Odom, S.L.; Rindskopf, D.M.; Shadish, W.R. Single-case intervention research design standards. Remedial Spec. Educ. 2012, 34, 26–38. [Google Scholar] [CrossRef]
- Vannest, K.J.; Parker, R.I.; Gonen, O.; Adiguzel, T. Single Case Research: Web Based Calculators for SCR Analysis (Version 2.0) [Web-Based Application]. 2016. Available online: singlecaseresearch.org (accessed on 5 April 2019).
- Bruni, T.P.; Drevon, D.; Hixson, M.; Wyse, R.; Corcoran, S.; Fursa, S. The effect of functional behavior assessment on school-based interventions: A meta-analysis of single-case research. Psychol. Sch. 2017, 54, 351–369. [Google Scholar] [CrossRef]
- Jacobson, N.S.; Truax, P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Kratochwill, T.R.; Elliott, S.N.; Loitz, P.A.; Sladeczek, I.; Carlson, J.S. Conjoint consultation using self-administered manual and videotape parent-teacher training: Effects on children’s behavioral difficulties. Sch. Psychol. Q. 2003, 18, 269–302. [Google Scholar] [CrossRef]
- Skedgell, K.K.; Fornander, M.; Kearney, C.A. Personalized individual and group therapy for multifaceted selective mutism. Clin. Case Stud. 2017, 16, 166–181. [Google Scholar] [CrossRef]
- Wergeland, G.J.H.; Fjermestad, K.W.; Marin, C.E.; Bjelland, I.; Haugland, B.S.M.; Silverman, W.K.; Öst, L.G.; Bjaastad, J.F.; Oeding, K.; Havik, O.E.; et al. Predictors of treatment outcome in an effectiveness trial of cognitive behavioral therapy for children with anxiety disorders. Behav. Res. Ther. 2016, 76, 1–12. [Google Scholar] [CrossRef]
- Christ, T.J.; Riley-Tillman, T.C.; Chafouleas, S.M. Foundation for the development and use of direct behavior rating (DBR) to assess and evaluate student behavior. Assess. Eff. Interv. 2009, 34, 201–213. [Google Scholar] [CrossRef]
- Volpe, R.J.; Briesch, A.M. Generalizability and dependability of single-item and multiple-item direct behavior rating scales for engagement and disruptive behavior. Sch. Psychol. Rev. 2012, 41, 246. [Google Scholar] [CrossRef]
- Gensthaler, A.; Dieter, J.; Raisig, S.; Hartmann, B.; Ligges, M.; Kaess, M.; Freitag, C.M.; Schwenck, C. Evaluation of a novel parent-rated scale for selective mutism. Assessment 2020, 27, 1007–1015. [Google Scholar] [CrossRef]
- Xu, H.Y.; Stroud, J.; Jozanovic, R.K.; Clucas, J.; Son, J.J.; Koo, B.; Schwarz, J.; Klein, A.; Busman, R.; Milham, M.P. Clinical perspective on passive audio vocal measurement in the evaluation of selective mutism. Psychiatry 2018, 9, 443. [Google Scholar] [CrossRef]
| Age | Sex | Race | ADIS-P, Clinical Severity Rating (CSR) | SMQ | ||||
|---|---|---|---|---|---|---|---|---|
| Selective Mutism | Social Phobia | GAD | Separation Anxiety | Total Score at Baseline | ||||
| Child 1 | 8 | M | Biracial | 8 | 8 | 5 | 5 | 16 |
| Child 2 | 7 | M | Caucasian | 8 | 5 | n/a | n/a | 13 |
| Child 3 | 6 | F | Caucasian | 4 | n/a | n/a | n/a | 17 |
| Child 4 | 6 | M | Caucasian | 6 | 6 | 7 | n/a | 16 |
| Child 5 | 4 | F | Caucasian | 7 | n/a | n/a | n/a | 15 |
| IBTSM Sessions (24 Weeks, 20 Treatment Sessions Total) | Condensed IBTSM Sessions (M = 19 Weeks, 16 Treatment Sessions) | ||
|---|---|---|---|
| Pre-treatment (Parent Only) | Assessment and Psychoeducation | Pre-treatment Intake Session | Assessment and Psychoeducation |
| Session 1 | Introduction, Rapport Building | Session 1 | Introduction, Rapport Building |
| Session 2 | Rapport Building, Reward System, Feelings Chart | Session 2 | Rapport Building, Reward System, Feelings Chart |
| Session 3 | Classroom Chart, Fear Ladder, Exposure Practice | Session 3 | Classroom Chart, Fear Ladder, Exposure Practice |
| Sessions 4–9 | Initial Exposure Sessions | Sessions 4–7 | Initial Exposure Sessions |
| Session 10 | Midpoint Session | Session 8 | Midpoint Session |
| Sessions 11–14 | Intermediate Exposure Sessions | Sessions 9–10 | Intermediate Exposure Sessions |
| Session 15 | Exposure, Introduction to Transfer of Control | Session 11 | Exposure, Introduction to Transfer of Control |
| Sessions 16–17 | Exposure, Additional Transfer of Control | Sessions 12–13 | Exposure, Additional Transfer of Control |
| Sessions 18–19 | Exposure, Transfer of Control, Progress Review | Sessions 14–15 | Exposure, Transfer of Control, Progress Review |
| Session 20 | Relapse Prevention and Graduation | Session 16 | Relapse Prevention and Graduation |
| Study Phase | Assessment Plan | Variable |
|---|---|---|
| Intake | Behavioral Concerns Inventory | Clinical profile of SM |
| Clinical Intake Interview with Developmental and Medical History | ||
| Social Anxiety Scale for Children—Parent Version (Full scale) | Social anxiety severity | |
| Selective Mutism Questionnaire (Full scale) | SM symptom severity | |
| Anxiety Disorders Interview Schedule for Children—Parent Interview Screen for Child Anxiety Related Disorders—Parent Version | Clinical diagnoses | |
| Baseline/ Treatment | Once weekly: Analog observations | Words spoken |
| Once weekly: Session checklists | Treatment adherence | |
| Daily during baseline, Weekly during treatment: Social Anxiety Scale for Children—Parent Form (FNE subscale) | Caregiver-reported social anxiety levels | |
| Daily during baseline, Weekly during treatment: Brief Ratings of Observed Speaking Behaviors | Caregiver-reported speaking behaviors across contexts | |
| Four times per case: Direct observation of treating clinicians | Treatment adherence (inter-observer agreement) | |
| End of treatment | Treatment Evaluation Questionnaire Social Anxiety Scale for Children—Parent Version (Full scale) Selective Mutism Questionnaire (Full scale) Anxiety Disorders Interview Schedule for Children—Parent Interview Screen for Child Anxiety Related Disorders—Parent Version | Treatment acceptability Social anxiety severity SM symptom severity Clinical diagnoses |
| Measure/Child | Baseline | End of Treatment | RCI | |
|---|---|---|---|---|
| SASC-R Total Score | ||||
| Child 1 | 58 | 33 | −7.99 * | |
| Child 2 | 56 | 51 | −1.60 | |
| Child 3 | 64 | 27 | −11.82 * | |
| Child 4 | 46 | 39 | −2.24 * | |
| Child 5 | 67 | 35 | −10.22 * | |
| Average (SD) | 58.20 (8.14) | 37.00 (8.94) | −6.71 * | |
| SCARED Total Score | ||||
| Child 1 | 35 | 15 | −4.29 * | |
| Child 2 | 27 | 19 | −1.72 * | |
| Child 3 | 40 | 17 | −4.93 * | |
| Child 4 | 35 | 23 | −2.57 * | |
| Child 5 | 26 | 17 | −2.57 * | |
| Average (SD) | 32.60 (5.94) | 17.60 (3.58) | −3.22 * | |
| ADIS-P—Social Phobia CSR | ||||
| Child 1 | 8 | n/a | - | |
| Child 2 | 5 | 6 | - | |
| Child 4 | 6 | n/a | - | |
| ADIS-P—GAD CSR | ||||
| Child 1 | 5 | n/a | - | |
| Child 4 | 7 | n/a | - | |
| ADIS-P—Separation Anxiety CSR | ||||
| Child 1 | 5 | n/a | - | |
| Child 4 | n/a | 4 | - | |
| Measure/Child | Baseline | End of Treatment | RCI | |
|---|---|---|---|---|
| SMQ Total Score | ||||
| Child 1 | 16 | 36 | 5.42 * | |
| Child 2 | 13 | 18 | 1.36 | |
| Child 3 | 17 | 24 | 1.90 | |
| Child 4 | 16 | 32 | 4.34 * | |
| Child 5 | 15 | 38 | 6.23 * | |
| Average (SD) | 15.40 (1.52) | 29.60 (8.41) | 3.85 * | |
| ADIS-P—Selective Mutism CSR | ||||
| Child 1 | 8 | n/a | - | |
| Child 2 | 8 | 6 | - | |
| Child 3 | 4 | 4 | - | |
| Child 4 | 6 | n/a | - | |
| Child 5 | 7 | n/a | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siroky, A.K.; Carlson, J.S.; Kotrba, A. Integrated Behavior Therapy for Exclusively Anxious Selective Mutism: A Nonconcurrent Multiple-Baseline Design across Five Participants. Pediatr. Rep. 2023, 15, 617-635. https://doi.org/10.3390/pediatric15040057
Siroky AK, Carlson JS, Kotrba A. Integrated Behavior Therapy for Exclusively Anxious Selective Mutism: A Nonconcurrent Multiple-Baseline Design across Five Participants. Pediatric Reports. 2023; 15(4):617-635. https://doi.org/10.3390/pediatric15040057
Chicago/Turabian StyleSiroky, Allison K., John S. Carlson, and Aimee Kotrba. 2023. "Integrated Behavior Therapy for Exclusively Anxious Selective Mutism: A Nonconcurrent Multiple-Baseline Design across Five Participants" Pediatric Reports 15, no. 4: 617-635. https://doi.org/10.3390/pediatric15040057
APA StyleSiroky, A. K., Carlson, J. S., & Kotrba, A. (2023). Integrated Behavior Therapy for Exclusively Anxious Selective Mutism: A Nonconcurrent Multiple-Baseline Design across Five Participants. Pediatric Reports, 15(4), 617-635. https://doi.org/10.3390/pediatric15040057







