Diagnostic Barriers in Children with Immunodeficiencies in Central Asia: A Case-Based Discussion
Abstract
:1. Introduction
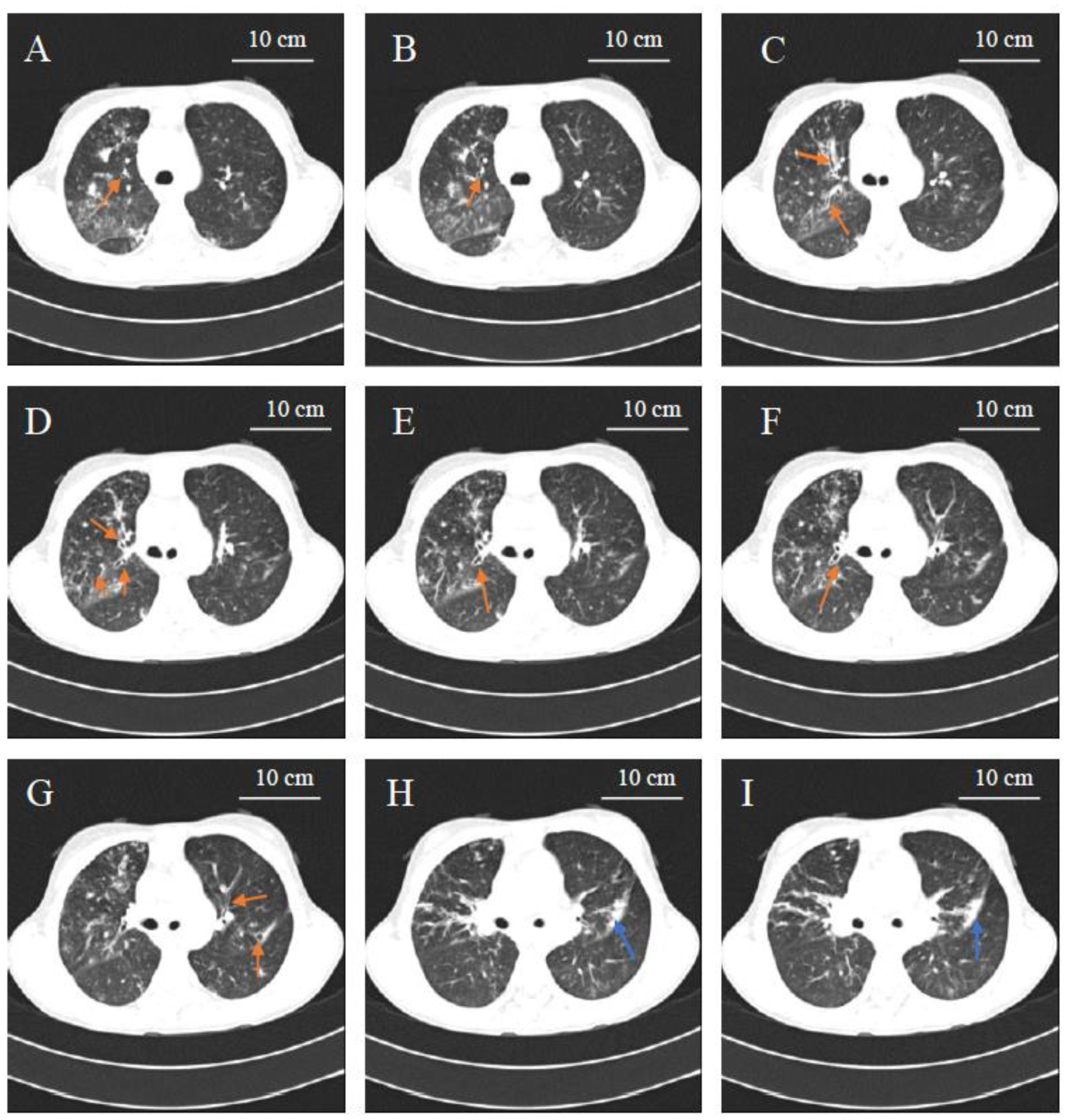
2. Clinical Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chapel, H.; Lucas, M.; Lee, M.; Bjorkander, J.; Webster, D.; Grimbacher, B.; Fieschi, C.; Thon, V.; Abedi, M.R.; Hammarstrom, L. Common variable immunodeficiency disorders: Division into distinct clinical phenotypes. Blood 2008, 112, 277–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abbott, J.K.; Gelfand, E.W. Common variable immunodeficiency: Diagnosis, management, and treatment. Immunol. Allergy Clin. 2015, 35, 637–658. [Google Scholar] [CrossRef]
- Azizi, G.; Abolhassani, H.; Asgardoon, M.H.; Alinia, T.; Yazdani, R.; Mohammadi, J.; Rezaei, N.; Ochs, H.D.; Aghamohammadi, A. Autoimmunity in common variable immunodeficiency: Epidemiology, pathophysiology and management. Expert Rev. Clin. Immunol. 2017, 13, 101–115. [Google Scholar] [CrossRef] [PubMed]
- Lopes, J.P.; Ho, H.E.; Cunningham-Rundles, C. Interstitial lung disease in common variable immunodeficiency. Front. Immunol. 2021, 12, 605945. [Google Scholar] [CrossRef] [PubMed]
- Abolhassani, H.; Hammarstrom, L.; Cunningham-Rundles, C. Current genetic landscape in common variable immune deficiency. Blood 2020, 135, 656–667. [Google Scholar] [CrossRef] [PubMed]
- Bogaert, D.J.; Dullaers, M.; Lambrecht, B.N.; Vermaelen, K.Y.; De Baere, E.; Haerynck, F. Genes associated with common variable immunodeficiency: One diagnosis to rule them all? J. Med. Genet. 2016, 53, 575–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fenando, A.; Tadi, P. Common Variable Hypogammaglobulinemia; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Seidel, M.G.; Kindle, G.; Gathmann, B.; Quinti, I.; Buckland, M.; van Montfrans, J.; Scheible, R.; Rusch, S.; Gasteiger, L.M.; Grimbacher, B.; et al. ESID Registry Working Party and Collaborators. The European Society for Immunodeficiencies (ESID) registry working definitions for the clinical diagnosis of inborn errors of immunity. J. Allergy Clin. Immunol. Pract. 2019, 7, 1763–1770. [Google Scholar] [CrossRef] [PubMed]
- Pilania, R.K.; Chaudhary, H.; Jindal, A.K.; Rawat, A.; Singh, S. Current status and prospects of primary immunodeficiency diseases in Asia. Genes. Dis. 2019, 7, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, R.; Mac Aogáin, M.; Chalmers, J.D.; Elborn, S.J.; Chotirmall, S.H. Geographic variation in the aetiology, epidemiology and microbiology of bronchiectasis. BMC Pulm. Med. 2018, 18, 83. [Google Scholar] [CrossRef] [PubMed]
- Odnoletkova, I.; Kindle, G.; Quinti, I.; Grimbacher, B.; Knerr, V.; Gathmann, B.; Ehl, S.; Mahlaoui, N.; Van Wilder, P.; Bogaerts, K.; et al. Plasma Protein Therapeutics Association (PPTA) Taskforce. The burden of common variable immunodeficiency disorders: A retrospective analysis of the European Society for Immunodeficiency (ESID) registry data. Orphanet. J. Rare Dis. 2018, 13, 201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Modell, V.; Knaus, M.; Modell, F.; Roifman, C.; Orange, J.; Notarangelo, L.D. Global overview of primary immunodeficiencies: A report from Jeffrey Modell Centers worldwide focused on diagnosis, treatment, and discovery. Immunol. Res. 2014, 60, 132–144. [Google Scholar] [CrossRef] [PubMed]
- Mukusheva, Z.; Assylbekova, M.; Poddighe, D. Management of pediatric rheumatic patients in kazakhstan during the coronavirus disease 2019 (COVID-19) Pandemic. Rheumatol Int. 2020, 40, 1351–1352. [Google Scholar] [CrossRef] [PubMed]
- Poddighe, D.; Telman, A.; Tuleutayev, E.; Ibrayeva, A. Pediatric ulcerative colitis in kazakhstan: First case series from central asia and current clinical management. Gastroenterol. Insights 2020, 11, 27–35. [Google Scholar] [CrossRef]
- Poddighe, D.; Turganbekova, A.; Baymukasheva, D.; Saduakas, Z.; Zhanzakova, Z.; Abdrakhmanova, S. Genetic predisposition to celiac disease in Kazakhstan: Potential impact on the clinical practice in Central Asia. PLoS ONE 2020, 15, e0226546. [Google Scholar] [CrossRef] [PubMed]
- Poddighe, D.; Abdukhakimova, D. Celiac disease in Asia beyond the Middle East and Indian subcontinent: Epidemiological burden and diagnostic barriers. World J. Gastroenterol. 2021, 27, 2251–2256. [Google Scholar] [CrossRef] [PubMed]
- Imankulova, K.; Nauryzaliyeva, S.; Bakybayev, D.; Expert Commission on Healthcare Development of the Ministry of Health of the Republic of Kazakhstan. Protocol No. 10: Бронхоэктатическая Болезнь У Детей. 2014. Database: MedElement. Available online: https://diseases.medelement.com/disease/%D0%B1%D1%80%D0%BE%D0%BD%D1%85%D0%BE%D1%8D%D0%BA%D1%82%D0%B0%D1%82%D0%B8%D1%87%D0%B5%D1%81%D0%BA%D0%B0%D1%8F-%D0%B1%D0%BE%D0%BB%D0%B5%D0%B7%D0%BD%D1%8C-%D1%83-%D0%B4%D0%B5%D1%82%D0%B5%D0%B9/13885 (accessed on 28 June 2020).
- Gupta, S.; Pattanaik, D.; Krishnaswamy, G. Common variable immune deficiency and associated complications. Immunotherapy 2019, 14, 1177–1180. [Google Scholar] [CrossRef] [PubMed]
- Cagdas, D.; Pehlivanturk Kyzylkan, M.; Tagiyev, A.; Emiralioglu, N.; Keleæ, A.; Yalcyn, E.; Dogru, D.; OzCelik, U.; Kiper, N.; Tezcan, Y. Primary immunodeficiency disorders in children with Non-Cystic Fibrosis Bronchiectasis. Eur. Ann. Allergy Clin. Immunol. 2020, 52, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.; Cunningham-Rundles, C. Non-infectious complication of common variable immunodeficiency: Updated clinical spectrum, sequelae, and insights to pathogenesis. Front. Immunol. 2020, 11, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moazzami, B.; Mohayeji Nasrabadi, M.A.; Abolhassani, H.; Olbrich, P.; Azizi, G.; Shirzadi, R.; Modaresi, M.; Sohani, M.; Delavari, S.; Shahkarami, S.; et al. Comprehensive assessment of respiratory complications in patients with common variable immunodeficiency. Ann. Allergy Asthma. Immunol. 2020, 124, 505–511. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Result | Units | Reference Range |
|---|---|---|---|
| WBC | 9.84 | 109/L | 4.50–13.00 |
| HGB | 113 | g/L | 115.00–150.00 |
| RBC | 5.27 | 1012/L | 3.80–5.00 |
| MCH | 21.40 | pg | 26.00–34.00 |
| MCHC | 30.80 | g/dL | 31.00–38.00 |
| MCV | 69.60 | fL | 79.00–96.00 |
| PLT | 424.00 | 109/L | 150.00–400.00 |
| MPV | 9.50 | fL | 9.00–13.00 |
| Neutrophils | 58.80 | % | 40.50–71.00 |
| Eosinophils | 3.40 | % | 0.50–6.00 |
| Basophils | 0.40 | % | 0.00–0.50 |
| Lymphocytes | 29.10 | % | 18.00–40.00 |
| Monocytes | 7.80 | % | 2.00–10.00 |
| ESR | 14.00 | mm/h | 2.00–15.00 |
| CRP | 15.86 | mg/dl | 0.00–5.00 |
| Cholesterol | 3.98 | μmol/L | 3.21–5.20 |
| Creatinine | 44.00 | μmol/L | 34.00–65.00 |
| Protein | 64.70 | g/L | 64.00–83.00 |
| ALT | 15.60 | U/L | 0.00–44.00 |
| AST | 10.10 | U/L | 0.00–44.00 |
| Ferritin | 30.30 | μg/L | 15.00–150.00 |
| Parameter | Result | Units | Reference Range |
|---|---|---|---|
| IgA | <0.08 | g/L | 0.47–2.49 |
| IgM | 0.1 | g/L | 0.15–1.88 |
| IgG | 0.85 | g/L | 7.16–17.11 |
| IgE | <1 | IU/mL | <100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dauyey, Z.; Poddighe, D. Diagnostic Barriers in Children with Immunodeficiencies in Central Asia: A Case-Based Discussion. Pediatr. Rep. 2021, 13, 483-489. https://doi.org/10.3390/pediatric13030055
Dauyey Z, Poddighe D. Diagnostic Barriers in Children with Immunodeficiencies in Central Asia: A Case-Based Discussion. Pediatric Reports. 2021; 13(3):483-489. https://doi.org/10.3390/pediatric13030055
Chicago/Turabian StyleDauyey, Zhanna, and Dimitri Poddighe. 2021. "Diagnostic Barriers in Children with Immunodeficiencies in Central Asia: A Case-Based Discussion" Pediatric Reports 13, no. 3: 483-489. https://doi.org/10.3390/pediatric13030055
APA StyleDauyey, Z., & Poddighe, D. (2021). Diagnostic Barriers in Children with Immunodeficiencies in Central Asia: A Case-Based Discussion. Pediatric Reports, 13(3), 483-489. https://doi.org/10.3390/pediatric13030055






