Factors Influencing the Screw Stability of Implant-Supported Single Crowns: An In Vitro Study
Highlights
- This study investigates the influence of retention type, implant/abutment angulation and the presence of sealant or disinfectant agents on the screw stability of implant-supported single crowns.
- Screw-retained restorations are more prone to screw loosening than cement-retained ones.
- Abutment angulation and the presence of gutta-percha or chlorhexidine gel did not show a significant impact on the screw stability of implant-supported single restorations.
- No restorations became loose after a simulated clinical service of 5 years under 98 N load.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
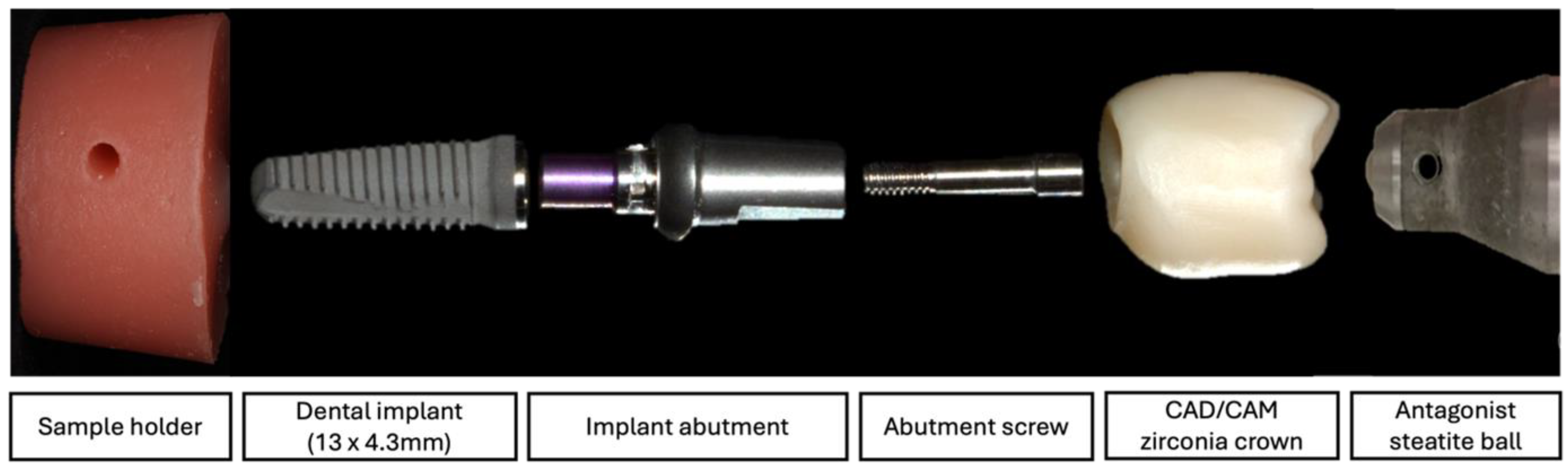
2.2. Sample Preparation
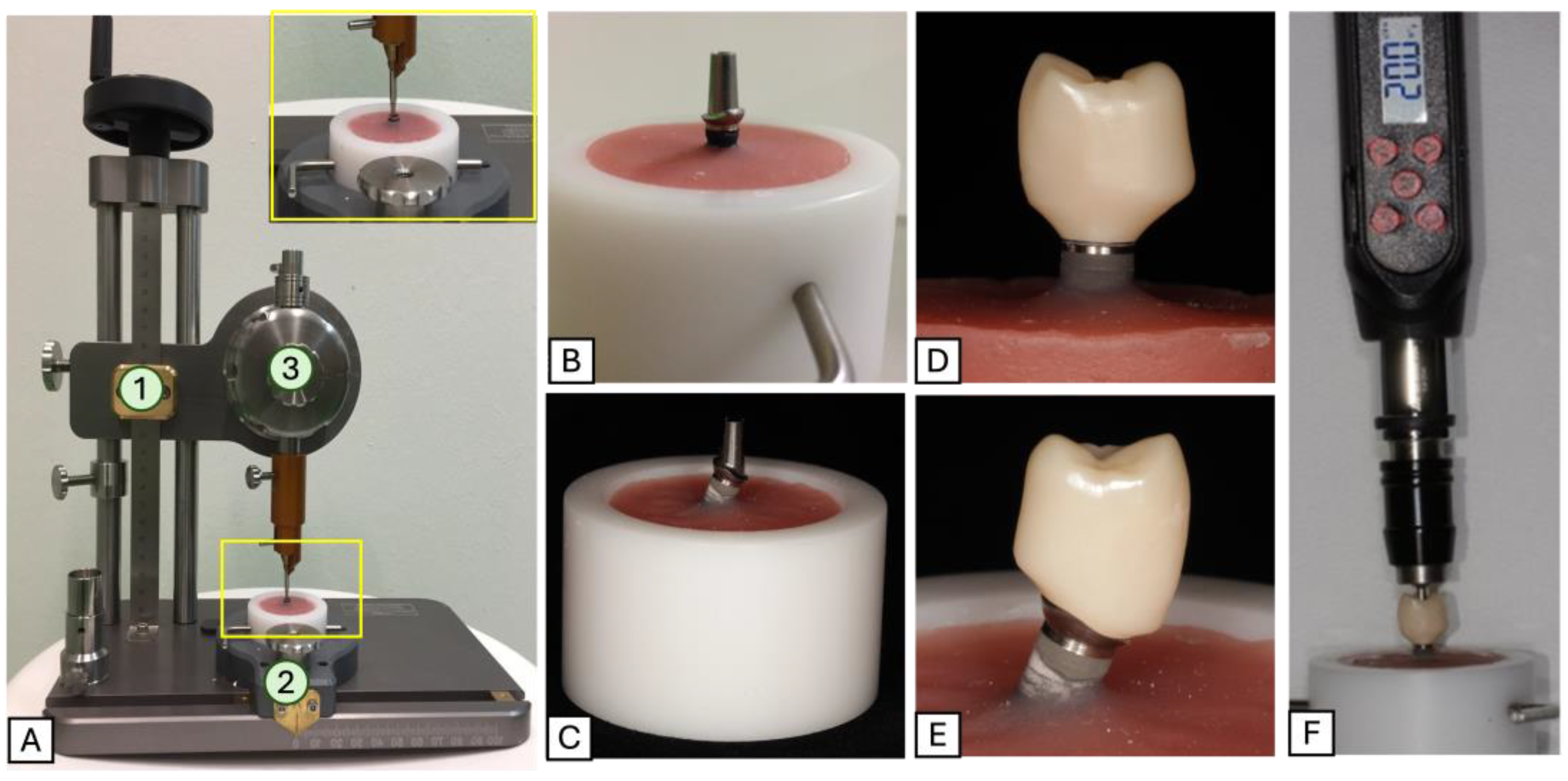
2.3. Dynamic Loading Tests
2.4. Reverse Torque Measurements
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Ang | Angulated |
| Cem | Cemented |
| CHX | Chlorhexidine |
| FDP | Fixed dental prosthesis |
| GP | Gutta-percha |
| Ncm | Newton centimeter |
| RTD | Reverse torque difference |
| RTV | Reverse torque value |
| SC | Single crown |
References
- Ranjan, M.; Almudarris, B.A.; Almalki, S.A.; Miyajiwala, J.; Irengbam, A.; Jadhav, M.S.; Makkad, R.S. Clinical Evaluation of the Long-Term Survival and Success Rates of Different Types of Implant-Supported Prostheses. J. Pharm. Bioallied Sci. 2024, 16, S2156–S2158. [Google Scholar] [CrossRef] [PubMed]
- Velasco-Ortega, E.; del Rocío Jiménez-Martin, I.; Moreno-Muñoz, J.; Núñez-Márquez, E.; Rondón-Romero, J.L.; Cabanillas-Balsera, D.; Jiménez-Guerra, Á.; Ortiz-García, I.; López-López, J.; Monsalve-Guil, L. Long-Term Treatment Outcomes of Implant Prostheses in Partially and Totally Edentulous Patients. Materials 2022, 15, 4910. [Google Scholar] [CrossRef] [PubMed]
- Hjalmarsson, L.; Gheisarifar, M.; Jemt, T. A systematic review of survival of single implants as presented in longitudinal studies with a follow-up of at least 10 years. Eur. J. Oral Implant. 2016, 9 (Suppl. S1), S155–S162. [Google Scholar]
- Jung, R.E.; Pjetursson, B.E.; Glauser, R.; Zembic, A.; Zwahlen, M.; Lang, N.P. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin. Oral Implant. Res. 2008, 19, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Li, X.C.; Bidra, A.S. Clinical outcomes of implant-supported monolithic zirconia crowns and fixed partial dentures: A systematic review. J. Prosthodont. 2023, 32, 102–107. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Valente, N.A.; Strasding, M.; Zwahlen, M.; Liu, S.; Sailer, I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 199–214. [Google Scholar] [CrossRef]
- Rabel, K.; Spies, B.C.; Pieralli, S.; Vach, K.; Kohal, R.J. The clinical performance of all-ceramic implant-supported single crowns: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29 (Suppl. S18), 196–223. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Makarov, N.A.; Thoma, D.S.; Zwahlen, M.; Pjetursson, B.E. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent. Mater. 2015, 31, 603–623. [Google Scholar] [CrossRef]
- Jung, R.E.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thoma, D.S. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implant. Res. 2012, 23 (Suppl. S6), 2–21. [Google Scholar] [CrossRef]
- Sailer, I.; Karasan, D.; Todorovic, A.; Ligoutsikou, M.; Pjetursson, B.E. Prosthetic failures in dental implant therapy. Periodontology 2000 2022, 88, 130–144. [Google Scholar] [CrossRef]
- Nissan, J.; Narobai, D.; Gross, O.; Ghelfan, O.; Chaushu, G. Long-term outcome of cemented versus screw-retained implant-supported partial restorations. Int. J. Oral Maxillofac. Implant. 2011, 26, 1102–1107. [Google Scholar]
- Gracis, S.; Michalakis, K.; Vigolo, P.; Vult von Steyern, P.; Zwahlen, M.; Sailer, I. Internal vs. external connections for abutments/reconstructions: A systematic review. Clin. Oral Implant. Res. 2012, 23 (Suppl. S6), 202–216. [Google Scholar] [CrossRef] [PubMed]
- Pirc, M.; Gadzo, N.; Balmer, M.; Naenni, N.; Jung, R.E.; Thoma, D.S. Maintenance Costs, Time, and Efforts Following Implant Therapy With Fixed Restorations Over an Observation Period of 10 Years: A Randomized Controlled Clinical Trial. Clin. Implant. Dent. Relat. Res. 2024. [CrossRef] [PubMed]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implant. Res. 2012, 23 (Suppl. S6), 22–38. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Zembic, A.; Jung, R.E.; Siegenthaler, D.; Holderegger, C.; Hämmerle, C.H. Randomized controlled clinical trial of customized zirconia and titanium implant abutments for canine and posterior single-tooth implant reconstructions: Preliminary results at 1 year of function. Clin. Oral Implant. Res. 2009, 20, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Henry, P.J.; Laney, W.R.; Jemt, T.; Harris, D.; Krogh, P.H.; Polizzi, G.; Zarb, G.A.; Herrmann, I. Osseointegrated implants for single-tooth replacement: A prospective 5-year multicenter study. Int. J. Oral Maxillofac. Implant. 1996, 11, 450–455. [Google Scholar]
- Jemt, T. Single implants in the anterior maxilla after 15 years of follow-up: Comparison with central implants in the edentulous maxilla. Int. J. Prosthodont. 2008, 21, 400–408. [Google Scholar] [PubMed]
- Mattheos, N.; Vergoullis, I.; Janda, M.; Miseli, A. The implant supracrestal complex and its significance for long-term successful clinical outcomes. Int. J. Prosthodont. 2021, 34, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Chae-Heon, C. Screw joint stability according to abutment screw materials. J. Korean Acad. Prosthodont. 2001, 39, 297–305. [Google Scholar]
- Elias, C.; Figueira, D.; Rios, P. Influence of the coating material on the loosing of dental implant abutment screw joints. Mater. Sci. Eng. C 2006, 26, 1361–1366. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, J. Mechanism of and factors associated with the loosening of the implant abutment screw: A review. J. Esthet. Restor. Dent. 2019, 31, 338–345. [Google Scholar] [CrossRef]
- Martin, W.C.; Woody, R.D.; Miller, B.H.; Miller, A.W. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J. Prosthet. Dent. 2001, 86, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.-S.; Shin, S.-Y. Influence of the implant abutment types and the dynamic loading on initial screw loosening. J. Adv. Prosthodont. 2013, 5, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Theoharidou, A.; Petridis, H.P.; Tzannas, K.; Garefis, P. Abutment screw loosening in single-implant restorations: A systematic review. Int. J. Oral Maxillofac. Implant. 2008, 23, 681–690. [Google Scholar]
- Bakaeen, L.G.; Winkler, S.; Neff, P.A. The effect of implant diameter, restoration design, and occlusal table variations on screw loosening of posterior single-tooth implant restorations. J. Oral Implantol. 2001, 27, 63–72. [Google Scholar] [CrossRef]
- Kourtis, S.; Damanaki, M.; Kaitatzidou, S.; Kaitatzidou, A.; Roussou, V. Loosening of the fixing screw in single implant crowns: Predisposing factors, prevention and treatment options. J. Esthet. Restor. Dent. 2017, 29, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, R.A.; Decker, A.M.; Plonka, A.B.; Wang, H.-L. The role of occlusion in implant therapy: A comprehensive updated review. Implant. Dent. 2016, 25, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Tak, S.; Jeong, Y.; Kim, J.E.; Kim, J.H.; Lee, H. A comprehensive study on the mechanical effects of implant-supported prostheses under multi-directional loading and different occlusal contact points. BMC Oral Health 2023, 23, 338. [Google Scholar] [CrossRef]
- Ma, S.; Fenton, A. Screw- versus cement-retained implant prostheses: A systematic review of prosthodontic maintenance and complications. Int. J. Prosthodont. 2015, 28, 127–145. [Google Scholar] [CrossRef] [PubMed]
- Quirynen, M.; van Steenberghe, D. Bacterial colonization of the internal part of two-stage implants. An in vivo study. Clin. Oral Implant. Res. 1993, 4, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Quirynen, M.; Vogels, R.; Peeters, W.; van Steenberghe, D.; Naert, I.; Haffajee, A. Dynamics of initial subgingival colonization of ’pristine’ peri-implant pockets. Clin. Oral Implant. Res. 2006, 17, 25–37. [Google Scholar] [CrossRef]
- Duarte, A.R.; Rossetti, P.H.; Rossetti, L.M.; Torres, S.A.; Bonachela, W.C. In vitro sealing ability of two materials at five different implant-abutment surfaces. J. Periodontol. 2006, 77, 1828–1832. [Google Scholar] [CrossRef]
- Harder, S.; Dimaczek, B.; Açil, Y.; Terheyden, H.; Freitag-Wolf, S.; Kern, M. Molecular leakage at implant-abutment connection--in vitro investigation of tightness of internal conical implant-abutment connections against endotoxin penetration. Clin. Oral Investig. 2010, 14, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Rimondini, L.; Marin, C.; Brunella, F.; Fini, M. Internal contamination of a 2-component implant system after occlusal loading and provisionally luted reconstruction with or without a washer device. J. Periodontol. 2001, 72, 1652–1657. [Google Scholar] [CrossRef] [PubMed]
- Koutouzis, T.; Gadalla, H.; Kettler, Z.; Elbarasi, A.; Nonhoff, J. The role of chlorhexidine on endotoxin penetration to the implant-abutment interface (IAI). Clin. Implant. Dent. Relat. Res. 2015, 17, 476–482. [Google Scholar] [CrossRef]
- Ozdiler, A.; Dayan, S.C.; Gencel, B.; Ozkol, G.I. Reverse Torque Values of Abutment Screws After Dynamic Loading: Effects of Sealant Agents and the Taper of Conical Connections. J. Oral Implant. 2021, 47, 287–293. [Google Scholar] [CrossRef] [PubMed]
- ISO 14801:2016; International Organization of Standardization. Dentistry—Implants—Dynamic Fatigue Test for Endosseous Dental Implants. International Organization for Standardization: Geneva, Switzerland, 2016.
- Strub, J.R.; Gerds, T. Fracture strength and failure mode of five different single-tooth implant-abutment combinations. Int. J. Prosthodont. 2003, 16, 167–171. [Google Scholar] [PubMed]
- Gaddale, R.; Mishra, S.K.; Chowdhary, R. Complications of screw-and cement-retained implant-supported full-arch restorations: A systematic review and meta-analysis. Int. J. Oral Implantol. 2020, 13, 11. [Google Scholar]
- Millen, C.; Brägger, U.; Wittneben, J.-G. Influence of prosthesis type and retention mechanism on complications with fixed implant-supported prostheses: A systematic review applying multivariate analyses. Int. J. Oral Maxillofac. Implant. 2015, 30, 110. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Mühlemann, S.; Zwahlen, M.; Hämmerle, C.H.; Schneider, D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin. Oral Implant. Res. 2012, 23 (Suppl. S6), 163–201. [Google Scholar] [CrossRef] [PubMed]
- Siamos, G.; Winkler, S.; Boberick, K.G. The relationship between implant preload and screw loosening on implant-supported prostheses. J. Oral Implantol. 2002, 28, 67–73. [Google Scholar] [CrossRef]
- Michalakis, K.X.; Hirayama, H.; Garefis, P.D. Cement-retained versus screw-retained implant restorations: A critical review. Int. J. Oral Maxillofac. Implant. 2003, 18, 719–728. [Google Scholar]
- Pietrabissa, R.; Gionso, L.; Quaglini, V.; Di Martino, E.; Simion, M. An in vitro study on compensation of mismatch of screw versus cement-retained implant supported fixed prostheses. Clin. Oral Implant. Res. 2000, 11, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Winkler, S.; Ring, K.; Ring, J.D.; Boberick, K.G. Implant screw mechanics and the settling effect: An overview. J. Oral Implant. 2003, 29, 242–245. [Google Scholar] [CrossRef]
- Mehl, C.; Harder, S.; Wolfart, M.; Kern, M.; Wolfart, S. Retrievability of implant-retained crowns following cementation. Clin. Oral Implant. Res. 2008, 19, 1304–1311. [Google Scholar] [CrossRef]
- Wolfart, M.; Wolfart, S.; Kern, M. Retention forces and seating discrepancies of implant-retained castings after cementation. Int. J. Oral Maxillofac. Implant. 2006, 21, 519–525. [Google Scholar]
- Chen, J.; Guo, J.; Yang, L.; Wang, L.; Zhang, X. Effect of different implant angulations on the biomechanical performance of prosthetic screws in two implant-supported, screw-retained prostheses: A numerical and experimental study. J. Prosthet. Dent. 2023, 130, 240.e1–240.e10. [Google Scholar] [CrossRef] [PubMed]
- Rasaie, V.; Abduo, J.; Falahchai, M. Clinical and laboratory outcomes of angled screw channel implant prostheses: A systematic review. Eur. J. Dent. 2022, 16, 488–499. [Google Scholar] [CrossRef] [PubMed]
- Cavallaro Jr, J.; Greenstein, G. Angled implant abutments: A practical application of available knowledge. J. Am. Dent. Assoc. 2011, 142, 150–158. [Google Scholar] [CrossRef]
- Pitman, J.; Van Craenenbroeck, M.; Glibert, M.; Christiaens, V. Screw loosening in angulation-correcting single implant restorations: A systematic review of in vitro studies. J. Prosthet. Dent. 2024, 132, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Ye, S.; Lyu, X.; Feng, H.; Liu, M.; Wen, C. Evaluation of sealing efficacy and removal convenience of sealing materials for implant abutment screw access holes. BMC Oral Health 2022, 22, 362. [Google Scholar] [CrossRef]
- Asli, H.N.; Saberi, B.V.; Fatemi, A.S. In vitro effect of chlorhexidine gel on torque and detorque values of implant abutment screw. Indian J. Dent. Res. 2017, 28, 314–319. [Google Scholar] [PubMed]
- Coelho, L.; Manzanares-Céspedes, M.C.; Mendes, J.; Tallón-Walton, V.; Astudillo-Rozas, W.; Aroso, C.; Mendes, J.M. Coating Materials to Prevent Screw Loosening in Single Dental Implant Crowns: A Systematic Review. Materials 2024, 17, 5053. [Google Scholar] [CrossRef] [PubMed]
- Koosha, S.; Toraji, S.; Mostafavi, A.S. Effect of fluid contamination on the reverse torque values of abutment screws at implant-abutment connections. J. Prosthet. Dent. 2020, 123, 618–621. [Google Scholar] [CrossRef]
- Prado, A.M.; Pereira, J.; Henriques, B.; Benfatti, C.A.; Magini, R.S.; Lopez-Lopez, J.; Souza, J.C. Biofilm Affecting the Mechanical Integrity of Implant-Abutment Joints. Int. J. Prosthodont. 2016, 29, 381–383. [Google Scholar] [CrossRef]
- Sahin, C.; Ayyildiz, S. Correlation between microleakage and screw loosening at implant-abutment connection. J. Adv. Prosthodont. 2014, 6, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Gumus, H.O.; Zortuk, M.; Albayrak, H.; Dincel, M.; Kocaagaoglu, H.H.; Kilinc, H.I. Effect of fluid contamination on reverse torque values in bone-level implants. Implant. Dent. 2014, 23, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Byrne, D.; Jacobs, S.; O’Connell, B.; Houston, F.; Claffey, N. Preloads generated with repeated tightening in three types of screws used in dental implant assemblies. J. Prosthodont. Implant. Esthet. Reconstr. Dent. 2006, 15, 164–171. [Google Scholar] [CrossRef]
- Alsubaiy, E.F. Abutment screw loosening in implants: A literature review. J. Fam. Med. Prim. Care 2020, 9, 5490–5494. [Google Scholar] [CrossRef] [PubMed]
- Yeo, I.S.; Lee, J.H.; Kang, T.J.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Park, J.M.; Lee, S.Y. The effect of abutment screw length on screw loosening in dental implants with external abutment connections after thermocycling. Int. J. Oral Maxillofac. Implant. 2014, 29, 59. [Google Scholar] [CrossRef]
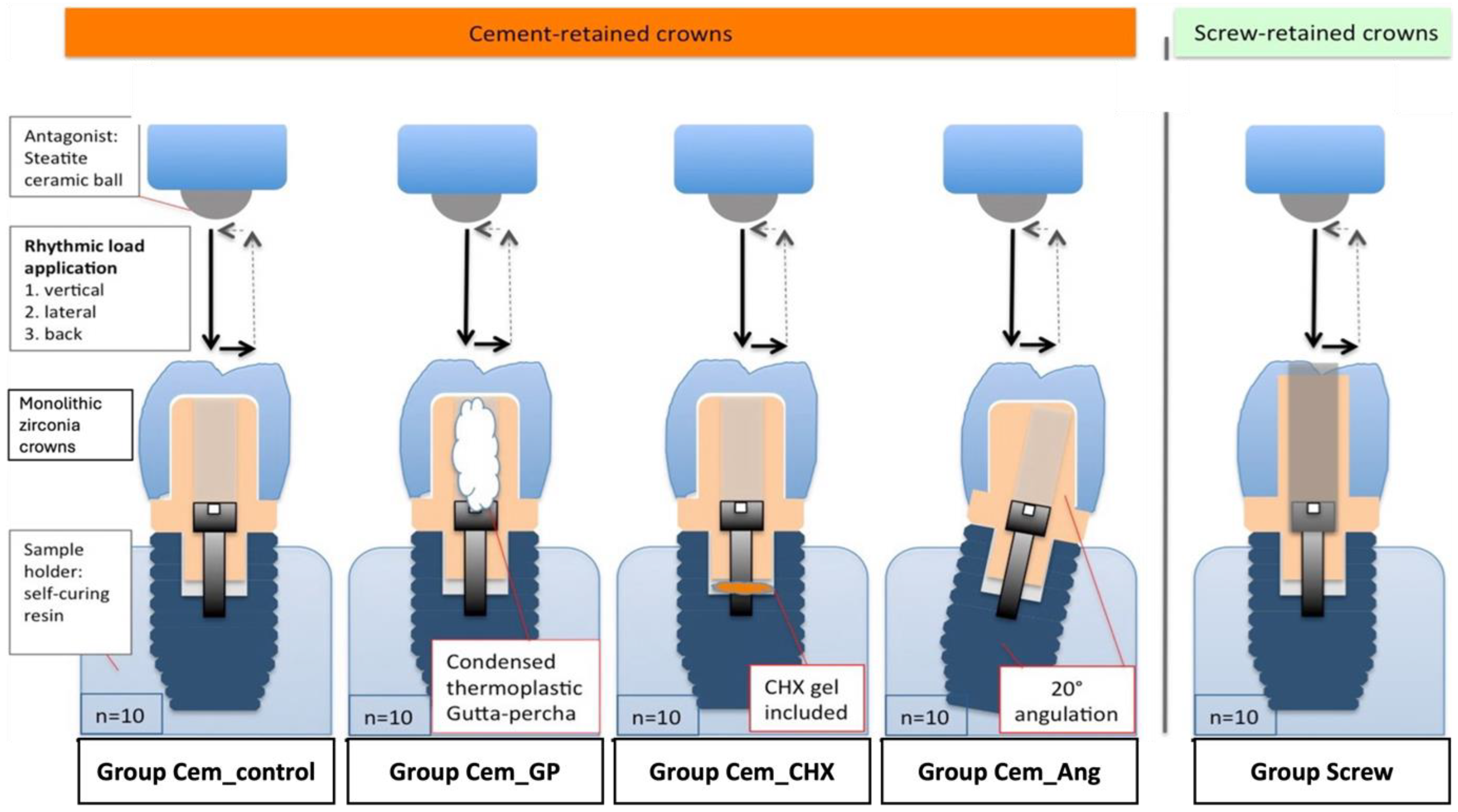


| Group Name | Type of Retention | Implant/Abutment Angulation | Screw Chamber Filling |
|---|---|---|---|
| Cem_control | Cement-retained | straight | No |
| Cem_GP | Cement-retained | straight | Gutta-percha (in screw access hole above the screw |
| Cem_CHX | Cement-retained | straight | Chlorhexidine gel (in screw chamber below the screw) |
| Cem_Ang | Cement-retained | angulated (20°) | No |
| Screw | Screw-retained | straight | No |
| Tested Group | Preloading Screw-In Torque (Ncm) | Postloading Screw-In Torque (Ncm) | Reverse Torque Difference (RTD) | Removal Torque Loss (%) |
|---|---|---|---|---|
| Cem_control | 20.14 ± 0.12 | 17.88 ± 2.16 | 2.26 ± 2.16 | 11.22 ± 10.79% |
| Cem_GP | 20.12 ± 0.09 | 17.90 ± 1.04 | 2.22 ± 1.03 | 11.03 ± 5.12% |
| Cem_CHX | 20.09 ± 0.10 | 17.18 ± 2.57 | 2.91 ± 2.56 | 14.48 ± 13.02% |
| Cem_Ang | 20.08 ± 0.08 | 17.04 ± 1.91 | 3.04 ± 1.91 | 15.13 ± 9.36% |
| Screw | 20.11 ± 0.16 | 15.46 ± 1.77 | 4.65 ± 1.76 | 23.12 ± 8.90% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bishti, S.; Alsagher, M.S.E.; Homa, M.; Wolfart, S.; Tuna, T. Factors Influencing the Screw Stability of Implant-Supported Single Crowns: An In Vitro Study. Materials 2025, 18, 506. https://doi.org/10.3390/ma18030506
Bishti S, Alsagher MSE, Homa M, Wolfart S, Tuna T. Factors Influencing the Screw Stability of Implant-Supported Single Crowns: An In Vitro Study. Materials. 2025; 18(3):506. https://doi.org/10.3390/ma18030506
Chicago/Turabian StyleBishti, Shaza, Mohamad Shams Eddin Alsagher, Martin Homa, Stefan Wolfart, and Taşkın Tuna. 2025. "Factors Influencing the Screw Stability of Implant-Supported Single Crowns: An In Vitro Study" Materials 18, no. 3: 506. https://doi.org/10.3390/ma18030506
APA StyleBishti, S., Alsagher, M. S. E., Homa, M., Wolfart, S., & Tuna, T. (2025). Factors Influencing the Screw Stability of Implant-Supported Single Crowns: An In Vitro Study. Materials, 18(3), 506. https://doi.org/10.3390/ma18030506






