Abstract
In recent years, cutting-edge technologies, such as artificial intelligence (AI), blockchain, and digital twin (DT), have revolutionized the healthcare sector by enhancing public health and treatment quality through precise diagnosis, preventive measures, and real-time care capabilities. Despite these advancements, the massive amount of generated biomedical data puts substantial challenges associated with information security, privacy, and scalability. Applying blockchain in healthcare-based digital twins ensures data integrity, immutability, consistency, and security, making it a critical component in addressing these challenges. Federated learning (FL) has also emerged as a promising AI technique to enhance privacy and enable decentralized data processing. This paper investigates the integration of digital twin concepts with blockchain and FL in the healthcare domain, focusing on their architecture and applications. It also explores platforms and solutions that leverage these technologies for secure and scalable medical implementations. A case study on federated learning for electroencephalogram (EEG) signal classification is presented, demonstrating its potential as a diagnostic tool for brain activity analysis and neurological disorder detection. Finally, we highlight the key challenges, emerging opportunities, and future directions in advancing healthcare digital twins with blockchain and federated learning, paving the way for a more intelligent, secure, and privacy-preserving medical ecosystem.
1. Introduction
Due to recent developments in information and communication technologies (ICTs), there are significant advantages and prospects for growth. The medical industry has transformed, and there has been a magnificent increase in the generation of medical data through smart biomedical systems. The availability and accuracy of patient data, which are enhanced by health record systems and other digital tools, lead to improved patient care and treatment plans. Furthermore, ICTs make it possible to continuously monitor patients’ health in real time by integrating medical sensors into wearable technology and other home-based equipment. By concentrating on various challenges that the healthcare industry encounters, this integration will ultimately improve people’s wellness and quality of life [1,2,3,4,5].
The methodologies used for remote monitoring and diagnosis of the patient with wearable electroencephalogram (EEG) devices are examples of a combination of new technological developments and data processing techniques with biomedical applications. Virtual representations of real-world items, procedures, or systems are known as digital twins (DT) [6]. Through digital twins, new avenues are provided for individuals and businesses to engage with the physical world in novel ways [7].
DTs have emerged as indispensable assets across diverse industries, including manufacturing [8], medical [9], and automotive [10]. By replicating physical systems, they serve as a foundational component that facilitates data fusion, simulation, and the integration of technology. This integration enables effective problem-solving for complex multidisciplinary challenges [11,12]. Notably, the significance of this technology has also been acknowledged within various fields, encompassing disciplines such as hydrology [13], agriculture [14], smart garden [15], industrial fault diagnosis [16], remote measuring [17], and soil disciplines [18]. Moreover, DT technology plays a significant role in making progress in crucial sectors, especially in the medical field.
This technology offers a comprehensive digital representation that can aid the medical sector [19], as it is significantly impacting this industry by optimizing clinical operations and driving innovation to enhance the cost-effectiveness, reliability, quality, and flexibility of the biomedical system. DT technology can create virtual replicas of human organs, bodily systems, and processes, which can be used for personalized medicine, treatment planning, and medical research [20]. For instance, the European Union has made significant progress in establishing initiatives for the creation of a digital representation of a human or disease state, which is referred to as the European virtual human twin (VHT) [21]. VHT technology is designed to replicate and predict the behavior of its physical equivalents, including interactions with any extra ailments a person may have. It is constructed using software models and data. Simultaneously, researchers globally have made remarkable progress in developing DTs for healthcare, personalized medicine, and predictive care [22,23]. The size of the medical industry’s digital twin market was estimated at USD 1.41 billion in 2023 and is projected to expand at a compound annual growth rate of 40.01% to reach USD 28.88 billion by 2032, according to SNS Insider Research [23].
To obtain a good digital representation of a patient, DT can gather and analyze data about them from a variety of sources, including wearables, medical devices, and electronic health records. Distinctive treatment plans, precision assessment, and real-time monitoring become feasible through this, enhancing patient outcomes from medical care. With the use of machine learning algorithms, DT can predict the progression of diseases, identify individuals at a higher risk, and suggest ways to avoid them. Consequently, this prevention strategy improves patient safety, long-term results, and the distribution of resources across medical systems. Additionally, it allows professionals to collaborate by facilitating information sharing and enhancing coordination. Additionally, they offer simulation and training programs that let medical professionals hone their abilities in a virtual environment [24,25,26]. Even though DT technology has so much potential, there are still several issues to be solved, such as data privacy and security assurances. For medical services, further research and investment are essential to fully exploit all benefits.
Federated learning (FL) is one of the emerging fields in artificial intelligence that revolves around the concept of decentralized data. However, due to the frequent occurrence of cyberattacks in real-time applications, many industry professionals are hesitant to embrace Internet of Everything (IoE) technology [27]. When integrated with new DT technologies in health services, FL is an effective method of artificial intelligence that has enormous potential. This combination could reduce privacy concerns, increase telemedicine accuracy, and improve machine learning forecasts and efficiency. Furthermore, it might make it possible for real-time monitoring across several medical sectors, including intelligent patient care platforms, personalized medicine, and informed prediction. When FL and DT are combined, local patient data are generated, increasing personal security and encouraging the widespread use of DT in clinical systems.
On the other hand, blockchain has emerged as a notable solution for mitigating cyberattacks in medical systems, effectively addressing various threats by ensuring data integrity, security, and transparency. However, despite its successes, blockchain technology has some limitations when applied in practice [28]. So, blockchain can complement FL by providing a decentralized, immutable ledger to track and verify model updates, enhancing data integrity and security. By combining these two technologies, medical networks could ensure that the FL process is transparent, tamper-proof, and traceable, particularly in multi-party collaborations across institutions and nations. This could foster greater trust and accountability in medical data sharing, particularly in sensitive areas like clinical trials and patient record aggregation.
Blockchain can be leveraged to create decentralized and secure healthcare-based digital twin systems that operate autonomously while ensuring robust security and resilience [29]. In essence, the integration of DT technology, FL, and blockchain offers a synergistic approach to developing intelligent and secure systems. By combining these advanced technologies, it becomes possible to design solutions that optimize performance, predict and prevent potential issues, and function autonomously with enhanced security, transparency, and reliability.
In summary, this paper presents a comprehensive review of the utilization of healthcare-based digital twins with blockchain and FL for advanced secure medical applications. By addressing these objectives, this aims to contribute to the understanding and advancement of healthcare-based digital twins, shedding light on their potential applications and providing insights into their development and future directions. While prior studies have explored the integration of new technology in healthcare, they have also overlooked its unique challenges. Few works systematically address security, scalability, and future research directions, and there is no prior work covering the integration of FL, blockchain, and digital twin in healthcare systems. This gap underscores the need for a comprehensive review that unites blockchain, FL, and DT to advance next-generation healthcare solutions. The selected research papers were sourced from different publishers such as Springer, Elsevier, MDPI, IEEE Xplore, and other databases, as depicted in Figure 1, using systematic searches. The keywords used were as follows: healthcare, bioengineering, blockchain, federated learning, healthcare security, AI, IoT systems, and digital twins.

Figure 1.
Percentage distribution of the surveyed literature by publisher.
The selection criteria were peer-reviewed status, publication within the last decade, and relevance to the study’s focus, i.e., leveraging blockchain and federated learning in biomedical and digital twins, thus ensuring a diverse and impactful range of contributions to this evolving field. In summary, the survey aimed to realize the following objectives:
- Investigation of Healthcare, Digital Twins, Blockchain and Federated Learning: This paper explores the concepts and terminologies related to healthcare, digital twins, blockchain, and federated learning, providing a clear understanding of these foundational concepts.
- Exploration of Healthcare-based Digital Twins: This study delves into the concept, architecture, and components of healthcare-based digital twins, examining their applications.
- Investigation of Healthcare-based Digital Twins with Federated Learning: This study delves into the concept of federated learning in healthcare-based digital twins, examining their application in EEG.
- Exploring Blockchain in Healthcare-Based Digital Twins: This study examines the integration of blockchain technology within healthcare and digital twins.
- Highlighting Development Platforms and Solutions: This paper highlights recent development platforms and solutions available for the implementation of healthcare-based digital twins, showcasing the tools and technologies that enable their creation and integration.
- Exploration of Challenges, Opportunities, and Future Trends: This study identifies and examines the challenges associated with healthcare-based digital twins, while also discussing opportunities and future trends for further advancements in this field.
The rest of this paper is laid out as follows: Section 2 introduces an overview of the fundamental concepts and principles of digital twins, blockchain, and federated learning. Section 3 presents healthcare with digital twins while platforms and solutions are presented in Section 4. Section 5 presents a case study on federated learning for electroencephalogram (EEG) signal classification, and Section 6 provides tools for the deployment of federated learning models. Section 7 presents real-world federated learning (FL) healthcare projects, and blockchain-based DT is presented in Section 8. The challenges, opportunities, limitations, and open research directions in the paper’s subject are presented in Section 9. Finally, the conclusion to this innovative theme is presented in Section 10.
2. Preliminaries
This section provides an overview of the fundamental concepts and principles of three innovative topics: digital twins and healthcare systems, blockchain, and federated learning. Understanding the basics of these technologies is essential for understanding their combinations and potential impact.
2.1. Digital Twins and Healthcare Systems
DTs are virtual replicas or representations of physical objects, systems, or processes [12]. They are created by capturing real-time data from sensors, devices, or other sources connected to the physical object or system. It provides a digital counterpart that mirrors the behavior, characteristics, and performance of their physical counterparts. They enable the real-time monitoring, analysis, and simulation of the physical objects or systems, allowing for predictive maintenance, optimization, and improved decision-making. One can find applications of this technology in various industries such as manufacturing, biomedical, transportation, and energy. Figure 2 illustrates the three fundamental components of a DT as follows:
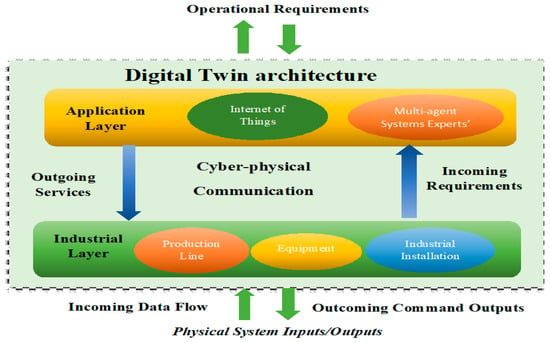
Figure 2.
The architecture of the DTs model.
- Industrial Component: This encompasses complex systems that rely on the environment in a virtual sense and on the physical environment. The industrial part represents the connection between the physical world and the DT.
- Application Component: This is focused on the characteristics and contents related to the virtual representation. It deals with the virtual vision and functionalities of the DT, providing a platform for the monitoring, analysis, and simulation of the physical system.
- Communication Component: This focuses on establishing cyber–physical connections. It enables the exchange of information and data flow between the physical system and its DT counterpart. Communication plays a crucial role in facilitating real-time interactions and synchronization between the physical and virtual domains.
Together, these three components form the foundation of the technology, encompassing the industrial, application, and communication aspects necessary for its operation and integration with the physical world. Since the COVID-19 pandemic, the world has been focusing on digitizing and improving healthcare in many aspects by introducing wearable devices, mobile apps, and other monitoring technologies. With the increasing digitalization of public health, the handling of information and big data has been focused on and researched by many scientists and researchers. Significant effort has been made in the field of big data, machine learning, and other computational methods to provide an effective method for the monitoring, treatment, and prevention of disease, as shown in Table 1.

Table 1.
Application of artificial intelligence in healthcare.
One of the methods that can be used to measure, monitor, diagnose, and manage brain and mental activity is electroencephalography (EEG). Recent developments in wearable EEG technology have made it possible to remotely collect brain activity data in real time, which is a huge step forward in the biomedical field. Therefore, there is a large amount of research on remote monitoring and diagnosis through wearable EEG devices. Integrating new technology with EEG signals improves the ability to monitor and detect difficult medical conditions, such as epileptic seizures [43], mental depression [44], Parkinson’s disease [45], Alzheimer’s disease [46], and Autism detection [47], in real time. Also, integrating IoT technology with medical systems facilitates more reliable real-time monitoring which can help to advance remedial methods, particularly in terms of managing brain activity, and supporting areas like emotion and depression [48,49]. However, the privacy and safety of the patient and their data are of great importance; this aspect has become paramount due to the linking of EEG data with new technology [50,51].
2.2. Federated Learning
Federated learning is an innovative approach in machine learning that facilitates the training of models using data from various sources distributed across different locations, such as local data centers or a central server, without the need to share the actual training data. This decentralized approach ensures that personal data remains secure and reduces the risk of data breaches.
By enabling the model to gain insights from diverse datasets while preserving data privacy, federated learning offers a promising solution that balances the benefits of collective learning with the protection of individual data [52,53]. Due to its benefits in data privacy and collaborative ML models, federated learning has attracted great interest and has many applications in the medical sector. Table 2 summarizes some of the main applications and aspects of federated learning in biomedical.

Table 2.
Federated learning applications in the biomedical sector.
Figure 3 visually depicts the primary distinction between federated learning and centralized learning. Several medical facilities or data centers, each with their own local datasets, participated in training a common model which involved federated learning for DTs in the health sector. They only shared model updates, which show, for example, how much the DT model improves while keeping all patient databases isolated and confidential. This integration ensures that the patients’ privacy is well maintained, while still enabling the development of highly effective DTs without sharing sensitive medical information on a centralized platform. On the other hand, centralized learning involves a central server that collects and stores all the training data from various devices or sources. The central server performs the training process using the combined dataset. This comparison highlights the decentralized nature of federated learning, where data remain distributed, and the collaborative aspect of the learning process, in contrast to the centralized approach where all data are aggregated and processed by a single entity [53].
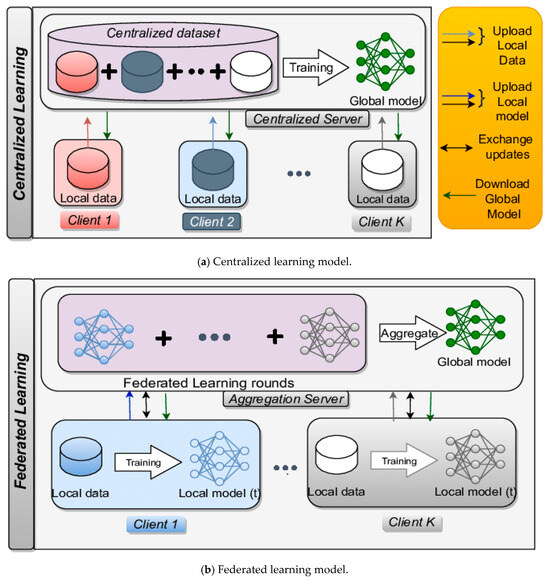
Figure 3.
Difference between (a) centralized learning and (b) federated learning.
Likewise, Figure 4 illustrates the three main types of federated learning currently used:
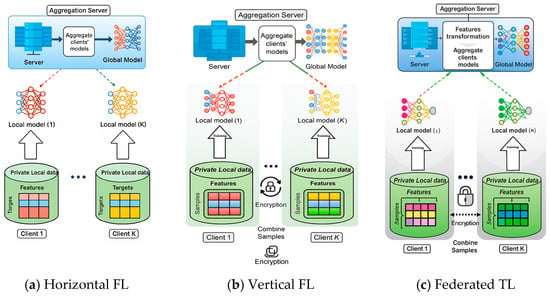
Figure 4.
Three main types of federated learning: (a) horizontal, (b) vertical, and (c) federated.
- Horizontal federated learning: This method is utilized when the participating datasets share the same feature space but vary in the sampling space. In other words, the data collected from different sources have similar attributes or characteristics but differ in terms of the instances or samples.
- Vertical federated learning: This method is applied when the datasets differ in the feature space but have a common sampling space. This means that the data collected from different sources have different attributes or characteristics but share the same instances or samples.
- Federated transfer learning: This method is employed in situations where the datasets not only differ in the feature space but also have distinct sampling spaces. In other words, the data collected from different sources have both different attributes or characteristics and different instances or samples.
These three types of federated learning allow for collaboration and model training across disparate datasets while accounting for variations in the feature space, sampling space, or both.
In terms of individuals’ health data, horizontal, vertical, and federated transfer learning promote the development of models from various medical databases, supporting the development of highly personalized virtual models of patients. Horizontal federated learning enables entities with similar infrastructural organization, such as hospitals with similar types of patient records, to collaborate with one another. Conversely, within vertical federated learning, a group of different but interrelated entities can merge their data for analysis without any overlap of the types of data they possess. For example, hospitals may have patient records, while drug manufacturers may have information on the genetics of those patients.
This section examines the comparison between federated learning and centralized learning approaches, particularly in biomedical applications. These two paradigms have distinct characteristics when applied to sensitive data, such as patient records, which are subject to stringent privacy regulations like the Health Insurance Portability And Accountability Act (HIPAA) [60] and the General Data Protection Regulation (GDPR).
- i.
- Privacy:
- Federated learning (FL) inherently supports privacy-preserving machine learning by allowing data to remain on local devices (e.g., hospitals or clinics), while sharing only model updates. This minimizes the exposure of sensitive data to potential breaches or misuse.
- In contrast, centralized learning requires the aggregation of all data into a central server, increasing the risk of data leakage during transmission or storage. Even with encryption and secure storage, centralized repositories remain a high-value target for cyberattacks.
- ii.
- Performance:
- Centralized learning typically offers better model performance since it has access to a full dataset, providing comprehensive training on all available data. This results in more accurate models, particularly when dealing with diverse datasets. However, this advantage comes at the cost of privacy and data-sharing concerns.
- On the other hand, federated learning often deals with non-independent and identically distributed (non-IID) data across nodes, which may introduce biases and reduce model performance. Additionally, due to decentralized data, the models may converge more slowly or reduce their effectiveness as a result of generalization.
- iii.
- Implementation Challenges:
- Federated learning faces significant technical challenges in biomedical applications, such as heterogeneity in data quality, device resources, and network connectivity across different hospitals or institutions. Ensuring secure model updates, synchronization, and efficient communication without compromising patient confidentiality are hurdles that need to be addressed.
- Centralized learning, although simpler to implement from a model-building perspective, demands sophisticated security protocols to protect the stored centralized data. Moreover, compliance with clinical regulations when sharing sensitive information poses further implementation challenges.
Overall, while federated learning offers promising privacy advantages, centralized learning may still outperform it in terms of model accuracy. A hybrid or balanced approach could potentially bridge the gap by incorporating privacy-preserving techniques such as differential privacy or secure multi-party computation within centralized systems. The further exploration of trade-offs in healthcare-specific use cases is necessary to determine the best approach for balancing privacy with performance.
Privacy preservation is a critical aspect of federated learning, especially in telemedicine, where sensitive data like patient records must remain secure. Techniques such as differential privacy (adding noise to model updates to protect individual data), homomorphic encryption (allowing encrypted computations without decryption), and secure multi-party computation (enabling collaborative computations without sharing private data) are key methods used to enhance privacy in federated setups. While these techniques offer robust privacy protection, they come with trade-offs in computational complexity and model performance. Each technique’s effectiveness depends on balancing privacy with efficiency, making them essential for ensuring secure, real-time applications in patient care.
2.3. Blockchain
Blockchain is a continuously expanding sequence of blocks interconnected through cryptographic techniques [61]. The structure of a blockchain network is depicted as an organized chain of blocks, as illustrated in Figure 5, where each block references its predecessor, forming a linked chain. Once a block is created and added to the blockchain, the transactions within that block become immutable and irreversible.
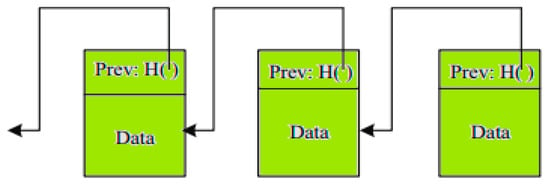
Figure 5.
Nodes on blockchain network.
At the heart of blockchain lies its consensus mechanism, which ensures that all consensus nodes in the network agree on a unified global state of the blockchain. A blockchain network generally comprises data producers, consensus nodes, and a data pool. When data producers wish to record information on the blockchain, they first submit it to the data pool, as depicted in Figure 6. Consensus nodes then retrieve this data from the pool, verify its authenticity, and execute the consensus protocol to designate a bookkeeping node. The bookkeeping node is tasked with writing the verified data onto the blockchain, ensuring its integrity and consistency.
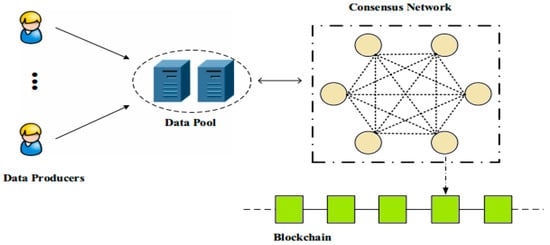
Figure 6.
Operational process of a blockchain network.
The character of blockchain can be as follows:
- Decentralization: Blockchain operates without a central authority. Any participant node can validate transactions via the proof of work (PoW) mechanism, avoiding bottlenecks and single points of failure.
- Anonymity: Participants use public/private keys, concealing their real identities.
- Autonomy: Nodes communicate directly without server involvement.
- Security: Smart contracts ensure secure communication, preventing unauthorized access and loss of data by encrypting data with public/private keys.
- Non-repudiation: Transactions, once validated and added to the chain, are irreversible and easily verified.
- Resiliency: Each node maintains a copy of the ledger, eliminating single points of failure.
- Smart Contracts: Self-executing programs define agreements among participants, ensuring efficiency, transparency, and trust. Each contract is uniquely addressed on the chain and invoked via transactions.
- Auditing: Blockchain records ownership changes, updates, and maintenance details, ensuring traceability throughout a device’s lifecycle.
- Immutability: Once verified, transactions cannot be altered, ensuring data integrity and accountability.
- Capacity: Blockchain leverages the resources of participant devices, storing data securely until needed.
- Cryptography: Advanced algorithms ensure data privacy and prevent unauthorized access, even if nodes gain fake chain access.
- Publicity: All devices have a ledger copy, enabling visibility into transactions while protecting content via private keys.
- Speed: Transactions are validated and distributed across the network in minutes.
- Cost-Efficiency: Decentralized architecture reduces costs by sharing resources for storing and transmitting large datasets.
The blockchain is classified, as shown in Table 3, and its applications vary across different domains. By distributing data across a network of nodes, blockchain eliminates the risk of a single point of failure and reduces the likelihood of unauthorized tampering. Additionally, each transaction is encrypted and linked to the previous one, creating an immutable chain that ensures data integrity [62].

Table 3.
Classification of blockchain.
3. Digital Twins for Health Systems
There are multiple layers of digital twins based in the health sector (also explored in Figure 7):
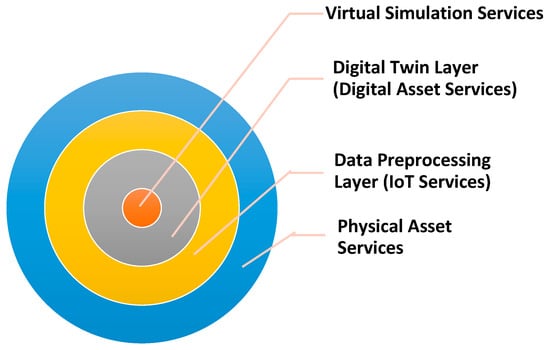
Figure 7.
The architecture of healthcare-based digital twins.
- Layer 1: Considered the foundational layer that encompasses the real device or system being replicated, which can range from buildings and manufacturing plants to vehicles. The physical asset, installed with instruments and Internet of Things devices, gathers information on its functioning, condition, and operations. These data are sent to the DT, which can be housed on-site or in the cloud.
- Layer 2: The data processing layer, made up of several components that work together to handle the information gathered from the physical devices: data handling and analysis, visualization, reporting, and data acquisition and storing. Advanced analytics methods like ML and AI are used in data processing and analysis to glean insights and spot trends.
- Layer 3: This layer is responsible for generating a simulated representation of the physical asset or system. It comprises a virtualization engine, a DT model, and APIs. The virtualization engine handles the creation and management of the DT, while the model defines the relationships between the physical asset and its virtual counterpart. The APIs provide an interface for users to interact with the DT.
- Layer 4: The virtual layer is where the DT is activated and comes to life. This layer includes an immersive environment, a social interaction engine, and a real-time simulation engine. The immersive environment serves as a virtual space where the DT is presented, providing a realistic and interactive representation. The social interaction engine facilitates user interactions, communication, collaboration, and shared experiences within biomedical systems.
The real-time simulation engine is responsible for simulating the behavior and characteristics of the physical asset in real time. It utilizes the data collected from the IoT devices embedded in the physical asset to dynamically simulate its operations, performance, and responses.
3.1. Elements of Healthcare-Based Digital Twins
Healthcare-based digital twins comprise several key elements, as illustrated in Figure 8, which enable their functionality and interaction within the virtual world. These include the following [24,25,26]:
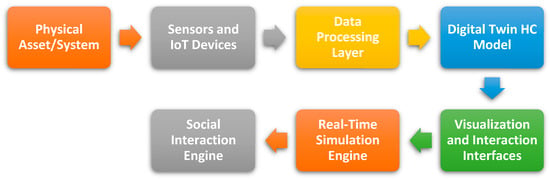
Figure 8.
Typical elements of healthcare-based digital twins.
- Physical Asset/System: The physical asset or system serves as the real-world counterpart that the digital twin replicates. It may represent a patient, a medical device, or another medical entity.
- Sensors and IoT Devices: These devices are embedded within the physical asset/system and are responsible for collecting data on its operations, condition, and performance. The sensors capture various parameters and transmit the data to the DT for analysis and visualization.
- Data Processing Layer: The components that manage the handling, analysis, and archiving of the information gathered from an actual asset or system form this layer. It covers methods for ingesting, storing, processing, and analyzing data, including artificial intelligence algorithms and machine learning.
- Digital Twin Model: This model identifies the virtual representation of the real asset/system within the medical system. It establishes the relationships and interconnections between the different components of the DT and the physical component.
- Visualization and Interaction Interfaces: These interfaces enable users to view and interact with the DT. They may include immersive environments, user interfaces, and interactive controls that allow users to explore, manipulate, and engage with this technology.
- Real-Time Simulation Engine: The simulation engine is responsible for modeling the behavior and responses of the digital twin based on the real-time data received from the physical component/system. It ensures that the DT closely mirrors the actions and characteristics of the physical counterpart.
- Social Interaction Engine: This component facilitates social interactions and collaboration within the biomedical process. It enables users to connect, communicate, and collaborate while interacting with the virtual components.
These elements work together to create a healthcare-based digital twin that offers an immersive, interactive, and dynamically simulated experience of the physical asset/system. They enable data-driven analysis, visualization, real-time monitoring, and collaborative exploration within the virtual environment.
3.2. Benefits of Healthcare with Digital Twins
There are many significant benefits of integrating healthcare with digital twins as follows [24,25,26,27]:
- There are several benefits for a variety of businesses when DT are integrated with care solutions. DTs provide virtual replicas of physical entities, so it facilitates the precise diagnosis of a patient. This combination enables the real-time monitoring of a patient and their wellness.
- One significant advantage is improved operational efficiency. By creating virtual replicas, physicians can simulate operations and analyze data to identify a person’s health status. This process optimizes resource allocation and streamlines workflow, which leads to improved patient outcomes.
- One significant advantage is improved surgical procedures or medical interventions. By creating virtual replicas, physicians can simulate operations and analyze data to identify the person’s health. This process optimizes resource allocation and gives patients a clearer understanding of their treatment options before proceeding.
- DTs can model the biomedical system and its constituents, such as hospitals, as well as clinical procedures, to determine the processes that are ineffective and to mitigate the threat of wasting resources. Moreover, DTs can be used to avoid excessive surgeries, to appropriately distribute resources, and to forecast medical outcomes in patients. These lead to operational efficiency, cost reduction, and the improved management of health services.
- Implementing DTs in the biomedical field enables experimentation and hypothesis testing in a virtual setting, thus facilitating research, and it offers realistic simulations for medical teaching and research.
- Additionally, DTs improve the management of risks and safety. Professionals and operators can proactively detect and reduce dangers by modeling situations and forecasting risks. For instance, in a pandemic, DTs could monitor social distancing using a virtual system and identify potential risks.
3.3. Applications for Medical-Based Digital Twins
DTs have many applications in the medical sector, as shown in Table 4. They significantly impact clinical services through the monitoring of patient care, optimizing clinical operations, and driving innovation.

Table 4.
The application of digital twins in the medical sector.
3.4. Platforms and Solutions for Healthcare-Based Digital Twins
DTs can be used to model organs, systems within the body, or even entire medical processes. Many companies [63,64,65,66,67,68,69] provide such solutions for the biomedical sector, as also exemplified in Figure 9:
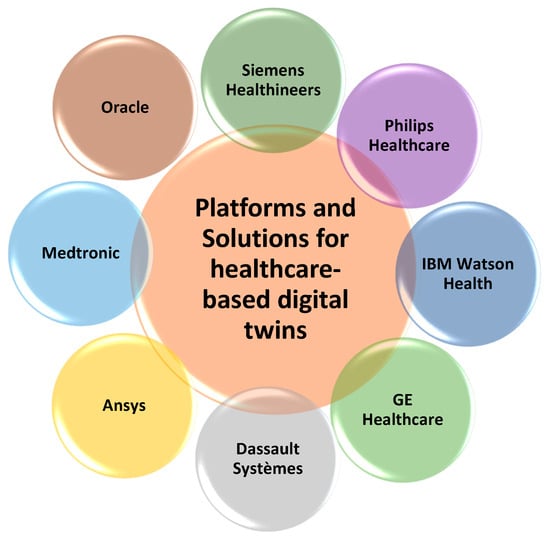
Figure 9.
Platforms for healthcare-based digital twins.
- Siemens Healthineers: Provide virtual twin solutions that simulate patient-specific organ and body systems to support diagnosis, treatment planning, and therapy optimization. Their technologies are applicable in cardiovascular diseases, oncology, and personalized medicine.
- Philips Healthcare: Leverages their IntelliSpace Discovery platform to develop virtual replica for personalized treatment plans. The platform’s applications include disease progression modeling, patient monitoring, and treatment optimization.
- IBM Watson Health: IBM integrates AI and analytics to create DTs that aid in clinical decision support and personalized medicine for chronic disease, drug development, and operational efficiency in hospitals.
- GE Healthcare: They provide the Hospital of the Future (HoF) Simulation Suite, which creates a digital replica of hospital(s) (and related ambulatory services) to be used in health management with the aim of focusing on the problems and scenarios.
- Dassault Systèmes: They provide a 3DEXPERIENCE platform that enables the creation of virtual representations for organs, entire body systems, and care workflows. This can be applied in virtual surgery, treatment planning, and drug development.
- Ansys: Ansys provides simulation tools for creating replicas that model the mechanical and fluid dynamics of organs and medical devices. Its applications are cardiovascular simulations, orthopedic implants, and medical device testing.
- Medtronic: Medtronic is developing DTs to enhance the design and performance of its medical devices and improve patient outcomes.
- Oracle: Oracle provides a platform for creating DTs of therapeutic processes to optimize patient care and operational efficiency.
4. Federated Learning for Healthcare-Based Digital Twin Systems
In the last few years, machine learning (ML) techniques have seen significant success, which is largely attributed to three key factors that have contributed to their widespread adoption and achievements; these are as follows [70]:
- Factor 1: The abundance of big data collected from diverse domains, such as image processing and mobile networking.
- Factor 2: Recent advancements in computational power and novel learning models.
- Factor 3: The advancement of machine learning (ML) techniques, which have played a critical role in enabling intelligent behavior in computational systems and enhancing data-driven decision-making across various medical applications.
Despite the considerable success of ML, there are challenges preventing its real-time implementation in most domains, primarily concerns regarding data privacy and the compromise of user data confidentiality during central learning, where data needs to be collected by the server. Additionally, the potential of leveraging the vast amount of data and computing resources available at the network edge for learning improvement remains largely untapped. While several companies offer well-trained ML models that can impart knowledge at lower computational costs, significant privacy and confidentiality issues remain unaddressed.
To address these challenges, federated learning (FL) has emerged as a promising concept in machine learning (ML) for healthcare-based digital twin systems. In contrast to the traditional central learning approach, FL allows multiple devices to collaboratively learn a shared ML model without the requirement of sharing their data with a centralized server. For example, instead of pooling information from various hospitals or clinics into one place, which can compromise the security of the information, a more dispersed approach could be used; this is what federated learning offers. Each organization’s learning becomes a localized activity by utilizing its digital data and only model updates are sent out. This data sharing or exchange process enhances the use of DTs technology in healthcare through improved patient privacy, which is very useful, especially given the sensitive nature of healthcare data. So, this technology creates a personalized virtual model of patients, while federated learning ensures that these models can be trained on diverse and comprehensive data in a privacy-preserving, decentralized manner. By enabling local model updates on individual devices and aggregating them in a privacy-preserving manner, FL ensures data privacy while leveraging the collective intelligence of distributed devices. This decentralized learning paradigm revolutionizes the ML landscape, providing a solution that addresses the limitations of centralized approaches and opens new opportunities for efficient and secure collaborative learning [62].
Trust and privacy preservation are crucial aspects of federated learning, playing a pivotal role in its successful implementation. Federated learning leverages a collaborative approach to model training while ensuring that sensitive data remains decentralized and protected. Trust is essential in federated learning as it involves multiple parties or entities contributing their data for model training. Each participant needs to trust that their data will be used appropriately and that the collaborative process is conducted fairly and securely. Building trust involves establishing clear communication, transparency, and adherence to privacy policies and data usage agreements. It is important to foster an environment where participants feel confident in the privacy and integrity of their information during the federated learning process.
Privacy preservation is a main objective of federated learning. The decentralized nature of this approach allows data to remain on local devices or servers, reducing the risks associated with data breaches and unauthorized access. Instead of sharing raw data, only model updates or gradients are exchanged during the FL process. This ensures that individuals’ data remain private and secure, as they are never exposed or transmitted to a central server. To further enhance privacy, various techniques are employed within federated learning. These include methods such as differential privacy, which add noise to the model updates to protect individual data contributions from being inferred. Secure aggregation techniques are also utilized to encrypt the exchanged model updates, preventing unauthorized access to sensitive information. By implementing these privacy preservation measures, federated learning enables participants to collaborate on model training without compromising the privacy of their data.
Overall, trust and privacy preservation are essential considerations in federated learning. By establishing trust among participants and employing privacy-preserving techniques, federated learning ensures the confidentiality, integrity, and security of data, allowing for collaborative and effective machine learning while respecting privacy concerns. Federated learning can be used for the cybersecurity of the Internet of Things (IoT). In this context, federated learning is employed as a mechanism to enhance the security of IoT systems.
5. Federated Learning for EEG Signal Classification: A Case Study
A recent case study which utilized FL in the biomedical field implemented EEG signals. Bringing together encephalographic data recorded from several patients in different hospitals and medical centers using this approach requires cooperation and coordinated efforts. Collectively, while trying to create an external knowledge base, every effort is made to ensure that information remains within the organization. This is very important in care settings where there is a need for confidentiality concerning patient information. This approach indicates the effectiveness of federated learning in improving EEG signal classification accuracy without compromising patient data security. This method can improve the evaluation of disorders associated with the brain. In addition, it can provide personalized treatment using a wider range of patient information without needing to centralize that information.
Recently, numerous studies have applied federated learning to EEG signals for various applications. In [71], researchers developed a federated learning system for emotion recognition using EEG signals and dense neural networks, enabling the privacy-preserving training of a server-hosted model without accessing users’ private data. In [72], a privacy-preserving federated learning framework was designed for epileptic seizure detection from EEG signals within a fog-computing-based IoMT. Another framework, group federated learning (Group-FL), was proposed for large-scale driver drowsiness detection, efficiently utilizing diverse client data while ensuring privacy [73]. In [74], a federated learning method was introduced for emotion recognition based on EEG signals. Additionally, [75] proposed a federated learning approach for MI-EEG signal classification using a CNN in the PhysioNet dataset, which includes EEG recordings of left- and right-hand imagery movements. Federated transfer learning (FTL), a novel privacy-preserving deep learning architecture for EEG categorization, was presented in [76]. Lastly, a comparison of studies on the use of federated learning algorithms for EEG data classification and associated applications is presented in Table 5, focusing on the methods used and the privacy-preserving aspects involved. Finally, one of the most important studies that used EEG signals involved seizure detection through centralized learning, as clarified in Figure 10.

Table 5.
A comparison among various studies using federated learning to EEG signal.
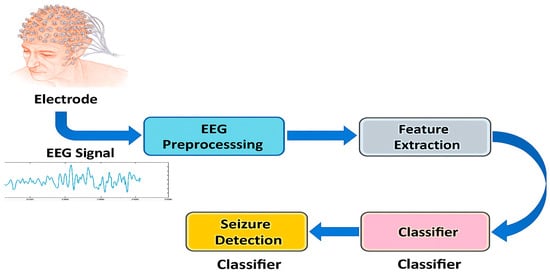
Figure 10.
Seizure detection using centralized learning.
In conclusion, the evaluation of the models in these studies is as follows: In [71], FLER-Net was trained on the DEAP dataset of EEG signals, achieving accuracy scores of 89.30% for valence, 86.85% for arousal, and 88.16% for dominance, surpassing previous privacy-preserving emotion recognition models by utilizing a broader feature space and a federated learning-optimized architecture. Similarly, the proposed Fed-ESD model in [72] demonstrated strong detection performance in the standard setting, with accuracy at 79.2%, sensitivity at 76.8%, specificity at 81.74%, geometric mean at 79.25%, and an F1-measure of 79.28%, though results varied significantly between participants, likely due to random variations in data distribution and individual EEG patterns. Furthermore, extensive experimentation in [73] validated the effectiveness of each component within the framework, achieving mean scores of 81.0% for accuracy, 82.0% for F1-score, and 87.9% for the area under curve (AUC) on a publicly available dataset with 11 subjects, highlighting the robust performance of the framework in processing the data.
6. Tools for the Deployment of Federated Learning Models
Federated learning (FL) frameworks play a crucial role in deploying models that ensure secure, distributed computation while maintaining data privacy. There are various tools for federated learning deployment, as illustrated in Figure 11. FederatedScope is a flexible and easy-to-use federated learning platform built on an event-driven architecture, offering extensive functionality to support diverse academic and industrial FL applications [77]. Intel’s OpenFL focuses on developing multiplatform applications, offering flexibility and cross-platform compatibility for various FL use cases [78].
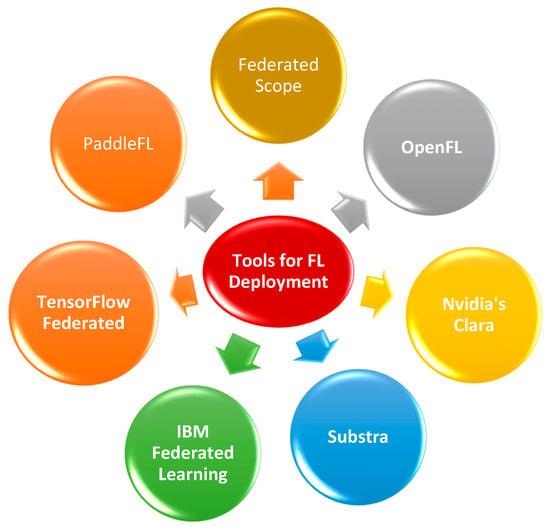
Figure 11.
Tools for federated learning deployment.
NVIDIA’s Clara [79] is a high-performance, AI-driven framework specifically tailored for building, handling, and implementing biomedical imaging systems, underscoring its significance in the biomedical sector. Owkin’s Substra [80] emphasizes meticulous privacy, allowing various stakeholders to collaborate in a distributed environment, which is essential for handling sensitive data. IBM Federated Learning supports enterprises in collecting, cleaning, and training data across different formats without data migration. It ensures compliance with privacy and security regulations, making it ideal for large-scale, enterprise-level applications [81]. Google’s TensorFlow Federated is an open-source frame designed to enable allocated computation and mutual model algorithms, promoting community-driven development and innovation [82]. Another open-source toolkit called PaddleFL is dedicated to enabling scalable deployment and easy experimentation with various FL algorithms and strategies across applications like computer vision, NLP, and recommendation systems [83].
These tools and frameworks collectively advance the deployment and development of federated learning models, addressing the critical need for privacy, security, and distributed computation across various industries.
7. Real-World Federated Learning (FL) Health Projects
In recent years, there have been several real-world federated learning (FL) health projects, illustrating their diverse applications across various countries and medical fields [84].
Project 1: Leveraging AI and blockchain technologies, a partnership between NVIDIA, Owkin, and King’s College London (UK) utilizes platforms such as Owkin Connect and NVIDIA Clara. This project targets multiple medical domains, including neurodegenerative diseases, cancer diagnosis and treatment, and heart disease diagnosis.
Project 2: In the US, Intel is using its Xeon Scalable processors and Software Guard Extensions (Intel SGX) to develop advanced FL-based care models. This initiative focuses on improving medical imaging while maintaining patient data privacy.
Project 3: The San Paolo Hospital in Italy, the Self-Defense Forces Central Hospital in Japan, and Hubei University in China are all part of an international effort. This project applies machine learning and image processing technologies to segment chest CT images for COVID-19 diagnosis, ensuring the confidentiality of patient information.
8. Blockchain-Based Healthcare Digital Twins
Blockchain and DT can be effectively combined in the healthcare domain to enhance security and combat fraud related to medical records, equipment, and services. In recent years, the biomedical industry has faced challenges with counterfeit medical products and the unauthorized duplication of sensitive data. As technology advances rapidly, it has become easier for malicious actors to create fake medical devices, duplicate records, or sell counterfeit pharmaceuticals, leading to financial losses and jeopardizing patient safety. Such fraudulent activities not only impact the credibility of care providers but can also cause lasting reputational damage. The integration of DT and blockchain technologies offers a robust solution to ensure the authenticity, integrity, and traceability of medical products and services, thereby safeguarding both providers and patients.
Likewise, their integration into the medical sector enables secure, real-time data collection and management within the medical IoT ecosystem. Medical data from devices in smart hospitals are analyzed, providing insights through artificial intelligence models. Combined with blockchain, these technologies ensure data security, privacy, and transparency. The blockchain can facilitate the collection of behavioral data essential for creating a patient’s DT. Amofa et al. [85] provides a visual representation of blockchain, highlighting how transactions are interconnected using smart contracts. They also illustrate the system architecture, which comprises several key entities: the data owner (patient), data users (hospitals), and the system infrastructure, including data management, a query system, and the blockchain network.
9. Challenges, Opportunities, Limitations, and Future Trends
The integration of DT in the medical field is developing quickly and is transforming a number of businesses by improving consumer service, streamlining processes, and boosting general productivity. However, this integration also presents several challenges that can be stated as follows:
- Data Integration and Interoperability: It might be challenging to incorporate real-time information from real systems or objects into DTs for medical systems. For data integration to be easy, compatibility and interoperability across many data formats, protocols, and devices must be guaranteed.
- Scalability and Performance: Developing DTs that can manage many concurrent users and complex interactions requires scalable infrastructure. Maintaining optimal performance, such as low latency and high responsiveness, is essential for a smooth user experience.
- Security and Privacy: DTs frequently contain vulnerable information, requiring robust security measures to protect against unauthorized access, data breaches, and privacy violations. Implementing authentication, encryption, and access controls is essential to ensure data security and privacy for secure medical data.
- User Experience and Interaction: Creating intuitive and participating person experiences within biomedical systems is crucial for user adoption. Seamless interactions between users and their DTs, as well as with other users, require thoughtful interface design, haptic feedback, natural language processing, and gesture recognition.
- Standardization and Interoperability: Lack of standardization and interoperability among different platforms and devices can hinder seamless integration. Developing industry-wide standards and protocols is necessary to ensuring compatibility and a connected ecosystem.
- Cost and Infrastructure Requirements: Creating and preserving medical-based digital twins can involve significant costs. Creating high-fidelity virtual environments, managing real-time data streams, and ensuring robust infrastructure requires substantial investments.
- Ethical Considerations: As the use of the new technology increases, ethical considerations regarding data ownership, privacy, algorithmic bias, and the misuse of DT arise. DTs depend on private patient information, like health records, DNA data, and live health tracking from wearables. This brings up questions about who owns the data: does the patient own the data used to make their model? Patients should control their health info, but the use of these data by different doctors, scientists, and outside groups can make ownership unclear. Also, strict rules need to exist to keep patient information safe in systems, particularly in federated learning environments where data are decentralized. Patients need to agree to and understand how people will use their data and why. Thus, regulators must monitor these technologies to make sure they are used in the right way and to protect patients’ rights. Establishing ethical guidelines and frameworks is crucial for governing their development and use.
Addressing these challenges will contribute to successful healthcare-based digital twin solutions, unlocking their full potential in various industries while ensuring data security, positive user experience, and ethical practices. Regardless of its promising potential, federated learning (FL) in care faces various significant challenges:
- Data Heterogeneity: Medical data vary widely across institutions in terms of format, quality, and completeness. This heterogeneity can complicate model training and reduce the generalizability of FL models.
- Computational and Communication Overhead: FL requires significant computational resources and efficient communication protocols. Ensuring that all participating devices and institutions can handle these demands is a challenge, especially in resource-constrained settings.
- Privacy and Security Risks: While FL aims to enhance data privacy, there are still potential risks of data leakage and attacks. Ensuring robust encryption and secure aggregation methods is critical to protecting patient information.
- Regulatory and Compliance Issues: Navigating the complex landscape of biomedical regulations and ensuring compliance with data protection laws such as HIPAA and GDPR can be challenging, particularly when dealing with international collaborations.
- Model Validation and Standardization: Establishing standardized protocols for validating and benchmarking FL models in the health sector is necessary to ensure their reliability and efficacy across different clinical environments.
- Patient Consent and Trust: Gaining patient consent for data use in FL and building trust in the system’s ability to protect their privacy and provide tangible benefits is crucial for widespread adoption.
- Resource Disparities: Disparities in technical and financial resources among participating institutions can affect quality and contributions to FL, potentially skewing results and benefits towards better-equipped organizations.
- Maintenance and Updates: Continuously maintaining and updating FL models to reflect new medical knowledge and changing care practices requires ongoing effort and coordination among all stakeholders.
Addressing these challenges is essential to fully realizing the capability of federated learning in transforming care and adjusting patient results. On the other hand, FL presents numerous opportunities to advance medical by enabling collaborative, secure, and efficient data use.
- Improved Predictive Models: By training on diverse datasets from multiple institutions, FL can develop more accurate and robust predictive models for disease diagnosis, progression, and treatment outcomes.
- Enhanced Patient Privacy: FL allows institutions to collaborate without sharing raw patient data, thereby enhancing privacy, and complying with stringent data protection regulations.
- Accelerated Research: Researchers can leverage FL to aggregate insights from a broad range of studies and clinical trials, speeding up the discovery of new treatments and medical innovations.
- Personalized Medicine: FL can support the development of personalized treatment plans by analyzing data from various sources, leading to more effective and tailored healing interventions.
- Real-Time Monitoring and Alerts: Integrating FL with IoT devices can enable real-time health monitoring and immediate alerts for critical conditions, improving patient care and response times.
- Cross-Institutional Collaboration: FL fosters collaboration among hospitals, research institutions, and care providers, leading to a more unified and comprehensive approach to medical research and patient care.
- Resource Optimization: Care providers can optimize resources by using FL models to predict patient needs, manage hospital workflows, and improve overall efficiency.
- Global Health Insights: FL can aggregate data from different regions and populations, providing valuable insights into global health trends and enabling better preparation for public health challenges.
- Drug Development: Pharmaceutical companies can use FL to securely analyze multi-institutional data, enhancing drug development processes and accelerating the identification of potential new therapies.
- Telemedicine Advancements: FL can improve telemedicine by providing accurate, data-driven insights for remote diagnosis and treatment, making quality healing more accessible to remote and underserved populations.
- Early Detection and Prevention: FL can enhance early detection and prevention strategies by analyzing patterns across large datasets, identifying risk factors, and enabling proactive measures.
- Quality Assurance: Continuous learning and validation through FL can help actors maintain high standards in medical practice by integrating the latest research findings and clinical best practices into everyday care delivery.
These opportunities highlight the transformative potential of federated learning, offering pathways to more effective, efficient, and equitable patient care.
Likewise, some limitations of implementing federated learning (FL) with DTs in the medical field as follows:
- Computational Complexity: Integrating real-time data from digital models with decentralized FL systems can require significant computational resources, including storage, bandwidth, and processing power, which may be inconsistent across biomedical institutions.
- Data Synchronization: Ensuring consistency and the synchronization of real-time data across multiple sources in DTs, while maintaining the integrity of FL models, is challenging and can affect model performance.
- Privacy vs. Performance Trade-off: Although FL enhances privacy by keeping data decentralized, the transmission of model updates still carries the risk of information leakage. Privacy-preserving techniques, like differential privacy, may degrade model accuracy.
- Scalability Challenges: Scaling FL with models to accommodate large telemedicine networks may increase latency, communication overhead, and resource requirements, making real-time applications more difficult.
- Infrastructure Variability: Medical institutions may have differing levels of technological infrastructure, which could limit widespread adoption and integration due to inconsistencies between hardware and connectivity capabilities.
These points highlight the key technical and practical challenges that need to be addressed for the successful implementation of FL and DTs in the biomedical field.
On the other hand, the integration of blockchain in medical systems also allows benefits such as data integrity, transparency, and security; however, serious limitations exist. Scalability is an important issue, as traditional blockchain networks struggle to keep up with the enormous numbers of transactions generated by big healthcare systems, resulting in delays and paralyzing system efficiency. In addition, the energy consumption of the various consensus mechanisms, mainly PoW, brings into question the sustainability of blockchain solutions, especially in medical systems, and their negative effects on the environment. Also, smart contracts can result in additional vulnerabilities: bugs or coding errors may lead to unforeseen consequences and data breaches that malevolent individuals can take advantage of. These limitations should, therefore, be tackled to ensure that blockchain applications in healthcare are scalable, energy-efficient, secure, and transparent, in order to be able to counter rapidly emerging cyber threats.
Ultimately, FL and blockchain are poised to revolutionize the biomedical industry by enabling secure and collaborative data sharing across institutions without compromising patient privacy. Some anticipated future trends are listed as follows:
- (1)
- Enhanced Data Privacy and Security: Continued advancements in federated learning algorithms will focus on strengthening data privacy and security, ensuring patient information remains confidential while facilitating large-scale medical research and repelling any fraudulent behavior or attacks [86,87].
- (2)
- Integration with IoT and Edge Devices: The integration of FL with Internet of Things (IoT) devices and edge computing will enable real-time health monitoring and analysis, providing immediate insights and interventions without the need for data to leave the device.
- (3)
- Personalized Medicine: FL will support the development of personalized medicine by allowing researchers to train models on diverse datasets from different populations, leading to more accurate and individualized treatment plans.
- (4)
- Collaborative Research Networks: The establishment of extensive collaborative networks across hospitals, research institutions, and pharmaceutical companies will drive innovation and accelerate the discovery of new treatments and diagnostic tools.
- (5)
- Improved Model Robustness: Techniques to improve the robustness and generalizability of federated learning models will be developed, ensuring they perform well across varied care settings and patient demographics.
- (6)
- Regulatory Compliance: Efforts will be made to align federated learning practices with global regulatory standards, promoting wider adoption in the medical industry by ensuring compliance with data protection laws.
- (7)
- Interoperability Standards: The development of interoperability standards will facilitate seamless data integration and model training across diverse biomedical systems and electronic health record (EHR) platforms.
- (8)
- Scalable Infrastructure: Investments in scalable and efficient federated learning infrastructure will enable the handling of increasing volumes of health data, making the technology accessible to more providers.
- (9)
- Clinical Trial Optimization: FL will be used to optimize clinical trials by securely aggregating data from multiple sites, enhancing patient recruitment, monitoring, and outcome assessment without compromising data privacy.
- (10)
- Patient Engagement and Trust: Increased focus on patient engagement and building trust in federated learning systems will be essential, ensuring that patients are informed and confident in their privacy and that their data is being used beneficially.
These trends indicate a promising future for federated learning in the biomedical field, with the potential to transform patient care, research, and the overall efficiency of biomedical systems. Likewise, to further enhance the forward-looking perspective of future trends in federated learning (FL), it is essential to consider emerging technologies like quantum computing. The rise in quantum computing holds significant promise for the future of federated learning, potentially solving the computational bottlenecks associated with secure multi-party computation and homomorphic encryption. Quantum algorithms could drastically reduce the time required for encryption and decryption tasks, allowing for faster and more efficient privacy-preserving operations in FL. This breakthrough could enable the large-scale deployment of FL systems in real-time medical diagnostics, genomic research, and drug discovery, further advancing the precision and speed of biomedical innovations.
By integrating these emerging technologies, federated learning could become more robust, scalable, and secure, paving the way for transformative improvements in medical research and patient care.
To conclude, the authors of this work emphasize the key concepts, issues, and challenges of integrating DTs with federated learning in smart biomedical systems. Table 6 compares existing research in this domain with the present study across various parameters. This comparison reveals that the present study addresses several aspects not covered in any single existing survey, making this research a significant novelty. The table also highlights the scope of various studies on new technologies and related fields, such as health informatics, edge computing, medical processes, big data, and IoMT security. It focuses on key aspects like security issues, challenges, and future research directions. Most existing studies (Refs. [88,89,90,91,92]) either neglect security issues, challenges, or DTs, or only partially cover future research directions. In contrast, the present review (published in 2025) comprehensively addresses security issues, challenges, and future research directions, and incorporates DTs, underscoring its unique and thorough approach in the context of FL and healthcare.

Table 6.
Comparison of characteristics of this study with previous surveys.
10. Conclusions
The rapid development of new technologies is moving the health sector toward intelligent, efficient, and patient-centric methods of service delivery. Some of these technologies are AI, IoT, blockchain, and digital twins. Among others, digital twins are avatars of a physical system or a human, which can simulate, monitor, and analyze real-time data for advanced medical decision-making. While initially developed in industries like manufacturing and aerospace, their adaptation to the field of healthcare has opened new opportunities for predictive diagnostics, personalized treatment, and operational optimization. Within this context, the present paper aims to explore how digital twin technologies, in conjunction with federated learning and blockchain, can solve certain core challenges surrounding privacy, security, and interoperability in medical environments. Thus, this paper provides a thorough review of the current state of the art, a breakdown of DT architecture, implementation tools, applications in healthcare, and emerging trends driving DTs integration into clinical practice. Furthermore, there is an emphasis on the necessity of integrating intelligent and secure infrastructure to support scalable and adaptable healthcare solutions. As healthcare systems become increasingly data-driven, the ability of digital twins to bridge real-world entities and virtual simulations offers transformative potential.
This review also emphasizes that federated learning facilitates the collaborative development of machine learning models across decentralized health datasets without the requirement to share sensitive patient information, thus maintaining privacy. Blockchain, concomitantly, establishes secure, transparent, and tamper-proof mechanisms for managing data, instilling trust in the digital healthcare system. With such integration, these technologies strengthen digital twin systems’ capabilities and credibility while solving problems related to data protection, reliability, and ethical compliance. Additionally, the integration of these technologies supports real-time, adaptive healthcare interventions that can respond dynamically to patient conditions. This paper further explores implementations in real world scenarios and monitors future research directions that can be undertaken to realize the full implementation of digital twins in next-generation intelligent and secure healthcare systems.
Author Contributions
Writing—original draft preparation, E.E.-D.H. and A.S.; writing—review and editing, E.E.-D.H. and A.S. All authors have read and agreed to the published version of the manuscript.
Funding
The authors would like to acknowledge Prince Sultan University for paying the article processing charges (APCs) of this publication.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
The authors would like to thank Prince Sultan University for their support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef]
- Sayed, A.; Zalam, B.A.; Elhoushy, M.; Nabil, E. Optimized type-2 fuzzy controller based on IoMT for stabilizing the glucose level in type-1 diabetic patients. Sci. Rep. 2023, 13, 14508. [Google Scholar] [CrossRef]
- Shalaby, A.S.; Gad, R.; Hemdan, E.E.D.; El-Fishawy, N. An efficient CNN based encrypted Iris recognition approach in cognitive-IoT system. Multimed. Tools Appl. 2021, 80, 26273–26296. [Google Scholar] [CrossRef]
- Babar, M.; Tariq, M.U.; Ullah, Z.; Arif, F.; Khan, Z.; Qureshi, B. An Efficient and Hybrid Deep Learning-Driven Model to Enhance Security and Performance of Healthcare Internet of Things. IEEE Access 2025, 13, 22931–22945. [Google Scholar] [CrossRef]
- Hammad, M.; Ahmad, S. Cognitive Computing Approaches for IoT, Healthcare, Big Data, and Cybersecurity: A Review. Navig. Chall. Object Detect. Through Cogn. Comput. 2025, 1–32. [Google Scholar] [CrossRef]
- El Saddik, A. Digital twins: The convergence of multimedia technologies. IEEE Multimed. 2018, 25, 87–92. [Google Scholar] [CrossRef]
- Zayed, S.M.; Attiya, G.M.; El-Sayed, A.; Hemdan, E.E.D. A review study on digital twins with artificial intelligence and internet of things: Concepts, opportunities, challenges, tools and future scope. Multimed. Tools Appl. 2023, 82, 47081–47107. [Google Scholar] [CrossRef]
- He, B.; Bai, K.-J. Digital twin-based sustainable intelligent manufacturing: A review. Adv. Manuf. 2021, 9, 1–21. [Google Scholar]
- Liu, Y.; Zhang, L.; Yuan, Y.; Zhou, L.; Ren, L.; Wang, F.; Liu, R.; Pang, Z.; Jamal Deen, M. A novel cloud- based framework for elderly healthcare Services using a digital twin. IEEE Access 2019, 7, 49088–49101. [Google Scholar] [CrossRef]
- Caputo, F.; Greco, A.; Fera, M.; Macchiaroli, R. Digital twins to enhance the integration of ergonomics in workplace design. Int. J. Ind. Ergon. 2019, 71, 20–31. [Google Scholar] [CrossRef]
- Hemdan, E.E.-D.; Zayed, S.M.; Attiya, G.; El-Sayed, A.; Sayed, A. Hybrid voting-GA ensemble learning for multi-class fault detection in digital twin-driven IIoT systems. Computing 2025, 107, 56. [Google Scholar] [CrossRef]
- Hemdan, E.E.D.; El-Shafai, W.; Sayed, A. Integrating Digital Twins with IoT-Based Blockchain: Concept, Architecture, Challenges, and Future Scope. Wirel. Pers. Commun. 2023, 131, 2193–2216. [Google Scholar] [CrossRef]
- Pedersen, A.N.; Borup, M.; Brink-Kjær, A.; Christiansen, L.E.; Mikkelsen, P.S. Living and prototyping digital twins for urban water systems: Towards multi-purpose value creation using models and sensors. Water 2021, 13, 592. [Google Scholar] [CrossRef]
- Pylianidis, C.; Osinga, S.; Athanasiadis, I.N. Introducing digital twins to agriculture. Comput. Electron. Agric. 2021, 184, 105942. [Google Scholar] [CrossRef]
- Verdouw, C.; Tekinerdogan, B.; Beulens, A.; Wolfert, S. Digital twins in smart farming. Agric. Syst. 2021, 189, 103046. [Google Scholar] [CrossRef]
- Sayed, A.; Alshathri, S.; Hemdan, E.E.-D. Conditional Generative Adversarial Networks with Optimized Machine Learning for Fault Detection of Triplex Pump in Industrial Digital Twin. Processes 2024, 12, 2357. [Google Scholar] [CrossRef]
- Nativi, S.; Mazzetti, P.; Craglia, M. Digital ecosystems for developing digital twins of the earth: The destination earth case. Remote Sens. 2021, 13, 2119. [Google Scholar] [CrossRef]
- Guo, H.; Nativi, S.; Liang, D.; Craglia, M.; Wang, L.; Schade, S.; Corban, C.; He, G.; Pesaresi, M.; Li, J.; et al. Big Earth Data science: An information framework for a sustainable planet. Int. J. Digit. Earth 2020, 13, 743–767. [Google Scholar] [CrossRef]
- Faisal, S.M.; Ishrat, M.; Khan, W. Digital Twins in Healthcare: Revolutionizing Patient Care and Medical Operations. In Digital Twins for Smart Cities and Urban Planning; CRC Press: Boca Raton, FL, USA, 2025; pp. 69–89. [Google Scholar]
- Mohamed, N.; Al-Jaroodi, J.; Jawhar, I.; Kesserwan, N. Leveraging Digital Twins for Healthcare Systems Engineering. IEEE Access 2023, 11, 69841–69853. [Google Scholar] [CrossRef]
- Shaping Europe’s Digital Future. Available online: https://digital-strategy.ec.europa.eu/en/policies/virtual-human-twins (accessed on 5 October 2024).
- Okegbile, S.D.; Cai, J.; Niyato, D.; Yi, C. Human digital twin for personalized healthcare: Vision, architecture and future directions. IEEE Netw. 2022, 37, 262–269. [Google Scholar] [CrossRef]
- Digital Twins in Healthcare Market Report Scope & Overview. Available online: https://www.snsinsider.com/reports/digital-twins-in-healthcare-market-3213 (accessed on 5 October 2024).
- Chen, J.; Yi, C.; Okegbile, S.D.; Cai, J.; Shen, X. Networking architecture and key supporting technologies for human digital twin in personalized healthcare: A comprehensive survey. IEEE Commun. Surv. Tutor. 2023, 26, 706–746. [Google Scholar] [CrossRef]
- Balasubramanyam, A.; Ramesh, R.; Sudheer, R.; Honnavalli, P.B. Revolutionizing Healthcare: A Review Unveiling the Transformative Power of Digital Twins. IEEE Access 2024, 12, 69652–69676. [Google Scholar] [CrossRef]
- Chen, J.; Yi, C.; Du, H.; Niyato, D.; Kang, J.; Cai, J.; Shen, X. A revolution of personalized healthcare: Enabling human digital twin with mobile AIGC. IEEE Netw. 2024, 38, 234–242. [Google Scholar] [CrossRef]
- Sami, A.; Malik, F.; Khan, Q.W.; Ahmad, N.; Shah, S.; Elaffendi, M.; Ahmad, N. Federated Learning for Sarcasm Detection: A Study of Attention-Enhanced BILSTM, GRU, and LSTM Architectures. IEEE Access 2024, 12, 196786–196802. [Google Scholar] [CrossRef]
- Deepak; Gulia, P.; Gill, N.S.; Yahya, M.; Gupta, P.; Shukla, P.K. Exploring the potential of blockchain technology in an iot-enabled environment: A review. IEEE Access 2024, 12, 31197–31227. [Google Scholar] [CrossRef]
- Hemdan, E.E.-D.; Mahmoud, A.S.A. BlockTwins: A blockchain-based digital twins framework. In Blockchain Applications in IoT Ecosystem; Springer International Publishing: Cham, Switzerland, 2021; pp. 177–186. [Google Scholar]
- Mehta, N.; Pandit, A.; Shukla, S. Transforming healthcare with big data analytics and artificial intelligence: A systematic mapping study. J. Biomed. Inform. 2019, 100, 103311. [Google Scholar] [CrossRef]
- Ali, M.; Paul, B.K.; Ahmed, K.; Bui, F.M.; Quinn, J.M.; Moni, M.A. Heart disease prediction using supervised machine learning algorithms: Performance analysis and comparison. Comput. Biol. Med. 2021, 136, 104672. [Google Scholar] [CrossRef]
- Lambay, M.A.; Mohideen, S.P. Big data analytics for healthcare recommendation systems. In Proceedings of the 2020 International Conference on System, Computation, Automation and Networking (ICSCAN), Pondicherry, India, 3–4 July 2020; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar]
- Gurupur, V.P.; Shelleh, M. Machine learning analysis for data incompleteness (madi): Analyzing the data completeness of patient records using a random variable approach to predict the incompleteness of electronic health records. IEEE Access 2021, 9, 95994–96001. [Google Scholar] [CrossRef]
- Singh, A.K.; Ghalib, M.R. KM-LA: Knowledge-based mining for linear analysis of inconsistent medical data for healthcare applications. Pers. Ubiquitous Comput. 2021, 28, 1. [Google Scholar] [CrossRef]
- Mwanza, J.; Telukdarie, A.; Igusa, T. Impact of industry 4.0 on healthcare systems of low-and middle-income countries: A systematic review. Health Technol. 2023, 13, 35–52. [Google Scholar] [CrossRef]
- Singh, G.; Violi, V.; Fisichella, M. Federated learning to safeguard patients data: A medical image retrieval case. Big Data Cogn. Comput. 2023, 7, 18. [Google Scholar] [CrossRef]
- Zahlan, A.; Ranjan, R.P.; Hayes, D. Artificial intelligence innovation in healthcare: Literature review, exploratory analysis, and future research. Technol. Soc. 2023, 74, 102321. [Google Scholar] [CrossRef]
- Yashudas, A.; Gupta, D.; Prashant, G.C.; Dua, A.; AlQahtani, D.; Reddy, A.S.K. DEEP-CARDIO: Recommendation System for Cardiovascular Disease Prediction using IOT Network. IEEE Sens. J. 2024, 24, 14539–14547. [Google Scholar] [CrossRef]
- Ullah, U.; Garcia-Zapirain, B. Quantum Machine Learning Revolution in Healthcare: A Systematic Review of Emerging Perspectives and Applications. IEEE Access 2024, 12, 11423–11450. [Google Scholar] [CrossRef]
- Torkey, H.; Hashish, S.; Souissi, S.; Hemdan, E.E.-D.; Sayed, A. Seizure Detection in Medical IoT: Hybrid CNN-LSTM-GRU Model with Data Balancing and XAI Integration. Algorithms 2025, 18, 77. [Google Scholar] [CrossRef]
- Jafari, M.; Adibnia, F. Securing IoMT healthcare systems with federated learning and BigchainDB. Future Gener. Comput. Syst. 2025, 165, 107609. [Google Scholar] [CrossRef]
- Gan, C.; Xiao, X.; Zhang, Y.; Zhu, Q.; Bi, J.; Jain, D.K.; Saini, A. An asynchronous federated learning-assisted data sharing method for medical blockchain. Appl. Intell. 2025, 55, 208. [Google Scholar] [CrossRef]
- Ein Shoka, A.A.; Dessouky, M.M.; El-Sayed, A.; Hemdan, E.E.D. EEG seizure detection: Concepts, techniques, challenges, and future trends. Multimed. Tools Appl. 2023, 82, 42021–42051. [Google Scholar] [CrossRef]
- Sharma, G.; Joshi, A.M.; Gupta, R.; Cenkeramaddi, L.R. DepCap: A smart healthcare framework for EEG based depression detection using time-frequency response and deep neural network. IEEE Access 2023, 11, 52327–52338. [Google Scholar] [CrossRef]
- Li, K.; Ao, B.; Wu, X.; Wen, Q.; Haq, E.U.; Yin, J. Parkinson’s disease detection and classification using EEG based on deep CNN-LSTM model. Biotechnol. Genet. Eng. Rev. 2023, 40, 2577–2596. [Google Scholar] [CrossRef]
- Khare, S.K.; Acharya, U.R. Adazd-Net: Automated adaptive and explainable Alzheimer’s disease detection system using EEG signals. Knowl.-Based Syst. 2023, 278, 110858. [Google Scholar] [CrossRef]
- Xu, Y.; Yu, Z.; Li, Y.; Liu, Y.; Li, Y.; Wang, Y. Autism spectrum disorder diagnosis with EEG signals using time series maps of brain functional connectivity and a combined CNN–LSTM model. Comput. Methods Programs Biomed. 2024, 250, 108196. [Google Scholar] [CrossRef]
- Meng, W.; Cai, Y.; Yang, L.T.; Chiu, W.-Y. Hybrid emotion-aware monitoring system based on brainwaves for internet of medical things. IEEE Internet Things J. 2021, 8, 16014–16022. [Google Scholar] [CrossRef]
- Sharma, G.; Joshi, A.M.; Pilli, E.S. DepML: An efficient machine learning-based MDD detection system in IoMT framework. SN Comput. Sci. 2022, 3, 394. [Google Scholar] [CrossRef]
- Landau, O.; Puzis, R.; Nissim, N. Mind your mind: EEG-based brain-computer interfaces and their security in cyber space. ACM Comput. Surv. (CSUR) 2020, 53, 1–38. [Google Scholar] [CrossRef]
- Hossen, I.; Tu, Y.; Hei, X. A first look at the security of EEG-based systems and intelligent algorithms under physical signal injections. In Proceedings of the 2023 Secure and Trustworthy Deep Learning Systems Workshop, Melbourne, VIC, Australia, 10–14 July 2023. [Google Scholar]
- Ferrag, M.A.; Friha, O.; Maglaras, L.; Janicke, H.; Shu, L. Federated deep learning for cyber security in the internet of things: Concepts, applications, and experimental analysis. IEEE Access 2021, 9, 138509–138542. [Google Scholar] [CrossRef]
- Babar, M.; Qureshi, B.; Koubaa, A. Review on Federated Learning for digital transformation in healthcare through big data analytics. Future Gener. Comput. Syst. 2024, 160, 14–28. [Google Scholar] [CrossRef]
- Patel, V.A.; Bhattacharya, P.; Tanwar, S.; Gupta, R.; Sharma, G.; Bokoro, P.N.; Sharma, R. Adoption of federated learning for healthcare informatics: Emerging applications and future directions. IEEE Access 2022, 10, 90792–90826. [Google Scholar] [CrossRef]
- Reddy, K.D.; Gadekallu, T.R.; Doulamis, A.D. A comprehensive survey on federated learning techniques for healthcare informatics. Comput. Intell. Neurosci. 2023, 2023, 8393990. [Google Scholar] [CrossRef]
- Poulain, R.; Bin Tarek, M.F.; Beheshti, R. Improving fairness in ai models on electronic health records: The case for federated learning methods. In Proceedings of the 2023 ACM Conference on Fairness, Accountability, and Transparency, Chicago, IL, USA, 12–15 June 2023. [Google Scholar]
- Muazu, T.; Mao, Y.; Muhammad, A.U.; Ibrahim, M.; Kumshe, U.M.M.; Samuel, O. A federated learning system with data fusion for healthcare using multi-party computation and additive secret sharing. Comput. Commun. 2024, 216, 168–182. [Google Scholar] [CrossRef]
- Almalki, J.; Alshahrani, S.M.; Khan, N.A. A comprehensive secure system enabling healthcare 5.0 using federated learning, intrusion detection and blockchain. PeerJ Comput. Sci. 2024, 10, e1778. [Google Scholar] [CrossRef]
- Alruwaili, M.; Siddiqi, M.H.; Idris, M.; Alruwaili, S.; Alanazi, A.S.; Khan, F. Advancing Disability Healthcare Solutions Through Privacy-Preserving Federated Learning with Theme Framework. Expert Syst. 2025, 42, e13807. [Google Scholar] [CrossRef]
- Edemekong, P.F.; Annamaraju, P.; Afzal, M.; Haydel, M.J. Health Insurance Portability and Accountability Act (HIPAA) Compliance. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Shahzad, M.; Rizvi, S.; Khan, T.A.; Ahmad, S.; Ateya, A.A. An Exhaustive Parametric Analysis for Securing SDN Through Traditional, AI/ML, and Blockchain Approaches: A Systematic Review. Int. J. Networked Distrib. Comput. 2025, 13, 1–16. [Google Scholar] [CrossRef]
- Liu, X.; Shah, R.; Shandilya, A.; Shah, M.; Pandya, A. A systematic study on integrating blockchain in healthcare for electronic health record management and tracking medical supplies. J. Clean. Prod. 2024, 447, 141371. [Google Scholar] [CrossRef]
- Available online: https://www.siemens-healthineers.com/digital-health-solutions (accessed on 6 October 2024).
- Available online: https://www.philips.com.eg/healthcare/product/HC881072/intellispace-portal-90-advanced-visual-analysis (accessed on 6 October 2024).
- Available online: https://www.ibm.com/industries/healthcare (accessed on 6 October 2024).
- Available online: https://www.gehccommandcenter.com/digital-twin (accessed on 6 October 2024).
- Available online: https://my.3dexperience.3ds.com/welcome/compass-world/3dexperience-life-sciences-and-healthcare (accessed on 6 October 2024).
- Available online: https://www.ansys.com/industries/healthcare (accessed on 6 October 2024).
- Available online: https://www.medtronic.com/us-en/our-company/healthcare-technology-innovation-ai-data-robotics.html (accessed on 6 October 2024).
- Alazab, M.; Rm, S.P.; Parimala, M.; Maddikunta, P.K.R.; Gadekallu, T.R.; Pham, Q.V. Federated learning for cybersecurity: Concepts, challenges, and future directions. IEEE Trans. Ind. Inform. 2021, 18, 3501–3509. [Google Scholar] [CrossRef]
- Anwar, M.A.; Agrawal, M.; Sethia, D. FLER-Net: Federated Learning for Emotion Recognition Using EEG Signals and Dense Neural Networks. SSRN 2023. [Google Scholar] [CrossRef]
- Ding, W.; Abdel-Basset, M.; Hawash, H.; Abdel-Razek, S.; Liu, C. Fed-ESD: Federated learning for efficient epileptic seizure detection in the fog-assisted internet of medical things. Inf. Sci. 2023, 630, 403–419. [Google Scholar] [CrossRef]
- Chen, X.; Niu, Y.; Zhao, Y.; Qin, X. An Efficient Group Federated Learning Framework for Large-Scale EEG-Based Driver Drowsiness Detection. Int. J. Neural Syst. 2023, 34, 2450003. [Google Scholar] [CrossRef]
- Xu, C.; Liu, H.; Qi, W. EEG Emotion Recognition Based on Federated Learning Framework. Electronics 2022, 11, 3316. [Google Scholar] [CrossRef]
- Ghader, M.; Farahani, B.; Rezvani, Z.; Shahsavari, M.; Fazlali, M. Exploiting Federated Learning for EEG-based Brain-Computer Interface System. In Proceedings of the 2023 IEEE International Conference on Omni-layer Intelligent Systems (COINS), Berlin, Germany, 23–25 July 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 1–6. [Google Scholar]
- Ju, C.; Gao, D.; Mane, R.; Tan, B.; Liu, Y.; Guan, C. Federated transfer learning for EEG signal classification. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 3040–3045. [Google Scholar]
- Available online: https://federatedscope.io/ (accessed on 12 May 2025).
- Available online: https://www.openfl.org/ (accessed on 22 June 2024).
- Available online: https://developer.nvidia.com/industries/healthcare/ (accessed on 22 June 2024).
- Available online: https://www.labelia.org/en/ppfl (accessed on 22 June 2024).
- Available online: https://www.ibm.com/docs/en/watsonx/saas?topic=models-federated-learning (accessed on 12 May 2025).
- Available online: https://www.tensorflow.org/federated (accessed on 22 June 2024).
- Available online: https://github.com/PaddlePaddle/PaddleFL/ (accessed on 12 May 2025).
- Rani, S.; Kataria, A.; Kumar, S.; Tiwari, P. Federated learning for secure IoMT-applications in smart healthcare systems: A comprehensive review. Knowl. -Based Syst. 2023, 274, 110658. [Google Scholar]
- Amofa, S.; Xia, Q.; Xia, H.; Obiri, I.A.; Adjei-Arthur, B.; Yang, J.; Gao, J.; Alzubi, O.A. Blockchain-secure patient Digital Twin in healthcare using smart contracts. PLoS ONE 2024, 19, e0286120. [Google Scholar] [CrossRef] [PubMed]
- Abd El Naby, A.; Hemdan, E.E.D.; El-Sayed, A. Deep learning approach for credit card fraud detection. In Proceedings of the 2021 International Conference on Electronic Engineering (ICEEM), Menouf, Egypt, 3–4 July 2021. [Google Scholar]
- Hemdan, E.E.D.; Manjaiah, D.H. Cybercrimes investigation and intrusion detection in internet of things based on data science methods. In Cognitive Computing for Big Data Systems Over IoT: Frameworks, Tools and Applications; Springer: Cham, Switzerland, 2018; pp. 39–62. [Google Scholar]
- Xu, J.; Glicksberg, B.S.; Su, C.; Walker, P.; Bian, J.; Wang, F. Federated learning for healthcare informatics. J. Healthc. Inform. Res. 2021, 5, 1–19. [Google Scholar] [CrossRef]
- Li, T.; Sahu, A.K.; Talwalkar, A.; Smith, V. Federated learning: Challenges, methods, and future directions. IEEE Signal Process. Mag. 2020, 37, 50–60. [Google Scholar] [CrossRef]
- Xia, Q.; Ye, W.; Tao, Z.; Wu, J.; Li, Q. A survey of federated learning for edge computing: Research problems and solutions. High-Confid. Comput. 2021, 1, 100008. [Google Scholar] [CrossRef]
- Li, J.; Meng, Y.; Ma, L.; Du, S.; Zhu, H.; Pei, Q.; Shen, X. A federated learning based privacy-preserving smart healthcare system. IEEE Trans. Ind. Inform. 2021, 18, 2021–2031. [Google Scholar] [CrossRef]
- Dhiman, G.; Juneja, S.; Mohafez, H.; El-Bayoumy, I.; Sharma, L.K.; Hadizadeh, M.; Islam, M.A.; Viriyasitavat, W.; Khandaker, M.U. Federated learning approach to protect healthcare data over big data scenario. Sustainability 2022, 14, 2500. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).