Comparative Study of the Influence of Heat Treatment on Fracture Resistance of Different Ceramic Materials Used for CAD/CAM Systems
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Processing
2.2. Thermocycling
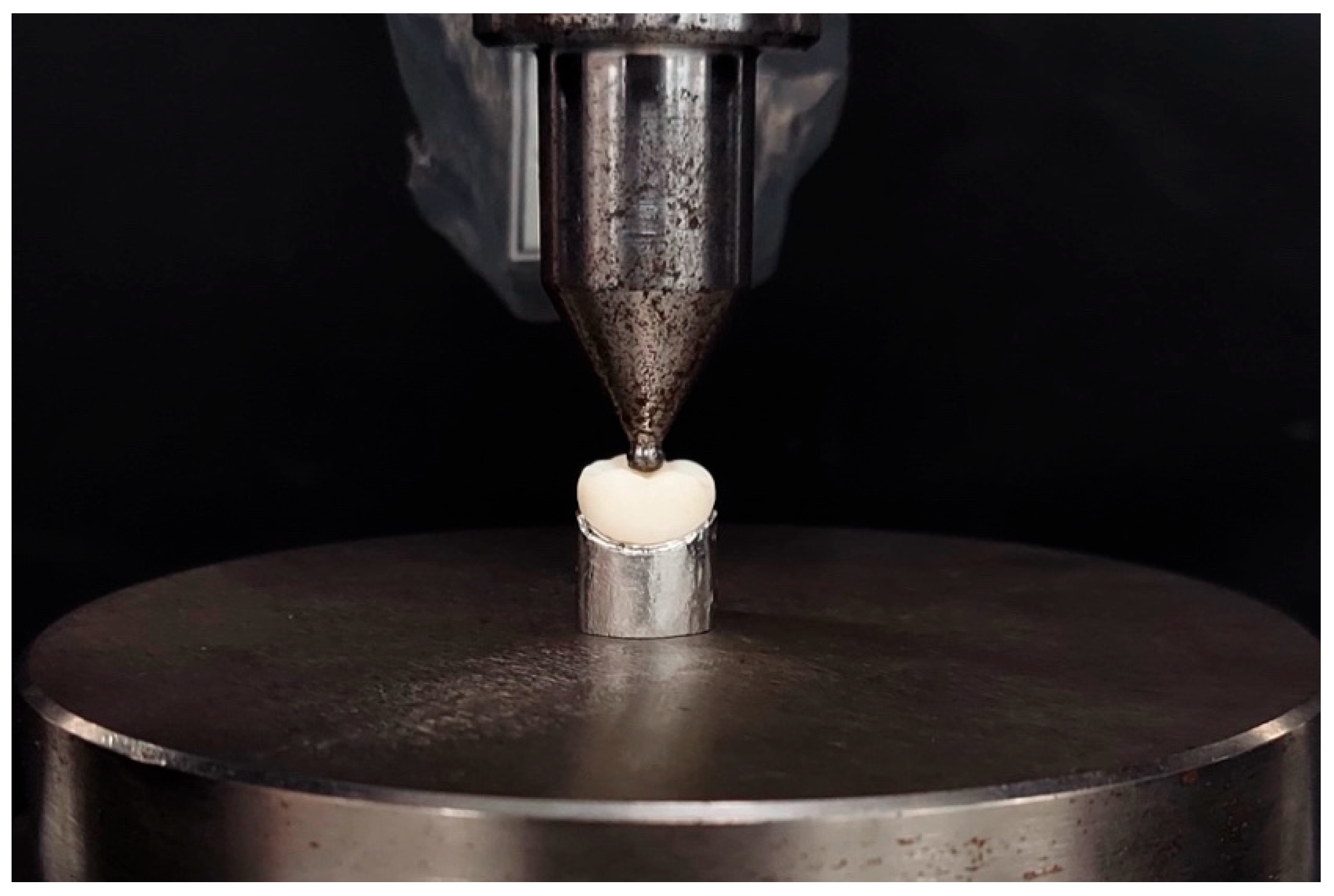
2.3. Fracture Resistance Test
2.4. Fracture Mode Evaluation
2.5. Data Analysis
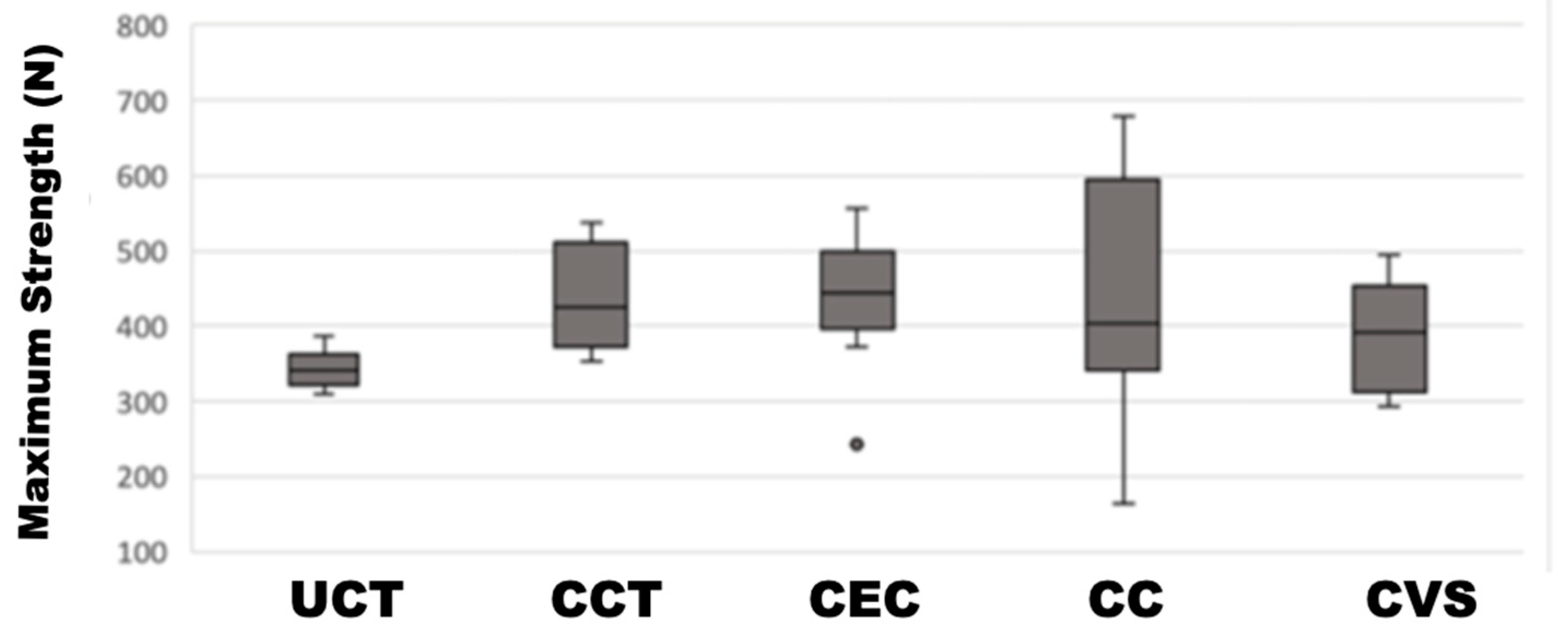
3. Results
4. Discussion
5. Conclusions
- In CCT, AHT optimizes the microstructure thanks to its advanced composition and the formation of new virgillite crystals, consequently increasing its FR, thus allowing for it to be resistant to possible fissures and cracks created by subtractive processes during the fabrication of restorations.
- The results given by CE allow for us to conclude that these ceramics have a high capacity of absorbing and distributing stresses without suffering fractures.
- Although CC displays the highest FR values, its high dispersion indicates inconsistencies; one must exercise caution while using it.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Choi, J.-W.; Kim, S.-Y.; Bae, J.-H.; Bae, E.-B.; Huh, J.-B. In Vitro Study of the Fracture Resistance of Monolithic Lithium Disilicate, Monolithic Zirconia, and Lithium Disilicate Pressed on Zirconia for Three-Unit Fixed Dental Prostheses. J. Adv. Prosthodont. 2017, 9, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Rada, S.; Zhang, J.; Rada, R.; Culea, E. Advanced Zirconia Ceramics Stabilized with Yttria and Magnesia: Structure and Vickers Microhardness. J. Mech. Behav. Biomed. Mater. 2022, 134, 105425. [Google Scholar] [CrossRef] [PubMed]
- Motro, P.F.K.; Kursoglu, P.; Kazazoglu, E. Effects of Different Surface Treatments on Stainability of Ceramics. J. Prosthet. Dent. 2012, 108, 231–237. [Google Scholar] [CrossRef] [PubMed]
- May, M.M.; Fraga, S.; May, L.G. Effect of Milling, Fitting Adjustments, and Hydrofluoric Acid Etching on the Strength and Roughness of CAD-CAM Glass-Ceramics: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2022, 128, 1190–1200. [Google Scholar] [CrossRef] [PubMed]
- Gautam, C.; Joyner, J.; Gautam, A.; Rao, J.; Vajtai, R. Zirconia based dental ceramics: Structure, mechanical properties, biocompatibility and applications. Dalton Trans. 2016, 45, 19194–19215. [Google Scholar] [CrossRef] [PubMed]
- Ordoñez Balladares, A.; Abad-Coronel, C.; Ramos, J.; Martín Biedma, B. Fracture Resistance of Sintered Monolithic Zirconia Dioxide in Different Thermal Units. Materials 2022, 15, 2478. [Google Scholar] [CrossRef]
- Rinke, S.; Zuck, T.; Hausdörfer, T.; Leha, A.; Wassmann, T.; Ziebolz, D. Prospective Clinical Evaluation of Chairside-Fabricated Zirconia-Reinforced Lithium Silicate Ceramic Partial Crowns—5-Year Results. Clin. Oral Investig. 2022, 26, 1593–1603. [Google Scholar] [CrossRef]
- Abdulrahman, S.; Von See Mahm, C.; Talabani, R.; Abdulateef, D. Evaluation of the clinical success of four different types of lithium disilicate ceramic restorations: A retrospective study. BMC Oral Health 2021, 21, 625. [Google Scholar] [CrossRef]
- Munoz, A.; Zhao, Z.; Paolone, G.; Louca, C.; Vichi, A. Flexural Strength of CAD/CAM Lithium-Based Silicate Glass–Ceramics: A Narrative Review. Materials 2023, 16, 4398. [Google Scholar] [CrossRef]
- Elsaka, S.E.; Elnaghy, A.M. Mechanical Properties of Zirconia Reinforced Lithium Silicate Glass-Ceramic. Dent. Mater. 2016, 32, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Cokic, S.M.; Vleugels, J.; Van Meerbeek, B.; Camargo, B.; Willems, E.; Li, M.; Zhang, F. Mechanical Properties, Aging Stability and Translucency of Speed-Sintered Zirconia for Chairside Restorations. Dent. Mater. 2020, 36, 959–972. [Google Scholar] [CrossRef] [PubMed]
- Kontonasaki, E.; Giasimakopoulos, P.; Rigos, A.E. Strength and Aging Resistance of Monolithic Zirconia: An Update to Current Knowledge. Jpn. Dent. Sci. Rev. 2020, 56, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital Dentistry: An Overview of Recent Developments for CAD/CAM Generated Restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Kirsch, C.; Ender, A.; Attin, T.; Mehl, A. Trueness of Four Different Milling Procedures Used in Dental CAD/CAM Systems. Clin. Oral Investig. 2017, 21, 551–558. [Google Scholar] [CrossRef]
- Yin, R.; Jang, Y.-S.; Lee, M.-H.; Bae, T.-S. Comparative Evaluation of Mechanical Properties and Wear Ability of Five CAD/CAM Dental Blocks. Materials 2019, 12, 2252. [Google Scholar] [CrossRef] [PubMed]
- Reid, D.; Matis, J.; Lien, W.; Raimondi, C.; Arnason, S.; DuVall, N.; Vandewalle, K. Optical and Mechanical Properties of New Ceramic CAD/CAM Materials. Oper. Dent. 2023, 48, 425–434. [Google Scholar] [CrossRef]
- Phark, J.; Duarte, S., Jr. Microstructural Considerations for Novel Lithium Disilicate Glass Ceramics: A Review. J. Esthet. Restor. Dent. 2022, 34, 92–103. [Google Scholar] [CrossRef]
- Hurle, K.; Lubauer, J.; Belli, R.; Lohbauer, U. On the Assignment of Quartz-like LiAlSi2O6-SiO2 Solid Solutions in Dental Lithium Silicate Glass-Ceramics: Virgilite, High Quartz, Low Quartz or Stuffed Quartz Derivatives? Dent. Mater. 2022, 38, 1558–1563. [Google Scholar] [CrossRef]
- Mangla, P. Measurement of Translucency, Biaxial Flexural Strength, and Radiopacity of Different Lithium Disilicate Materials. Master’s Thesis, The University of Alabama, Birmingham, AL, USA, 2022. [Google Scholar]
- Bosch, G.; Ender, A.; Mehl, A. A 3-Dimensional Accuracy Analysis of Chairside CAD/CAM Milling Processes. J. Prosthet. Dent. 2014, 112, 1425–1431. [Google Scholar] [CrossRef]
- Badawy, R.; El-Mowafy, O.; Tam, L.E. Fracture Toughness of Chairside CAD/CAM Materials–Alternative Loading Approach for Compact Tension Test. Dent. Mater. 2016, 32, 847–852. [Google Scholar] [CrossRef]
- Amesti-Garaizabal, A.; Agustín-Panadero, R.; Verdejo-Solá, B.; Fons-Font, A.; Fernández-Estevan, L.; Montiel-Company, J.; Solá-Ruíz, M.F. Fracture Resistance of Partial Indirect Restorations Made with CAD/CAM Technology. A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 1932. [Google Scholar] [CrossRef] [PubMed]
- Guarda, G.; Correr, A.; Gonçalves, L.; Costa, A.; Borges, G.; Sinhoreti, M.; Correr-Sobrinho, L. Effects of Surface Treatments, Thermocycling, and Cyclic Loading on the Bond Strength of a Resin Cement Bonded to a Lithium Disilicate Glass Ceramic. Oper. Dent. 2013, 38, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Seghi, R.; Denry, I.; Rosenstiel, S. Relative Fracture Toughness and Hardness of New Dental Ceramics. J. Prosthet. Dent. 1995, 74, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Sonmez, N.; Gultekin, P.; Turp, V.; Akgungor, G.; Sen, D.; Mijiritsky, E. Evaluation of Five CAD/CAM Materials by Microstructural Characterization and Mechanical Tests: A Comparative in Vitro Study. BMC Oral Health 2018, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Walker, P.D.; Ruse, N.D. “CAD-on” Interfaces–Fracture Mechanics Characterization. J. Prosthodont. 2019, 28, 982–987. [Google Scholar] [CrossRef]
- Elraggal, A.; Afifi, R.; Abdelraheem, I. Effect of Erosive Media on Microhardness and Fracture Toughness of CAD-CAM Dental Materials. BMC Oral Health 2022, 22, 191. [Google Scholar] [CrossRef]
- Wendler, M.; Belli, R.; Petschelt, A.; Mevec, D.; Harrer, W.; Lube, T.; Danzer, R.; Lohbauer, U. Chairside CAD/CAM Materials. Part 2: Flexural Strength Testing. Dent. Mater. 2017, 33, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.-S.; Choi, Y.-S.; Lee, H.-H.; Lee, J.-H.; Ahn, J. Comparison of Mechanical Properties of Chairside CAD/CAM Restorations Fabricated Using a Standardization Method. Materials 2021, 14, 3115. [Google Scholar] [CrossRef]
- Lohbauer, U.; Belli, R.; Alonso, A.A.; Goetz-Neunhoeffer, F.; Hurle, K. Effect of Sintering Parameters on Phase Evolution and Strength of Dental Lithium Silicate Glass-Ceramics. Dent. Mater. 2019, 35, 1360–1369. [Google Scholar] [CrossRef]
- Nejatidanesh, F.; Azadbakht, K.; Savabi, O.; Sharifi, M.; Shirani, M. Effect of Repeated Firing on the Translucency of CAD-CAM Monolithic Glass-Ceramics. J. Prosthet. Dent. 2020, 123, 530.e1–530.e6. [Google Scholar] [CrossRef]
- Vasiliu, R.-D.; Porojan, S.D.; Porojan, L. In Vitro Study of Comparative Evaluation of Marginal and Internal Fit between Heat-Pressed and CAD-CAM Monolithic Glass-Ceramic Restorations after Thermal Aging. Materials 2020, 13, 4239. [Google Scholar] [CrossRef]
- Azarbal, A.; Azarbal, M.; Engelmeier, R.L.; Kunkel, T.C. Marginal Fit Comparison of CAD/CAM Crowns Milled from Two Different Materials. J. Prosthodont. 2018, 27, 421–428. [Google Scholar] [CrossRef]
- Kim, J.-H.; Oh, S.; Uhm, S.-H. Effect of the Crystallization Process on the Marginal and Internal Gaps of Lithium Disilicate CAD/CAM Crowns. BioMed Res. Int. 2016, 2016, 8635483. [Google Scholar] [CrossRef] [PubMed]
- Falahchai, M.; Ghavami-Lahiji, M.; Rasaie, V.; Amin, M.; Neshandar Asli, H. Comparison of Mechanical Properties, Surface Roughness, and Color Stability of 3D-Printed and Conventional Heat-Polymerizing Denture Base Materials. J. Prosthet. Dent. 2023, 130, 266.e1–266.e8. [Google Scholar] [CrossRef]
- Stanley, M.; Paz, A.G.; Miguel, I.; Coachman, C. Fully Digital Workflow, Integrating Dental Scan, Smile Design and CAD-CAM: Case Report. BMC Oral Health 2018, 18, 134. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Benic, G.I.; Fehmer, V.; Hämmerle, C.H.; Mühlemann, S. Randomized Controlled Within-Subject Evaluation of Digital and Conventional Workflows for the Fabrication of Lithium Disilicate Single Crowns. Part II: CAD-CAM versus Conventional Laboratory Procedures. J. Prosthet. Dent. 2017, 118, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Zarone, F.; Ferrari, M. The Complete Digital Workflow in Fixed Prosthodontics: A Systematic Review. BMC Oral Health 2017, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Conejo, J. The Current State of Chairside Digital Dentistry and Materials. Dent. Clin. 2019, 63, 175–197. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, L.H.; de Lima, E.; Miranda, R.B.d.P.; Favero, S.S.; Lohbauer, U.; Cesar, P.F. Dental Ceramics: A Review of New Materials and Processing Methods. Braz. Oral Res. 2017, 31, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Saleh, A.R.M.; Al-Ani, M.; ALRawi, T.; Al-Edressi, G. An In-Vitro Comparison of Fracture Resistance of Three CAD/CAM Ceramic Materials for Fabricating Veneer. Saudi Dent. J. 2021, 33, 745–752. [Google Scholar] [CrossRef]
- Blunck, U.; Fischer, S.; Hajtó, J.; Frei, S.; Frankenberger, R. Ceramic Laminate Veneers: Effect of Preparation Design and Ceramic Thickness on Fracture Resistance and Marginal Quality in Vitro. Clin. Oral Investig. 2020, 24, 2745–2754. [Google Scholar] [CrossRef]
- Heidari, N.; Amawi, R.; Seweryniak, P.; Bakitian, F.; Vult von Steyern, P. Fracture Resistance and Fracture Behaviour of Monolithic Multi-Layered Translucent Zirconia Fixed Dental Prostheses with Different Placing Strategies of Connector: An in Vitro Study. Clin. Cosmet. Investig. Dent. 2022, 14, 61–69. [Google Scholar] [CrossRef]
- Zacher, J.; Bauer, R.; Hanie Krifka, S.; Rosentritt, M. In Vitro Performance and Fracture Resistance of Pressed or CAD/CAM Milled Ceramic Implant-Supported Screw-Retained or Cemented Anterior FDPs. J. Prosthodont. Res. 2021, 65, 208–212. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Ordoñez Balladares, A.; Fajardo, J.I.; Martín Biedma, B.J. Resistance to Fracture of Lithium Disilicate Feldspathic Restorations Manufactured Using a CAD/CAM System and Crystallized with Different Thermal Units and Programs. Materials 2021, 14, 3215. [Google Scholar] [CrossRef]
- Denry, I.; Goudouri, O.; Harless, J.D.; Hubbard, E.; Holloway, J.A. Strontium-releasing Fluorapatite Glass-ceramics: Crystallization Behavior, Microstructure, and Solubility. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018, 106, 1421–1430. [Google Scholar] [CrossRef]
- Cattell, M.J.; Patzig, C.; Bissasu, S.; Tsoutsos, A.; Karpukhina, N. Nucleation Efficacy and Flexural Strength of Novel Leucite Glass-Ceramics. Dent. Mater. 2020, 36, 592–602. [Google Scholar] [CrossRef] [PubMed]
- Gold, S.A.; Ferracane, J.L.; da Costa, J. Effect of Crystallization Firing on Marginal Gap of CAD/CAM Fabricated Lithium Disilicate Crowns. J. Prosthodont. 2018, 27, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Lubauer, J.; Belli, R.; Peterlik, H.; Hurle, K.; Lohbauer, U. Grasping the Lithium Hype: Insights into Modern Dental Lithium Silicate Glass-Ceramics. Dent. Mater. 2022, 38, 318–332. [Google Scholar] [CrossRef]
- Rosentritt, M.; Hahnel, S.; Engelhardt, F.; Behr, M.; Preis, V. In Vitro Performance and Fracture Resistance of CAD/CAM-Fabricated Implant Supported Molar Crowns. Clin. Oral Investig. 2017, 21, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Riquieri, H.; Monteiro, J.B.; Viegas, D.C.; Campos, T.M.B.; De Melo, R.M.; De Siqueira Ferreira Anzaloni Saavedra, G. Impact of Crystallization Firing Process on the Microstructure and Flexural Strength of Zirconia-Reinforced Lithium Silicate Glass-Ceramics. Dent. Mater. 2018, 34, 1483–1491. [Google Scholar] [CrossRef]
- Romanyk, D.L.; Guo, Y.; Rae, N.; Veldhuis, S.; Sirovica, S.; Fleming, G.J.; Addison, O. Strength-Limiting Damage and Its Mitigation in CAD-CAM Zirconia-Reinforced Lithium-Silicate Ceramics Machined in a Fully Crystallized State. Dent. Mater. 2020, 36, 1557–1565. [Google Scholar] [CrossRef]
- Kim, S.-H.; Choi, Y.-S.; Kang, K.-H.; Att, W. Effects of Thermal and Mechanical Cycling on the Mechanical Strength and Surface Properties of Dental CAD-CAM Restorative Materials. J. Prosthet. Dent. 2022, 128, 79–88. [Google Scholar] [CrossRef]
- Alakkad, L.; Kostagianni, A.; Finkelman, M.; Maawadh, A.; Ali, A.; Papathanasiou, A. Biaxial Flexural Strength of Various CAD-CAM Glass-Ceramic Materials. Am. J. Dent. 2021, 34, 91–96. [Google Scholar]
- Simba, B.G.; Ribeiro, M.V.; Suzuki, P.A.; Alves, M.F.R.P.; Strecker, K.; Santos, C.D. Mechanical Properties of Lithium Metasilicate after Short-Term Thermal Treatments. J. Mech. Behav. Biomed. Mater. 2019, 98, 179–186. [Google Scholar] [CrossRef]
- Serbena, F.C.; Zanotto, E.D. Internal Residual Stresses in Glass-Ceramics: A Review. J. Non-Cryst. Solids 2012, 358, 975–984. [Google Scholar] [CrossRef]
- Belli, R.; Lohbauer, U.; Goetz-Neunhoeffer, F.; Hurle, K. Crack-Healing during Two-Stage Crystallization of Biomedical Lithium (Di) Silicate Glass-Ceramics. Dent. Mater. 2019, 35, 1130–1145. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, F.; Spintzyk, S.; Geis-Gerstorfer, J.; Huettig, F. Influence of Minimal Extended Firing on Dimensional, Optical, and Mechanical Properties of Crystalized Zirconia-Reinforced Lithium Silicate Glass Ceramic. J. Mech. Behav. Biomed. Mater. 2020, 104, 103644. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Dal Piva, A.M.O.; Nedeljkovic, I.; Tribst, J.P.M.; Feilzer, A.J.; Kleverlaan, C.J. Effect of Glazing Technique and Firing on Surface Roughness and Flexural Strength of an Advanced Lithium Disilicate. Clin. Oral Investig. 2023, 27, 3917–3926. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Schmid, A.; Huber, C.; Strasser, T. In Vitro Mastication Simulation and Wear Test of Virgilite and Advanced Lithium Disilicate Ceramics. Int. J. Prosthodont. 2022, 35, 770–776. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Ruggiero, G.; Leone, R.; Breschi, L.; Leuci, S.; Sorrentino, R. Zirconia-Reinforced Lithium Silicate (ZLS) Mechanical and Biological Properties: A Literature Review. J. Dent. 2021, 109, 103661. [Google Scholar] [CrossRef] [PubMed]
- Pitiaumnuaysap, L.; Phokhinchatchanan, P.; Suputtamongkol, K.; Kanchanavasita, W. Fracture Resistance of Four Dental Computer-Aided Design and Computer-Aided Manufacturing Glass-Ceramics. Mahidol Dent. J. 2017, 37, 201–208. [Google Scholar]
- Hallmann, L.; Ulmer, P.; Kern, M. Effect of Microstructure on the Mechanical Properties of Lithium Disilicate Glass-Ceramics. J. Mech. Behav. Biomed. Mater. 2018, 82, 355–370. [Google Scholar] [CrossRef] [PubMed]
- Schwindling, F.S.; Rues, S.; Schmitter, M. Fracture Resistance of Glazed, Full-Contour ZLS Incisor Crowns. J. Prosthodont. Res. 2017, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, J.B.; Riquieri, H.; Prochnow, C.; Guilardi, L.F.; Pereira, G.K.R.; Borges, A.L.S.; de Melo, R.M.; Valandro, L.F. Fatigue Failure Load of Two Resin-Bonded Zirconia-Reinforced Lithium Silicate Glass-Ceramics: Effect of Ceramic Thickness. Dent. Mater. 2018, 34, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Corado, H.P.; da Silveira, P.H.; Ortega, V.L.; Ramos, G.G.; Elias, C.N. Flexural Strength of Vitreous Ceramics Based on Lithium Disilicate and Lithium Silicate Reinforced with Zirconia for CAD/CAM. Int. J. Biomater. 2022, 2022, 5896511. [Google Scholar] [CrossRef] [PubMed]
- Hampe, R.; Theelke, B.; Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Fracture Toughness Analysis of Ceramic and Resin Composite CAD/CAM Material. Oper. Dent. 2019, 44, E190–E201. [Google Scholar] [CrossRef]
- Vichi, A.; Zhao, Z.; Paolone, G.; Scotti, N.; Mutahar, M.; Goracci, C.; Louca, C. Factory Crystallized Silicates for Monolithic Metal-Free Restorations: A Flexural Strength and Translucency Comparison Test. Materials 2022, 15, 7834. [Google Scholar] [CrossRef]
- Freitas, J.S.; Souza, L.F.B.; Pereira, G.K.R.; May, L.G. Surface Properties and Flexural Fatigue Strength of an Advanced Lithium Disilicate. J. Mech. Behav. Biomed. Mater. 2023, 147, 106154. [Google Scholar] [CrossRef]
- Keshmiri, N.; Alaghehmand, H.; Mokhtarpour, F. Effect of Hydrofluoric Acid Surface Treatments on Surface Roughness and Three-Point Flexural Strength of Suprinity Ceramic. Front. Dent. 2020, 17, 1. [Google Scholar] [CrossRef]
- Matis, J.I. Optical Properties of Novel Ceramic CAD/CAM Materials. Ph.D. Thesis, Uniformed Services University of the Health Sciences, Bethesda, MD, USA, 20 May 2022. [Google Scholar]
- Ahlholm, P.; Sipilä, K.; Vallittu, P.; Jakonen, M.; Kotiranta, U. Digital versus Conventional Impressions in Fixed Prosthodontics: A Review. J. Prosthodont. 2018, 27, 35–41. [Google Scholar] [CrossRef]
- Fung, L.; Brisebois, P. Implementing Digital Dentistry into Your Esthetic Dental Practice. Dent. Clin. 2020, 64, 645–657. [Google Scholar] [CrossRef]
- Mota, E.G.; Smidt, L.N.; Fracasso, L.M.; Burnett Jr, L.H.; Spohr, A.M. The Effect of Milling and Postmilling Procedures on the Surface Roughness of CAD/CAM Materials. J. Esthet. Restor. Dent. 2017, 29, 450–458. [Google Scholar] [CrossRef]
- Albelasy, E.; Hamama, H.H.; Tsoi, J.K.; Mahmoud, S.H. Influence of Material Type, Thickness and Storage on Fracture Resistance of CAD/CAM Occlusal Veneers. J. Mech. Behav. Biomed. Mater. 2021, 119, 104485. [Google Scholar] [CrossRef]
- Hamza, T.A.; Sherif, R.M. Fracture Resistance of Monolithic Glass-ceramics versus Bilayered Zirconia-based Restorations. J. Prosthodont. 2019, 28, e259–e264. [Google Scholar] [CrossRef]
- Jurado, C.A.; Lee, D.; Cortes, D.; Kaleinikova, Z.; Hernandez, A.I.; Donato, M.V.; Tsujimoto, A. Fracture Resistance of Chairside CAD/CAM Molar Crowns Fabricated with Different Lithium Disilicate Ceramic Materials. Int. J. Prosthodont. 2023, 36, 722–729. [Google Scholar] [CrossRef]
- Chen, S.E.; Park, A.C.; Wang, J.; Knoernschild, K.L.; Campbell, S.; Yang, B. Fracture Resistance of Various Thickness e. Max CAD Lithium Disilicate Crowns Cemented on Different Supporting Substrates: An in Vitro Study. J. Prosthodont. 2019, 28, 997–1004. [Google Scholar] [CrossRef]
- Bencun, M.; Ender, A.; Wiedemeier, D.B.; Mehl, A. Fracture Load of CAD/CAM Feldspathic Crowns Influenced by Abutment Material. Materials 2020, 13, 3407. [Google Scholar] [CrossRef] [PubMed]
- García-Engra, G.; Fernandez-Estevan, L.; Casas-Terrón, J.; Fons-Font, A.; Castelo-Baz, P.; Agustín-Panadero, R.; Román-Rodriguez, J.L. Fracture Resistance of New Metal-Free Materials Used for CAD-CAM Fabrication of Partial Posterior Restorations. Medicina 2020, 56, 132. [Google Scholar] [CrossRef] [PubMed]
- Fouda, A.M.; Atta, O.; Özcan, M.; Stawarczyk, B.; Glaum, R.; Bourauel, C. An Investigation on Fatigue, Fracture Resistance, and Color Properties of Aesthetic CAD/CAM Monolithic Ceramics. Clin. Oral Investig. 2023, 27, 2653–2665. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Calle, C.; Abril, G.; Paltán, C.A.; Fajardo, J.I. Fracture Resistance Analysis of CAD/CAM Interim Fixed Prosthodontic Materials: PMMA, Graphene, Acetal Resin and Polysulfone. Polymers 2023, 15, 1761. [Google Scholar] [CrossRef] [PubMed]




| Name of Material | Manufacturer | Lot Number | Composition |
|---|---|---|---|
| Cerec Tessera | Dentsply Sirona™/Germany | 16015140 | Li2Si2O5: 90% Li3PO4: 5% Li0.5Al0.5Si2.5O6 (virgilite): 5% |
| Emax CAD | Ivoclar Vivadent™/Liechtenstein | 6788824 | SiO2: 57–80% Li2O: 11–19% K2O: 0–13% P2O5: 0–11% ZrO2: 0–8% ZnO: 0–8% Coloring oxides: 0–8% |
| Vita Suprinity | Vita Zahnfabrik/Germany | 7971329 | SiO2: 56–64% Li2O: 15–21% ZrO2: 8–12% P2O5: 3–8% K2O: 1–4% Al2O3: 1–4% CeO2: 0–4% Pigments: 0–4% |
| Cameo | Aidite/Singapore | 9180451 | 50–70% SiO2; 19–20% Li2O; 0–13% K2O; 0–11% P2O5; 0–5% ZrO2, 0–8% ZnO; 0–11% others + coloring |
| Groups | Ceramics | Samples |
|---|---|---|
| Group 1 | Cerec Tessera (CCT) | 10 |
| Group 2 | Cerec Tessera (UCT) | 10 |
| Group 3 | Emax Cad (CEC) | 20 |
| Group 4 | Suprinity (CVS) | 20 |
| Group 5 | Cameo (CC) | 20 |
| Name of Material | Oven | Manufacturer | Heating Units | Time |
|---|---|---|---|---|
| Cerec Tessera | Programat P310 | Ivoclar Vivadent™/ Liechtenstein | 760 °C | 2 min |
| Emax CAD | 850 °C | 7 min | ||
| Vita Suprinity | 840 °C | 8 min | ||
| Cameo | 840 °C | 6 min |
| Sample 1–Sample 2 | Test Statistic | Median | Sig. |
|---|---|---|---|
| Tessera uncrystallized–Cameo | −14,900 | 62.677 | 0.017 * |
| Tessera uncrystallized–Tessera crystallized | −17,189 | 83.924 | 0.008 * |
| Tessera uncrystallized–E-Max | −17,500 | 103.863 | 0.005 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balladares, A.O.; Abad-Coronel, C.; Ramos, J.C.; Fajardo, J.I.; Paltán, C.A.; Martín Biedma, B.J. Comparative Study of the Influence of Heat Treatment on Fracture Resistance of Different Ceramic Materials Used for CAD/CAM Systems. Materials 2024, 17, 1246. https://doi.org/10.3390/ma17061246
Balladares AO, Abad-Coronel C, Ramos JC, Fajardo JI, Paltán CA, Martín Biedma BJ. Comparative Study of the Influence of Heat Treatment on Fracture Resistance of Different Ceramic Materials Used for CAD/CAM Systems. Materials. 2024; 17(6):1246. https://doi.org/10.3390/ma17061246
Chicago/Turabian StyleBalladares, Andrea Ordoñez, Cristian Abad-Coronel, Joao Carlos Ramos, Jorge I. Fajardo, Cesar A. Paltán, and Benjamín José Martín Biedma. 2024. "Comparative Study of the Influence of Heat Treatment on Fracture Resistance of Different Ceramic Materials Used for CAD/CAM Systems" Materials 17, no. 6: 1246. https://doi.org/10.3390/ma17061246










