Perineal Groove: Is It More Common Than We Think? Clinical Characteristics of Four Cases and Review of Literature
Abstract
:1. Introduction
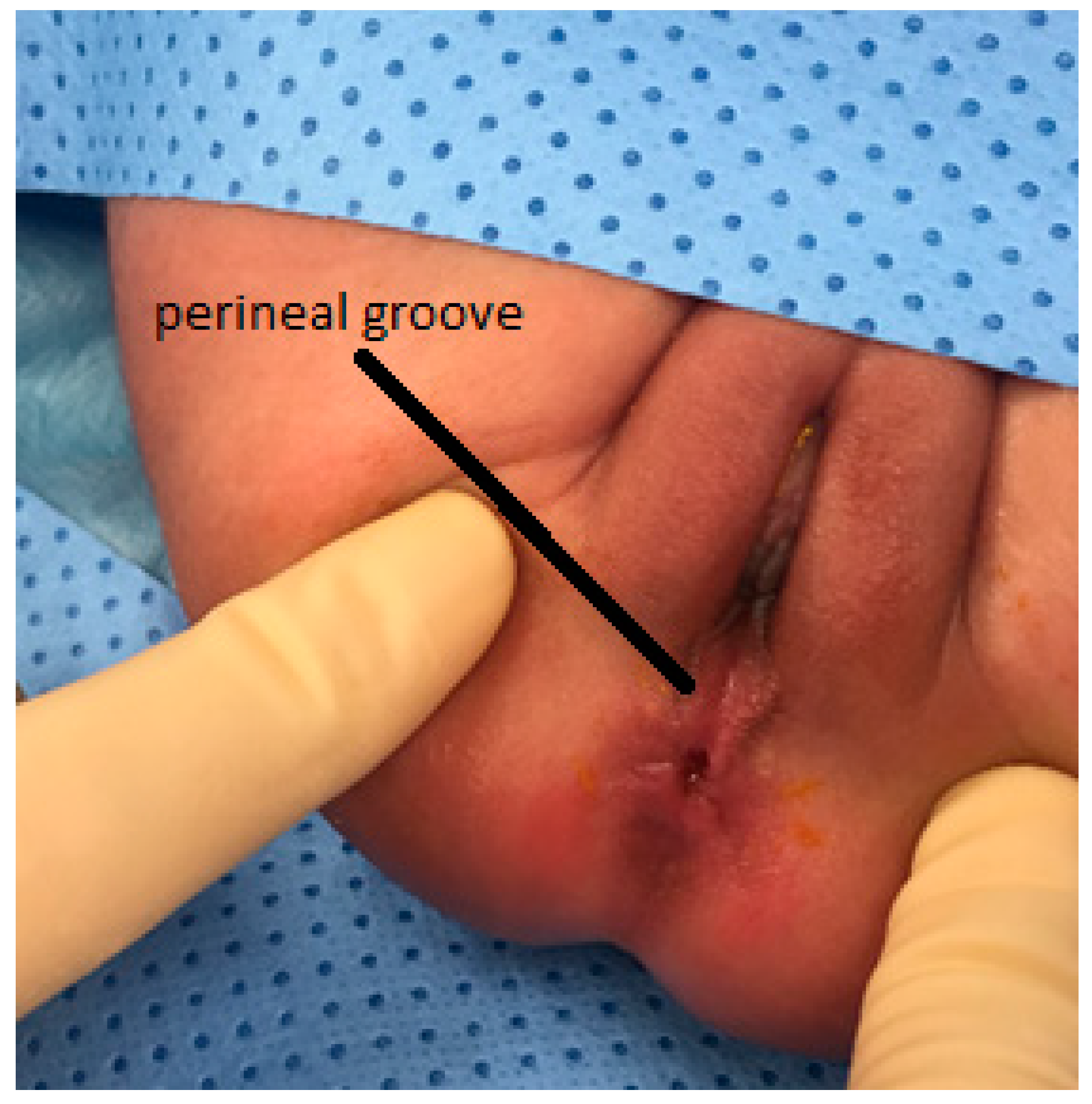
2. Case Presentation and Management
2.1. Case 1
2.2. Case 2
2.3. Case 3
2.4. Case 4
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ihn, K.; Na, Y.; Ho, I.G.; Oh, J.T. Clinical characteristics and conservative treatment of perineal groove. J Pediatr. Surg. 2019, 55, 1507–1510. [Google Scholar] [CrossRef]
- Chatterjee, S.K.; Chatterjee, U.S.; Chatterjee, U. Perineal groove with penoscrotal hypospadias. Pediatr. Surg. Int. 2003, 19, 554–556. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Wang, Z.; Zhao, Q.; Zhu, H.; Xu, T. Perineal Groove: Report of Two Cases and Review of the Literature. Front. Pediatr. 2018, 6, 227. [Google Scholar] [CrossRef] [PubMed]
- Harsono, M.; Pourcyrous, M. Perineal Groove: A Rare Congenital Midline Defect of Perineum. Am. J. Perinatol. Rep. 2016, 6, e30–e32. [Google Scholar]
- Granillo, S.F.; Garone, A.; Molina, T.L.; Luty, G.; Bello, C. Perineal Groove: Report of Three Cases. J. Dermat. 2018, 3, 111. [Google Scholar]
- Boutsikou, T.; Mougiou, V.; Sokou, R.; Kollia, M.; Kafalidis, G.; Iliodromiti, Z.; Salakos, C.; Iacovidu, N. Four Cases of Perineal Groove—Experience of a Greek Maternity Hospital. Medicina 2019, 55, 488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stephens, F.D. The female anus, perineum and vestibule: Embryogenesis and deformities. Aust. N. Z. J. Obstet. Gynaecol. 1968, 8, 55–73. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.B.; Wollina, U. Perineal groove-a case report. Pediatr. Dermatol. 2010, 27, 626–627. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.; Giurin, I.; Savanelli, A.; Alicchio, F.; Settimi, A. Current trends in the management of pediatric patients with perineal groove. J. Pediatr. Adolesc. Gynecol. 2011, 24, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Mullassery, D.; Turnock, R.; Kokai, G. Perineal groove. J. Pediatr. Surg. 2006, 41, e41–e43. [Google Scholar] [CrossRef] [PubMed]
- Aleem, A.A.; El Sheikh, S.; Mokhtar, A.; Ghafouri, H.; Saleem, M. The perineal groove and canal in males and females–a third look. Z. Kinderchir. 1985, 40, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Myers, M.F.; Li, S.; Correa-Villaseñor, A.; Li, Z.; Moore, C.A.; Hong, S.X.; Berry, R.J. Folic Acid Supplementation and Risk for Imperforate Anus in China. Am. J. Epidemiol. 2001, 154, 1051–1056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wijers, C.H.W.; de Blaauw, I.; Zwink, N.; Draaken, Z.; Van der Zanden, L.F.M.; Brunner, H.G.; Brooks, A.S.; Hofstra, R.M.; Sloots, C.E.J.; Broens, P.M.A.; et al. No Major Role for Periconceptional Folic Acid Use and Its Interaction With the MTHFR C677T Polymorphism in the Etiology of Congenital Anorectal Malformations. Birth Defects Res. Part A Clin. Mol. Teratol. 2014, 100, 483–492. [Google Scholar] [CrossRef] [PubMed]

| Case | Age of Patient | Gender | Other Associated Anomalies | Folic Acid Intake during Pregnancy | Mother’s Age and Parity | Follow Up | Outcome |
|---|---|---|---|---|---|---|---|
| One | 7 days | Female | None | None | 26 yo G1P1 | 2 years | Spontaneous resolution |
| Two | 15 days | Female | None | None | 38 yo G3P3 | 18 months | Spontaneous resolution |
| Three | 2 months | Female | Mild VSD closed spontan-eously at 9 months of age | None | 40 yo G2P2 | 18 months | Spontaneous resolution |
| Four | 6 months | Female | None | None | 31 yo G3P2 | 6 months | Under observation |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naji, H.; Ali Hassan, R. Perineal Groove: Is It More Common Than We Think? Clinical Characteristics of Four Cases and Review of Literature. Pediatr. Rep. 2021, 13, 490-494. https://doi.org/10.3390/pediatric13030056
Naji H, Ali Hassan R. Perineal Groove: Is It More Common Than We Think? Clinical Characteristics of Four Cases and Review of Literature. Pediatric Reports. 2021; 13(3):490-494. https://doi.org/10.3390/pediatric13030056
Chicago/Turabian StyleNaji, Hussein, and Rola Ali Hassan. 2021. "Perineal Groove: Is It More Common Than We Think? Clinical Characteristics of Four Cases and Review of Literature" Pediatric Reports 13, no. 3: 490-494. https://doi.org/10.3390/pediatric13030056
APA StyleNaji, H., & Ali Hassan, R. (2021). Perineal Groove: Is It More Common Than We Think? Clinical Characteristics of Four Cases and Review of Literature. Pediatric Reports, 13(3), 490-494. https://doi.org/10.3390/pediatric13030056





