The Role of Reference Materials in the Research and Development of Diagnostic Tools and Treatments for Haemorrhagic Fever Viruses
Abstract
1. Background on Reference Materials and Their Use
2. Setting the Scene for Haemorrhagic Fever Virus Applications
3. Current Status of WHO Standards for Haemorrhagic Fever Viruses
3.1. Diagnostics
3.2. Serological Standard
3.3. Antigen Standard
3.4. Vaccine Standard
4. Future Outlook
Author Contributions
Funding
Conflicts of Interest
References
- Hartley, P. Diphtheria Antigens-Their Preparation, Properties, Laboratory Testing and Statutory Control. Proc. R. Soc. Med. 1945, 38, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Hartley, P. International Biological Standards: Prospect and Retrospect. Proc. R. Soc. Med. 1945, 39, 45–58. [Google Scholar] [CrossRef] [PubMed]
- Bristow, A.F.; Barrowcliffe, T.; Bangham, D.R. Standardization of biological medicines: The first hundred years, 1900–2000. Notes Rec. R. Soc. Lond. 2006, 60, 271–289. [Google Scholar] [CrossRef] [PubMed]
- WHO. Recommendations for the Preparation, Characterization and Establishment of International and Other Biological Reference Standards (WHO Technical Report Series No. 932); World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Sandle, L.N. The management of external quality assurance. J. Clin. Pathol. 2005, 58, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, J.; Richards, G.A.; Jimenez, J.I.S.; Baker, T.; Amin, P. Viral hemorrhagic fever in the tropics: Report from the task force on tropical diseases by the World Federation of Societies of Intensive and Critical Care Medicine. J. Crit. Care 2017, 42, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Racsa, L.D.; Kraft, C.S.; Olinger, G.G.; Hensley, L.E. Viral Hemorrhagic Fever Diagnostics. Clin. Infect. Dis. 2016, 62, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, E. Arboviruses and viral hemorrhagic fevers (VHF). Infect. Dis. Clin. N. Am. 2012, 26, 479–496. [Google Scholar] [CrossRef]
- Broadhurst, M.J.; Brooks, T.J.; Pollock, N.R. Diagnosis of Ebola Virus Disease: Past, Present, and Future. Clin. Microbiol. Rev. 2016, 29, 773–793. [Google Scholar] [CrossRef]
- Grolla, A.; Jones, S.; Kobinger, G.; Sprecher, A.; Girard, G.; Yao, M.; Roth, C.; Artsob, H.; Feldmann, H.; Strong, J.E. Flexibility of mobile laboratory unit in support of patient management during the 2007 Ebola-Zaire outbreak in the Democratic Republic of Congo. Zoonoses Public Health 2012, 59 (Suppl. S2), 151–157. [Google Scholar] [CrossRef]
- Towner, J.S.; Sealy, T.K.; Ksiazek, T.G.; Nichol, S.T. High-throughput molecular detection of hemorrhagic fever virus threats with applications for outbreak settings. J. Infect. Dis. 2007, 196, S205–S212. [Google Scholar] [CrossRef]
- Weidmann, M.; Faye, O.; Faye, O.; Abd El Wahed, A.; Patel, P.; Batejat, C.; Manugerra, J.C.; Adjami, A.; Niedrig, M.; Hufert, F.T.; et al. Development of Mobile Laboratory for Viral Hemorrhagic Fever Detection in Africa. J. Infect. Dis. 2018, 218, 1622–1630. [Google Scholar] [CrossRef] [PubMed]
- Wolfel, R.; Stoecker, K.; Fleischmann, E.; Gramsamer, B.; Wagner, M.; Molkenthin, P.; Di Caro, A.; Gunther, S.; Ibrahim, S.; Genzel, G.H.; et al. Mobile diagnostics in outbreak response, not only for Ebola: A blueprint for a modular and robust field laboratory. Eur. Surveill. 2015, 20, 30055. [Google Scholar] [CrossRef] [PubMed]
- FDA. Emergency Use Authorizations. United States Food and Drug Administration. Available online: https://www.fda.gov/medical-devices/emergency-situations-medical-devices/emergency-use-authorizations#ebola (accessed on 11 July 2019).
- Fhogartaigh, C.N.; Aarons, E. Viral haemorrhagic fever. Clin. Med. (Lond.) 2015, 15, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Warner, B.M.; Safronetz, D.; Stein, D.R. Current research for a vaccine against Lassa hemorrhagic fever virus. Drug Des. Dev. Ther. 2018, 12, 2519–2527. [Google Scholar] [CrossRef] [PubMed]
- Hamblion, E.L.; Raftery, P.; Wendland, A.; Dweh, E.; Williams, G.S.; George, R.N.C.; Soro, L.; Katawera, V.; Clement, P.; Gasasira, A.N.; et al. The challenges of detecting and responding to a Lassa fever outbreak in an Ebola-affected setting. Int. J. Infect. Dis. 2018, 66, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Emperador, D.M.; Mazzola, L.T.; Wonderly Trainor, B.; Chua, A.; Kelly-Cirino, C. Diagnostics for filovirus detection: Impact of recent outbreaks on the diagnostic landscape. BMJ Glob. Health 2019, 4, e001112. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, L.T.; Kelly-Cirino, C. Diagnostics for Lassa fever virus: A genetically diverse pathogen found in low-resource settings. BMJ Glob. Health 2019, 4, e001116. [Google Scholar] [CrossRef] [PubMed]
- Nikisins, S.; Rieger, T.; Patel, P.; Muller, R.; Gunther, S.; Niedrig, M. International external quality assessment study for molecular detection of Lassa virus. PLoS Negl. Trop. Dis. 2015, 9, e0003793. [Google Scholar] [CrossRef] [PubMed]
- Bartolini, B.; Gruber, C.E.; Koopmans, M.; Avsic, T.; Bino, S.; Christova, I.; Grunow, R.; Hewson, R.; Korukluoglu, G.; Lemos, C.M.; et al. Laboratory management of Crimean-Congo haemorrhagic fever virus infections: Perspectives from two European networks. Eur. Surveill. 2019, 24. [Google Scholar] [CrossRef]
- Drosten, C.; Kummerer, B.M.; Schmitz, H.; Gunther, S. Molecular diagnostics of viral hemorrhagic fevers. Antivir. Res. 2003, 57, 61–87. [Google Scholar] [CrossRef]
- Mazzola, L.T.; Kelly-Cirino, C. Diagnostic tests for Crimean-Congo haemorrhagic fever: A widespread tickborne disease. BMJ Glob. Health 2019, 4, e001114. [Google Scholar] [CrossRef] [PubMed]
- Trombley, A.R.; Wachter, L.; Garrison, J.; Buckley-Beason, V.A.; Jahrling, J.; Hensley, L.E.; Schoepp, R.J.; Norwood, D.A.; Goba, A.; Fair, J.N.; et al. Comprehensive panel of real-time TaqMan polymerase chain reaction assays for detection and absolute quantification of filoviruses, arenaviruses, and New World hantaviruses. Am. J. Trop. Med. Hyg. 2010, 82, 954–960. [Google Scholar] [CrossRef] [PubMed]
- UK Vaccine Network. Available online: https://www.gov.uk/government/groups/uk-vaccines-network (accessed on 11 July 2019).
- WHO. 2018 Annual review of diseases prioritized under the Research and Development Blueprint Informal consultation. In Proceedings of the Workshop on Prioritization of Pathogens, Geneva, Switzerland, 6–7 February 2018. [Google Scholar]
- SAGE Working Group on Dengue Vaccine and WHO Secretariat. Background Paper on Dengue Vaccines. Available online: https://www.who.int/immunization/sage/meetings/2018/april/2_DengueBackgrPaper_SAGE_Apr2018.pdf?ua=1 (accessed on 11 July 2019).
- Barrett, A.D.T. Yellow fever live attenuated vaccine: A very successful live attenuated vaccine but still we have problems controlling the disease. Vaccine 2017, 35, 5951–5955. [Google Scholar] [CrossRef] [PubMed]
- Marzi, A.; Mire, C.E. Current Ebola Virus Vaccine Progress. BioDrugs 2019, 33, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Venkatraman, N.; Silman, D.; Folegatti, P.M.; Hill, A.V.S. Vaccines against Ebola virus. Vaccine 2018, 36, 5454–5459. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, J.; Hu, Y.; Liang, Q.; Wei, M.; Zhu, F. Ebola vaccines in clinical trial: The promising candidates. Hum. Vaccin. Immunother. 2017, 13, 153–168. [Google Scholar] [CrossRef] [PubMed]
- Akanmori, B.M.D.; Bellah, A.; Traore, T.; Ward, M.; Mihigo, R. The Role of the African Vaccine Regulatory Forum (AVAREF) in the Accelerated Clinical Evaluation of Ebola Vaccine Candidates During the Large West Africa Epidemic. J. Immunol. Sci. 2018, S (011), 75–79. [Google Scholar] [CrossRef]
- Henao-Restrepo, A.M.; Preziosi, M.P.; Wood, D.; Moorthy, V.; Kieny, M.P.; Who Ebola Research, D.T. On a path to accelerate access to Ebola vaccines: The WHO’s research and development efforts during the 2014–2016 Ebola epidemic in West Africa. Curr. Opin. Virol. 2016, 17, 138–144. [Google Scholar] [CrossRef]
- Henao-Restrepo, A.M.; Camacho, A.; Longini, I.M.; Watson, C.H.; Edmunds, W.J.; Egger, M.; Carroll, M.W.; Dean, N.E.; Diatta, I.; Doumbia, M.; et al. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: Final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ca Suffit!). Lancet 2017, 389, 505–518. [Google Scholar] [CrossRef]
- Dowall, S.D.; Carroll, M.W.; Hewson, R. Development of vaccines against Crimean-Congo haemorrhagic fever virus. Vaccine 2017, 35, 6015–6023. [Google Scholar] [CrossRef]
- Faburay, B.; LaBeaud, A.D.; McVey, D.S.; Wilson, W.C.; Richt, J.A. Current Status of Rift Valley Fever Vaccine Development. Vaccines (Basel.) 2017, 5, 29. [Google Scholar] [CrossRef]
- CEPI. Coalition for Epidemic Preparendess Innovations. Available online: https://cepi.net/ (accessed on 11 July 2019).
- Plotkin, S.A. Vaccines for epidemic infections and the role of CEPI. Hum. Vaccin. Immunother. 2017, 13, 2755–2762. [Google Scholar] [CrossRef]
- McCormick, J.B.; Webb, P.A.; Krebs, J.W.; Johnson, K.M.; Smith, E.S. A prospective study of the epidemiology and ecology of Lassa fever. J. Infect. Dis. 1987, 155, 437–444. [Google Scholar] [CrossRef]
- NCDC. 2019 Lassa Fever Outbreak Situation Report; Nigeria Centre for Disease Control (NCDC): Abuja, Nigeria, 2019. Available online: https://ncdc.gov.ng/themes/common/files/sitreps/28e15c98c6b1da4232f2d3a4b2db40b5.pdf (accessed on 11 July 2019).
- Siddle, K.J.; Eromon, P.; Barnes, K.G.; Mehta, S.; Oguzie, J.U.; Odia, I.; Schaffner, S.F.; Winnicki, S.M.; Shah, R.R.; Qu, J.; et al. Genomic Analysis of Lassa Virus during an Increase in Cases in Nigeria in 2018. N. Engl. J. Med. 2018, 379, 1745–1753. [Google Scholar] [CrossRef]
- WHO. Technical Guidance on Lassa Fever. Available online: https://www.who.int/emergencies/diseases/lassa-fever/technical-guidance/en/ (accessed on 11 July 2019).
- WHO. WHO Target Product Profile for Lassa Virus Vaccine. Available online: https://www.who.int/blueprint/priority-diseases/key-action/LassaVirusVaccineTPP.PDF?ua=1 (accessed on 11 July 2019).
- WHO. Disease Outbreaks. Crimean-Congo Haemorrhagic Fever (CCHF). Available online: https://www.who.int/emergencies/diseases/crimean-congo-haemorrhagic-fever/en/ (accessed on 11 July 2019).
- WHO. R&D Blueprint Crimean-Congo Haemorrhagic Fever (CCHF). Available online: https://www.who.int/blueprint/priority-diseases/key-action/crimean-congo-haemorrhagic-fever/en/ (accessed on 11 July 2019).
- Bird, B.H.; Ksiazek, T.G.; Nichol, S.T.; Maclachlan, N.J. Rift Valley fever virus. J. Am. Vet. Med. Assoc. 2009, 234, 883–893. [Google Scholar] [CrossRef]
- Fawzy, M.; Helmy, Y.A. The One Health Approach is Necessary for the Control of Rift Valley Fever Infections in Egypt: A Comprehensive Review. Viruses 2019, 11, 139. [Google Scholar] [CrossRef]
- Anez, G.; Volkova, E.; Jiang, Z.; Heisey, D.A.R.; Chancey, C.; Fares, R.C.G.; Rios, M.; The Collaborative Study Group. Collaborative study to establish World Health Organization international reference reagents for dengue virus Types 1 to 4 RNA for use in nucleic acid testing. Transfusion 2017, 57, 1977–1987. [Google Scholar] [CrossRef]
- Public Health Agency of Canada. Human Pathogens and Toxins Act (HPTA). Available online: https://www.canada.ca/en/public-health/services/laboratory-biosafety-biosecurity/human-pathogens-toxins-act/security-sensitive-biological-agents.html (accessed on 11 July 2019).
- Directive 2000/54/EC of the European Parliament and the Council of 18 September 2000 on the Protection of Workers from Risks Related to Exposure to Biological Agents at Work (Seventh Individual Directive within the Meaning of Article 16(1) of Directive 89/391/EEC). Off. J. L 2000, 262, 21–45. Available online: http://data.europa.eu/eli/dir/2000/54/oj (accessed on 11 July 2019).
- Advisory Committee on Dangerous Pathogens, Health and Safety Executive. The Approved List of Biological Agents, 3th ed.; Health and Safety Executive: Bootle, UK, 2013. Available online: http://www.hse.gov.uk/pubns/misc208.pdf (accessed on 11 July 2019).
- U.S. Department of Health and Human Services, Public Health Service, Centre for Disease Control and Prevention, National Institute of Health. Biosafety in Microbiological and Biomedical Laboratories, 5th ed.; no. (CDC) 21-1112; HHS Publication: Atlanta, GA, USA, 2009.
- Mitchell, S.W.; McCormick, J.B. Physicochemical inactivation of Lassa, Ebola, and Marburg viruses and effect on clinical laboratory analyses. J. Clin. Microbiol. 1984, 20, 486–489. [Google Scholar]
- Smither, S.J.; Weller, S.A.; Phelps, A.; Eastaugh, L.; Ngugi, S.; O’Brien, L.M.; Steward, J.; Lonsdale, S.G.; Lever, M.S. Buffer AVL Alone Does Not Inactivate Ebola Virus in a Representative Clinical Sample Type. J. Clin. Microbiol. 2015, 53, 3148–3154. [Google Scholar] [CrossRef]
- WHO. Expert Committee on Biological Standardization, Sixty-Sixth Report (WHO Technical Report Series No. 999); World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Mattiuzzo, G.; Ashall, J.; Doris, K.S.; MacLellan-Gibson, K.; Nicolson, C.; Wilkinson, D.E.; Harvey, R.; Almond, N.; Anderson, R.; Efstathiou, S.; et al. Development of Lentivirus-Based Reference Materials for Ebola Virus Nucleic Acid Amplification Technology-Based Assays. PLoS ONE 2015, 10, e0142751. [Google Scholar] [CrossRef]
- Wilkinson, D.E.; Page, M.; Almond, N.; Anderson, R.; Ashall, J.; Berry, N.; Doris, K.S.; Efsthatiou, S.; Harvey, R.; Hassall, M.; et al. WHO Collaborative Study to Assess the Suitability of Interim Standards for Ebola Virus NAT Assays 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/197763/WHO_BS_2015.2279_eng.pdf?sequence=1&isAllowed=y (accessed on 23 August 2019).
- WHO. Expert Committee on Biological Standardization, Sixty-Eighth Report (WHO Technical Report Series No. 1011); World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- WHO. Expert Committee on Biological Standardization, Sixty-Ninth Report (WHO Technical Report Series No. 1016); World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- WHO. Expert Committee on Biological Standardization, Fifteenth Report (WHO Technical Report Series No. 259); World Health Organization: Geneva, Switzerland, 1963. [Google Scholar]
- WHO. Expert Committee on Biological Standardization, Fifty-Sixth Report (WHO Technical Series No. 941); World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- WHO. Expert Committee on Biological Standardization, Sixty-Seventh Report (WHO Technical Report Series No.1004); World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Krag, P.; Macnamara, F.N.; Lyng, J.; Bentzon, M.W.; Larsen, S.O. International collaborative assay of the international reference preparation of anti-yellow-fever serum. Bull. World Health Organ. 1965, 33, 243–255. [Google Scholar]
- Vesper, H.W.; Miller, W.G.; Myers, G.L. Reference materials and commutability. Clin. Biochem. Rev. 2007, 28, 139–147. [Google Scholar]
- Fryer, J.F.; Morris, C.L.; Almond, N.M.; Minor, P.D. Commutability of the World Health Organization International Standard for Human Cytomegalovirus: Standard or Assay. J. Clin. Microbiol. 2016, 54, 3073. [Google Scholar] [CrossRef]
- Rampling, T.; Page, M.; Horby, P. International Biological Reference Preparations for Epidemic Infectious Diseases. Emerg. Infect. Dis. 2019, 25, 205–211. [Google Scholar] [CrossRef]
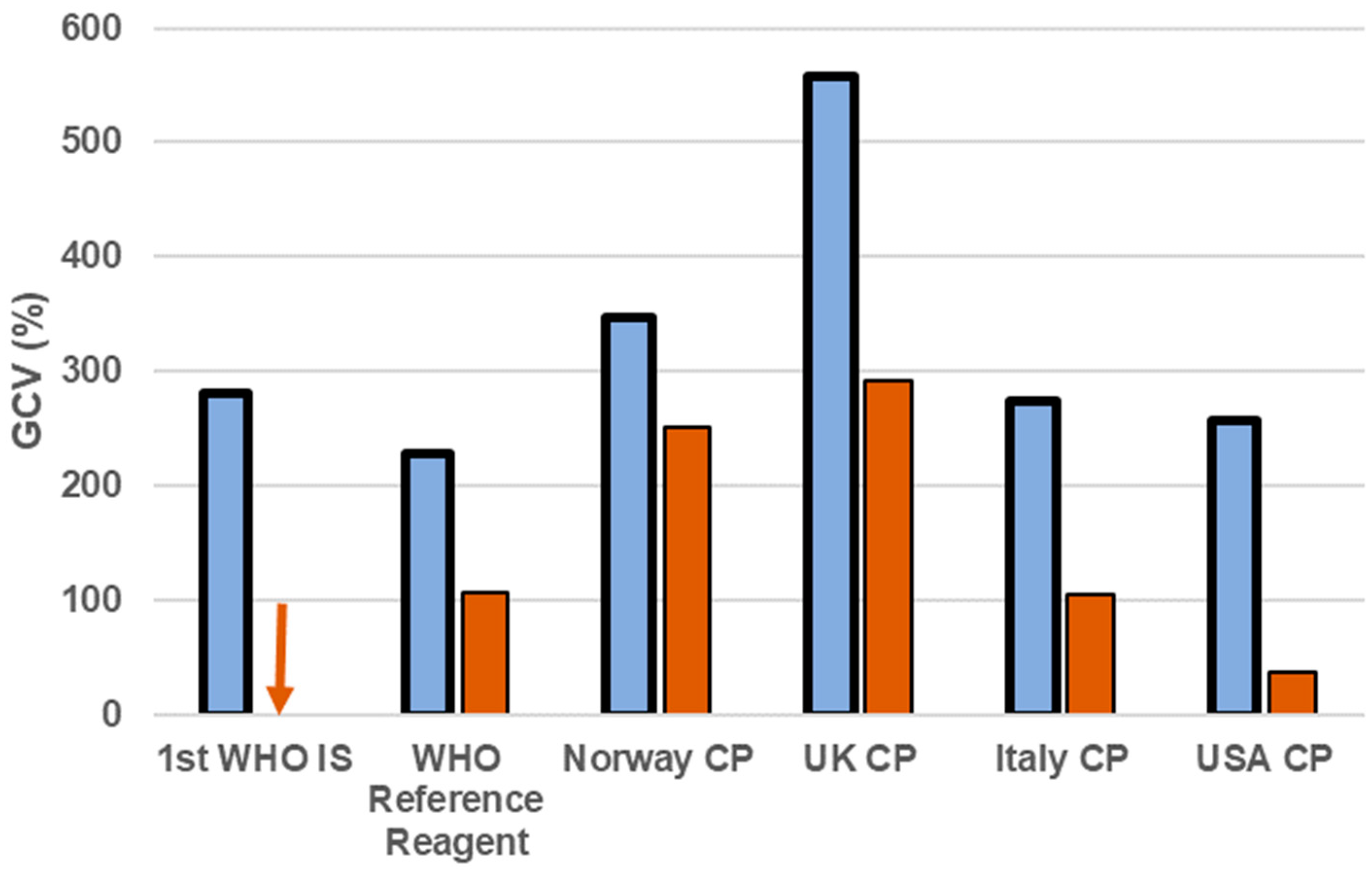
- Wilkinson, D.E.; Page, M.; Mattiuzzo, G.; Hassall, M.; Dougall, T.; Rigsby, P.; Stone, L.; Minor, P. Comparison of platform technologies for assaying antibody to Ebola virus. Vaccine 2017, 35, 1347–1352. [Google Scholar] [CrossRef]
- Wilkinson, D.H.M.; Mattiuzzo, G.; Stone, L.; Atkinson, E.; Hockley, J.; Rigsby, P.; Di Caro, A.; McLennan, S.; Olaussen, R.W.; Rijal, P.; et al. WHO Collaborative Study to Assess the Suitability of the 1st International Standard and the 1st International Reference Panel for Antibodies to Ebola Virus 2017. Available online: https://www.who.int/biologicals/expert_committee/BS2316_Anti-EBOV_Antibodies_WHO_1st_IS_and_WHO_1st_International_Ref_Panel.pdf (accessed on 23 August 2019).
- WHO. Target Product Profile for Zaïre Ebolavirus Rapid, Simple Test to be Used in the Control of the Ebola Outbreak in West Africa; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Dhillon, R.S.; Srikrishna, D.; Garry, R.F. Early detection of Lassa fever: The need for point-of-care diagnostics. Lancet Infect. Dis. 2018, 18, 601–602. [Google Scholar] [CrossRef]
- Pang, J.; Chia, P.Y.; Lye, D.C.; Leo, Y.S. Progress and Challenges towards Point-of-Care Diagnostic Development for Dengue. J. Clin. Microbiol. 2017, 55, 3339–3349. [Google Scholar] [CrossRef]
- Ferguson, M.; Heath, A. Collaborative study to assess the suitability of a candidate International Standard for yellow fever vaccine. Biologicals 2004, 32, 195–205. [Google Scholar] [CrossRef]
- WHO. Requirements for Yellow Fever Vaccine (Requirements for Biological Substances No.3); WHO Expert Committee on Biological Standardization, Forty-Sixth Report (WHO Technical Report Series No. 872); World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- WHO. Immunization, Vaccines and Biologicals—Questions and Answers on Dengue Vaccines. Available online: https://www.who.int/immunization/research/development/dengue_q_and_a/en/ (accessed on 11 July 2019).
- Zhu, F.C.; Wurie, A.H.; Hou, L.H.; Liang, Q.; Li, Y.H.; Russell, J.B.; Wu, S.P.; Li, J.X.; Hu, Y.M.; Guo, Q.; et al. Safety and immunogenicity of a recombinant adenovirus type-5 vector-based Ebola vaccine in healthy adults in Sierra Leone: A single-centre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 2017, 389, 621–628. [Google Scholar] [CrossRef]
- Dolzhikova, I.V.; Zubkova, O.V.; Tukhvatulin, A.I.; Dzharullaeva, A.S.; Tukhvatulina, N.M.; Shcheblyakov, D.V.; Shmarov, M.M.; Tokarskaya, E.A.; Simakova, Y.V.; Egorova, D.A.; et al. Safety and immunogenicity of GamEvac-Combi, a heterologous VSV- and Ad5-vectored Ebola vaccine: An open phase I/II trial in healthy adults in Russia. Hum. Vaccin. Immunother. 2017, 13, 613–620. [Google Scholar] [CrossRef]
- Coxon, C.H.; Longstaff, C.; Burns, C. Applying the science of measurement to biology: Why bother? PLoS Biol. 2019, 17, e3000338. [Google Scholar] [CrossRef]
- Innovative UK. Available online: www.gov.uk/government/organisations/innovate-uk (accessed on 11 July 2019).
- Foundation for Innovative New Diagnostics (FIND). Available online: https://www.finddx.org/at-a-glance/ (accessed on 11 July 2019).
- Page, M.; Wilkinson, D.E.; Mattiuzzo, G.; Efstathiou, S.; Minor, P. Developing biological standards for vaccine evaluation. Future Virol. 2017, 12, 431–437. [Google Scholar] [CrossRef]
- WHO. Guidelines for National Authorities on Quality Assurance for Biological Products (WHO Technical Report SERIES No. 822); World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]

| WHO International Standard | External Controls (Secondary Standard) | Internal Standard/In-Run Control | |
|---|---|---|---|
| Sample Quantification | yes | yes | yes |
| Assay Performance (over time/between operators) | yes | yes | no |
| Data Comparison (between labs/assay) | yes | yes/no | no |
| Assay Calibration in International Unit | yes | no | no |
| Pathogen | RNA | Antibody | Antigen | Vaccine | Reference |
|---|---|---|---|---|---|
| Ebola virus | 2015 | 2017 | 2015 | - | [55,58] |
| Sudan virus | Endorsed 2018 | Endorsed 2018 | - | - | [59] |
| Marburg virus | endorsed 2018 | endorsed 2018 | - | - | [59] |
| Yellow fever virus | - | 1962 | - | 2003 | [60,61] |
| Dengue virus | 2016 | endorsed 2017 | - | - | [58,62] |
| Lassa virus | Endorsed 2018 | Endorsed 2018 | - | - | [59] |
| CCHF virus | endorsed 2018 | endorsed 2018 | - | - | [59] |
| RVF virus | proposed 2019 | proposed 2019 | - | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mattiuzzo, G.; Bentley, E.M.; Page, M. The Role of Reference Materials in the Research and Development of Diagnostic Tools and Treatments for Haemorrhagic Fever Viruses. Viruses 2019, 11, 781. https://doi.org/10.3390/v11090781
Mattiuzzo G, Bentley EM, Page M. The Role of Reference Materials in the Research and Development of Diagnostic Tools and Treatments for Haemorrhagic Fever Viruses. Viruses. 2019; 11(9):781. https://doi.org/10.3390/v11090781
Chicago/Turabian StyleMattiuzzo, Giada, Emma M. Bentley, and Mark Page. 2019. "The Role of Reference Materials in the Research and Development of Diagnostic Tools and Treatments for Haemorrhagic Fever Viruses" Viruses 11, no. 9: 781. https://doi.org/10.3390/v11090781
APA StyleMattiuzzo, G., Bentley, E. M., & Page, M. (2019). The Role of Reference Materials in the Research and Development of Diagnostic Tools and Treatments for Haemorrhagic Fever Viruses. Viruses, 11(9), 781. https://doi.org/10.3390/v11090781





