Design, Stereolithographic 3D Printing, and Characterization of TPMS Scaffolds
Abstract
1. Introduction
2. Materials and Methods
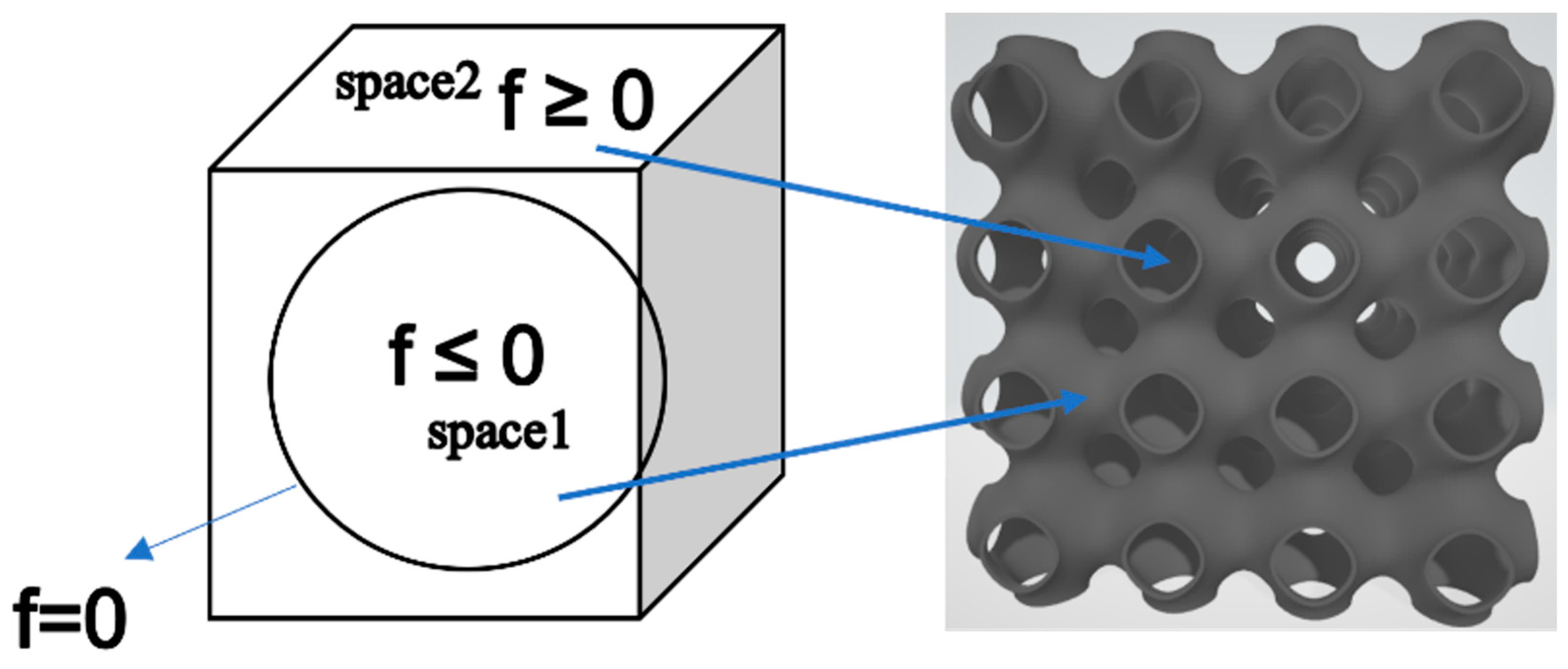
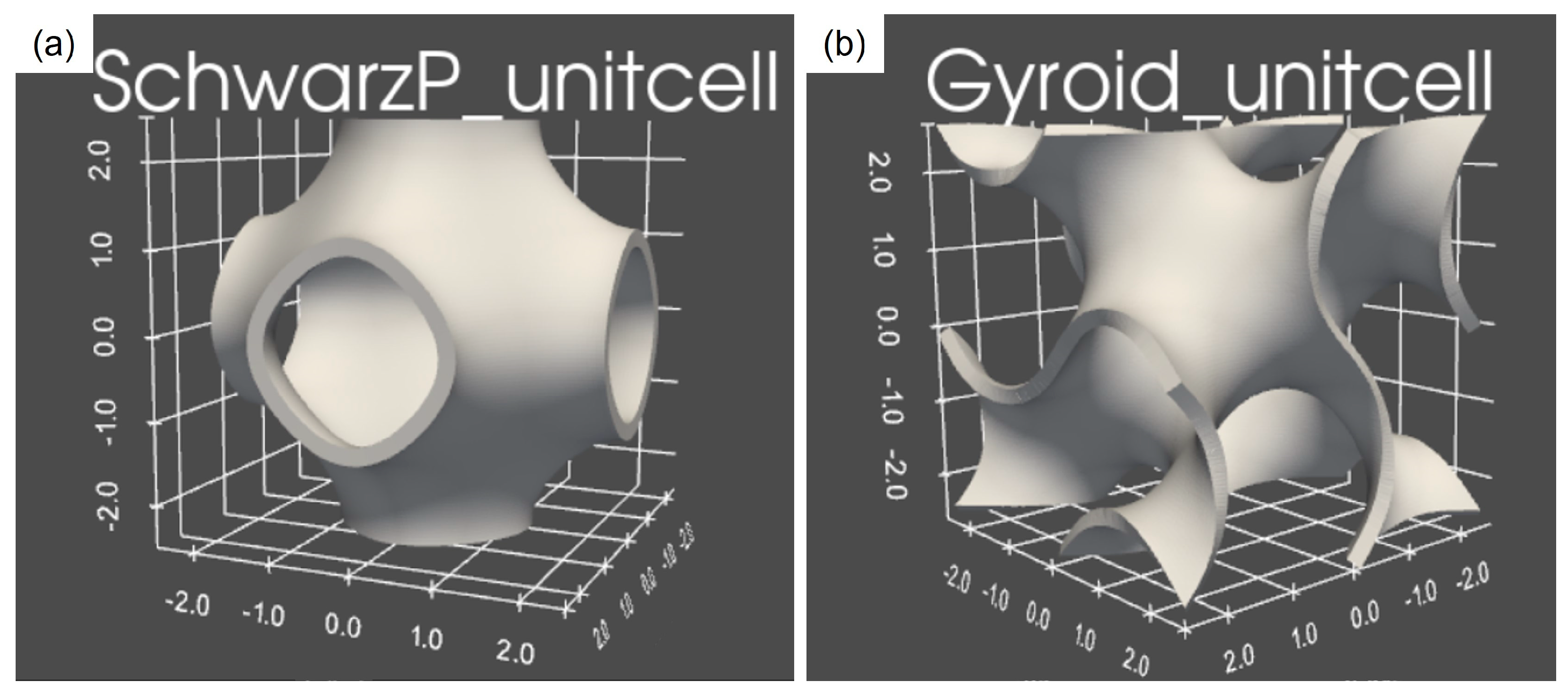
2.1. Design of Scaffolds Based on TPMSs
2.2. Scaffold Fabrication
2.3. Materials
2.4. Case Studies
2.5. Scaffold Characterizations
3. Results and Discussion
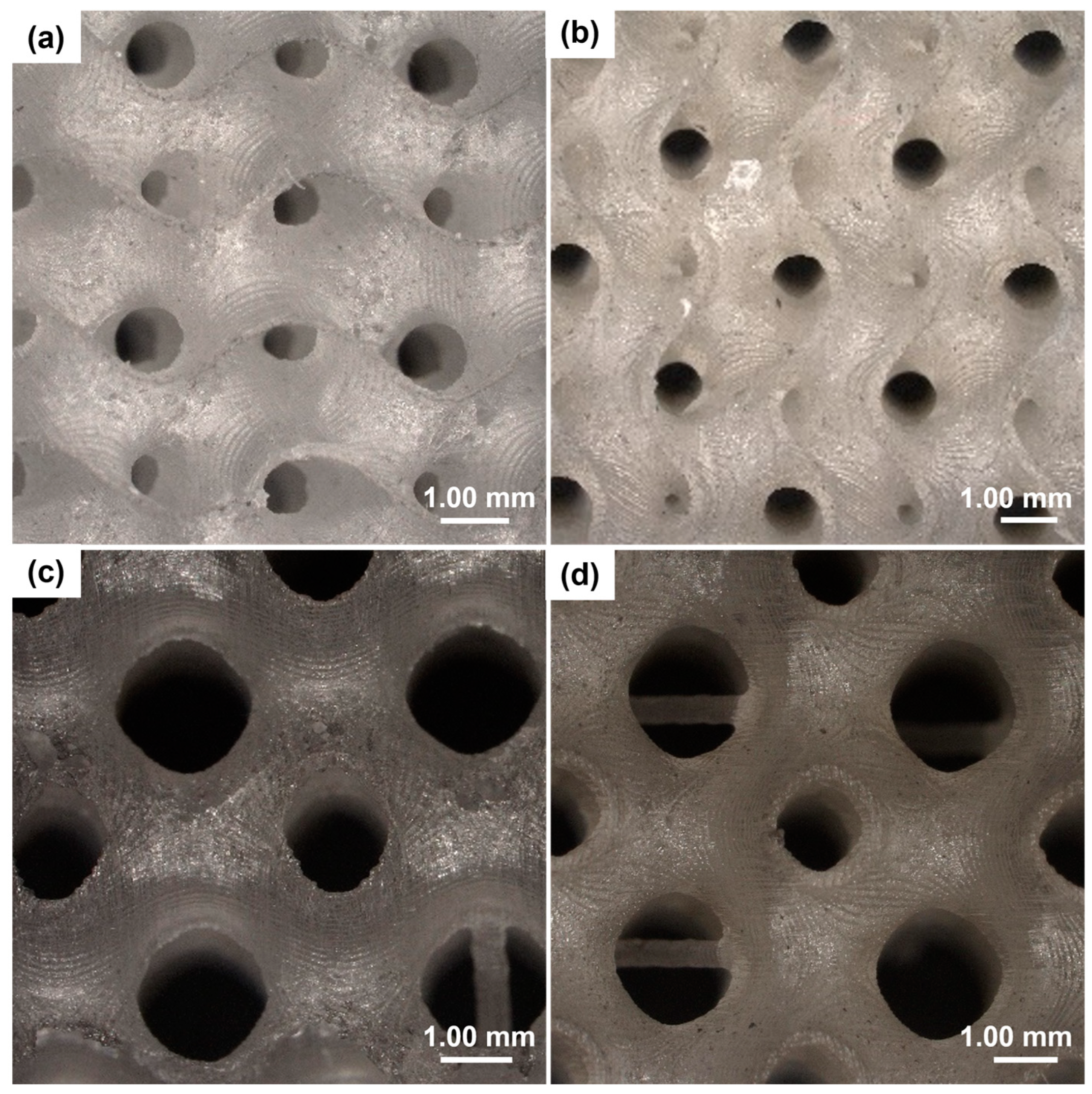
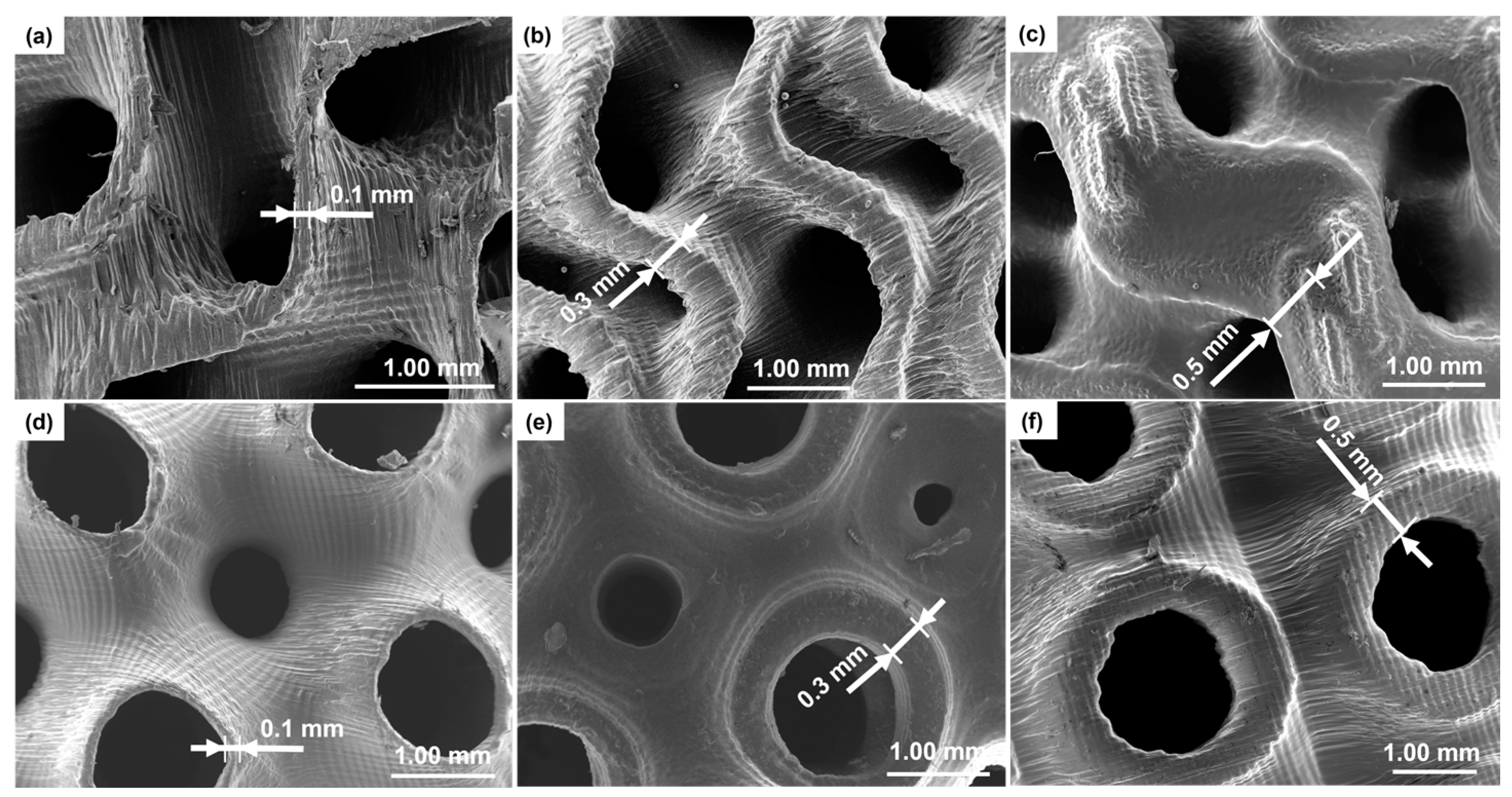
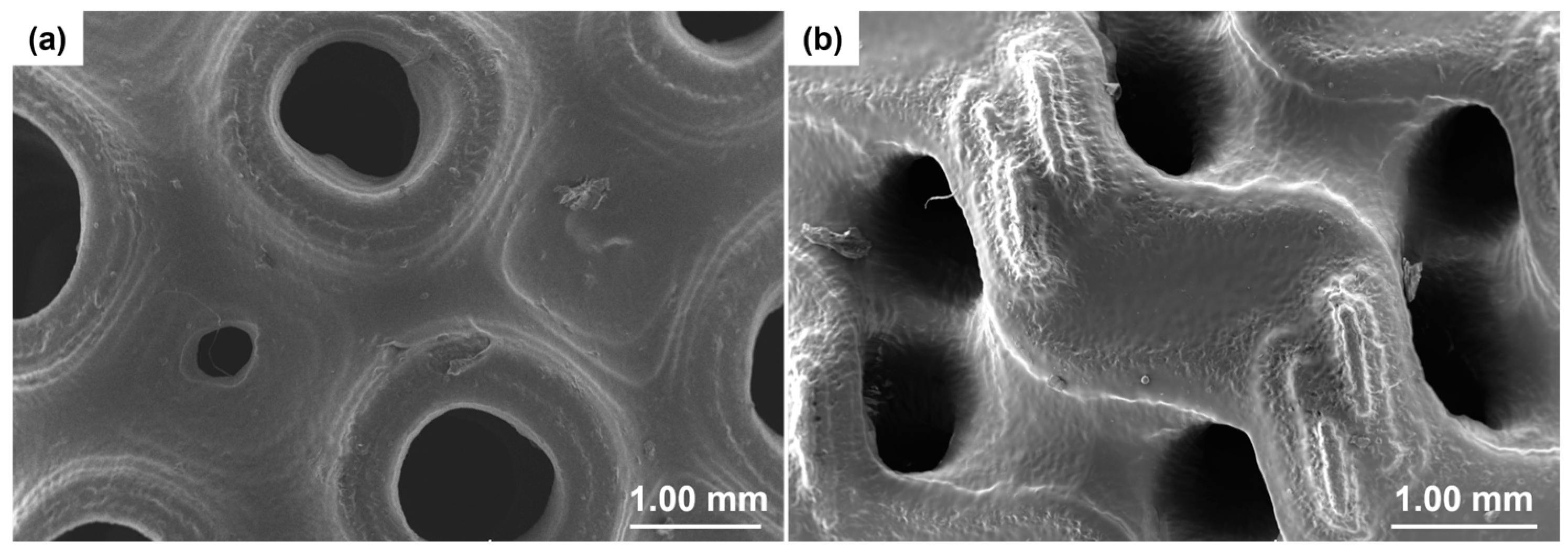
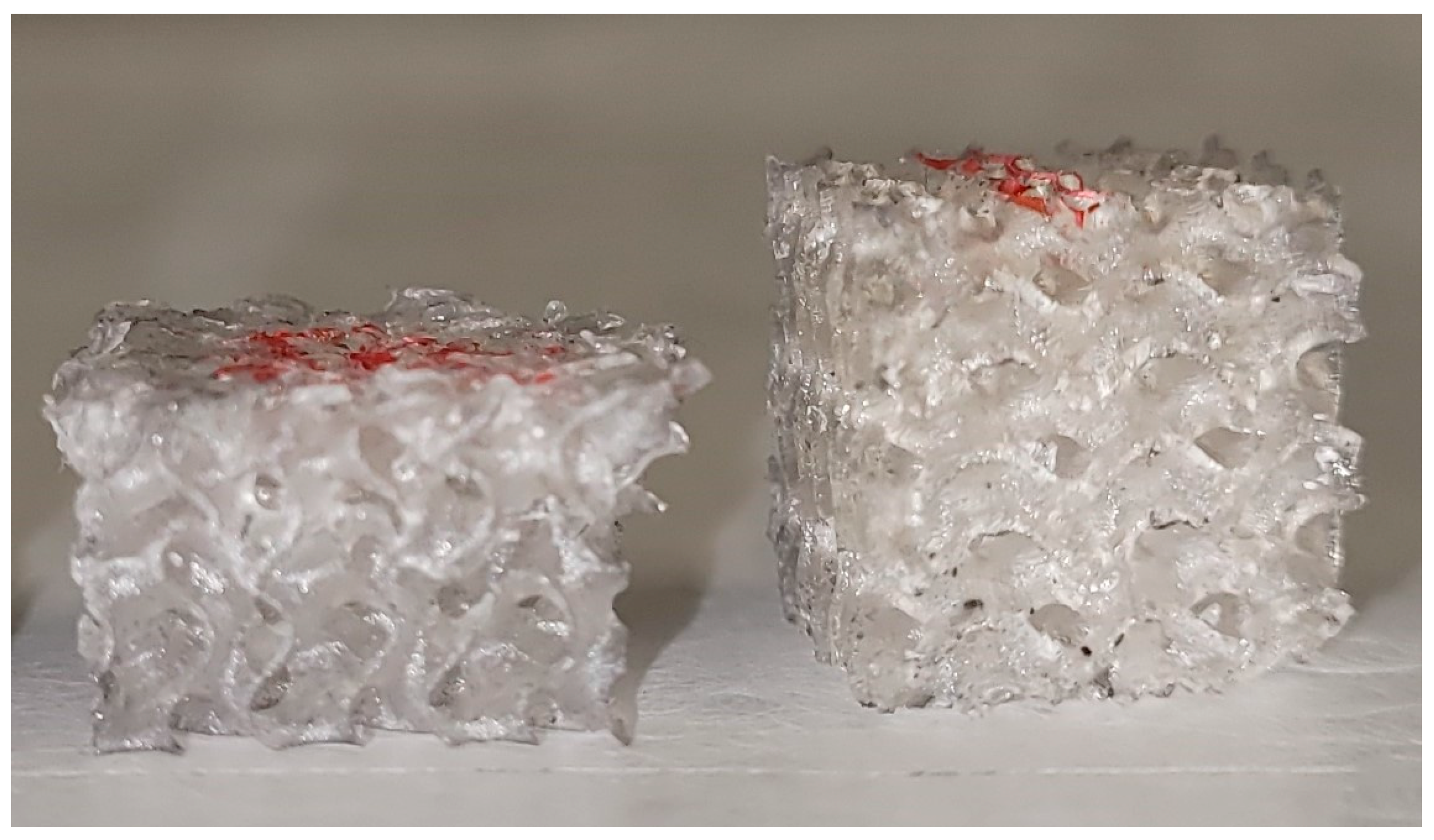
3.1. Geometry and Morphology of Scaffolds
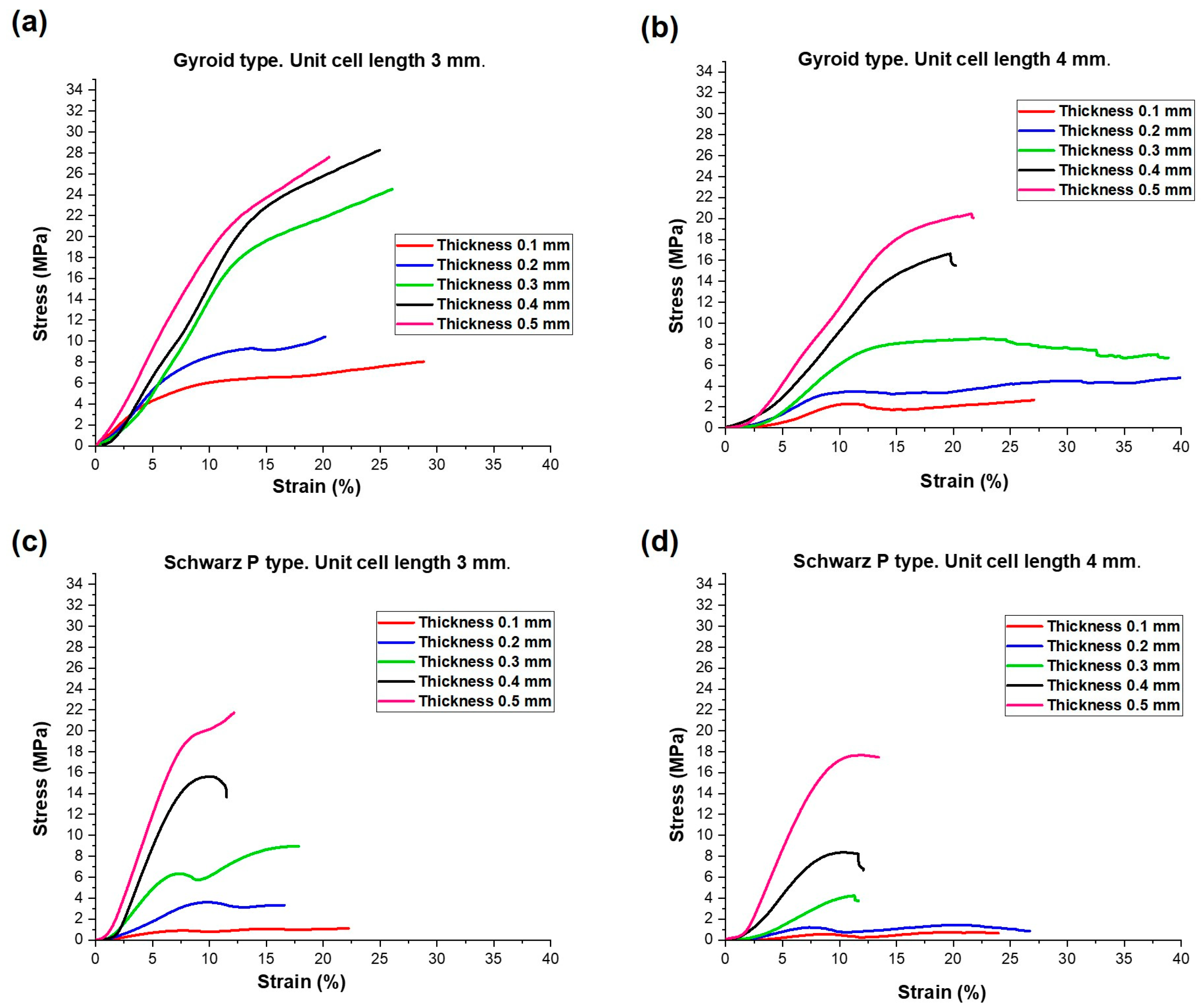
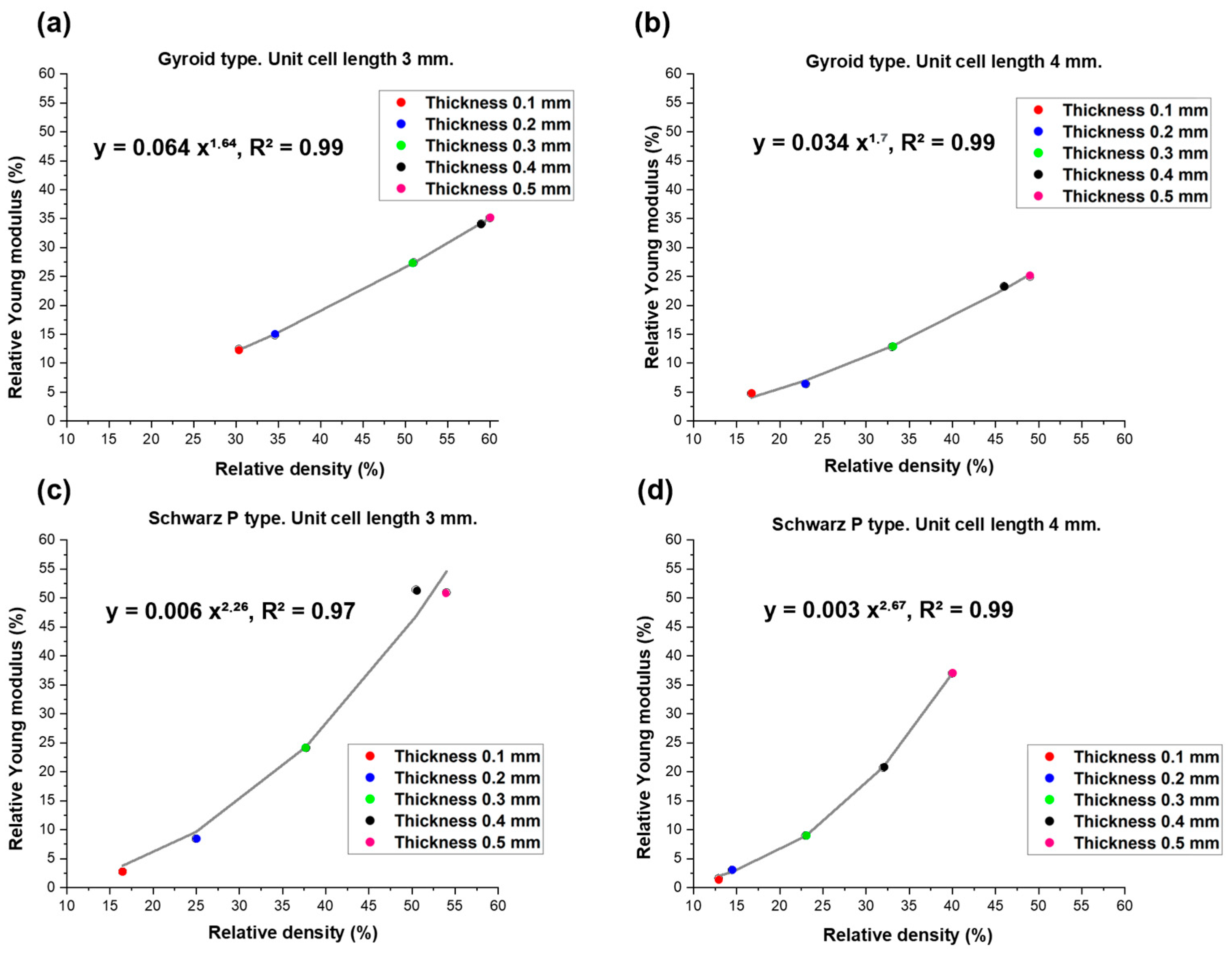
3.2. Mechanical Results
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tofail, S.A.M.; Koumoulos, E.P.; Bandyopadhyay, A.; Bose, S.; O’Donoghue, L.; Charitidis, C. Additive manufacturing: Scientific and technological challenges, market uptake and opportunities. Mater. Today 2018, 21, 22–37. [Google Scholar] [CrossRef]
- Langer, R.; Vacanti, J.P. Tissue engineering. Science 1993, 260, 920–926. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, F.J. Biomaterials & scaffolds for tissue engineering. Mater. Today 2011, 14, 88–95. [Google Scholar]
- Dimitriou, R.; Mataliotakis, G.I.; Angoules, A.G.; Kanakaris, N.K.; Giannoudis, P.V. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: A systematic review. Injury 2011, 42 (Suppl. S2), S3–S15. [Google Scholar] [CrossRef] [PubMed]
- Hutmacher, D.W. Scaffolds in tissue engineering bone and cartilage. Biomaterials 2000, 21, 2529–2543. [Google Scholar] [CrossRef] [PubMed]
- Baino, F.; Fiume, E.; Barberi, J.; Kargozar, S.; Marchi, J.; Massera, J.; Verné, E. Processing methods for making porous bioactive glass-based scaffolds—A state-of-the-art review. Int. J. Appl. Ceram. Technol. 2019, 16, 1762–1796. [Google Scholar] [CrossRef]
- Chocholata, P.; Kulda, V.; Babuska, V. Fabrication of scaffolds for bone-tissue regeneration. Materials 2019, 12, 568. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, T.; Shahroodi, A.; Ebrahimzadeh, M.H.; Mousavian, A.; Movaffagh, J.; Moradi, A. Current concepts in scaffolding for bone tissue engineering. Arch. Bone Jt. Surg. 2018, 6, 90–99. [Google Scholar]
- Reznikov, N.; Shahar, R.; Weiner, S. Bone hierarchical structure in three dimensions. Acta Biomater. 2014, 10, 3815–3826. [Google Scholar] [CrossRef]
- Perić Kačarević, Ž.; Rider, P.; Alkildani, S.; Retnasingh, S.; Čandrlić, M.; Schnettler, R.; Gosau, M.; Smeets, R.; Jung, O.; Barbeck, M. An introduction to bone tissue engineering. Int. J. Artif. Organs 2020, 43, 69–86. [Google Scholar] [CrossRef]
- Salgado, A.J.; Coutinho, O.P.; Reis, R.L. Bone tissue engineering: State of the art and future trends. Macromol. Biosci. 2004, 4, 743–765. [Google Scholar] [CrossRef] [PubMed]
- Stevens, B.; Yang, Y.; Mohandas, A.; Stucker, B.; Nguyen, K.T. A review of materials, fabrication methods, and strategies used to enhance bone regeneration in engineered bone tissues. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 85, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Farag, M.M. Recent trends on biomaterials for tissue regeneration applications: Review. J. Mater. Sci. 2023, 58, 527–558. [Google Scholar] [CrossRef]
- Donnaloja, F.; Jacchetti, E.; Soncini, M.; Raimondi, M.T. Natural and synthetic polymers for bone scaffolds optimization. Polymers 2020, 12, 905. [Google Scholar] [CrossRef]
- Huang, Y.-Z.; Xie, H.-Q.; Li, X. Scaffolds in bone tissue engineering: Research progress and current applications. In Encyclopedia of Bone Biology; Elsevier: Amsterdam, The Netherlands, 2020; pp. 204–215. [Google Scholar]
- Baino, F.; Novajra, G.; Vitale-Brovarone, C. Bioceramics and scaffolds: A winning combination for tissue engineering. Front. Bioeng. Biotechnol. 2015, 3, 202. [Google Scholar] [CrossRef] [PubMed]
- Qu, H.; Fu, H.; Han, Z.; Sun, Y. Biomaterials for bone tissue engineering scaffolds: A review. RSC Adv. 2019, 9, 26252–26262. [Google Scholar] [CrossRef]
- Torquato, S.; Donev, A. Minimal surfaces and multifunctionality. Proc. R. Soc. A 2004, 460, 1849–1856. [Google Scholar] [CrossRef]
- Yan, C.; Hao, L.; Hussein, A.; Bubb, S.L.; Young, P.; Raymont, D. Evaluation of light-weight AlSi10Mg periodic cellular lattice structures fabricated via direct metal laser sintering. J. Mater. Process. Technol. 2014, 214, 856–886. [Google Scholar] [CrossRef]
- Yan, C.; Hao, L.; Hussein, A.; Young, P.; Raymont, D. Advanced lightweight 316L stainless steel cellular lattice structures fabricated via selective laser melting. Mater. Des. 2014, 55, 533–541. [Google Scholar] [CrossRef]
- Mustafa, N.S.; Akhmal, N.H.; Izman, S.; Ab Talib, M.H.; Shaiful, A.I.M.; Omar, M.N.B.; Yahaya, N.Z.; Illias, S. Application of computational method in designing a unit cell of bone tissue engineering scaffold: A review. Polymers 2021, 13, 1584. [Google Scholar] [CrossRef]
- Whitehead, A.S. Triply Periodic Minimal Surfaces. WeWantToLearn.net. 2019. Available online: https://wewanttolearn.wordpress.com/2019/02/03/triply-periodic-minimal-surfaces/ (accessed on 18 January 2024).
- Zhou, X.; Jin, Y.; Du, J. Functionally Graded Scaffolds with programmable pore size distribution based on triply periodic minimal surface fabricated by selective laser melting. Materials 2020, 13, 5046. [Google Scholar] [CrossRef]
- Jin, Y.; Kong, H.; Zhou, X.; Li, G.; Du, J. Design and characterization of sheet-based gyroid porous structures with bioinspired functional gradients. Materials 2020, 13, 3844. [Google Scholar] [CrossRef]
- Kapfer, S.C.; Hyde, S.T.; Mecke, K.; Arns, C.H.; Schroeder-Turk, G.E. Minimal surface scaffold designs for tissue engineering. Biomaterials 2011, 32, 6875–6882. [Google Scholar] [CrossRef]
- Melchels, F.P.; Bertoldi, K.; Gabbrielli, R.; Velders, A.H.; Feijen, J.; Grijpma, D.W. Mathematically designed tissue engineering scaffold architectures prepared by stereolithography. Biomaterials 2010, 31, 6909–6916. [Google Scholar] [CrossRef] [PubMed]
- Olivares, A.L.; Marsal, E.; Planell, J.A.; Lacroix, D. Finite element study of scaffold architecture design and culture conditions for tissue engineering. Biomaterials 2009, 30, 6142–6149. [Google Scholar] [CrossRef]
- Al-Ketan, O.; Rowshan, R.; Abu Al-Rub, R.K. Topology-mechanical property relationship of 3D printed strut, skeletal, and sheet based periodic metallic cellular materials. Addit. Manuf. 2018, 19, 167–183. [Google Scholar] [CrossRef]
- Feng, J.; Fu, J.; Yao, X.; He, Y. Triply periodic minimal surface (TPMS) porous structures: From multi-scale design, precise additive manufacturing to multidisciplinary applications. Int. J. Extrem. Manuf. 2022, 4, 022001. [Google Scholar] [CrossRef]
- Wang, S.; Shi, Z.; Liu, L.; Zhou, X.; Zhu, L.; Hao, Y. The Design of Ti6Al4V Primitive Surface Structure with Symmetrical Gradient of Pore Size in Biomimetic Bone Scaffold. Mater. Des. 2020, 193, 108830. [Google Scholar] [CrossRef]
- Zhu, J.; Zou, S.; Mu, Y.; Wang, J.; Jin, Y. Additively manufactured scaffolds with optimized thickness based on triply periodic minimal surface. Materials 2022, 15, 7084. [Google Scholar] [CrossRef]
- Peloquin, J.; Han, Y.; Gall, K. Printability and mechanical behavior as a function of base material, structure, and a wide range of porosities for polymer lattice structures fabricated by vat-based 3D printing. Addit. Manuf. 2023, 78, 103892. [Google Scholar] [CrossRef]
- Kirillova, A.; Kelly, C.; Liu, S.; Francovich, J.; Gall, K. High-strength composites based on 3D printed porous scaffolds infused with a bioresorbable mineral–organic bone adhesive. Adv. Eng. Mater. 2022, 24, 2101367. [Google Scholar] [CrossRef]
- Ramírez, E.A.; Béraud, N.; Pourroy, F.; Villeneuve, F.; Museau, M. Design parameters effects on relative density of triply periodic minimal surfaces for additive manufacturing. Procedia CIRP 2021, 100, 13–18. [Google Scholar] [CrossRef]
- Al-Ketan, O.; Abu Al-Rub, R.K. MSLattice: A free software for generating uniform and graded lattices based on triply periodic minimal surfaces. Mater. Des. Process. Commun. 2021, 3, e205. [Google Scholar] [CrossRef]
- Baino, F.; Magnaterra, G.; Fiume, E.; Schiavi, A.; Tofan, L.P.; Schwentenwein, M.; Verné, E. Digital light processing stereolithography of hydroxyapatite scaffolds with bone-like architecture, permeability, and mechanical properties. J. Am. Ceram. Soc. 2022, 105, 1648–1657. [Google Scholar] [CrossRef]
- D’Andrea, L.; Gastaldi, D.; Baino, F.; Verné, E.; Saccomano, G.; D’Amico, L.; Longo, E.; Schwentenwein, M.; Vena, P. Mechanical characterization of miniaturized 3D-printed hydroxyapatite parts obtained through vat photopolymerization: An experimental study. J. Mech. Behav. Biomed. Mater. 2023, 141, 105760. [Google Scholar] [CrossRef] [PubMed]
- Formlabs. Buy Dental LT Clear Resin. Available online: https://dental.formlabs.com/store/materials/dental-lt-clear-resin-v2/ (accessed on 18 January 2024).
- Formlabs. La Guida Definitiva Alla Stampa 3D Stereolitografica (SLA). Available online: https://formlabs.com/it/blog/guida-definitiva-stampa-3d-stereolitografia-sla/ (accessed on 18 January 2024).
- Thurzo, A.; Šufliarsky, B.; Urbanová, W.; Čverha, M.; Strunga, M.; Varga, I. Pierre Robin sequence and 3D printed personalized composite appliances in interdisciplinary approach. Polymers 2022, 14, 3858. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Malysa, A.; Mikulewicz, M. Comparison of the compression and tensile modulus of two chosen resins used in dentistry for 3D printing. Materials 2022, 15, 8956. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Juloski, J.; D’Amico, C.; Balestra, D.; Volpe, A.; Juloski, J.; Vichi, A. Clinically relevant properties of 3D printable materials for intraoral use in orthodontics: A critical review of the literature. Materials 2023, 16, 2166. [Google Scholar] [CrossRef]
- Formlabs. Formlabs Dental LT Clear Safety Data Sheet. Available online: https://formlabs.com/3d-printers/form-3/tech-specs/#data-sheets (accessed on 18 January 2024).
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofacial. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef]
- Milovanović, A.; Sedmak, A.; Golubović, Z.; Mihajlović, K.Z.; Žurkić, A.; Trajković, I.; Milošević, M. The effect of time on mechanical properties of biocompatible photopolymer resins used for fabrication of clear dental aligners. J. Mech. Behav. Biomed. Mater. 2021, 119, 104494. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Wieckiewicz, M.; Kozakiewicz, M.; Jurczyszyn, K. Mechanical properties, fractal dimension, and texture analysis of selected 3D-printed resins used in dentistry that underwent the compression test. Polymers 2023, 15, 1772. [Google Scholar] [CrossRef] [PubMed]
- Mohnish Kumar, S. Cytotoxicity of 3D Printed Materials: An In Vitro Study. Master’s Thesis, Sri Ramakrishna Dental College and Hospital, Coimbatore, India, 2019. [Google Scholar]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D printing of clear orthodontic aligners: Current state and future possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef] [PubMed]
- Karageorgiou, V.; Kaplan, D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 2005, 26, 5474–5491. [Google Scholar] [CrossRef] [PubMed]
- ISO 604:2002; Plastics—Determination of Compressive Properties. International Organization for Standarization: Geneva, Switzerland, 2002. Available online: https://www.iso.org/standard/31261.html (accessed on 20 December 2023).
- Zhang, S.; Vijayavenkataraman, S.; Lu, W.F.; Fuh, J.Y.H. A review on the use of computational methods to characterize, design, and optimize tissue engineering scaffolds, with a potential in 3D printing fabrication. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107, 1329–1351. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, T.; Laib, A.; Muller, R.; Dequeker, J.; Ruegsegger, P. Direct three-dimensional morphometric analysis of human cancellous bone: Microstructural data from spine, femur, iliac crest, and calcaneus. J. Bone Min. Res. 1999, 14, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Gibson, L.J.; Ashby, M.F. The mechanics of three-dimensional cellular materials. Proc. R. Soc. Lond. A 1982, 382, 43–59. [Google Scholar]
- Pabst, W.; Gregorova, E.; Ticha, G. Elasticity of porous ceramics—A critical study of modulus-porosity relations. J. Eur. Ceram. Soc. 2006, 26, 1085–1097. [Google Scholar] [CrossRef]
- Warren, W.E.; Kraynik, A.M. The linear elastic properties of open cell foams. J. Appl. Mech. 1988, 55, 341–346. [Google Scholar] [CrossRef]
- Zhu, H.X.; Knott, J.F.; Mills, N.J. Analysis of the elastic properties of open-cell foams with tetrakaidecahedral cells. Mech. Phys. Solids 1997, 45, 319–343. [Google Scholar] [CrossRef]
- Gibson, L.J.; Ashby, M.F. Cellular Solids: Structure and Properties; Cambridge University Press: Cambridge, UK, 1999. [Google Scholar]
- Huber, N.; Viswanath, R.N.; Mameka, N.; Markmann, J.; Weißmüller, J. Scaling laws of nanoporous metals under uniaxial compression. Acta Mater. 2014, 67, 252–265. [Google Scholar] [CrossRef]
- Maconachie, T.; Tino, R.; Lozanovski, B.; Watson, M.; Jones, A.; Pandelidi, C.; Alghamdi, A.; Almalki, A.; Downing, D.; Brandt, M.; et al. The compressive behaviour of ABS gyroid lattice structures manufactured by fused deposition modelling. Int. J. Adv. Manuf. Technol. 2020, 107, 4449–4467. [Google Scholar] [CrossRef]

| Unit Cell Length (mm) | Constant Thickness (mm) | Theoretical Volume (mm3) |
|---|---|---|
| 3 | 0.1 | 12 × 12 × 12 |
| 3 | 0.2 | 12 × 12 × 12 |
| 3 | 0.3 | 12 × 12 × 12 |
| 3 | 0.4 | 12 × 12 × 12 |
| 3 | 0.5 | 12 × 12 × 12 |
| 4 | 0.1 | 12 × 12 × 12 |
| 4 | 0.2 | 12 × 12 × 12 |
| 4 | 0.3 | 12 × 12 × 12 |
| 4 | 0.4 | 12 × 12 × 12 |
| 4 | 0.5 | 12 × 12 × 12 |
| Thickness (mm) | Density (kg/m3) | Relative Density (%) | Porosity (vol.%) | |
|---|---|---|---|---|
| Gyroid | 0.1 | 195.1 | 16.7 | 83.3 |
| 0.2 | 268.2 | 22.9 | 77.0 | |
| 0.3 | 379.1 | 32.4 | 67.6 | |
| 0.4 | 539.9 | 46.2 | 53.8 | |
| 0.5 | 574.5 | 49.2 | 50.9 | |
| Schwarz P | 0.1 | 150.9 | 12.9 | 87.0 |
| 0.2 | 168.9 | 14.5 | 85.6 | |
| 0.3 | 271.9 | 23.3 | 76.7 | |
| 0.4 | 369.8 | 31.6 | 68.4 | |
| 0.5 | 476.3 | 40.7 | 59.3 |
| Thickness (mm) | Density (kg/m3) | Relative Density (%) | Porosity (vol.%) | |
|---|---|---|---|---|
| Gyroid | 0.1 | 354.5 | 30.3 | 69.7 |
| 0.2 | 404.3 | 34.6 | 65.4 | |
| 0.3 | 605.4 | 51.8 | 48.2 | |
| 0.4 | 706.4 | 60.4 | 39.6 | |
| 0.5 | 690.6 | 59.1 | 40.9 | |
| Schwarz P | 0.1 | 192.4 | 16.5 | 83.5 |
| 0.2 | 291.9 | 24.9 | 75.0 | |
| 0.3 | 441.5 | 37.8 | 62.2 | |
| 0.4 | 589.6 | 50.4 | 49.6 | |
| 0.5 | 631.7 | 54.1 | 45.9 |
| Thickness (mm) | Young’s Modulus (MPa) | Compressive Strength (MPa) | |
|---|---|---|---|
| Gyroid | 0.1 | 29.7 ± 7.8 | 1.7 ± 0.6 |
| 0.2 | 39.9 ± 9.0 | 3.1 ± 1.1 | |
| 0.3 | 80.4 ± 11.4 | 5.6 ± 1.5 | |
| 0.4 | 145.3 ± 25.0 | 13.8 ± 2.5 | |
| 0.5 | 156 ± 10.3 | 17.7 ± 1.8 | |
| Schwarz P | 0.1 | 10.1 ± 1.5 | 0.5 ± 0.1 |
| 0.2 | 19.1 ± 9.2 | 1.1 ± 0.3 | |
| 0.3 | 56.3 ± 11.9 | 3.6 ± 0.1 | |
| 0.4 | 129.3 ± 33.5 | 7.9 ± 1.0 | |
| 0.5 | 231 ± 41.9 | 11.9 ± 1.5 |
| Thickness (mm) | Young’s Modulus (MPa) | Compressive Strength (MPa) | |
|---|---|---|---|
| Gyroid | 0.1 | 77.5 ± 25.7 | 3.3 ± 0.3 |
| 0.2 | 92.7 ± 27.5 | 5.3 ± 1.2 | |
| 0.3 | 171.0 ± 4.1 | 14.9 ± 0.1 | |
| 0.4 | 219.2 ± 32.1 | 22.9 ± 4.3 | |
| 0.5 | 213.1 ± 21.1 | 20.1 ± 2.0 | |
| Schwarz P | 0.1 | 17.2 ± 3.4 | 0.8 ± 0.1 |
| 0.2 | 52.7 ± 23.3 | 2.9 ± 0.9 | |
| 0.3 | 150.7 ± 48.9 | 6.9 ± 2.0 | |
| 0.4 | 321.7 ± 25.0 | 15.5 ± 2.8 | |
| 0.5 | 317.9 ± 48.9 | 19.9 ± 1.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gabrieli, R.; Wenger, R.; Mazza, M.; Verné, E.; Baino, F. Design, Stereolithographic 3D Printing, and Characterization of TPMS Scaffolds. Materials 2024, 17, 654. https://doi.org/10.3390/ma17030654
Gabrieli R, Wenger R, Mazza M, Verné E, Baino F. Design, Stereolithographic 3D Printing, and Characterization of TPMS Scaffolds. Materials. 2024; 17(3):654. https://doi.org/10.3390/ma17030654
Chicago/Turabian StyleGabrieli, Roberta, Raphael Wenger, Marco Mazza, Enrica Verné, and Francesco Baino. 2024. "Design, Stereolithographic 3D Printing, and Characterization of TPMS Scaffolds" Materials 17, no. 3: 654. https://doi.org/10.3390/ma17030654
APA StyleGabrieli, R., Wenger, R., Mazza, M., Verné, E., & Baino, F. (2024). Design, Stereolithographic 3D Printing, and Characterization of TPMS Scaffolds. Materials, 17(3), 654. https://doi.org/10.3390/ma17030654







