3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature
Abstract
:1. Introduction
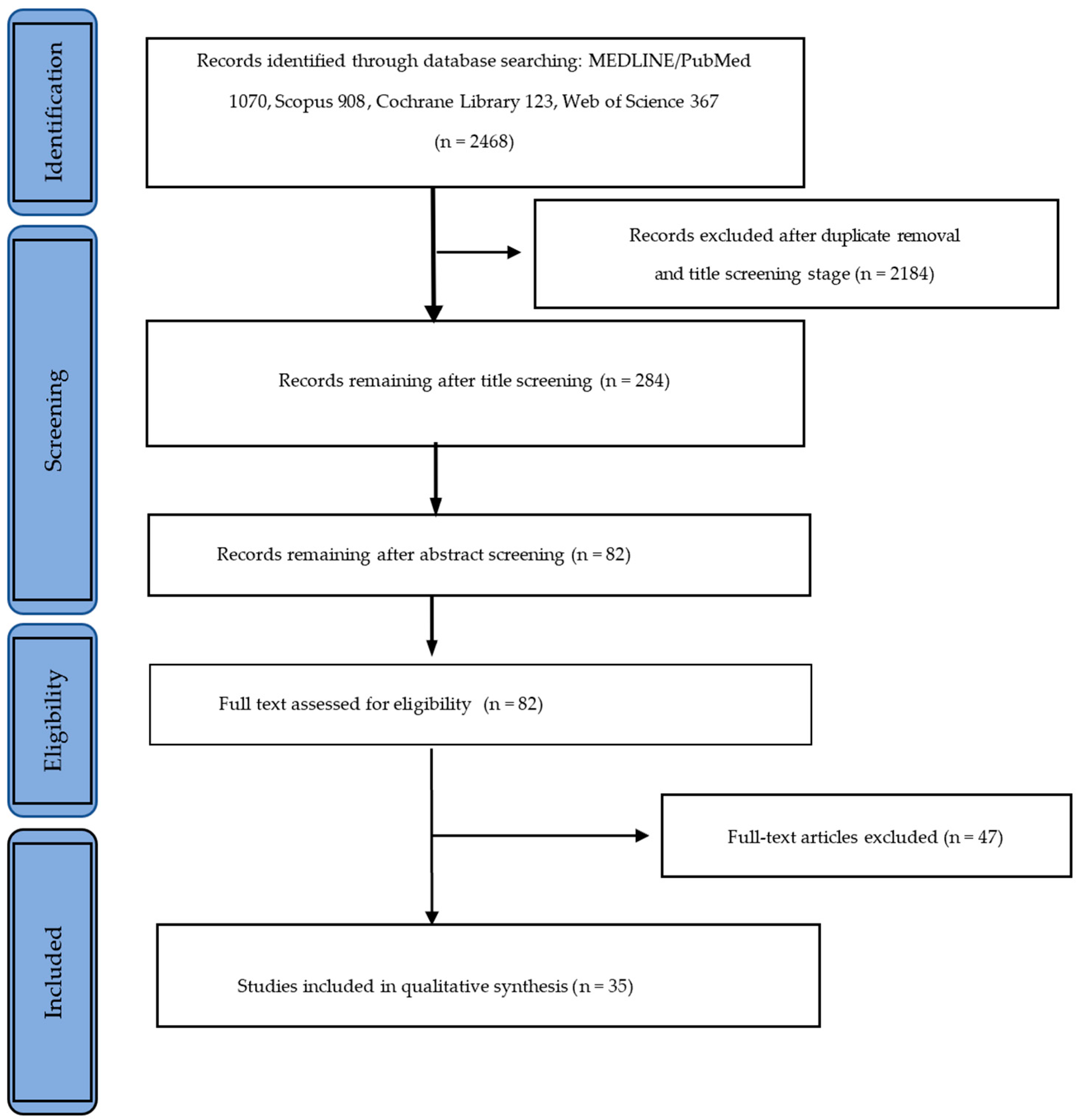
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Information Sources and Research Strategies
2.3. Sources of Evidence Selection
3. Results
3.1. Mechanical Properties
3.2. Dimensional Accuracy and Fit
3.3. Aesthetic Properties
3.4. Biological Properties
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D Printing Restorative Materials Using a Stereolithographic Technique: A Systematic Review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Dawood, A.; Marti Marti, B.; Sauret-Jackson, V.; Darwood, A. 3D Printing in Dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry-State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Liaw, C.-Y.; Guvendiren, M. Current and Emerging Applications of 3D Printing in Medicine. Biofabrication 2017, 9, 024102. [Google Scholar] [CrossRef] [PubMed]
- Bhargav, A.; Sanjairaj, V.; Rosa, V.; Feng, L.W.; Fuh Yh, J. Applications of Additive Manufacturing in Dentistry: A Review. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 2058–2064. [Google Scholar] [CrossRef] [PubMed]
- Vandenberghe, B. The Crucial Role of Imaging in Digital Dentistry. Dent. Mater. 2020, 36, 581–591. [Google Scholar] [CrossRef]
- Alammar, A.; Kois, J.C.; Revilla-León, M.; Att, W. Additive Manufacturing Technologies: Current Status and Future Perspectives. J. Prosthodont. 2022, 31, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applications in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Wilkins, G.N. 3D printing in dentistry—Exploring the new horizons. J. Dent. Sci. 2021, 16, 1037–1038. [Google Scholar] [CrossRef]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; et al. 3D and 4D Printing in Dentistry and Maxillofacial Surgery: Printing Techniques, Materials, and Applications. Acta Biomater. 2021, 122, 26–49. [Google Scholar] [CrossRef]
- Lin, H.-H.; Lonic, D.; Lo, L.-J. 3D Printing in Orthognathic Surgery—A Literature Review. J. Formos. Med. Assoc. 2018, 117, 547–558. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, F.; Zhai, W.; Cheng, S.; Li, J.; Wang, Y. Unraveling of Advances in 3D-Printed Polymer-Based Bone Scaffolds. Polymers 2022, 14, 566. [Google Scholar] [CrossRef]
- Shuai, C.; Yanga, W.; Fenga, P.; Peng, S.; Pan, H. Accelerated degradation of HAP/PLLA bone scaffold by PGA blending facilitates bioactivity and osteoconductivity. Bioact. Mater. 2021, 6, 490–502. [Google Scholar] [CrossRef]
- Revilla-León, M.; Sadeghpour, M.; Özcan, M. An Update on Applications of 3D Printing Technologies Used for Processing Polymers Used in Implant Dentistry. Odontology 2020, 108, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Yang, Z.; Lin, W.-S.; Chen, L.; Tan, J. Digital Duplication and 3D Printing for Implant Overdenture Fabrication. J. Prosthodont. 2021, 30, 139–142. [Google Scholar] [CrossRef]
- Anderson, J.; Wealleans, J.; Ray, J. Endodontic Applications of 3D Printing. Int. Endod. J. 2018, 51, 1005–1018. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.; Chong, B.S. 3D Imaging, 3D Printing and 3D Virtual Planning in Endodontics. Clin. Oral Investig. 2018, 22, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Carmone, S.; Brambilla, D.; Leroux, J.-C. 3D printing of a wearable personalized oral delivery device. A first-in-human study. Sci. Adv. 2018, 4, 2544. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Balestra, D.; Goracci, C.; Rudford, D.R.; Louca, C. The mask fitter, a simple method to improve medical face mask adaptation using customized 3D-printed frame during COVID-19: A survey on user’s acceptability in clinical dentistry. Appl. Sci. 2022, 12, 8921. [Google Scholar] [CrossRef]
- Cousley, R.R. Introducing 3D Printing in Your Orthodontic Practice. J. Orthod. 2020, 47, 265–272. [Google Scholar] [CrossRef]
- Goracci, C.; Juloski, J.; D’Amico, C.; Balestra, D.; Volpe, A.; Juloski, J.; Vichi, A. Clinically Relevant Properties of 3D Printable Materials for Intraoral Use in Orthodontics: A Critical Review of the Literature. Materials 2023, 16, 2166. [Google Scholar] [CrossRef]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D Printed Complete Removable Dental Prostheses: A Narrative Review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.-F.; Xie, P.-J.; Wu, J.-H. Accuracy of Digital Complete Dentures: A Systematic Review of in Vitro Studies. J. Prosthet. Dent. 2021, 125, 249–256. [Google Scholar] [CrossRef]
- Alhallak, K.R.; Nankali, A. 3D Printing Technologies for Removable Dentures Manufacturing: A Review of Potentials and Challenges. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Methani, M.M.; Morton, D.; Zandinejad, A. Internal and Marginal Discrepancies Associated with Stereolithography (SLA) Additively Manufactured Zirconia Crowns. J. Prosthet. Dent. 2020, 124, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Bae, E.-J.; Jeong, I.-D.; Kim, W.-C.; Kim, J.-H. A Comparative Study of Additive and Subtractive Manufacturing for Dental Restorations. J. Prosthet. Dent. 2017, 118, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Zandinejad, A.; Methani, M.M.; Schneiderman, E.D.; Revilla-León, M.; Bds, D.M. Fracture Resistance of Additively Manufactured Zirconia Crowns When Cemented to Implant Supported Zirconia Abutments: An In Vitro Study. J. Prosthodont. 2019, 28, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Sun, J. Dimensional Accuracy and Clinical Adaptation of Ceramic Crowns Fabricated with the Stereolithography Technique. J. Prosthet. Dent. 2021, 125, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Kihara, H.; Sugawara, S.; Yokota, J.; Takafuji, K.; Fukazawa, S.; Tamada, A.; Hatakeyama, W.; Kondo, H. Applications of Three-Dimensional Printers in Prosthetic Dentistry. J. Oral Sci. 2021, 63, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Al Hamad, K.Q.; Al-Rashdan, B.A.; Ayyad, J.Q.; Al Omrani, L.M.; Sharoh, A.M.; Al Nimri, A.M.; Al-Kaff, F.T. Additive Manufacturing of Dental Ceramics: A Systematic Review and Meta-Analysis. J. Prosthodont. 2022, 31, e67–e86. [Google Scholar] [CrossRef]
- Valenti, C.; Isabella Federici, M.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical Properties of 3D-Printed Prosthetic Materials Compared with Milled and Conventional Processing: A Systematic Review and Meta-Analysis of in Vitro Studies. J. Prosthet. Dent. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Revilla-León, M.; Al-Haj Husain, N.; Ceballos, L.; Özcan, M. Flexural Strength and Weibull Characteristics of Stereolithography Additive Manufactured versus Milled Zirconia. J. Prosthet. Dent. 2021, 125, 685–690. [Google Scholar] [CrossRef]
- Uçar, Y.; Aysan Meriç, İ.; Ekren, O. Layered Manufacturing of Dental Ceramics: Fracture Mechanics, Microstructure, and Elemental Composition of Lithography-Sintered Ceramic. J. Prosthodont. 2019, 28, e310–e318. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Wang, Y.; Hu, M.; Wang, Y.; Xv, Y.; Liu, Y.; Sun, Y. Strength and Adaptation of Stereolithography-Fabricated Zirconia Dental Crowns: An In Vitro Study. Int. J. Prosthodont. 2019, 32, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Munoz, S.; Ramos, V.; Dickinson, D.P. Comparison of Margin Discrepancy of Complete Gold Crowns Fabricated Using Printed, Milled, and Conventional Hand-Waxed Patterns. J. Prosthet. Dent. 2017, 118, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, S.; Gmeiner, R.; Schönherr, J.A.; Stampfl, J. Stereolithography-Based Additive Manufacturing of Lithium Disilicate Glass Ceramic for Dental Applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 116, 111180. [Google Scholar] [CrossRef]
- Council of the European Communities. Council Directive of 14th June 1993 Concerning Medical Devices; 93/42/EEC; Council of the European Communities: Brussels, Belgium, 2007. [Google Scholar]
- Borella, P.S.; Alvares, L.A.S.; Ribeiro, M.T.H.; Moura, G.F.; Soares, C.J.; Zancopé, K.; Mendonça, G.; Rodrigues, F.P.; das Neves, F.D. Physical and Mechanical Properties of Four 3D-Printed Resins at Two Different Thick Layers: An In Vitro Comparative Study. Dent. Mater. 2023, 39, 686. [Google Scholar] [CrossRef]
- Çakmak, G.; Donmez, M.B.; de Paula, M.S.; Akay, C.; Fonseca, M.; Kahveci, Ç.; Abou-Ayash, S.; Yilmaz, B. Surface Roughness, Optical Properties, and Microhardness of Additively and Subtractively Manufactured CAD-CAM Materials after Brushing and Coffee Thermal Cycling. J. Prosthodont. 2023. [Google Scholar] [CrossRef]
- Çakmak, G.; Oosterveen-Rüegsegger, A.L.; Akay, C.; Schimmel, M.; Yilmaz, B.; Donmez, M.B. Influence of Polishing Technique and Coffee Thermal Cycling on the Surface Roughness and Color Stability of Additively and Subtractively Manufactured Resins Used for Definitive Restorations. J. Prosthodont. 2023. [Google Scholar] [CrossRef]
- Cantó-Navés, O.; Michels, K.; Figueras-Alvarez, O.; Fernández-Villar, S.; Cabratosa-Termes, J.; Roig, M. In Vitro Comparison of Internal and Marginal Adaptation between Printed and Milled Onlays. Materials 2023, 16, 6962. [Google Scholar] [CrossRef] [PubMed]
- Daghrery, A. Color Stability, Gloss Retention, and Surface Roughness of 3D-Printed versus Indirect Prefabricated Veneers. J. Funct. Biomater. 2023, 14, 492. [Google Scholar] [CrossRef] [PubMed]
- Espinar, C.; Bona, A.D.; Pérez, M.M.; Tejada-Casado, M.; Pulgar, R. The Influence of Printing Angle on Color and Translucency of 3D Printed Resins for Dental Restorations. Dent. Mater. 2023, 39, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Espinar, C.; Della Bona, A.; Tejada-Casado, M.; Pulgar, R.; Pérez, M.M. Optical Behavior of 3D-Printed Dental Restorative Resins: Influence of Thickness and Printing Angle. Dent. Mater. 2023, 39, 894–902. [Google Scholar] [CrossRef]
- Giugliano, T.S.; Zhang, Y.; Janal, M.N.; Lim, C.H.; Smith, R.M.; Choi, M. In Vitro Comparison of Physical Characteristics of Milled versus Printed Zirconia Discs. J. Prosthodont. 2023. [Google Scholar] [CrossRef] [PubMed]
- Homsy, F.R.; Özcan, M.; Khoury, M.; Majzoub, Z.A.K. Marginal and Internal Fit of Pressed Lithium Disilicate Inlays Fabricated with Milling, 3D Printing, and Conventional Technologies. J. Prosthet. Dent. 2018, 119, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, A.; Park, J.-M.; Hüsler, J.; Bomze, D.; Mühlemann, S.; Özcan, M. An in Vitro Comparison of the Marginal and Internal Adaptation of Ultrathin Occlusal Veneers Made of 3D-Printed Zirconia, Milled Zirconia, and Heat-Pressed Lithium Disilicate. J. Prosthet. Dent. 2022, 128, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Karaoğlanoğlu, S.; Aydın, N.; Oktay, E.A.; Ersöz, B. Comparison of the Surface Properties of 3D-Printed Permanent Restorative Resins and Resin-Based CAD/CAM Blocks. Oper. Dent. 2023, 48, 588–598. [Google Scholar] [CrossRef]
- Lyu, J.; Yang, X.; Li, Y.; Tan, J.; Liu, X. Effect of Build Angle on the Dimensional Accuracy of Monolithic Zirconia Crowns Fabricated with the Nanoparticle Jetting Technique. J. Prosthet. Dent. 2023, 130, 613.e1–613.e8. [Google Scholar] [CrossRef]
- Lyu, J.; Yang, X.; Li, Y.; Tan, J.; Liu, X. Dimensional Accuracy and Clinical Adaptation of Monolithic Zirconia Crowns Fabricated with the Nanoparticle Jetting Technique. J. Prosthet. Dent. 2023. online ahead of print. [Google Scholar] [CrossRef]
- Miura, S.; Shinya, A.; Ishida, Y.; Fujisawa, M. Mechanical and Surface Properties of Additive Manufactured Zirconia under the Different Building Directions. J. Prosthodont. Res. 2023, 67, 410–417. [Google Scholar] [CrossRef]
- Miura, S.; Shinya, A.; Ishida, Y.; Fujita, T.; Vallittu, P.; Lassila, L.; Fujisawa, M. The Effect of Low-Temperature Degradation and Building Directions on the Mechanical Properties of Additive-Manufactured Zirconia. Dent. Mater. J. 2023, 42, 800–805. [Google Scholar] [CrossRef]
- Nakai, H.; Inokoshi, M.; Nozaki, K.; Komatsu, K.; Kamijo, S.; Liu, H.; Shimizubata, M.; Minakuchi, S.; Van Meerbeek, B.; Vleugels, J.; et al. Additively Manufactured Zirconia for Dental Applications. Materials 2021, 14, 3694. [Google Scholar] [CrossRef]
- Nam, N.-E.; Hwangbo, N.-K.; Kim, J.-E. Effects of Surface Glazing on the Mechanical and Biological Properties of 3D Printed Permanent Dental Resin Materials. J. Prosthodont. Res. 2023. online ahead of print. [Google Scholar] [CrossRef]
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical Properties of 3D-Printed and Milled Composite Resins for Definitive Restorations: An In Vitro Comparison of Initial Strength and Fatigue Behavior. J. Esthet. Restor. Dent. 2023, 36, 391–401. [Google Scholar] [CrossRef]
- Refaie, A.; Bourauel, C.; Fouda, A.M.; Keilig, L.; Singer, L. The Effect of Cyclic Loading on the Fracture Resistance of 3D-Printed and CAD/CAM Milled Zirconia Crowns-an In Vitro Study. Clin. Oral Investig. 2023, 27, 6125–6133. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Mostafavi, D.; Methani, M.M.; Zandinejad, A. Manufacturing Accuracy and Volumetric Changes of Stereolithography Additively Manufactured Zirconia with Different Porosities. J. Prosthet. Dent. 2022, 128, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Rauch, A.; Hahnel, S.; Schmidt, M. In-Vitro Performance of Subtractively and Additively Manufactured Resin-Based Molar Crowns. J. Mech. Behav. Biomed. Mater. 2023, 141, 105806. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.; Kang, Y.-J.; Kim, H.; Kim, J.-H. Effect of Cement Space Settings on the Marginal and Internal Fit of 3D-Printed Definitive Resin Crowns. J. Prosthet. Dent. 2023. online ahead of print. [Google Scholar] [CrossRef]
- Suksuphan, P.; Krajangta, N.; Didron, P.P.; Wasanapiarnpong, T.; Rakmanee, T. Marginal Adaptation and Fracture Resistance of Milled and 3D-Printed CAD/CAM Hybrid Dental Crown Materials with Various Occlusal Thicknesses. J. Prosthodont. Res. 2023. [Google Scholar] [CrossRef]
- Wang, W.; Yu, H.; Liu, Y.; Jiang, X.; Gao, B. Trueness Analysis of Zirconia Crowns Fabricated with 3-Dimensional Printing. J. Prosthet. Dent. 2019, 121, 285–291. [Google Scholar] [CrossRef]
- Zhu, H.; Zhou, Y.; Jiang, J.; Wang, Y.; He, F. Accuracy and Margin Quality of Advanced 3D-Printed Monolithic Zirconia Crowns. J. Prosthet. Dent. 2023. online ahead of print. [Google Scholar] [CrossRef]
- Zimmermann, M.; Ender, A.; Egli, G.; Özcan, M.; Mehl, A. Fracture Load of CAD/CAM-Fabricated and 3D-Printed Composite Crowns as a Function of Material Thickness. Clin. Oral Investig. 2019, 23, 2777–2784. [Google Scholar] [CrossRef]
- Nishigawa, K.; Bando, E.; Nakano, M. Quantitative Study of Bite Force during Sleep Associated Bruxism. J. Oral Rehabil. 2001, 28, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Jonasch, M. Effect of Cyclic Fatigue Tests on Aging and Their Translational Implications for Survival of All-Ceramic Tooth-Borne Single Crowns and Fixed Dental Prostheses. J. Prosthodont. 2018, 27, 364–375. [Google Scholar] [CrossRef]
- Kim, K.-H.; Ong, J.L.; Okuno, O. The Effect of Filler Loading and Morphology on the Mechanical Properties of Contemporary Composites. J. Prosthet. Dent. 2002, 87, 642–649. [Google Scholar] [CrossRef]
- ISO Standard 6872:2015; Dentistry-Ceramic Materials. International Organization for Standardization: Geneva, Switzerland, 2015.
- Branco, A.C.; Silva, R.; Santos, T.; Jorge, H.; Rodrigues, A.R.; Fernandes, R.; Bandarra, S.; Barahona, I.; Matos, A.P.A.; Lorenz, K.; et al. Suitability of 3D Printed Pieces of Nanocrystalline Zirconia for Dental Applications. Dent. Mater. 2020, 36, 442–455. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Goracci, C.; Carrabba, M.; Tozzi, G.; Louca, C. Flexural Resistance of CAD-CAM Blocks. Part 3: Polymer-Based Restorative Materials for Permanent Restorations. Am. J. Dent. 2020, 33, 243–247. [Google Scholar] [PubMed]
- Lim, K.; Yap, A.U.-J.; Agarwalla, S.V.; Tan, K.B.-C.; Rosa, V. Reliability, Failure Probability, and Strength of Resin-Based Materials for CAD/CAM Restorations. J. Appl. Oral Sci. 2016, 24, 447–452. [Google Scholar] [CrossRef]
- Harada, A.; Nakamura, K.; Kanno, T.; Inagaki, R.; Örtengren, U.; Niwano, Y.; Sasaki, K.; Egusa, H. Fracture Resistance of Computer-Aided Design/Computer-Aided Manufacturing-Generated Composite Resin-Based Molar Crowns. Eur. J. Oral Sci. 2015, 123, 122–129. [Google Scholar] [CrossRef]
- Vichi, A.; Balestra, D.; Scotti, N.; Louca, C.; Paolone, G. Translucency of CAD/CAM and 3D Printable Composite Materials for Permanent Dental Restorations. Polymers 2023, 15, 1443. [Google Scholar] [CrossRef] [PubMed]
- Hébert, M.; Hersch, R.D.; Becker, J.-M. Compositional Reflectance and Transmittance Model for Multilayer Specimens. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2007, 24, 2628–2644. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Bui, P.H.-B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects Build Orientation, Positioning, and Curing Influence Dimensional Accuracy and Flexural Properties of Stereolithographically Printed Resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef] [PubMed]
- Paolone, G.; Mandurino, M.; De Palma, F.; Mazzitelli, C.; Scotti, N.; Breschi, L.; Gherlone, E.; Cantatore, G.; Vichi, A. Color Stability of Polymer-Based Composite CAD/CAM Blocks: A Systematic Review. Polymers 2023, 15, 464. [Google Scholar] [CrossRef]
- Rechendorff, K.; Hovgaard, M.B.; Foss, M.; Zhdanov, V.P.; Besenbacher, F. Enhancement of protein adsorption induced by surface roughness. Langmuir 2006, 22, 10885–10888. [Google Scholar] [CrossRef]
| MEDLINE/PubMed | |
|---|---|
| Search query | (restorative dentistry OR prosthetic dentistry) AND (3D printing OR additive manufacturing OR rapid prototyping) AND materials |
| Search strategy | ((“restorative dent”[Journal] OR (“restorative”[All Fields] AND “dentistry”[All Fields]) OR “restorative dentistry”[All Fields] OR (“prosthodontics”[MeSH Terms] OR “prosthodontics”[All Fields] OR (“prosthetic”[All Fields] AND “dentistry”[All Fields]) OR “prosthetic dentistry”[All Fields])) AND (“printing, three dimensional”[MeSH Terms] OR (“printing”[All Fields] AND “three dimensional”[All Fields]) OR “three-dimensional printing”[All Fields] OR (“3d”[All Fields] AND “printing”[All Fields]) OR “3d printing”[All Fields] OR (“addit manuf”[Journal] OR (“additive”[All Fields] AND “manufacturing”[All Fields]) OR “additive manufacturing”[All Fields]) OR ((“rapid”[All Fields] OR “rapidities”[All Fields] OR “rapidity”[All Fields] OR “rapidness”[All Fields]) AND (“prototypal”[All Fields] OR “prototype”[All Fields] OR “prototype s”[All Fields] OR “prototyped”[All Fields] OR “prototypes”[All Fields] OR “prototypic”[All Fields] OR “prototypical”[All Fields] OR “prototypicality”[All Fields] OR “prototypically”[All Fields] OR “prototyping”[All Fields]))) AND (“material”[All Fields] OR “material s”[All Fields] OR “materials”[All Fields])) AND ((y_10[Filter]) AND (fft[Filter]) AND (english[Filter])) |
| Retrieval | 1070 items |
| Scopus | |
| Search query | (restorative dentistry OR prosthetic dentistry) AND (3D printing OR additive manufacturing OR rapid prototyping) AND materials |
| Search strategy | (restorative dentistry OR prosthetic dentistry) AND (3D printing OR additive manufacturing OR rapid prototyping) AND materials |
| Retrieval | 908 items |
| Cochrane Library | |
| Search query | (restorative dentistry OR prosthetic dentistry) AND (3D printing OR additive manufacturing OR rapid prototyping) AND materials |
| Search strategy | ((restorative dentistry OR prosthetic dentistry) AND (3D printing OR additive manufacturing OR rapid prototyping) AND materials) in Title Abstract Keyword |
| Retrieval | 123 items |
| Web of Science | |
| Search query | (restorative dentistry OR prosthetic dentistry) AND (3D printing OR additive manufacturing OR rapid prototyping) AND materials |
| Search strategy | (restorative dentistry OR prosthetic dentistry) AND (3D printing OR additive manufacturing OR rapid prototyping) AND materials |
| Retrieval | 367 items |
| Study | Objective (S) | Material and 3D Printer | Mat.Type | Evaluated Parameter (S) | Main Conclusion (S) |
|---|---|---|---|---|---|
| Bae et al., 2017 [27] | To evaluate the accuracy of inlay restorations fabricated by AM compared to subtractive methods. | Polymer (VisiJet FTX Green, 3D Systems); 3D Printer (ProJet 1200–3D Systems). | P | Dimensional accuracy and surface morphology. | The accuracy of inlays fabricated by AM is higher than that of subtractive methods. |
| Baumgartner et al., 2020 [38] | To use stereolithographic ceramic manufacturing (LCM) to reproducibly print dense and reliable lithium disilicate glass-ceramic samples. | Powder (IPS e.max Press LT, Ivoclar Vivadent AG, Schaan). | C | Mechanical properties and aesthetics. | It is possible to use stereolithographic ceramic manufacturing (LCM) to reproducibly print dense and reliable lithium disilicate glass-ceramic samples that meet the high requirements for dental restorations regarding mechanical properties and aesthetics. |
| Borella et al., 2023 [40] | To evaluate the physical and mechanical properties of four 3D printed resins with two different thickness layers. | Polymer (VarseoSmile Crown Plus, VSC); 3D printer (Anycubic Photon Mono, Anycubic 3D). | P | Raman spectroscopy for degree of conversion, confocal laser scanning microscopy for surface roughness (Sa), three-point bending test for flexural strength and elastic modulus, and a Vickers hardness test (VHN). | The physical and mechanical properties of three-dimensional printed restorations can be affected by the layer thickness, which can interfere with the choice of the 3D printing resin for a desired clinical outcome. |
| Cakmak et al., 2023 [41] | To evaluate the surface roughness, optical properties, and microhardness of additively or subtractively manufactured CAD-CAM materials after simulated brushing and coffee thermal cycling. | Polymers (Crowntec, CT and VarseoSmile Crown Plus, VS); 3D printers (MAX UV; Asiga). | P | Surface roughness, Vickers microhardness, and color coordinates. | Tested additively manufactured resins can be considered more susceptible to simulated brushing and coffee thermal cycling than the other materials, given the fact that their surface roughness and ΔE00 values were higher than previously”reported acceptability thresholds and because they had the lowest microhardness after all procedures were complete. |
| Cakmak et al., 2023 [42] | To evaluate how different polishing techniques and coffee thermal cycling affect the surface roughness and stainability of additively and subtractively manufactured resins used for definitive prostheses. | Polymers (Crowntec, CT and VarseoSmile Crown Plus, VS); 3D printers (MAX UV; Asiga). | P | Surface roughness and color stability. | R(a) of CS was similar to or lower than the R(a) of other materials, regardless of the time interval or polishing technique. CP mostly led to lower R(a) than other polishing techniques, whereas VA resulted in a high R(a) regardless of the material–time interval pair. Polishing reduced the R(a), while coffee thermal cycling was found to have a small effect. Among tested material-polishing pairs, only CS-VA had moderately unacceptable color change when previously reported threshold values were considered. |
| Canto-Naves et al., 2023 [43] | To compare the gaps between the prepared tooth and milled and printed onlays fabricated with the same CAD design. It also aimed to determine the gap reproducibility across onlays fabricated by 3D printing and milling. | Polymer (Permanent Crown Resin A2; Bego GmbH); 3D printer (Formlabs Form 3+). | P | Internal and marginal adaptation. | This study concluded that the printed onlays adapted significantly better to the prepared tooth than the milled onlays. Printed onlays also showed significantly better gap reproducibility. |
| Daghrery et al., 2023 [44] | To evaluate the effect of artificial aging by immersion in different staining solutions on the color changes, gloss, and surface roughness (Ra) of 3D printed veneers compared to the prefabricated resin composite veneer systems (PRCVs) manufactured by Componeer and Edelweiss. | Polymers (Iris Max DWS, Componeer Brilliant); 3D printer (DFAB Chairside 3D blue edge laser printer). | P | Color stability, gloss retention, and surface roughness. | Veneers manufactured using the 3D printing technique are vulnerable to discoloration and are significantly affected by artificial aging in a staining solution compared to the PRCVs. Coffee and tea staining had a deleterious effect on the color, surface gloss, and surface roughness of all tested indirect composite veneers despite manufacturing techniques. The efficacy of stain removal was higher with an in-office bleaching technique compared to surface polishing in the PRCVs, while in-office bleaching and surface polishing showed comparable effects in the 3D printed veneers. Veneer production using 3D printing provides cost-effective, time-efficient, and on-demand solutions. However, material processing for 3D printing is crucial for long- term longevity. |
| Espinar et al., 2023 [45] | To evaluate the influence of printing orientation on color and translucency of 3D printing restorative resins. | Polymer (FP-Formlabs Permanent Crown); 3D printer (3D Form 3B+). | P | Color and translucency. | The selection of building orientation (0 degrees and 90 degrees) for the 3D printed resins influences the visual color and translucency and therefore their esthetic appearance. |
| Espinar et al., 2023 [46] | To evaluate the influence of thickness and printing angle on the optical properties of 3D printed dental restorative resins. | Polymer (FP-Formlabs Permanent Crown); 3D printer (3D Form 3B+). | P | Scattering (S), absorption (K) and albedo (a) coefficients, transmittance (T%), light reflectivity (RI), and infinite optical thickness (X infinity). | Optical properties of 3D printed restorative resins vary between thicknesses and could be affected by the building orientation. |
| Giugliano et al., 2023 [47] | To compare the dimensional accuracy, translucency, and biaxial flexural strength of milled zirconia (MZ) versus 3D printed zirconia (PZ) discs. | Zirconia (LithaCon 3Y 230, Lithoz America); 3D printer (Lithoz Cerafab 7500 Dental 3D-printer). | C | Translucency, flexural strength. | The results showed that the milled specimens achieved better dimensional accuracy and were more translucent, stronger, and less prone to failure than printed specimens. |
| Homsy et al., 2018 [48] | To compare the marginal and internal fit accuracy of lithium disilicate glass-ceramic inlays fabricated with conventional, milled, and three-dimensional (3D) printed wax patterns. | Polymer (VisiJet FTX Green, 3D Systems); 3D Printer (ProJet 1200–3D Systems). | P | Marginal and internal fit accuracy. | The CAD-CAM subtractive method of wax pattern fabrication produced IPS e.max. Press inlays with better marginal and internal fittings than those obtained through conventional workflow or additive 3D printing. Three-dimensional printing of inlay wax patterns yielded similar results to conventional waxing in terms of marginal and internal fit. |
| Ioannidis et al., 2022 [49] | To compare the marginal and internal fit of 3D printed zirconia occlusal veneers with CAD-CAM fabricated zirconia or heat-pressed lithium disilicate ceramic (LS2) restorations on molars. | Material (ceramic powder 3 mol% yttria-stabilized zirconia polycrystal); 3D Printer (CeraFab 7500; Lithoz GmbH). | C | Marginal and internal fit. | Three-dimensionally printed zirconia occlusal veneers produced by means of lithography-based ceramic manufacturing exhibit a marginal adaptation (95 mm) and a production accuracy (26 mm) similar to those of conventional methods. |
| Karaoglanoglu et al., 2023 [50] | To investigate the surface roughness, microhardness, and color changes of resin-based computer-aided design/computer-aided manufacturing (CAD/CAM) blocks and 3D printed permanent resins in different beverages. | Polymer (Crowntec and Permanent Crown); 3D printer (MAX UV; Asiga). | P | Surface roughness, microhardness, and color. | Although the surface roughness of 3D printed permanent resins was similar to that of resin-based CAD/CAM blocks, they had a lower microhardness value. Moreover, 3D printed permanent resins showed more color changes in tea and coffee. |
| Li et al., 2019 [36] | To evaluate the physical and mechanical properties of SL-manufactured zirconia dental crowns and analyze their internal and marginal adaptation. | Custom-made resin-based zirconia (45 vol%); 3D Printer (CSL 150–Porimy). | C | Density, sintering shrinkage, flexural strength, Weibull parameters, internal marginal adaptation. | The strength of SL-manufactured zirconia was adequate to fabricate dental crowns, which showed less-than-ideal internal and marginal adaptation for clinical applications. |
| Lyu et al., 2023 [51] | To evaluate the effect of the build angle on the dimensional accuracy of monolithic zirconia complete crowns fabricated by using NPJ. | Zirconia (C800 Xjet); 3D printer (Carmel 1400C Xjet). | Dimensional accuracies in the external, marginal, and intaglio regions. | The dimensional accuracy of monolithic zirconia crowns fabricated by using NPJ was affected by the build angle and was within clinically acceptable limits. | |
| Lyu et al., 2023 [52] | To compare the dimensional accuracy and clinical adaptation of zirconia crowns fabricated with NPJ and those fabricated with subtractive manufacturing (SM) and digital light processing (DLP). | Zirconia (C800 Xjet); 3D printer (Carmel 1400C Xjet). | C | Dimensional accuracy in the external, intaglio, and marginal areas, | Monolithic zirconia crowns fabricated using NPJ have higher dimensional accuracy and clinical adaptation than those fabricated using SM or DLP. |
| Miura et al., 2023 [53] | To evaluate the mechanical and surface properties of zirconia manufactured using additive manufacturing (AM) technology and the effect of the building direction on the mechanical and surface properties. | Zirconia (3Dmix ZrO(2) 3Dceram); 3D printer (CeraMaker 900 3D Ceram). | C | Flexural strength, Vickers hardness, fracture toughness, elastic modulus, and Poisson’s ratio. | The flexural strength and surface structure of the tested SLA-manufactured zirconia were influenced by the building direction; however, other mechanical properties remained unaffected. The layer boundaries affected the anisotropic behavior of the builds to a certain extent, owing to the layer-by-layer production method. |
| Miura et al., 2023 [54] | To investigate the effect of low-temperature degradation (LTD) on the mechanical properties of additive-manufactured zirconia. | Zirconia (3Dmix ZrO(2) 3Dceram); 3D printer (CeraMaker 900 3Dceram). | C | Flexural strength, modulus of elasticity, Vickers hardness, and fracture toughness. | High average material strengths that exceed the current ISO requirements for fixed ceramic prostheses were measured in flexural tests, except in the 0° direction. LTD had little effect on flexural strength, elastic modulus, Vickers hardness, and fracture toughness. However, the optimization of all processing steps, including 3D printing, cleaning, stripping, sintering, and color immersion, is necessary to achieve optimal reliability of 3D printed zirconia materials for clinical applications. |
| Munoz et al., 2017 [37] | To evaluate and compare margin discrepancy of complete gold crowns (CGCs) fabricated from printed, milled, and conventional hand-waxed patterns. | Material (Gold); 3D printer (ProJet DP 3000; 3D Systems). | M | Margin discrepancy. | The ProJet DP 3000 printed patterns were significantly different from LAVA CNC 500 milled and hand-waxed patterns, with an overall poorer result. Fabricating CGCs from printed patterns produced a significantly higher number of crowns with unacceptable margin discrepancy (>120 mm). |
| Nakai et al., 2021 [55] | To assess the crystallography, microstructure, and flexural strength of zirconia-based ceramics made by stereolithography (SLA). | Two additively manufactured 3Y-TZPs (LithaCon 3Y 230, Lithoz, Vienna, Austria; 3D Mix zirconia, 3Dceram Sinto, Limoges, France), one additively manufactured ATZ (3D Mix ATZ, 3Dceram Sinto, Limoges, France); 3D Printer (SLA). | C | Crystallography, microstructure, and flexural strength. | Additively manufactured zirconia revealed a crystal structure, biaxial flexural strength, and microstructure comparable to that of subtractively (conventionally) manufactured zirconia. Differences in the additive manufacturing process of zirconia may affect the biaxial flexural strength of additively manufactured zirconia. Additively manufactured ATZ had a higher biaxial flexural strength than additively and subtractively manufactured 3Y-TZP. |
| Nam et al., 2023 [56] | To determine the surface glazing effect on the mechanical and biological properties of three-dimensional printed dental permanent resins. | Polymer (Formlabs, Graphy Tera Harz permanent); 3D printer (Next Dent 5100). | P | Flexural strength, Vickers hardness, color stability, and surface roughness. | Surface glazing increased the mechanical strength, color stability, and cell compatibility while reducing the Ra and protein adsorption of 3D printed dental resins. Thus, a glazed surface exhibited a positive effect on the mechanical and biological properties of 3D printed resins. |
| Prause et al., 2023 [57] | To evaluate the flexural strength and fatigue behavior of a novel 3D printed composite resin for definitive restorations. | Polymer (Varseo Smile Crown Plus); 3D printer (Varseo XS). | P | Biaxial flexural strength and biaxial flexural fatigue strength. | The 3D printed composite resin exhibited the lowest mechanical properties, where areas of nonhomogeneous microstructure developed during the mixing procedure served as potential fracture origins. |
| Refaie et al., 2023 [58] | To evaluate the effect of cyclic mechanical loading on the fracture resistance of 3D printed zirconia crowns in comparison to milled zirconia crowns. | Zirconia (Lithoz 210 3Y); 3D printer (Cera Fab7500). | C | Fracture resistance. | The fabrication technique and cyclic loading affect the fracture resistance of zirconia crowns. Although the fracture resistance values for the 3D printed crowns were lower than those of the milled ones, they are higher than the masticatory forces and thus could be considered clinically acceptable. |
| Revilla-Leon et al., 2020 [26] | To measure and compare the marginal and internal discrepancies of milled and AM zirconia crowns by using the silicone replica technique. | Zirconia (3Dmix ZrO2 paste; 3Dceram Co.); 3D Printer (CERAMAKER 900; 3Dceram Co.). | C | Marginal and internal discrepancies. | CNC and SAM groups had clinically acceptable marginal and internal discrepancies, while the AM group had clinically unacceptable marginal and internal crown discrepancies. |
| Revilla-Leon et al., 2021 [34] | To compare the flexural strength and Weibull characteristics of milled and additively manufactured zirconia. | Photosensitive resin mixed with zirconia paste (3DmixZrO2L, 3Dceram Co.); 3D Printer (CERAMAKER 900; 3Dceram Co). | C, P | Flexural strength and Weibull characteristics. | AM zirconia material revealed significantly lower flexural strength mean values than milled zirconia material. Significantly decreased flexural strength values of milled and AM zirconia material as indicated by the Weibull. Moduli were significantly higher for the milled groups than the additively manufactured groups. |
| Revilla-Leon et al., 2022 [59] | To measure the manufacturing accuracy and volumetric changes of additively manufactured (AM) zirconia specimens with different porosities (0%, 20%, and 40%). | Material (3Dmix ZrO2 paste; 3Dceram Co.); 3D Printer (CERAMAKER 900; 3Dceram Co.). | C | Manufacturing accuracy and volumetric changes. | The 40%-porosity group obtained the highest manufacturing accuracy and the lowest manufacturing volume change, followed by the 20%-porosity and the 0%-porosity groups. An uneven manufacturing volume change in the x-, y-, and z-axes was observed. However, none of the groups tested were able to perfectly match the virtual design of the specimens. |
| Rosentritt et al., 2023 [60] | To compare the in vitro performance and wear behavior of additively or subtractively fabricated resin-based composite molar crowns for temporary and permanent application. | Polymer (VarseoSmile Crown plus); 3D printers (Varseo XS, Asiga MAX UV). | P | Fracture force, wear, and roughness. | Temporary and permanent molar crowns provided at least acceptable in vitro performance and fracture force for clinical mid-term application. Laboratory wear stability of the resin-based materials appeared sufficient but should be verified under clinical conditions. |
| Shin et al., 2023 [61] | To evaluate how cement gap settings affect the marginal and internal fit of a 3D printed definitive resin crown. | Polymer (TC-80DP); 3D printer (Sprint Ray Pro 95). | P | Marginal and internal fit. | Based on the findings of this in vitro study, a 70 μm cement gap setting is recommended for optimal marginal and internal fit of 3D printed resin crowns. |
| Suksuphan., 2023 [62] | To evaluate the marginal adaptation and fracture resistance of three computer-aided design/computer-assisted manufacturing hybrid dental materials with different occlusal thicknesses. | Polymer (Varseosmile Crown Plus); 3D printer (Freeform Pro 2). | P | Marginal adaptation and fracture resistance. | All hybrid-material crowns demonstrated favorable marginal adaptation within a clinically acceptable range, with 3D printing yielding superior results to milling. All materials could withstand normal occlusal force even with a 0.8 mm occlusal thickness. |
| Ucar et al., 2019 [35] | To compare the mechanical and microstructural properties of ceramics from lithography-based ceramic manufacturing (LCM) with pressing and CAD/CAM methods. | High-purity alumina (LithaLox HP 500, Lithoz); 3D Printer (CeraFab 7500, Lithoz). | C | Biaxial flexural strength, hardness, fracture toughness, structural reliability. | LCM can be used to produce ceramic parts. Mechanical properties and manufacturing of LCM ceramics seem to be promising but need improvements, mainly to reduce porosity. |
| Wang et al., 2019 [63] | To evaluate the trueness of zirconia crowns fabricated by 3D printing in comparison with crowns fabricated by CAD-CAM milling as a control. | Photosensitive resin mixed with zirconia paste (3DmixZrO2L, 3Dceram Co.); 3D Printer (CERAMAKER 900; 3Dceram Co.). | C, P | Trueness (dimensional accuracy considering 4 crown locations). | Zirconia crowns produced by 3D printing met the trueness requirements, and 3D printing may be suitable for fabricating zirconia crowns. |
| Wang et al., 2021 [29] | To evaluate the dimensional accuracy and clinical adaptation of ceramic crowns fabricated with the stereolithography technique. | Material (Alumina, multifunctional acrylate–Lithoz; Zirconia, HDDA, PET4A–PORIMY); 3D Printer (CeraFab 7500, Lithoz). | C, P | Dimensional accuracy and marginal adaptation. | Both CF and CL can fabricate ceramic crowns with high dimensional accuracy and marginal adaptation within clinically acceptable limits. The results indicated that the fabrication of ceramic crowns by using the SLA technique is promising. |
| Zandinejad et al., 2019 [28] | To compare the fracture resistance of milled zirconia (MZr), milled lithium disilicate (MLD), and AM zirconia (AMZr) crowns when cemented to MZr implant abutment. | Composite (3Dceram Co. Lemonge, France); 3D Printer; (CeraMaker 900; 3Dceram Co. Lemonge, France). | P | Fracture load. | AM all ceramic crowns cemented on zirconia abutments had a comparable fracture resistance to milled restorations in this in vitro study. AM appears to be a promising technology for the fabrication of all ceramic restorations with great potential for improvement in the near future. |
| Zhu 2023 [64] | To evaluate and compare the trueness, crown fit, and margin quality of monolithic zirconia crowns manufactured by NPJ with those milled by a computer numerical control system. | Zirconia (brand not available) | C | Trueness, crown fit, and margin quality. | All 3 manufacturing methods can fabricate zirconia crowns with a clinically acceptable crown fit. The NPJ system could be used to manufacture monolithic zirconia crowns with better margin quality and proximal surface trueness than milled crowns. |
| Zimmermann et al., 2019 [65] | To evaluate the fracture behavior of different CAD/CAM ceramics and composites and one 3D printed composite as a function of different crown thicknesses (0.5, 1, and 1.5 mm). | Composite (els-3D Harz, Saremco Dental AG); 3D Printer (DLP Freeform Pro 2–ASIGA). | P | Fatigue and fracture load. | As none of the 0.5 mm ceramic crowns survived fatigue testing and all 0.5 mm composite crowns did, composites may have advantageous material characteristics compared to ceramic CAD/CAM materials for minimal restoration thicknesses. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature. Materials 2024, 17, 1380. https://doi.org/10.3390/ma17061380
Balestra D, Lowther M, Goracci C, Mandurino M, Cortili S, Paolone G, Louca C, Vichi A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature. Materials. 2024; 17(6):1380. https://doi.org/10.3390/ma17061380
Chicago/Turabian StyleBalestra, Dario, Morgan Lowther, Cecilia Goracci, Mauro Mandurino, Silvia Cortili, Gaetano Paolone, Chris Louca, and Alessandro Vichi. 2024. "3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature" Materials 17, no. 6: 1380. https://doi.org/10.3390/ma17061380





