The Effect of Repetitive Transcranial Magnetic Stimulation on Cognition in Diffuse Axonal Injury in a Rat Model
Abstract
1. Introduction
2. Materials and Methods
Experimental Subjects
3. Methods
3.1. DAI Rat Model
3.2. Sample Size Calculation
3.3. Repetitive Transcranial Magnetic Stimulation
3.4. Morris Water Maze Test
3.5. Imaging Study
3.6. Immunohistochemistry
3.7. Western Blot Analysis
3.8. Statistical Analyses
4. Results
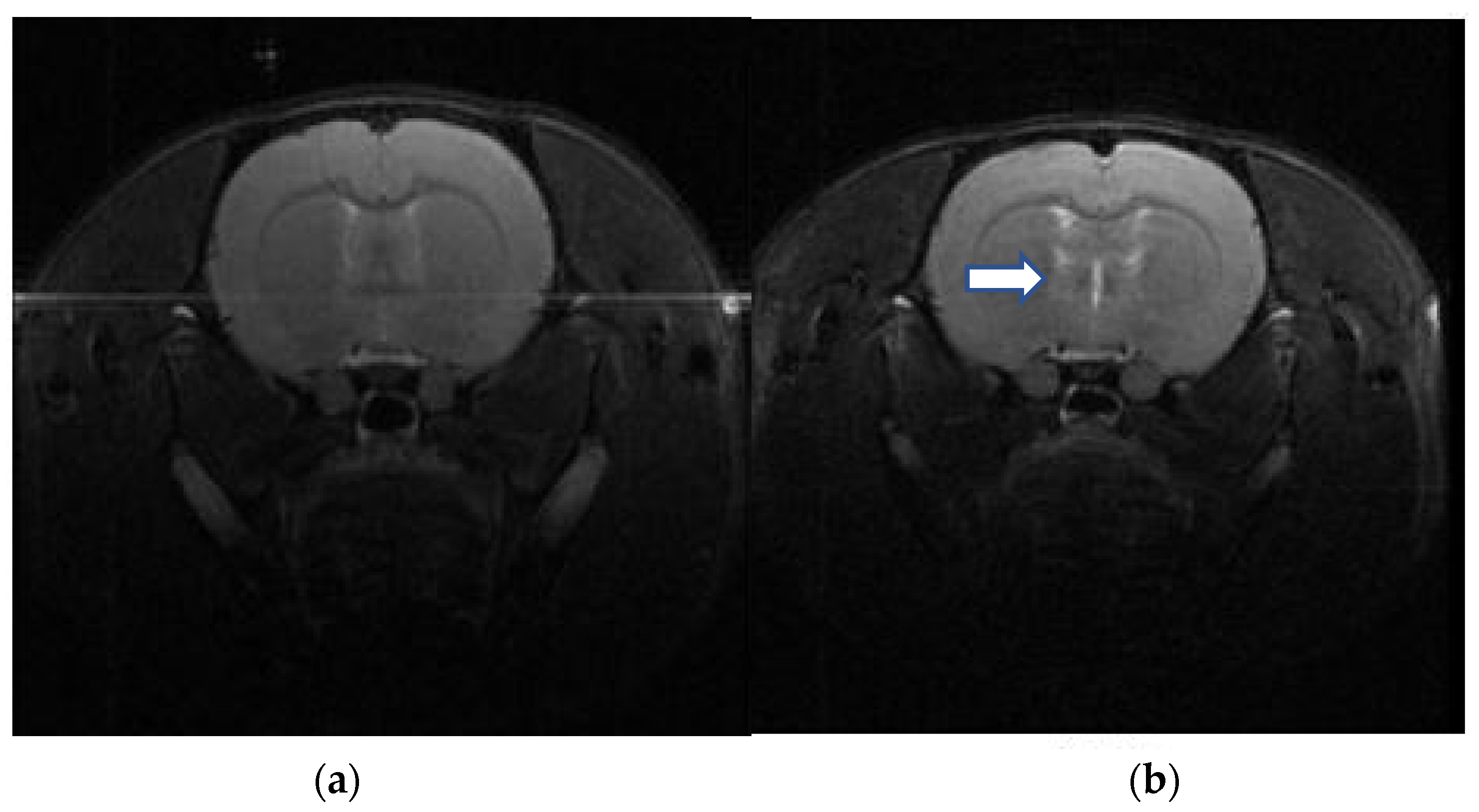
4.1. Imaging Study for DAI
4.2. Behavioral Test
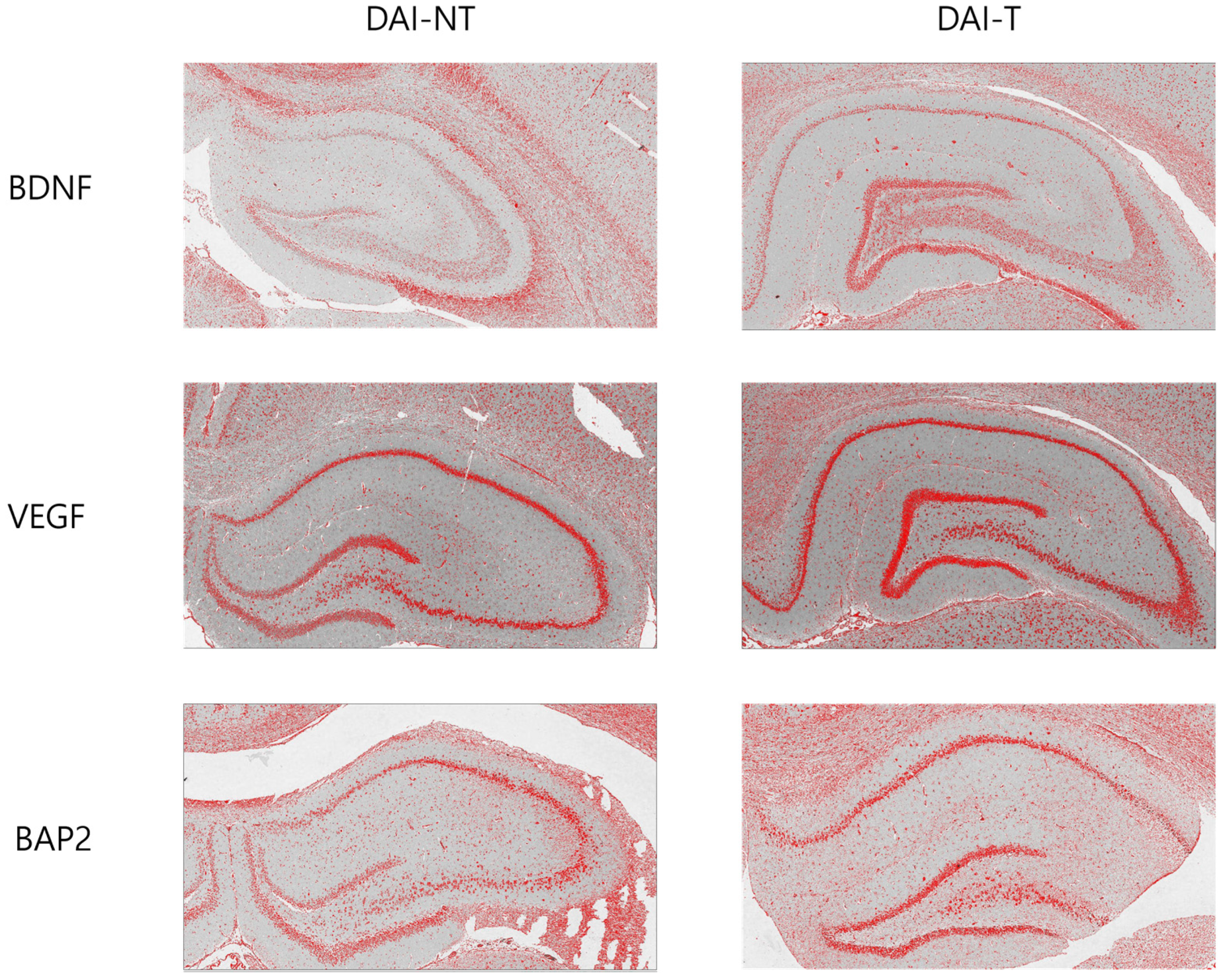
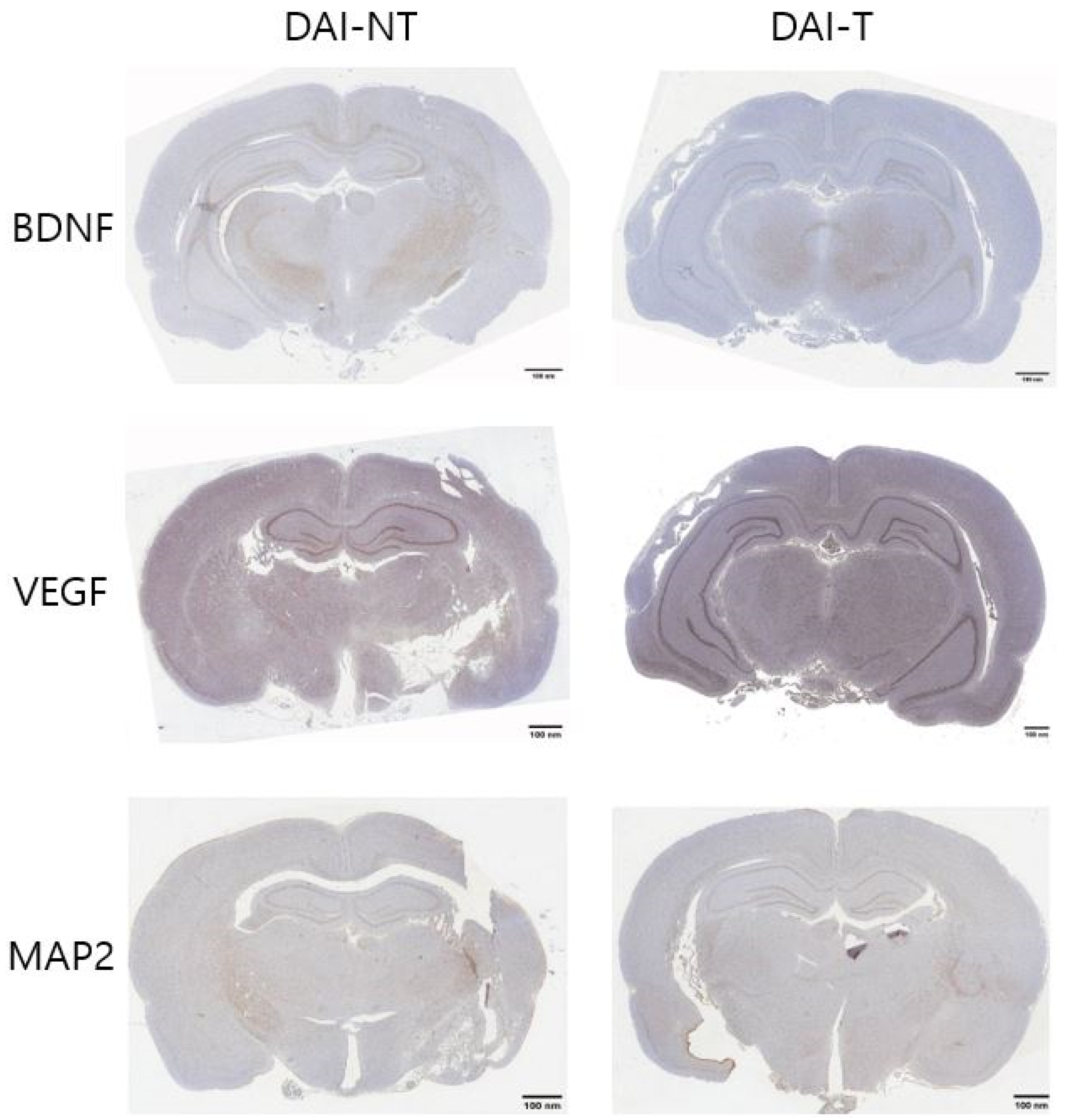
4.3. Immunohistochemistry
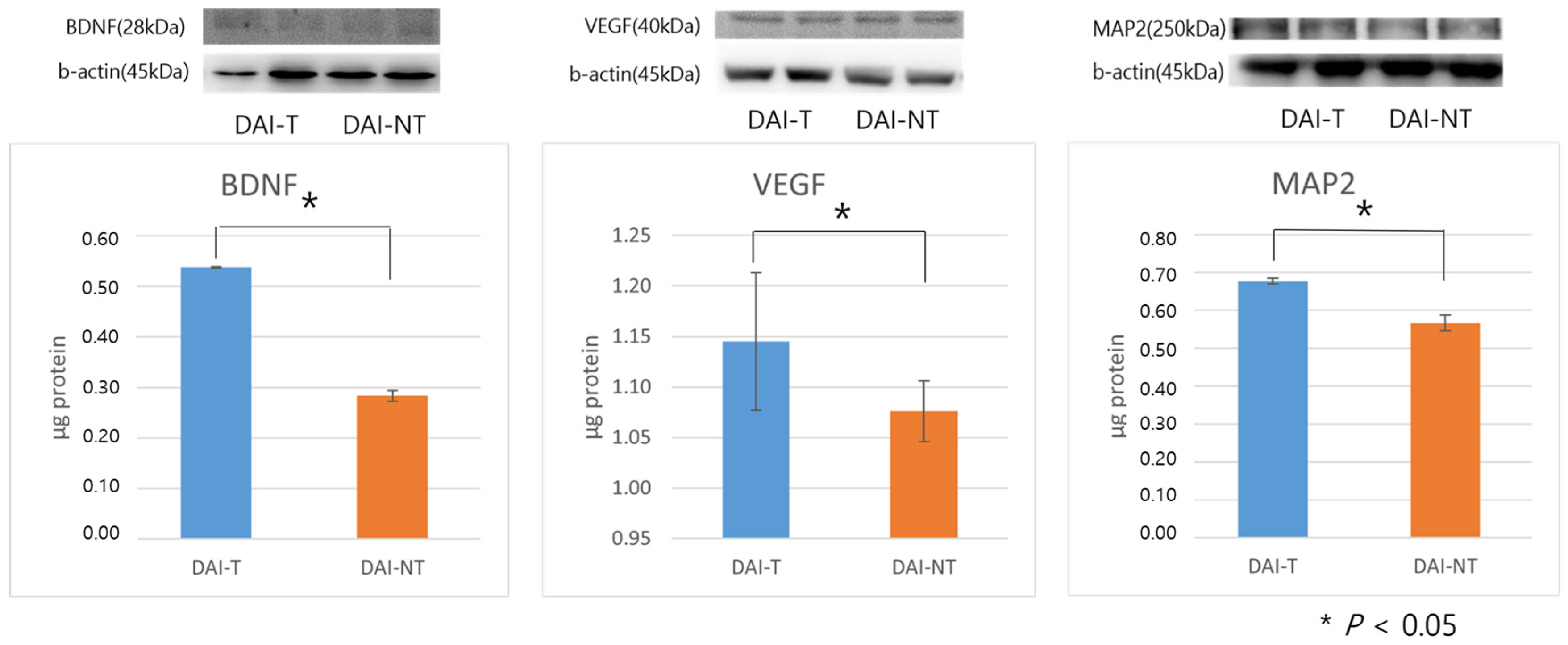
4.4. Western Blot Analysis
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Georges, A.; Das, J.M. Traumatic Brain Injury (Archive). In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Adams, J.H.; Doyle, D.; Ford, I.; Gennarelli, T.A.; Graham, D.I.; McLellan, D.R. Diffuse Axonal Injury in Head Injury: Definition, Diagnosis and Grading. Histopathology 1989, 15, 49–59. [Google Scholar] [CrossRef]
- Barman, A.; Chatterjee, A.; Bhide, R. Cognitive Impairment and Rehabilitation Strategies after Traumatic Brain Injury. Indian. J. Psychol. Med. 2016, 38, 172–181. [Google Scholar] [CrossRef] [PubMed]
- DeLisa, J.A.; Gans, B.M.; Walsh, N.E. Physical Medicine and Rehabilitation: Principles and Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005; ISBN 978-0-7817-4130-9. [Google Scholar]
- Arciniegas, D.B.; Held, K.; Wagner, P. Cognitive Impairment Following Traumatic Brain Injury. Curr. Treat. Options Neurol. 2002, 4, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Bosch, M.; McKenzie, J.E.; Ponsford, J.L.; Turner, S.; Chau, M.; Tavender, E.J.; Knott, J.C.; Gruen, R.L.; Francis, J.J.; Brennan, S.E.; et al. Evaluation of a Targeted, Theory-Informed Implementation Intervention Designed to Increase Uptake of Emergency Management Recommendations Regarding Adult Patients with Mild Traumatic Brain Injury: Results of the NET Cluster Randomised Trial. Implement. Sci. 2019, 14, 4. [Google Scholar] [CrossRef] [PubMed]
- Klein, A.P.; Tetzlaff, J.E.; Bonis, J.M.; Nelson, L.D.; Mayer, A.R.; Huber, D.L.; Harezlak, J.; Mathews, V.P.; Ulmer, J.L.; Sinson, G.P.; et al. Prevalence of Potentially Clinically Significant Magnetic Resonance Imaging Findings in Athletes with and without Sport-Related Concussion. J. Neurotrauma 2019, 36, 1776–1785. [Google Scholar] [CrossRef] [PubMed]
- Ananthaharan, A.; Kravdal, G.; Straume-Naesheim, T.M. Utility and Effectiveness of the Scandinavian Guidelines to Exclude Computerized Tomography Scanning in Mild Traumatic Brain Injury—A Prospective Cohort Study. BMC Emerg. Med. 2018, 18, 44. [Google Scholar] [CrossRef] [PubMed]
- Neville, I.S.; Zaninotto, A.L.; Hayashi, C.Y.; Rodrigues, P.A.; Galhardoni, R.; Ciampi de Andrade, D.; Brunoni, A.R.; Amorim, R.L.O.; Teixeira, M.J.; Paiva, W.S. Repetitive TMS Does Not Improve Cognition in Patients with TBI: A Randomized Double-Blind Trial. Neurology 2019, 93, e190–e199. [Google Scholar] [CrossRef] [PubMed]
- Emara, T.H.; Moustafa, R.R.; ElNahas, N.M.; ElGanzoury, A.M.; Abdo, T.A.; Mohamed, S.A.; ElEtribi, M.A. Repetitive Transcranial Magnetic Stimulation at 1 Hz and 5 Hz Produces Sustained Improvement in Motor Function and Disability after Ischaemic Stroke. Eur. J. Neurol. 2010, 17, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-H.; You, S.H.; Ko, M.-H.; Park, J.-W.; Lee, K.H.; Jang, S.H.; Yoo, W.-K.; Hallett, M. Repetitive Transcranial Magnetic Stimulation-Induced Corticomotor Excitability and Associated Motor Skill Acquisition in Chronic Stroke. Stroke 2006, 37, 1471–1476. [Google Scholar] [CrossRef]
- Mansur, C.G.; Fregni, F.; Boggio, P.S.; Riberto, M.; Gallucci-Neto, J.; Santos, C.M.; Wagner, T.; Rigonatti, S.P.; Marcolin, M.A.; Pascual-Leone, A. A Sham Stimulation-Controlled Trial of rTMS of the Unaffected Hemisphere in Stroke Patients. Neurology 2005, 64, 1802–1804. [Google Scholar] [CrossRef]
- Villamar, M.F.; Portilla, A.S.; Fregni, F.; Zafonte, R. Noninvasive Brain Stimulation to Modulate Neuroplasticity in Traumatic Brain Injury. Neuromodulation 2012, 15, 326–338. [Google Scholar] [CrossRef]
- Lu, X.; Bao, X.; Li, J.; Zhang, G.; Guan, J.; Gao, Y.; Wu, P.; Zhu, Z.; Huo, X.; Wang, R. High-Frequency Repetitive Transcranial Magnetic Stimulation for Treating Moderate Traumatic Brain Injury in Rats: A Pilot Study. Exp. Ther. Med. 2017, 13, 2247–2254. [Google Scholar] [CrossRef]
- Effect of Continuous Theta Burst Stimulation of the Right Dorsolateral Prefrontal Cortex on Cerebral Blood Flow Changes during Decision Making. Available online: https://pubmed.ncbi.nlm.nih.gov/22494829/ (accessed on 3 June 2024).
- Kito, S.; Fujita, K.; Koga, Y. Regional Cerebral Blood Flow Changes after Low-Frequency Transcranial Magnetic Stimulation of the Right Dorsolateral Prefrontal Cortex in Treatment-Resistant Depression. Neuropsychobiology 2008, 58, 29–36. [Google Scholar] [CrossRef]
- Speer, A.M.; Kimbrell, T.A.; Wassermann, E.M.; Repella, J.D.; Willis, M.W.; Herscovitch, P.; Post, R.M. Opposite Effects of High and Low Frequency rTMS on Regional Brain Activity in Depressed Patients. Biol. Psychiatry 2000, 48, 1133–1141. [Google Scholar] [CrossRef]
- Seewoo, B.J.; Feindel, K.W.; Etherington, S.J.; Rodger, J. Resting-State fMRI Study of Brain Activation Using Low-Intensity Repetitive Transcranial Magnetic Stimulation in Rats. Sci. Rep. 2018, 8, 6706. [Google Scholar] [CrossRef]
- Li, W.; Yang, Y.; Ye, Q.; Yang, B.; Wang, Z. Effect of Chronic and Acute Low-Frequency Repetitive Transcranial Magnetic Stimulation on Spatial Memory in Rats. Brain Res. Bull. 2007, 71, 493–500. [Google Scholar] [CrossRef]
- Yoon, K.J.; Lee, Y.-T.; Han, T.R. Mechanism of Functional Recovery after Repetitive Transcranial Magnetic Stimulation (rTMS) in the Subacute Cerebral Ischemic Rat Model: Neural Plasticity or Anti-Apoptosis? Exp. Brain Res. 2011, 214, 549–556. [Google Scholar] [CrossRef]
- Clarke, D.; Beros, J.; Bates, K.A.; Harvey, A.R.; Tang, A.D.; Rodger, J. Low Intensity Repetitive Magnetic Stimulation Reduces Expression of Genes Related to Inflammation and Calcium Signalling in Cultured Mouse Cortical Astrocytes. Brain Stimul. 2021, 14, 183–191. [Google Scholar] [CrossRef]
- Morris, R.G.; Garrud, P.; Rawlins, J.N.; O’Keefe, J. Place Navigation Impaired in Rats with Hippocampal Lesions. Nature 1982, 297, 681–683. [Google Scholar] [CrossRef] [PubMed]
- Crowe, A.R.; Yue, W. Semi-quantitative Determination of Protein Expression using Immunohistochemistry Staining and Analysis: An Integrated Protocol. Bio Protoc. 2019, 20, e3465. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-Y.; Feng, D.-F. Diffuse Axonal Injury: Novel Insights into Detection and Treatment. J. Clin. Neurosci. 2009, 16, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Shenton, M.E.; Hamoda, H.M.; Schneiderman, J.S.; Bouix, S.; Pasternak, O.; Rathi, Y.; Vu, M.-A.; Purohit, M.P.; Helmer, K.; Koerte, I.; et al. A Review of Magnetic Resonance Imaging and Diffusion Tensor Imaging Findings in Mild Traumatic Brain Injury. Brain Imaging Behav. 2012, 6, 137–192. [Google Scholar] [CrossRef] [PubMed]
- Mac Donald, C.L.; Dikranian, K.; Song, S.K.; Bayly, P.V.; Holtzman, D.M.; Brody, D.L. Detection of Traumatic Axonal Injury with Diffusion Tensor Imaging in a Mouse Model of Traumatic Brain Injury. Exp. Neurol. 2007, 205, 116–131. [Google Scholar] [CrossRef] [PubMed]
- Denic, A.; Macura, S.I.; Mishra, P.; Gamez, J.D.; Rodriguez, M.; Pirko, I. MRI in Rodent Models of Brain Disorders. Neurotherapeutics 2011, 8, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.; Gruenbaum, B.F.; Zvenigorodsky, V.; Shelef, I.; Oleshko, A.; Matalon, F.; Tsafarov, B.; Zlotnik, A.; Frenkel, A.; Boyko, M. Establishing a 3-Tesla Magnetic Resonance Imaging Method for Assessing Diffuse Axonal Brain Injury in Rats. Int. J. Mol. Sci. 2024, 25, 4234. [Google Scholar] [CrossRef] [PubMed]
- Miniussi, C.; Cappa, S.F.; Cohen, L.G.; Floel, A.; Fregni, F.; Nitsche, M.A.; Oliveri, M.; Pascual-Leone, A.; Paulus, W.; Priori, A.; et al. Efficacy of Repetitive Transcranial Magnetic Stimulation/Transcranial Direct Current Stimulation in Cognitive Neurorehabilitation. Brain Stimul. 2008, 1, 326–336. [Google Scholar] [CrossRef]
- Chou, Y.-H.; That, V.T.; Sundman, M. A Systematic Review and Meta-Analysis of rTMS Effects on Cognitive Enhancement in Mild Cognitive Impairment and Alzheimer’s Disease. Neurobiol. Aging 2020, 86, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lage, C.; Wiles, K.; Shergill, S.S.; Tracy, D.K. A Systematic Review of the Effects of Low-Frequency Repetitive Transcranial Magnetic Stimulation on Cognition. J. Neural Transm. 2016, 123, 1479–1490. [Google Scholar] [CrossRef]
- Huang, Y.-Z.; Edwards, M.J.; Rounis, E.; Bhatia, K.P.; Rothwell, J.C. Theta Burst Stimulation of the Human Motor Cortex. Neuron 2005, 45, 201–206. [Google Scholar] [CrossRef]
- Mesfin, F.B.; Gupta, N.; Hays Shapshak, A.; Taylor, R.S. Diffuse Axonal Injury. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Bullock, R.; Zauner, A.; Woodward, J.J.; Myseros, J.; Choi, S.C.; Ward, J.D.; Marmarou, A.; Young, H.F. Factors Affecting Excitatory Amino Acid Release Following Severe Human Head Injury. J. Neurosurg. 1998, 89, 507–518. [Google Scholar] [CrossRef]
- Arciniegas, D.B.; Bullock, M.R.; Katz, D.I.; Kreutzer, J.S.; Zafonte, R.D.; Zasler, N.D. Brain Injury Medicine: Principles and Practice; Demos Medical Publishing: New York, NY, USA, 2012; ISBN 978-1-61705-057-2. [Google Scholar]
- Mu, J.; Song, Y.; Zhang, J.; Lin, W.; Dong, H. Calcium Signaling Is Implicated in the Diffuse Axonal Injury of Brain Stem. Int. J. Clin. Exp. Pathol. 2015, 8, 4388–4397. [Google Scholar]
- Pérez-Navarro, E.; Gavaldà, N.; Gratacòs, E.; Alberch, J. Brain-Derived Neurotrophic Factor Prevents Changes in Bcl-2 Family Members and Caspase-3 Activation Induced by Excitotoxicity in the Striatum. J. Neurochem. 2005, 92, 678–691. [Google Scholar] [CrossRef] [PubMed]
- Vervliet, T.; Parys, J.B.; Bultynck, G. Bcl-2 Proteins and Calcium Signaling: Complexity beneath the Surface. Oncogene 2016, 35, 5079–5092. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.-Y.; Liu, Y.; Xie, J.-C.; Liu, N.-N.; Tian, X. Effects of Repetitive Transcranial Magnetic Stimulation on Synaptic Plasticity and Apoptosis in Vascular Dementia Rats. Behav. Brain Res. 2015, 281, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, C.; Díaz-Nido, J.; Avila, J. Phosphorylation of Microtubule-Associated Protein 2 (MAP2) and Its Relevance for the Regulation of the Neuronal Cytoskeleton Function. Prog. Neurobiol. 2000, 61, 133–168. [Google Scholar] [CrossRef] [PubMed]
- Siedler, D.G.; Chuah, M.I.; Kirkcaldie, M.T.K.; Vickers, J.C.; King, A.E. Diffuse Axonal Injury in Brain Trauma: Insights from Alterations in Neurofilaments. Front. Cell Neurosci. 2014, 8, 429. [Google Scholar] [CrossRef] [PubMed]
- More Than a Marker: Potential Pathogenic Functions of MAP2. Available online: https://pubmed.ncbi.nlm.nih.gov/36187353/ (accessed on 3 June 2024).
- Luo, L.; Liu, M.; Fan, Y.; Zhang, J.; Liu, L.; Li, Y.; Zhang, Q.; Xie, H.; Jiang, C.; Wu, J.; et al. Intermittent Theta-Burst Stimulation Improves Motor Function by Inhibiting Neuronal Pyroptosis and Regulating Microglial Polarization via TLR4/NFκB/NLRP3 Signaling Pathway in Cerebral Ischemic Mice. J. Neuroinflamm. 2022, 19, 141. [Google Scholar] [CrossRef] [PubMed]
- Hong, L.; Changjun, S.; Gong, J.U. Changes of HMW MAP-2 in Globus Pallidus and Substantia Nigra of Rats after Lowfrequency of Repetitive Transcranial Magnetic Stimulation. Zhongguo Shen Jing Ke Xue Za Zhi = Chin. J. Neurosci. 2001, 17, 219–225. [Google Scholar]
- Góra-Kupilas, K.; Jośko, J. The Neuroprotective Function of Vascular Endothelial Growth Factor (VEGF). Folia Neuropathol. 2005, 43, 31–39. [Google Scholar]
- Toffanin, T.; Folesani, F.; Ferrara, M.; Murri, M.B.; Zerbinati, L.; Caruso, R.; Nanni, M.G.; Koch, G.; Fadiga, L.; Palagini, L.; et al. Cognitive Functioning as Predictor and Marker of Response to Repetitive Transcranial Magnetic Stimulation in Depressive Disorders: A Systematic Review. Gen. Hosp. Psychiatry 2022, 79, 19–32. [Google Scholar] [CrossRef]
- Lu, B.; Nagappan, G.; Lu, Y. BDNF and Synaptic Plasticity, Cognitive Function, and Dysfunction. Handb. Exp. Pharmacol. 2014, 220, 223–250. [Google Scholar] [CrossRef] [PubMed]
- Buddle, M.; Eberhardt, E.; Ciminello, L.H.; Levin, T.; Wing, R.; DiPasquale, K.; Raley-Susman, K.M. Microtubule-Associated Protein 2 (MAP2) Associates with the NMDA Receptor and Is Spatially Redistributed within Rat Hippocampal Neurons after Oxygen-Glucose Deprivation. Brain Res. 2003, 978, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Garcia, K.O.; Ornellas, F.L.M.; Martin, P.K.M.; Patti, C.L.; Mello, L.E.; Frussa-Filho, R.; Han, S.W.; Longo, B.M. Therapeutic Effects of the Transplantation of VEGF Overexpressing Bone Marrow Mesenchymal Stem Cells in the Hippocampus of Murine Model of Alzheimer’s Disease. Front. Aging Neurosci. 2014, 6, 30. [Google Scholar] [CrossRef] [PubMed]


| Immunohistochemistry | Group | Area | Mean | % Area |
|---|---|---|---|---|
| BDNF | DAI-NT | 1,654,224 | 202.597 | 5.008 |
| DAI-T | 1,654,224 | 192.308 | 8.778 | |
| VEGF | DAI-NT | 1,654,224 | 168.547 | 8.711 |
| DAI-T | 1,654,224 | 158.346 | 12.105 | |
| MAP2 | DAI-NT | 1,654,224 | 204.679 | 10.475 |
| DAI-T | 1,654,224 | 202.148 | 12.814 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-M.; Jo, H.-S.; Kim, E.-J.; Na, J.-M.; Park, H.-K.; Han, J.-Y.; Kim, K.-H.; Choi, I.; Song, M.-K. The Effect of Repetitive Transcranial Magnetic Stimulation on Cognition in Diffuse Axonal Injury in a Rat Model. Neurol. Int. 2024, 16, 689-700. https://doi.org/10.3390/neurolint16040052
Kim H-M, Jo H-S, Kim E-J, Na J-M, Park H-K, Han J-Y, Kim K-H, Choi I, Song M-K. The Effect of Repetitive Transcranial Magnetic Stimulation on Cognition in Diffuse Axonal Injury in a Rat Model. Neurology International. 2024; 16(4):689-700. https://doi.org/10.3390/neurolint16040052
Chicago/Turabian StyleKim, Hyeong-Min, Hyun-Seok Jo, Eun-Jong Kim, Ji-Min Na, Hyeng-Kyu Park, Jae-Young Han, Ki-Hong Kim, Insung Choi, and Min-Keun Song. 2024. "The Effect of Repetitive Transcranial Magnetic Stimulation on Cognition in Diffuse Axonal Injury in a Rat Model" Neurology International 16, no. 4: 689-700. https://doi.org/10.3390/neurolint16040052
APA StyleKim, H.-M., Jo, H.-S., Kim, E.-J., Na, J.-M., Park, H.-K., Han, J.-Y., Kim, K.-H., Choi, I., & Song, M.-K. (2024). The Effect of Repetitive Transcranial Magnetic Stimulation on Cognition in Diffuse Axonal Injury in a Rat Model. Neurology International, 16(4), 689-700. https://doi.org/10.3390/neurolint16040052






