Mechanical Properties of Novel 3D-Printed Restorative Materials for Definitive Dental Applications
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Fabrication
- I.
- Midas, technology: DPS with λ = 385 nm, Sprintray Inc., Los Angeles, CA, USA;
- II.
- Pro 55s, technology: DLP with λ = 405 nm, Sprintray Inc., Los Angeles, CA, USA;
- III.
- Asiga Max, technology: DLP with λ = 385 nm, ASIGA, Sydney, Australia;
- IV.
- TrixPrint2, technology: DLP with λ = 385 nm, DEKEMA, Freilassing, Germany;
- V.
- Varseo XS, technology: DLP with λ = 405 nm, BEGO Bremer Goldschlägerei Wilh. Herbst, Bremen, Germany.
2.2. Artificial Aging
2.3. Flexural Strength with Elastic Modulus
2.4. Martens’ Parameters
2.5. Resonant Frequency Damping Analysis (RFDA)
2.6. Microstructural Analysis
2.7. Statistical Analysis
3. Results
3.1. Impact of Printer Within CCR
3.2. Impact of Printer Within VSC
3.3. Impact of the Resin Within the Asiga Max Printer
3.4. Comparability to the CG
3.5. Method to Assess the Elastic Properties
3.6. Results for Microstructural Analysis (Figure 7, Figure 8 and Figure 9)
4. Discussion
4.1. Impact of Printer
4.2. Impact of the Resin
4.3. Comparability to CG
4.4. Comparability of the Methods to Assess the Elastic Properties
4.5. Limitations and Future Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Balhaddad, A.A.; Garcia, I.M.; Mokeem, L.; Alsahafi, R.; Majeed-Saidan, A.; Albagami, H.H.; Khan, A.S.; Ahmad, S.; Collares, F.M.; Della Bona, A.; et al. Three-dimensional (3D) printing in dental practice: Applications, areas of interest, and level of evidence. Clin. Oral. Investig. 2023, 27, 2465–2481. [Google Scholar] [CrossRef]
- Caussin, E.; Moussally, C.; Le Goff, S.; Fasham, T.; Troizier-Cheyne, M.; Tapie, L.; Dursun, E.; Attal, J.-P.; François, P. Vat photopolymerization 3D printing in dentistry: A comprehensive review of actual popular technologies. Materials 2024, 17, 950. [Google Scholar] [CrossRef]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W.; Revilla-León, M. 3D printing parameters, supporting structures, slicing, and post-processing procedures of vat-polymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3D printing technique and its challenges. Bioact. Mater. 2020, 5, 110–115. [Google Scholar] [CrossRef]
- Nomoto, R. Effect of light wavelength on polymerization of light-cured resins. Dent. Mater. J. 1997, 16, 60–73. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D printing and customized additive manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef]
- Nejat, A.H. Overview of Current Dental Ceramics. Dent. Clin. 2024, 69, 155–171. [Google Scholar] [CrossRef]
- Duarte, S., Jr.; Phark, J.H. Advances in Dental Restorations: A Comprehensive Review of Machinable and 3D-Printed Ceramic-Reinforced Composites. J. Esthet. Restor. Dent. 2025, 37, 257–276. [Google Scholar] [CrossRef] [PubMed]
- Lankes, V.; Reymus, M.; Mayinger, F.; Coldea, A.; Liebermann, A.; Hoffmann, M.; Stawarczyk, B. Three-dimensional printed resin: Impact of different cleaning protocols on degree of conversion and tensile bond strength to a composite resin using various adhesive systems. Materials 2023, 16, 3580. [Google Scholar] [CrossRef] [PubMed]
- Jin, G.; Gu, H.; Jang, M.; Bayarsaikhan, E.; Lim, J.-H.; Shim, J.-S.; Lee, K.-W.; Kim, J.-E. Influence of postwashing process on the elution of residual monomers, degree of conversion, and mechanical properties of a 3D printed crown and bridge materials. Dent. Mater. 2022, 38, 1812–1825. [Google Scholar] [CrossRef] [PubMed]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Dai, J.; Lio, K.; Liu, Q.; Unikovskiy, A.; Spintzyk, S.; Xu, S.; Li, P. Post-processing of a 3D-printed denture base polymer: Impact of a centrifugation method on the surface characteristics, flexural properties, and cytotoxicity. J. Dent. 2024, 147, 105102. [Google Scholar] [CrossRef]
- Katheng, A.; Prawatvatchara, W.; Tonprasong, W.; Namano, S.; Kongkon, P. Effect of postrinsing times and methods on surface roughness, hardness, and polymerization of 3d-printed photopolymer resin. Eur. J. Dent. 2025, 19, 154–164. [Google Scholar] [CrossRef]
- Short, D.; Sirinterlikci, A.; Badger, P.; Artieri, B. Environmental, health, and safety issues in rapid prototyping. Rapid Prototyp. J. 2015, 21, 105–110. [Google Scholar] [CrossRef]
- Celikel, P.; Sengul, F. Investigating the impact of post-curing cycles on surface hardness and color stability in 3D printed resin crowns. Odontology 2025, 113, 156–162. [Google Scholar] [CrossRef]
- Li, P.; Lambart, A.-L.; Stawarczyk, B.; Reymus, M.; Spintzyk, S. Postpolymerization of a 3D-printed denture base polymer: Impact of post-curing methods on surface characteristics, flexural strength, and cytotoxicity. J. Dent. 2021, 115, 103856. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of postcuring temperature on the mechanical properties and biocompatibility of three-dimensional printed dental resin material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Lassila, L.; Mangoush, E.; He, J.; Vallittu, P.K.; Garoushi, S. Effect of post-printing conditions on the mechanical and optical properties of 3D-printed dental resin. Polymers 2024, 16, 1713. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging—An in vitro study. Clin. Oral. Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Evaluation of the mechanical properties and degree of conversion of 3D printed splint material. J. Mech. Behav. Biomed. Mater. 2021, 115, 104254. [Google Scholar] [CrossRef]
- Hassanpour, M.; Narongdej, P.; Alterman, N.; Moghtadernejad, S.; Barjasteh, E. Effects of Post-Processing Parameters on 3D-Printed Dental Appliances: A Review. Polymers 2024, 16, 2795. [Google Scholar] [CrossRef]
- Lim, J.-H.; Lee, S.-Y.; Gu, H.; Jin, G.; Kim, J.-E. Evaluating oxygen shielding effect using glycerin or vacuum with varying temperature on 3D printed photopolymer in post-polymerization. J. Mech. Behav. Biomed. Mater. 2022, 130, 105170. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef]
- Finck, N.S.; Fraga, M.A.A.; Correr, A.B.; Dalmaschio, C.J.; Rodrigues, C.S.; Moraes, R.R. Effects of solvent type and UV post-cure time on 3D-printed restorative polymers. Dent. Mater. 2024, 40, 451–457. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Durán Urdiales, D.; Benalcázar Arias, M.V.; Córdova, A.K.; Medina, M.S.; Bravo Torres, W. Flexural Strength, Fatigue Behavior, and Microhardness of Three-Dimensional (3D)-Printed Resin Material for Indirect Restorations: A Systematic Review. Materials 2025, 18, 556. [Google Scholar] [CrossRef] [PubMed]
- Zattera, A.C.A.; Morganti, F.A.; de Souza Balbinot, G.; Della Bona, A.; Collares, F.M. The influence of filler load in 3D printing resin-based composites. Dent. Mater. 2024, 40, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Gekle, S.; Mayinger, F.; Kreitmair, U.; Reymus, M.; Hoffmann, M.; Stawarczyk, B. Impact of different post-polymerization protocols on polymerization depth, degree of conversion, hardness, flexural strength and elastic modulus of 3D-printed objects. J. Mech. Behav. Biomed. Mater. 2025, 172, 107164. [Google Scholar]
- Shortall, A.; Palin, W.; Burtscher, P. Refractive index mismatch and monomer reactivity influence composite curing depth. J. Dent. Res. 2008, 87, 84–88. [Google Scholar] [CrossRef]
- Leprince, J.; Hadis, M.; Shortall, A.; Ferracane, J.; Devaux, J.; Leloup, G.; Palin, W. Photoinitiator type and applicability of exposure reciprocity law in filled and unfilled photoactive resins. Dent. Mater. 2011, 27, 157–164. [Google Scholar] [CrossRef]
- Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D printed materials for permanent restorations in indirect restorative and prosthetic dentistry: A critical review of the literature. Materials 2024, 17, 1380. [Google Scholar] [CrossRef]
- Liang, X.; Yu, B.; Dai, Y.; Wang, Y.; Hu, M.; Zhong, H.-J.; He, J. Three-Dimensional Printing Resin-Based Dental Provisional Crowns and Bridges: Recent Progress in Properties, Applications, and Perspectives. Materials 2025, 18, 2202. [Google Scholar] [CrossRef] [PubMed]
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical properties of 3D-printed and milled composite resins for definitive restorations: An in vitro comparison of initial strength and fatigue behavior. J. Esthet. Restor. Dent. 2024, 36, 391–401. [Google Scholar] [CrossRef]
- Rosentritt, M.; Rauch, A.; Hahnel, S.; Schmidt, M. In-vitro performance of subtractively and additively manufactured resin-based molar crowns. J. Mech. Behav. Biomed. Mater. 2023, 141, 105806. [Google Scholar] [CrossRef] [PubMed]
- Gale, M.; Darvell, B. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Li, P.; Kraemer-Fernandez, P.; Klink, A.; Xu, Y.; Spintzyk, S. Repairability of a 3D printed denture base polymer: Effects of surface treatment and artificial aging on the shear bond strength. J. Mech. Behav. Biomed. Mater. 2021, 114, 104227. [Google Scholar] [CrossRef]
- Geiger, V.; Mayinger, F.; Hoffmann, M.; Reymus, M.; Stawarczyk, B. Fracture toughness, work of fracture, flexural strength and elastic modulus of 3D-printed denture base resins in two measurement environments after artificial aging. J. Mech. Behav. Biomed. Mater. 2024, 150, 106234. [Google Scholar] [CrossRef] [PubMed]
- Radovic, M.; Lara-Curzio, E.; Riester, L. Comparison of different experimental techniques for determination of elastic properties of solids. Mater. Sci. Eng. A 2004, 368, 56–70. [Google Scholar] [CrossRef]
- Suansuwan, N. Swain Determination of elastic properties of metal alloys dental porcelains. J. Oral. Rehabil. 2001, 28, 133–139. [Google Scholar] [CrossRef]
- ASTM E1876-22; Standard Test Method for Dynamic Young’s Modulus, Shear Modulus, and Poisson’s Ratio by Impulse Excitation of Vibration. ASTM International: West Conshohocken, PA, USA, 2022; p. 19.
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Bütikofer, L.; Stawarczyk, B.; Roos, M. Two regression methods for estimation of a two-parameter Weibull distribution for reliability of dental materials. Dent. Mater. 2015, 31, e33–e50. [Google Scholar] [CrossRef]
- Borella, P.S.; Alvares, L.A.; Ribeiro, M.T.; Moura, G.F.; Soares, C.J.; Zancope, K.; Mendonça, G.; Rodrigues, F.P.; das Neves, F.D. Physical and mechanical properties of four 3D-printed resins at two different thick layers: An in vitro comparative study. Dent. Mater. 2023, 39, 686–692. [Google Scholar] [CrossRef]
- Bao, Y. Recent trends in advanced photoinitiators for vat photopolymerization 3D printing. Macromol. Rapid Commun. 2022, 43, 2200202. [Google Scholar] [CrossRef]
- Price, R.B. Light curing in dentistry. Dent. Clin. 2017, 61, 751–778. [Google Scholar] [CrossRef]
- Rodríguez, H.A.; Kriven, W.M.; Casanova, H. Development of mechanical properties in dental resin composite: Effect of filler size and filler aggregation state. Mater. Sci. Eng. C 2019, 101, 274–282. [Google Scholar] [CrossRef]
- Rudenko, Y.; Lozovaya, A.; Asanova, L.; Fedyakova, N.; Chapala, P. Light intensity influence on critical energy and penetration depth for vat photopolymerization technology. Prog. Addit. Manuf. 2024, 9, 553–561. [Google Scholar] [CrossRef]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Alshamrani, A.; Alhotan, A.; Kelly, E.; Ellakwa, A. Mechanical and biocompatibility properties of 3D-printed dental resin reinforced with glass silica and zirconia nanoparticles: In vitro study. Polymers 2023, 15, 2523. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.-F.; Migonney, V.; Ruse, N.D.; Sadoun, M. Resin composite blocks via high-pressure high-temperature polymerization. Dent. Mater. 2012, 28, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of flexural strength of different CAD/CAM PMMA-based polymers. J. Prosthodont. 2019, 28, e491–e495. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Donmez, M.B.; de Paula, M.S.; Akay, C.; Fonseca, M.; Kahveci, Ç.; Abou-Ayash, S.; Yilmaz, B. Surface roughness, optical properties, and microhardness of additively and subtractively manufactured CAD--CAM materials after brushing and coffee thermal cycling. J. Prosthodont. 2025, 34, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Miljojković, J.; Bijelić, I.; Vranić, N.; Radovanović, N.; Živković, M. Determining elastic modulus of the material by measuring the deflection of the beam loaded in bending. Teh. Vjesn. 2017, 24, 1227–1234. [Google Scholar] [CrossRef]




| Resin | Abbreviation | Manufacturer | Lot No. | Cleaning Protocol | Post-Polymerization Protocol |
|---|---|---|---|---|---|
| Ceramic Crown | CCR | SprintRay Inc., Los Angeles, CA, USA | M24K008 (Midas) S24D012 (Pro 55s) | Brush + isopropyl alcohol (99.7%. SAV Liquid ProductionFlintsbach am Inn, Germany), 30 s. Dried with an air syringe. | Pro Cure (SprintRay), 365 + 385 nm. Ceramic Crown curing program. Normal mode |
| 3Delta Crown | DCR | DeltaMed, Friedberg, Germany | 240403A | Centrifugation (Multifuge 1 S-R; Heraeus. Hanau, Germany), 1500 rpm, 2 min, and 20 °C. | Otoflash G171 (NK Optik. Baierbrunn. Germany). 12.5 mW/cm2 per flash 360–410 nm, 2 × 2000 flashes. Nitrogen atmosphere. A total of 2000 flashes each side. |
| Bridgetec | BRT | Saremco Dental, Rebstein, Switzerland | 280824-01 | Ethanol-soaked cloth (96%. Otto Fischar. Saarbrücken, Germany). Dried with an air syringe. | |
| Crowntec | CRT | F493 | |||
| Freeprint Crown | FCR | DETAX, Ettlingen, Germany | 270805 | Ultrasonic bath (DT 31 H. BANDELIN. Berlin, Germany) + isopropyl alcohol (99.7%. SAV Liquid Production. Flintsbach am Inn, Germany), 2 × 1 min. Dried with an air syringe. | |
| VarseoSmile triniQ | VST | BEGO Bremer Goldschlägerei Wilh. Herbst, Bremen, Germany | n.a. | Ultrasonic bath (DT 31 H. BANDELIN. Berlin, Germany) + ethanol (96%. Otto Fischar. Saarbrücken, Germany), 3 min precleaning and 2 min final cleaning. Dried with an air syringe. | |
| VarseoSmile Crown Plus | VSC | 601758 | Otoflash G171 (NK Optik. Baierbrunn. Germany), 12.5 mW/cm2 per flash 360–410 nm, and 2 × 1500 flashes. Nitrogen atmosphere. A total of 1500 flashes each side. |
| CCR | DCR | BRT | CRT | FCR | VST | VSC | VSC | BRC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Midas | Pro 55s | Asiga Max | TrixPrint2 | Varseo XS | - | |||||||
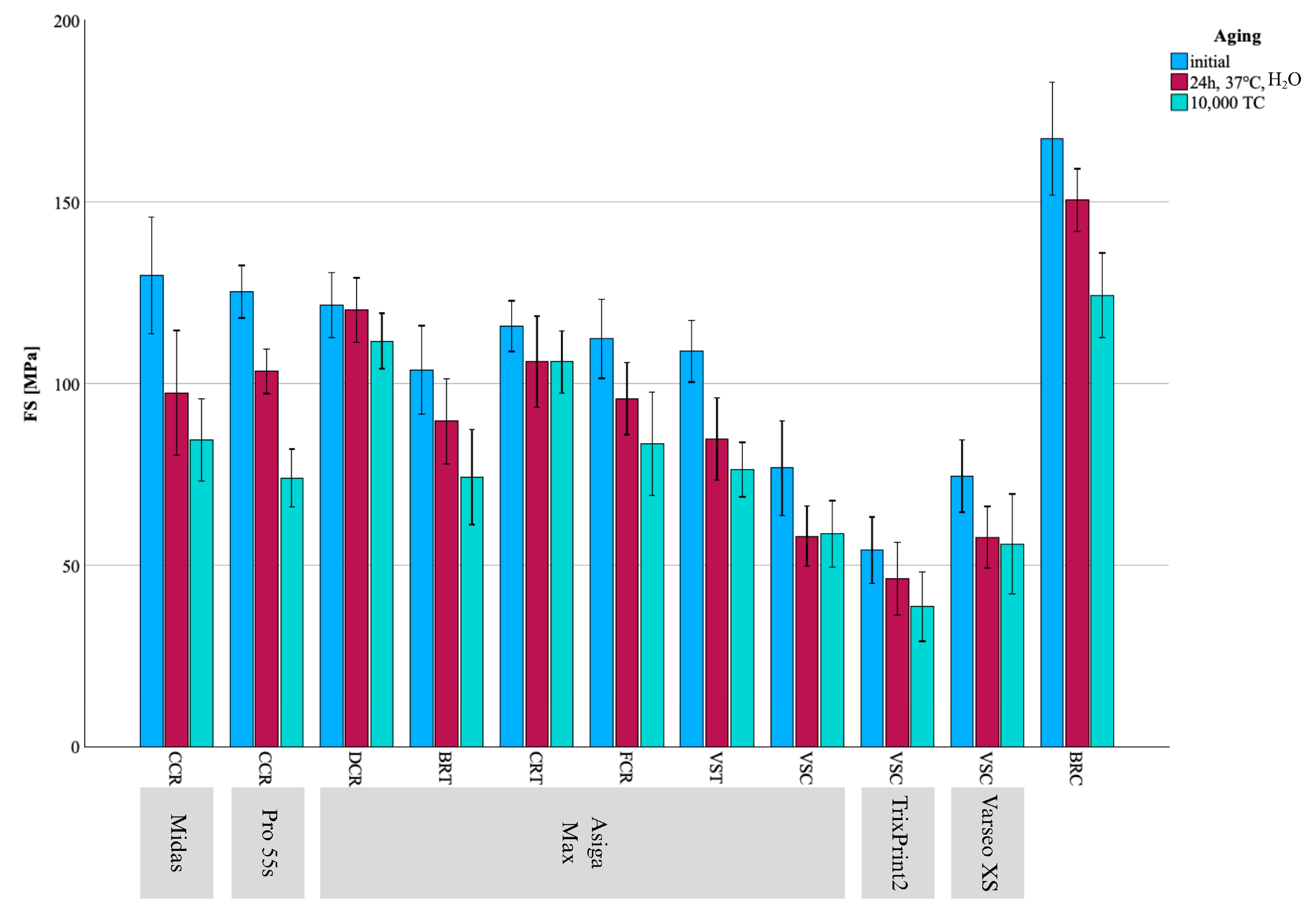
| FS [MPa] Mean ± SD | Initial | 130 ± 16.1 AIy | 125 ± 7.26 AIz | 122 ± 8.91 dIy | 104 ± 12.2 bIz | 116 ± 6.97 cdIy | 112 ± 10.9 bcdIz | 109 ± 8.49 bcIz | 77 ± 13.0 BaIy | 54 ± 9.17 *AIy | 74 ± 9.92 BIy | 167 ± 15.5 IIz |
| 24 h, H2O | 97.4 ± 17.2 AIx | 103 A ± 6.14 AIy | 120 ± 8.86 dIy | 89.6 ± 11.8 bIy | 106 ± 12.6 *cIx | 95.9 ± 10.0 bcIy | 84.7 ± 11.3 bIy | 58.0 ± 8.3 BaIx | 46.3 ± 10.0 *AIxy | 57.6 ± 8.56 BIx | 151 ± 8.68 IIy | |
| 10,000 TC | 84.5 ± 11.4 BIx | 74.0 ± 7.94 AIx | 112 ± 7.62 cIIx | 74.3 ± 13.2 bIx | 106 ± 8.62 cIIx | 83.4 ± 14.2 bIx | 76.3 ± 7.54 bIx | 58.5 ± 9.15 BaIx | 38.6 ± 9.59 AIx | 55.8 ± 13.8 *BIx | 124 ± 11.7 IIx | |
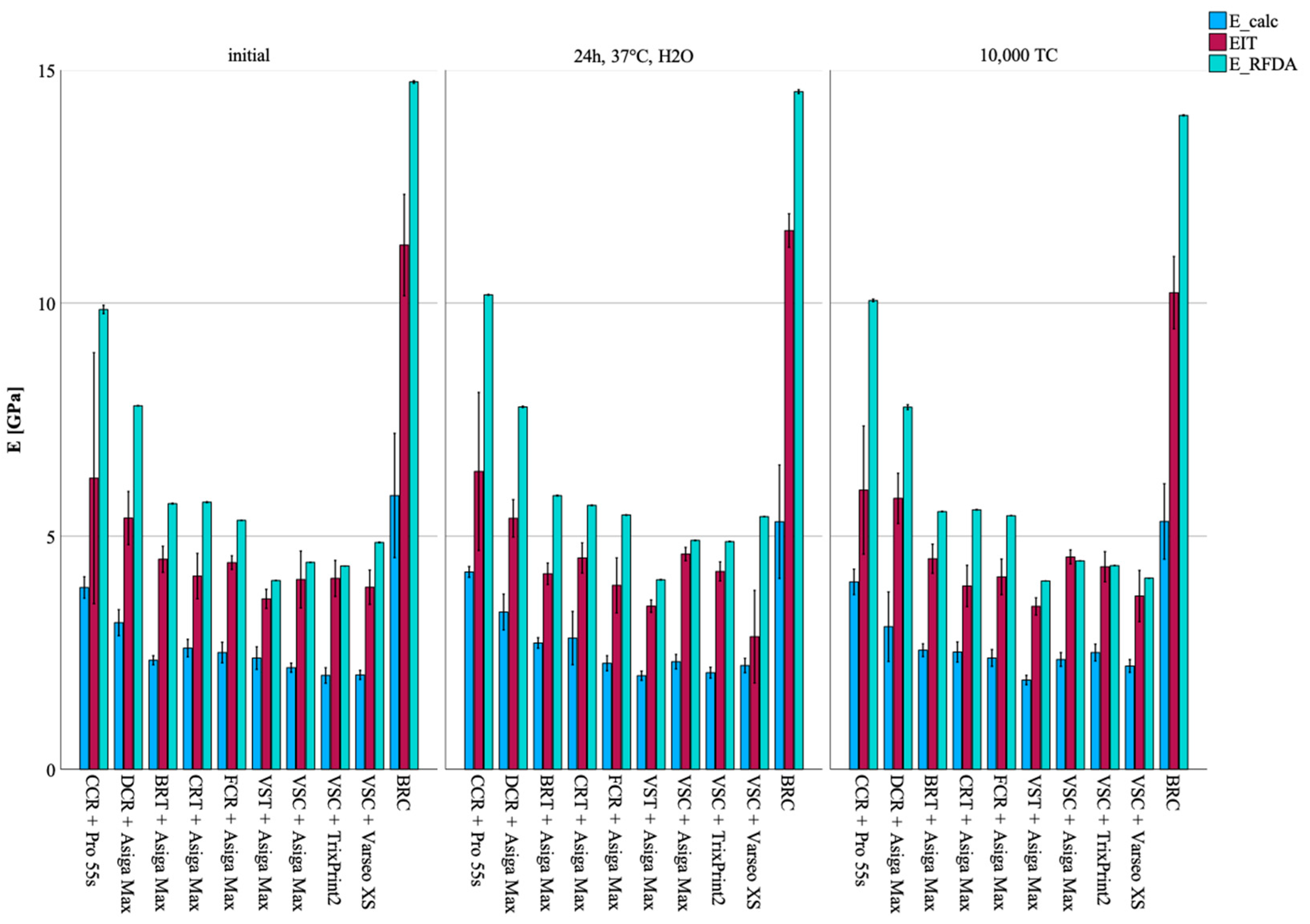
| E_calc [GPa] Mean ± SD | Initial | 5.35 ± 0.63 BIIx | 3.99 ± 0.38 AIx | 3.03 ± 0.33 cIx | 2.32 ± 0.11 *abIx | 2.43 ± 0.26 abIx | 2.63 ± 0.23 bIy | 2.54 ± 0.46 abIy | 2.23 ± 0.15 BaIx | 1.93 ± 0.13 AIx | 1.99 ± 0.17 AIx | 5.89 ± 1.06 IIx |
| 24 h, H2O | 5.73 ± 0.50 BIIx | 4.06 ± 0.34 *AIx | 3.32 ± 0.33 cIx | 2.61 ± 0.20 bIy | 2.69 ± 0.37 *bIy | 2.29 ± 0.17 aIx | 2.03 ± 0.10 aIx | 2.28 ± 0.15 *BaIx | 2.11 ± 0.12 AIy | 2.22 ± 0.26 ABIy | 5.67 ± 0.94 IIx | |
| 10,000 TC | 5.33 ± 0.52 BIIx | 4.02 ± 0.27 AIx | 3.29 ± 0.50 cIx | 2.57 ± 0.12 bIy | 2.53 ± 0.27 bIxy | 2.44 ± 0.21 bIx | 1.91 ± 0.10 aIx | 2.36 ± 0.16 BbIx | 2.40 ± 0.24 BIz | 2.12 ± 0.20 AIxy | 5.22 ± 0.63 IIx | |
| m (95%CI) | Initial | 9.5 (5; 16) | 19.9 (12; 33) | 15.8 (9; 26) | 9.6 (5; 16) | 19.7 (11; 33) | 11.8 (7; 20) | 15.0 (9; 25) | 6.6 (4; 11) | 7.9 (4; 14) | 8.6 (5; 15) | 12.3 (7; 21) |
| 24 h, H2O | 6.8 (3; 11) | 20.7 (13; 24) | 15.8 (9; 27) | 8.7 (5; 15) | 9.4 (5; 16) | 11.2 (6; 19) | 8.4 (5; 14) | 8.3 (5; 14) | 5.6 (3; 10) | 7.8 (4; 13) | 20.2 (12; 33) | |
| 10,000 TC | 8.9 (5; 14) | 10.7 (6; 18) | 18.0 (10; 30) | 6.4 (3; 11) | 14.4 (8; 24) | 6.9 (4; 12) | 11.6 (7; 20) | 7.6 (4; 13) | 5.0 (3; 9) | 5.6 (3; 10) | 12.9 (7; 22) | |
| CCR | DCR | BRT | CRT | FCR | VST | VSC | VSC | BRC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Midas | Pro 55s | Asiga Max | TrixPrint2 | Varseo XS | - | |||||||
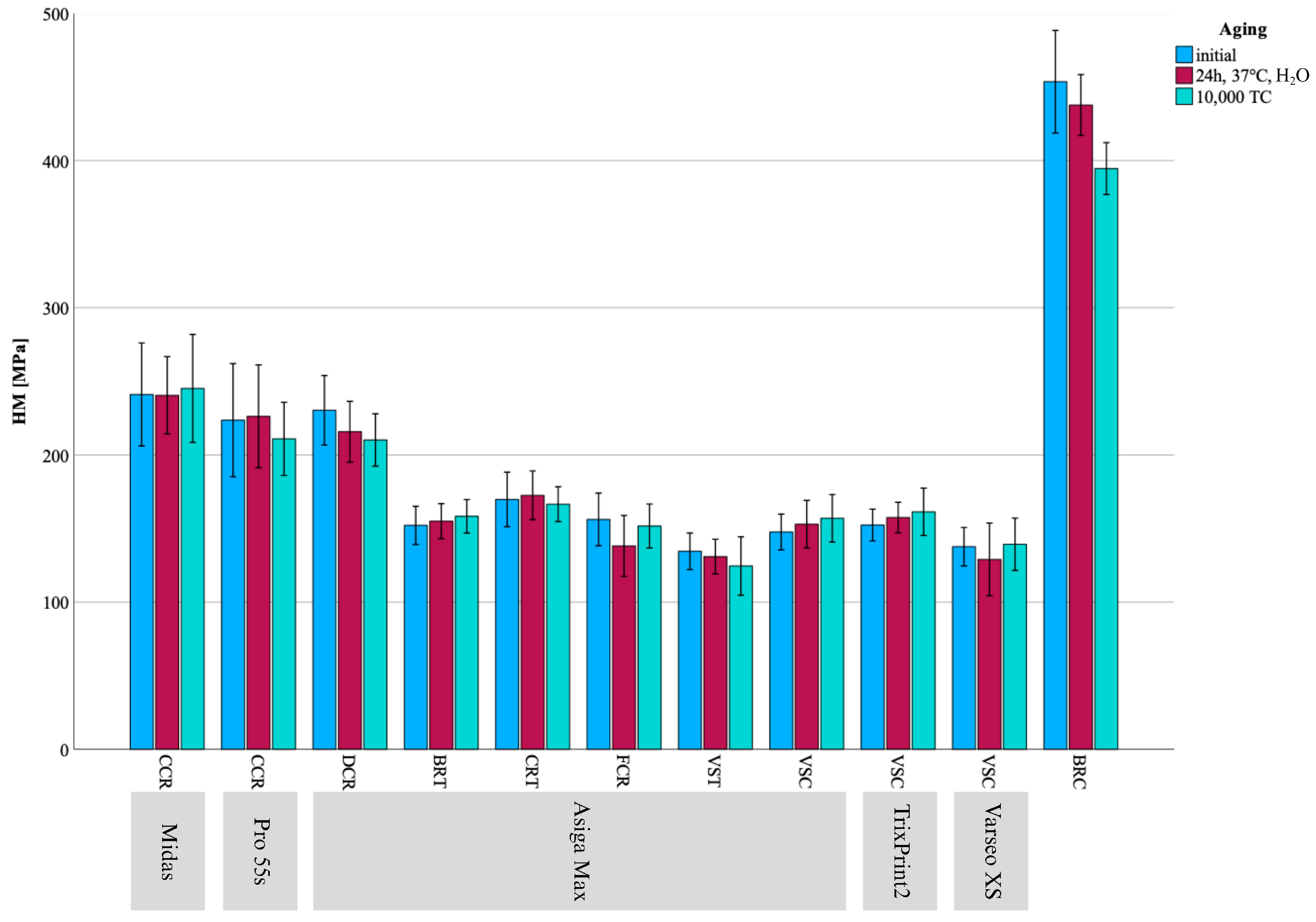
| HM [MPa] Mean ± SD | Initial | 241 ± 345.0 AIx | 224 ± 38.4 AIx | 230 ± 23.6 dIy | 152 ± 13.0 abcIx | 170 ± 18.5 cIx | 156 ± 17.9 bcIx | 135 ± 12.4 aIx | 148 ± 12.2 ABabIx | 152 ± 10.8 BIx | 138 ± 13.0 AIx | 453 ± 34.8 IIy |
| 24 h, H2O | 241 ± 26.2 AIx | 226 ± 34.9 AIx | 216 ± 20.6 dIxy | 155 ± 11.9 bcIx | 173 ± 16.5 cIx | 173 ± 20.7 abIy | 138 ± 11.8 aIx | 153 ± 16.2 BbIx | 157 ± 10.4 *BIx | 129 ± 24.7 AIx | 438 ± 20.7 IIy | |
| 10,000 TC | 245 ± 36.7 BIx | 211 ± 24.8 *AIx | 210 ± 17.8 cIx | 158 ± 11.4 bIx | 167 ± 11.8 bIx | 152 ± 14.9 bIx | 125 ± 19.9 *aIx | 157 ± 16.2 *BbIx | 161 ± 16.1 BIx | 139 ± 17.8 AIx | 394 ± 17.6 IIx | |
| EIT [GPa] Mean ± SD | Initial | 7.40 ± 1.40 AIx | 6.63 ± 1.73 AIx | 5.74 ± 0.66 cIx | 4.37 ± 0.39 bIx | 4.15 ± 0.46 abIx | 4.33 ± 0.39 bIy | 3.65 ± 0.28 aIy | 4.21 ± 0.43 *BbIx | 4.16 ± 0.33 *BIx | 3.70 ± 0.44 AIx | 11.9 ± 1.02 IIy |
| 24 h, H2O | 7.46 ± 0.86 BIx | 6.71 ± 1.47 AIx | 5.40 ± 0.62 cIx | 4.34 ± 0.31 bIx | 4.20 ± 0.59 bIx | 3.88 ± 0.52 abIx | 3.54 ± 0.25 aIxy | 4.37 ± 0.40 BbIx | 4.34 ± 0.22 BIx | 3.28 ± 0.75 AIx | 11.5 ± 0.47 IIy | |
| 10,000 TC | 7.35 ± 1.58 BIx | 6.01 ± 1.19 AIx | 5.62 ± 0.52 dIx | 4.49 ± 0.27 cIx | 3.94 ± 0.51 bIx | 4.00 ± 0.52 bcIxy | 3.30 ± 0.50 *aIx | 4.39 ± 0.37 BbcIx | 4.28 ± 0.40 *BIx | 3.47 ± 0.62 AIx | 10.6 ± 0.62 IIx | |
| CCR | DCR | BRT | CRT | FCR | VST | VSC | VSC | BRC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Midas | Pro 55s | Asiga Max | TrixPrint2 | Varseo XS | - | |||||||
| E_RFDA [GPa] Min/Med/Max 95%CI | Initial | - | 9.68/9.89/9.92 *Ix | 7.79/7.80/7.80 *fIy | 5.69/5.70/5.71 dIy | 5.72/5.73/5.74 eIz | 5.34/5.34/5.34 *cIx | 4.05/4.05/4.05 *aIy | 4.44/4.44/4.44 AbIx | 4.63/4.63/4.63 *BIy | 4.86/4.87/4.88 CIy | 14.73/14.73/14.80 *IIz |
| 24 h, H2O | - | 10.2/10.2/10.2 Iz | 7.76/7.77/7.79 fIx | 5.86/5.87/5.88 eIz | 5.66/5.66/5.67 *dIy | 5.45/5.46/5.46 cIz | 4.06/4.07/4.07 aIz | 4.91/4.91/4.92 *BbIz | 4.88/4.89/4.89 AIz | 5.42/5.42/5.42 CIz | 14.5/14.5/14.6 IIy | |
| 10,000 TC | - | 10.0/10.1/10.1 Iy | 7.66/7.79/7.80 *fIx | 5.52/5.53/5.53 *aIx | 5.56/5.57/5.57 *eIx | 5.44/5.44/5.44 dIy | 4.04/4.04/4.04 *bIx | 4.47/4.47/4.47 CcIy | 4.37/4.37/4.37 Bix | 4.10/4.10/4.10 Aix | 14.0/14.0/14.0 IIx | |
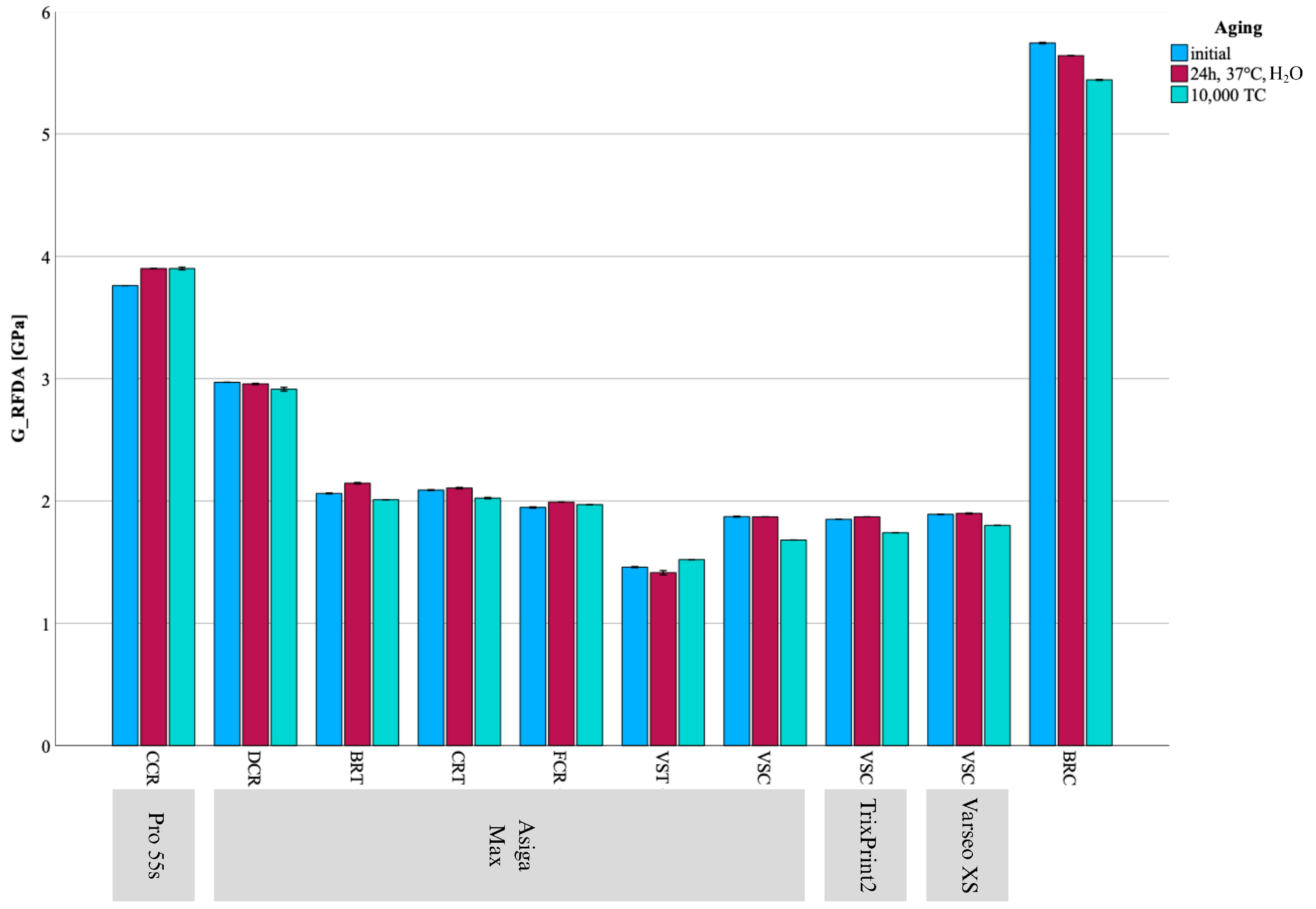
| G_RFDA [GPa] Min/Med/Max 95%CI | Initial | - | 3.76/3.76/3.76 *Ix | 2.97/2.97/2.97 *fIz | 2.06/2.06/2.07 *dIy | 2.08/2.09/2.09 *eIy | 1.94/1.95/1.95 *cIx | 1.45/1.46/1.46 *aIy | 1.87/1.87/1.88 *BbIy | 1.85/1.85/1.85 *AIy | 1.89/1.89/1.89 CIy | 5.74/5.74/5.75 *IIz |
| 24 h, H2O | - | 3.90/3.90/3.90 Iy | 2.95/2.96/2.96 *fIy | 2.14/2.15/2.15 eIz | 2.10/2.11/2.11 dIz | 1.99/1.99/1.99 cIz | 1.39/1.42/1.44 aIx | 1.87/1.87/1.87 AbIy | 1.87/1.87/1.87 AIz | 1.89/1.90/1.90 *BIz | 5.64/5.64/5.64 IIy | |
| 10,000 TC | - | 3.89/3.90/3.91 Iy | 2.90/2.91/2.93 fIx | 2.01/2.01/2.01 dIx | 2.02/2.02/2.03 *eIx | 1.97/1.97/1.97 cIy | 1.52/1.52/1.52 *aIz | 1.68/1.68/1.68 *AbIx | 1.74/1.74/1.74 *Bix | 1.80/1.80/1.80 *CIx | 5.44/5.44/5.45 *IIx | |
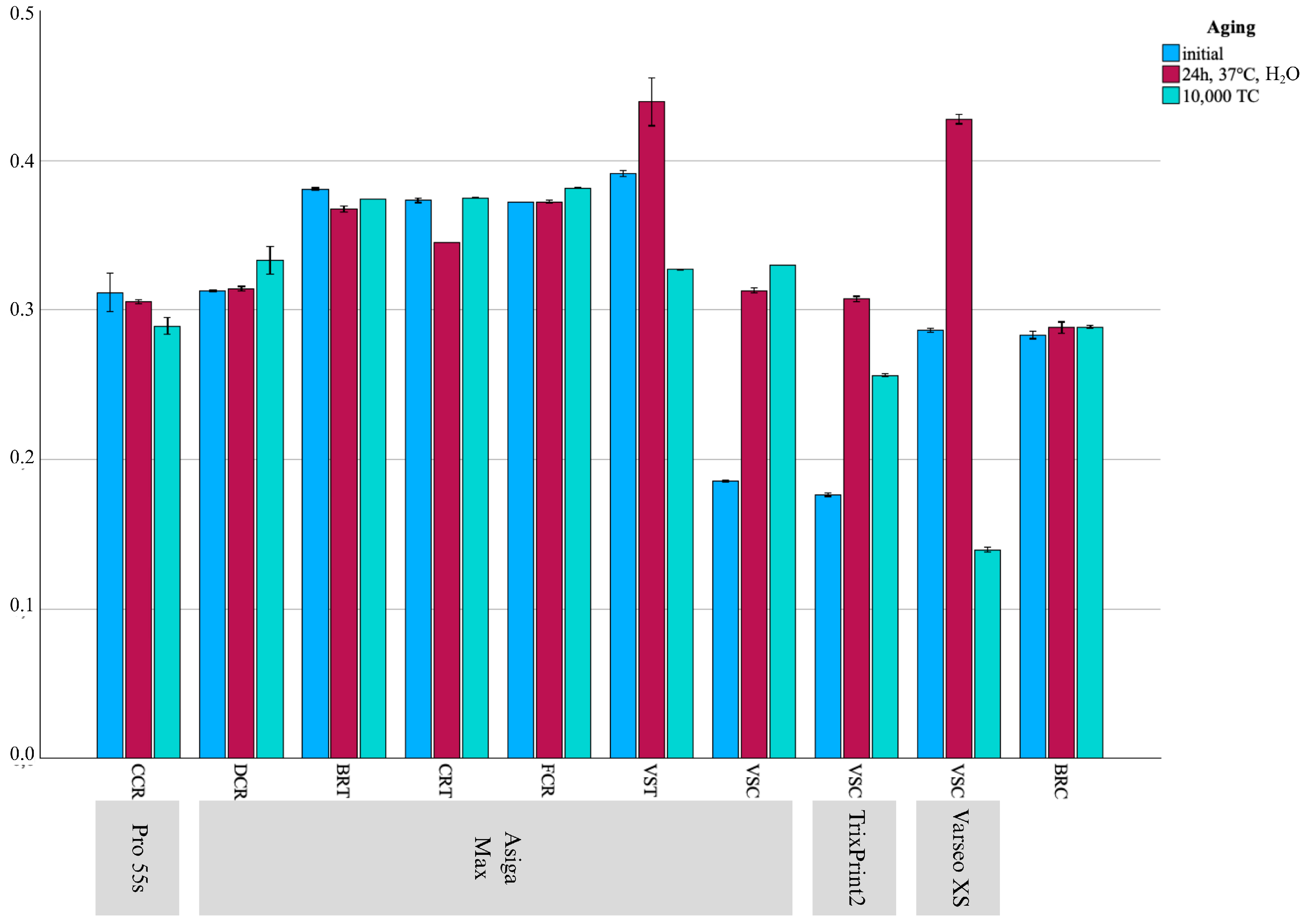
| ν | Initial | - | 0.290/0.316/0.320 *Iy | -/0.313/- *bIx | -/0.381/- *dIz | 0.370/0.373/0.380 cIy | -/0.372/- *cIx | -/0.392/- eIy | -/0.186/- *BaIx | -/0.176/- Aix | -/0.286/- CIy | 0.280/0.282/0.290 *IIx |
| 24 h, H2O | - | 0.300/0.306/0.310 Iy | 0.310/0.314/0.320 aIy | -/0.368/- cIx | -/0.345/- bIx | -/0.372/- dIx | 0.410/0.439/0.460 eIz | 0.310/0.313/0.320 BaIy | 0.300/0.308/0.310 AIz | -/0.427/- *CIz | -/0.287/- IIy | |
| 10,000 TC | - | 0.280/0.289/0.300 x | 0.320/0.331/0.340 bIz | -/0.374/- cIy | -/0.375/- dIz | -/0.382/- *eIy | -/0.327/- * aIx | 0.330/0.330/0.330 CbIz | -/0.256/- BIy | -/0.142/- Aix | -/0.289/- *IIz | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoffmann, M.; Coldea, A.; Stawarczyk, B. Mechanical Properties of Novel 3D-Printed Restorative Materials for Definitive Dental Applications. Materials 2025, 18, 4662. https://doi.org/10.3390/ma18204662
Hoffmann M, Coldea A, Stawarczyk B. Mechanical Properties of Novel 3D-Printed Restorative Materials for Definitive Dental Applications. Materials. 2025; 18(20):4662. https://doi.org/10.3390/ma18204662
Chicago/Turabian StyleHoffmann, Moritz, Andrea Coldea, and Bogna Stawarczyk. 2025. "Mechanical Properties of Novel 3D-Printed Restorative Materials for Definitive Dental Applications" Materials 18, no. 20: 4662. https://doi.org/10.3390/ma18204662
APA StyleHoffmann, M., Coldea, A., & Stawarczyk, B. (2025). Mechanical Properties of Novel 3D-Printed Restorative Materials for Definitive Dental Applications. Materials, 18(20), 4662. https://doi.org/10.3390/ma18204662








