Accuracy of Dental Models Fabricated Using Recycled Poly-Lactic Acid
Abstract
1. Introduction
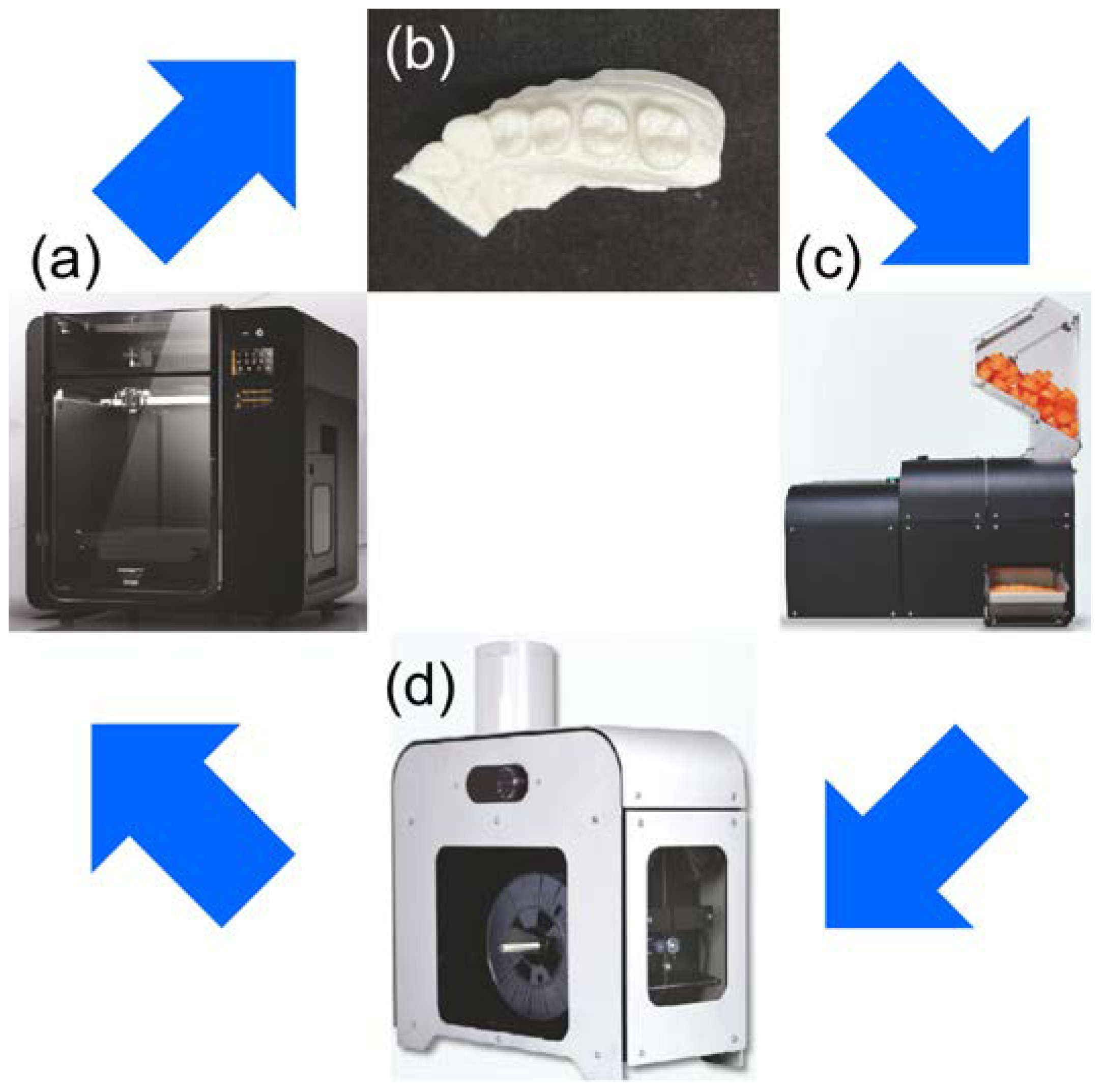
2. Materials and Methods
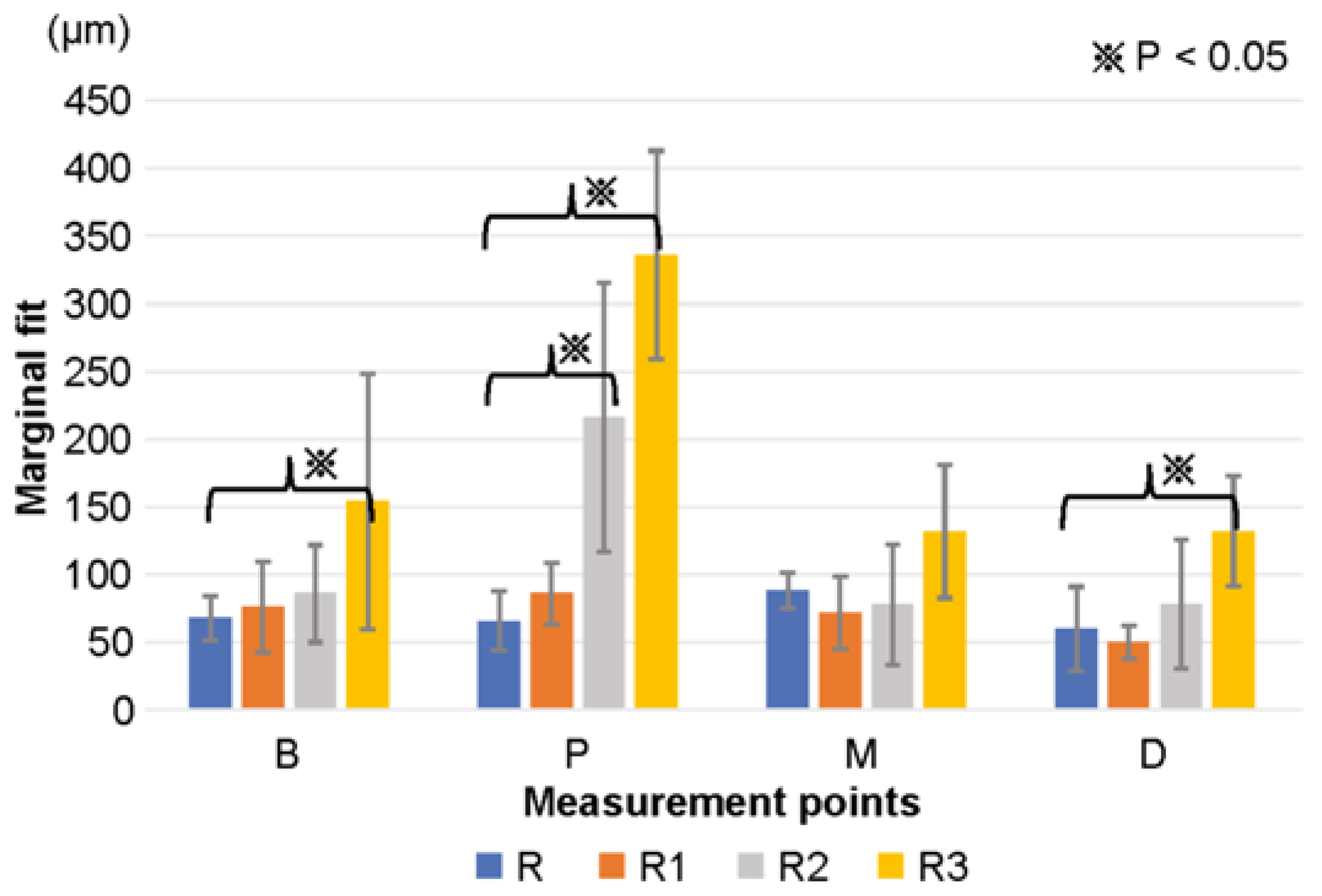
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hansson, O.; Eklund, J. A historical review of hydrocolloids and an investigation of the dimensional accuracy of the new alginates for crown and bridge impressions when using stock trays. Swed. Dent. J. 1984, 8, 81–95. [Google Scholar] [PubMed]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Laino, L.; Troiano, G.; Amoroso, G.; Crimi, S.; Matarese, M.; D’Amico, C.; Nastro Siniscalchi, E.; et al. Alginate materials and dental impression technique: A current state of the art and application to dental practice. Mar. Drugs 2018, 17, 18. [Google Scholar] [CrossRef] [PubMed]
- Papadiochos, I.; Papadiochou, S.; Emmanouil, I. The historical evolution of dental impression materials. J. Hist. Dent. 2017, 65, 79–89. [Google Scholar]
- Johnson, G.H.; Craig, R.G. Accuracy and bond strength of combination agar/alginate hydrocolloid impression materials. J. Prosthet. Dent. 1986, 55, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Naumovski, B.; Kapushevska, B. Dimensional stability and accuracy of silicone—Based impression materials using different impression techniques—A literature review. Prilozi 2017, 38, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Basapogu, S.; Pilla, A.; Pathipaka, S. Dimensional accuracy of hydrophilic and hydrophobic VPS impression materials using different impression techniques—An invitro study. J. Clin. Diagn. Res. 2016, 10, ZC56–ZC59. [Google Scholar] [CrossRef]
- Rajendran, R.; Chander, N.G.; Anitha, K.V.; Muthukumar, B. Dimensional accuracy of vinyl polyether and polyvinyl siloxane impression materials in direct implant impression technique for multiple dental implants. Eur. Oral Res. 2021, 55, 54–59. [Google Scholar] [CrossRef]
- Hulme, C.; Yu, G.; Browne, C.; O’Dwyer, J.; Craddock, H.; Brown, S.; Gray, J.; Pavitt, S.; Fernandez, C.; Godfrey, M.; et al. Cost-effectiveness of silicone and alginate impressions for complete dentures. J. Dent. 2014, 42, 902–907. [Google Scholar] [CrossRef]
- Chen, J.D.; Ma, A.B.; Sun, L.; Hong, G. The physical properties of new paste type alginate impression materials. In Proceedings of the 2021 IADR/AADR/CADR General Session (Virtual Experience), Virtual, 21–24 July 2021. Final Presentation ID: 0552. [Google Scholar]
- Buckingum, T.L. The force of expansion of plaster of Paris. Dent. Cosmos 1959, 1, 238–240. [Google Scholar]
- Mori, T.; Mcaloon, J.; Aghajani, F. Gypsum-bonded investment and dental precision casting (I) two investments. Dent. Mater. J. 2003, 22, 412–420. [Google Scholar] [CrossRef]
- Urstein, M.; Fitzig, S.; Moskona, D.; Cardash, H.S. A clinical evaluation of materials used in registering interjaw relationships. J. Prosthet. Dent. 1991, 65, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, J.A. The use of gold in dentistry: An historical overview. J. Hist. Dent. 2012, 60, 134–147. [Google Scholar]
- Vojdani, M.; Torabi, K.; Farjood, E.; Khaledi, A. Comparison the marginal and internal fit of metal copings cast from wax patterns fabricated by CAD/CAM and conventional wax up techniques. J. Dent. 2013, 14, 118–129. [Google Scholar]
- Yang, J.; Li, H. Accuracy of CAD-CAM milling versus conventional lost-wax casting for single metal copings: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, S0022-3913, 00344-4. [Google Scholar] [CrossRef] [PubMed]
- Reitemeier, B.; Hänsel, K.; Range, U.; Walter, M.H. Prospective study on metal ceramic crowns in private practice settings: 20-year results. Clin. Oral Investig. 2019, 23, 1823–1828. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Caradonna, G.; Biancardino, M.; De Lillo, A.; Troiano, G.; Guida, L. Digital versus conventional workflow for the fabrication of multiunit fixed prostheses: A systematic review and meta-analysis of vertical marginal fit in controlled in vitro studies. J. Prosthet. Dent. 2019, 122, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Kihara, H.; Hatakeyama, W.; Komine, F.; Takafuji, K.; Takahashi, T.; Yokota, J.; Oriso, K.; Kondo, H. Accuracy and practicality of intraoral scanner in dentistry: A literature review. J. Prosthodont. Res. 2020, 64, 109–113. [Google Scholar] [CrossRef]
- Chochlidakis, K.M.; Papaspyridakos, P.; Geminiani, A.; Chen, C.J.; Feng, I.J.; Ercoli, C. Digital versus conventional impressions for fixed prosthodontics: A systematic review and meta-analysis. J. Prosthet. Dent. 2016, 116, 184–190.e12. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Graiff, L.; Savio, G.; Vigolo, P.; Monaco, C.; Stellini, E. Full arch digital scanning systems performances for implant-supported fixed dental prostheses: A comparative study of 8 intraoral scanners. J. Prosthodont. Res. 2019, 63, 396–403. [Google Scholar] [CrossRef]
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 transmission in dental practice: Brief review of preventive measures in Italy. J. Dent. Res. 2020, 99, 1030–1038. [Google Scholar] [CrossRef]
- Papi, P.; Di Murro, B.; Penna, D.; Pompa, G. Digital prosthetic workflow during COVID-19 pandemic to limit infection risk in dental practice. Oral Dis. 2021, 27 (Suppl. S3), 723–726. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Lenherr, P.; Dedem, P.; Kovaltschuk, I.; Bragger, U.; Zitzmann, N.U. Time efficiency, difficulty, and operator’s preference comparing digital and conventional implant impressions: A randomized controlled trial. Clin. Oral Implant. Res. 2017, 28, 1318–1323. [Google Scholar] [CrossRef] [PubMed]
- Davidowitz, G.; Kotick, P.G. The use of CAD/CAM in dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM ceramic restorative materials for natural teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef] [PubMed]
- Albuha Al-Mussawi, R.M.; Farid, F. Computer-based technologies in dentistry: Types and applications. J. Dent. 2016, 13, 215–222. [Google Scholar]
- Ariwa, M.; Itamiya, T.; Koizumi, S.; Yamaguchi, T. Comparison of the observation errors of augmented and spatial reality systems. Appl. Sci. 2021, 11, 12076. [Google Scholar] [CrossRef]
- Wayman, C.; Niemann, H. The fate of plastic in the ocean environment—A minireview. Environ. Sci. Process. Impacts 2021, 23, 198–212. [Google Scholar] [CrossRef]
- Seo, Y.; Kudo, F. Charging plastic bags: Perceptions from Japan. PLoS Sustain. Transform. 2022, 1, e0000011. [Google Scholar] [CrossRef]
- Jonsson, A.; Andersson, K.; Stelick, A.; Dando, R. An evaluation of alternative biodegradable and reusable drinking straws as alternatives to single-use plastic. J. Food Sci. 2021, 86, 3219–3227. [Google Scholar] [CrossRef]
- Blanco, I. Lifetime prediction of food and beverage packaging wastes. J. Therm. Anal. Calorim. 2016, 125, 809–816. [Google Scholar] [CrossRef]
- Ishida, Y.; Miura, D.; Miyasaka, T.; Shinya, A. Dimensional accuracy of dental casting patterns fabricated using consumer 3D printers. Polymers 2020, 12, 2244. [Google Scholar] [CrossRef] [PubMed]
- Arrigo, R.; Frache, A. FDM printability of PLA based-materials: The key role of the rheological behavior. Polymers 2022, 14, 1754. [Google Scholar] [CrossRef] [PubMed]
- Nagata, K.; Muromachi, K.; Kouzai, Y.; Inaba, K.; Inoue, E.; Fuchigami, K.; Nihei, T.; Atsumi, M.; Kimoto, K.; Kawana, H. Fit accuracy of resin crown on a dental model fabricated using fused deposition modeling 3D printing and a polylactic acid filament. J. Prosthodont. Res. 2023, 67, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Singhvi, M.S.; Zinjarde, S.S.; Gokhale, D.V. Polylactic acid: Synthesis and biomedical applications. J. Appl. Microbiol. 2019, 127, 1612–1626. [Google Scholar] [CrossRef] [PubMed]
- Mikula, K.; Skrzypczak, D.; Izydorczyk, G.; Warchoł, J.; Moustakas, K.; Chojnacka, K.; Witek-Krowiak, A. 3D printing filament as a second life of waste plastics-a review. Environ. Sci. Pollut. Res. Int. 2021, 28, 12321–12333. [Google Scholar] [CrossRef] [PubMed]
- Shembesh, M.; Ali, A.; Finkelman, M.; Weber, H.P.; Zandparsa, R. An in vitro comparison of the marginal adaptation accuracy of CAD/CAM restorations using different impression systems. J. Prosthodont. 2017, 26, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.E.; Kim, Y.L.; Kong, H.J.; Chang, H.S.; Jung, J.H. Marginal and internal fit of 3D printed provisional crowns according to build directions. J. Adv. Prosthodont. 2020, 12, 225–232. [Google Scholar] [CrossRef]
- Dolev, E.; Bitterman, Y.; Meirowitz, A. Comparison of marginal fit between CAD-CAM and hot-press lithium disilicate crowns. J. Prosthet. Dent. 2019, 121, 124–128. [Google Scholar] [CrossRef]
- Teng, P.S.P.; Leong, K.F.; Kong, P.W.; Er, B.H.; Chew, Z.Y.; Tan, P.S.; Tee, C.H. A methodology to design and fabricate a smart brace using low-cost additive manufacturing. Virtual Phys. Prototyp. 2022, 17, 932–947. [Google Scholar] [CrossRef]
- Wickramasinghe, S.; Do, T.; Tran, P. Flexural behavior of 3D printed bio-inspired interlocking suture structures. Mater. Sci. Addit. Manuf. 2022, 1, 9. [Google Scholar] [CrossRef]
- Alsoufi, M.S.; Elsayed, A.E. Surface roughness quality and dimensional accuracy—A comprehensive analysis of 100% infill printed parts fabricated by a personal/desktop cost-effective FDM 3D printer. Mater. Sci. Appl. 2018, 9, 11–40. [Google Scholar] [CrossRef]
- Cicala, G.; Giordano, D.; Tosto, C.; Filippone, G.; Recca, A.; Blanco, I. Polylactide (PLA) filaments a biobased solution for additive manufacturing: Correlating rheology and thermomechanical properties with printing quality. Materials 2018, 11, 1191. [Google Scholar] [CrossRef] [PubMed]
- Palsikowski, P.A.; Kuchnier, C.N.; Pinheiro, I.F.; Morales, A.R. Biodegradation in soil of PLA/PBAT blends compatibilized with chain extender. J. Polym. Environ. 2018, 26, 330–341. [Google Scholar] [CrossRef]
- Beltrán, F.R.; Arrieta, M.P.; Moreno, E.; Gaspar, G.; Muneta, L.M.; Carrasco-Gallego, R.; Yáñez, S.; Hidalgo-Carvajal, D.; de la Orden, M.U.; Martínez Urreaga, J. Evaluation of the technical viability of distributed mechanical recycling of PLA 3D printing wastes. Polymers 2021, 13, 1247. [Google Scholar] [CrossRef]
- Agüero, A.; Morcillo, M.D.C.; Quiles-Carrillo, L.; Balart, R.; Boronat, T.; Lascano, D.; Torres-Giner, S.; Fenollar, O. Study of the influence of the reprocessing cycles on the final properties of polylactide pieces obtained by injection molding. Polymers 2019, 11, 1908. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Rao, C.; Gu, F.; Sharmin, N.; Fu, J. Close-looped recycling of polylactic acid used in 3D printing: An experimental investigation and life cycle assessment. J. Clean. Prod. 2018, 197, 1046–1055. [Google Scholar] [CrossRef]
- Anderson, I. Mechanical properties of specimens 3D printed with virgin and recycled polylactic acid. 3D Print Addit Manuf. 2017, 4, 110–115. [Google Scholar] [CrossRef]
- Beltrán, F.R.; Infante, C.; de la Orden, M.U.; Martínez Urreaga, J.M. Mechanical recycling of poly(lactic acid): Evaluation of a chain extender and a peroxide as additives for upgrading the recycled plastic. J. Clean. Prod. 2019, 219, 46–56. [Google Scholar] [CrossRef]
- Patwa, R.; Kumar, A.; Katiyar, V. Effect of silk nano-disc dispersion on mechanical, thermal, and barrier properties of poly(lactic acid) based bionanocomposites. J. Appl. Polym. Sci. 2018, 135, 46671. [Google Scholar] [CrossRef]
- Cisneros-López, E.O.; Pal, A.K.; Rodriguez, A.U.; Wu, F.; Misra, M.; Mielewski, D.F.; Kiziltas, A.; Mohanty, A.K. Recycled poly(lactic acid)–based 3D printed sustainable biocomposites: A comparative study with injection molding. Mater. Today Sustain. 2020, 7–8, 100027. [Google Scholar] [CrossRef]
- Coppola, B.; Cappetti, N.; Di Maio, L.; Scarfato, P.; Incarnato, L. 3D printing of PLA/clay nanocomposites: Influence of printing temperature on printed samples properties. Materials 2018, 11, 1947. [Google Scholar] [CrossRef] [PubMed]
- Bardot, M.; Schulz, M.D. Biodegradable poly(lactic acid) nanocomposites for fused deposition modeling 3D printing. Nanomaterials 2020, 10, 2567. [Google Scholar] [CrossRef] [PubMed]
- Gomes, T.E.; Cadete, M.S.; Dias-de-Oliveira, J.; Neto, V. Controlling the properties of parts 3D printed from recycled thermoplastics: A review of current practices. Polym. Degrad. Stab. 2022, 196, 109850. [Google Scholar] [CrossRef]
- Lagazzo, A.; Moliner, C.; Bosio, B.; Botter, R.; Arato, E. Evaluation of the mechanical and thermal properties decay of PHBV/sisal and PLA/sisal biocomposites at different recycle steps. Polymers 2019, 11, 1477. [Google Scholar] [CrossRef]
- Gai, M.; Li, W.; Frueh, J.; Sukhorukov, G.B. Polylactic acid sealed polyelectrolyte complex microcontainers for controlled encapsulation and NIR-laser based release of cargo. Colloids Surf. B Biointerfaces 2019, 173, 521–528. [Google Scholar] [CrossRef]
- Li, Z.; Wu, T.; Chen, Y.; Gao, X.; Ye, J.; Jin, Y.; Chen, B. Oriented homo-epitaxial crystallization of polylactic acid displaying a biomimetic structure and improved blood compatibility. J. Biomed. Mater. Res. A 2022, 110, 684–695. [Google Scholar] [CrossRef]
- Ahuja, R.; Kumari, N.; Srivastava, A.; Bhati, P.; Vashisth, P.; Yadav, P.K.; Jacob, T.; Narang, R.; Bhatnagar, N. Biocompatibility analysis of PLA based candidate materials for cardiovascular stents in a rat subcutaneous implant model. Acta Histochem. 2020, 122, 151615. [Google Scholar] [CrossRef]
- Benli, M.; Eker-Gümüş, B.; Kahraman, Y.; Huck, O.; Özcan, M. Can polylactic acid be a CAD/CAM material for provisional crown restorations in terms of fit and fracture strength? Dent. Mater. J. 2021, 40, 772–780. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Canals, S.; Gómez-Polo, M.; Solá-Ruiz, M.F.; Del Río Highsmith, J.; Viñuela, A.C. Polylactic acid as a material for three-dimensional printing of provisional restorations. Int. J. Prosthodont. 2018, 31, 349–350. [Google Scholar] [CrossRef]
- Crenn, M.J.; Rohman, G.; Fromentin, O.; Benoit, A. Polylactic acid as a biocompatible polymer for three-dimensional printing of interim prosthesis: Mechanical characterization. Dent. Mater. J. 2022, 41, 110–116. [Google Scholar] [CrossRef]
- Plavec, R.; Horváth, V.; Hlaváčiková, S.; Omaníková, L.; Repiská, M.; Medlenová, E.; Feranc, J.; Kruželák, J.; Přikryl, R.; Figalla, S.; et al. Influence of multiple thermomechanical processing of 3D filaments based on polylactic acid and polyhydroxybutyrate on their rheological and utility properties. Polymers 2022, 14, 1947. [Google Scholar] [CrossRef] [PubMed]
- Menčík, P.; Přikryl, R.; Stehnová, I.; Melčová, V.; Kontárová, S.; Figalla, S.; Alexy, P.; Bočkaj, J. Effect of selected commercial plasticizers on mechanical, thermal, and morphological properties of poly(3-hydroxybutyrate)/poly(lactic acid)/plasticizer biodegradable blends for three-dimensional (3D) print. Materials 2018, 11, 1893. [Google Scholar] [CrossRef] [PubMed]
- Greco, A.; Ferrari, F. Thermal behavior of PLA plasticized by commercial and cardanol-derived plasticizers and the effect on the mechanical properties. J. Therm. Anal. Calorim. 2021, 146, 131–141. [Google Scholar] [CrossRef]
- Li, Y.; Mi, J.; Fu, H.; Zhou, H.; Wang, X. Nanocellular foaming behaviors of chain-extended poly(lactic acid) induced by isothermal crystallization. ACS Omega 2019, 4, 12512–12523. [Google Scholar] [CrossRef]
- Yang, Y.; Xiong, Z.; Zhang, L.; Tang, Z.; Zhang, R.; Zhu, J. Isosorbide dioctoate as a “green” plasticizer for poly(lactic acid). Mater. Des. 2016, 91, 262–268. [Google Scholar] [CrossRef]
- Xu, P.; Tian, H.; Han, L.; Yang, H.; Bian, J.; Pan, H.; Zhang, H. Improved heat resistance in poly (lactic acid)/ethylene butyl methacrylate glycidyl methacrylate terpolymer blends by controlling highly filled talc particles. J. Ther. Anal. Calorim. 2022, 147, 5719–5732. [Google Scholar] [CrossRef]
- Barczewski, M.; Mysiukiewicz, O.; Hejna, A.; Biskup, R.; Szulc, J.; Michałowski, S.; Piasecki, A.; Kloziński, A. The effect of surface treatment with isocyanate and aromatic carbodiimide of thermally expanded vermiculite used as a functional filler for polylactide-based composites. Polymers 2021, 13, 890. [Google Scholar] [CrossRef]
- Andrzejewski, J.; Skórczewska, K.; Kloziński, A. Improving the toughness and thermal resistance of polyoxymethylene/poly(lactic acid) blends: Evaluation of structure-properties correlation for reactive processing. Polymers 2020, 12, 307. [Google Scholar] [CrossRef]
- Zhao, X.; Liu, J.; Li, J.; Liang, X.; Zhou, W.; Peng, S. Strategies and techniques for improving heat resistance and mechanical performances of poly(lactic acid) (PLA) biodegradable materials. Int. J. Biol. Macromol. 2022, 218, 115–134. [Google Scholar] [CrossRef]
- Chan, F.L.; Hon, C.Y.; Tarlo, S.M.; Rajaram, N.; House, R. Emissions and health risks from the use of 3D printers in an occupational setting. J. Toxicol. Environ. Health A 2020, 83, 279–287. [Google Scholar] [CrossRef]
- Dobrzyńska, E.; Kondej, D.; Kowalska, J.; Szewczyńska, M. State of the art in additive manufacturing and its possible chemical and particle hazards-review. Indoor Air 2021, 31, 1733–1758. [Google Scholar] [CrossRef] [PubMed]
- Ding, S.; Ng, B.F.; Shang, X.; Liu, H.; Lu, X.; Wan, M.P. The characteristics and formation mechanisms of emissions from thermal decomposition of 3D printer polymer filaments. Sci. Total Environ. 2019, 692, 984–994. [Google Scholar] [CrossRef] [PubMed]
- Wojtyła, S.; Klama, P.; Baran, T. Is 3D printing safe? Analysis of the thermal treatment of thermoplastics: ABS, PLA, PET, and nylon. J. Occup. Environ. Hyg. 2017, 14, D80–D85. [Google Scholar] [CrossRef] [PubMed]
- Suharjanto, G.; Adi, J.P. Design and manufacture of polylacticacid (PLA) filament storage for 3-dimensional printing with composite material. IOP Conf. Ser. Earth Environ. Sci. 2022, 998, 012028. [Google Scholar] [CrossRef]
- Liu, Y.; Sing, S.L.; Lim, R.X.E.; Yeong, W.Y.; Goh, B.T. Preliminary Investigation on the Geometric Accuracy of 3D Printed Dental Implant Using a Monkey Maxilla Incisor Model. Int. J. Bioprint. 2022, 8, 476. [Google Scholar] [CrossRef]

| Specifications | |
|---|---|
| PLA filament designed for Moment (Moment Co., Ltd., Seoul, Republic of Korea) | Material PLA: (>98%) Density: 1.25/cm Melting Point: 190 °C Recommended Print Temperature: 215–230 °C Thermal Distortion: 58 °C Water Absorption: 0.50% Molding shrinkage: 0.30 |
| Moment M350 (Moment Co., Ltd., Seoul, Republic of Korea) | XYZ accuracy: XY: 12 μm, Z: 0.625 μm Laminating pitch: 0.05–0.3 mm Modeling size: 350 mm × 190 mm × 196 mm Nozzle: 0.4 mm |
| B | P | M | D | |
|---|---|---|---|---|
| R | 68 ± 16 | 66 ± 22 | 88 ± 13 | 60 ± 31 |
| R1 | 76 ± 34 | 86 ± 23 | 72 ± 27 | 50 ± 12 |
| R2 | 86 ± 36 | 216 ± 99 | 78 ± 44 | 78 ± 48 |
| R3 | 154 ± 94 | 336 ± 77 | 132 ± 49 | 132 ± 41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagata, K.; Inaba, K.; Kimoto, K.; Kawana, H. Accuracy of Dental Models Fabricated Using Recycled Poly-Lactic Acid. Materials 2023, 16, 2620. https://doi.org/10.3390/ma16072620
Nagata K, Inaba K, Kimoto K, Kawana H. Accuracy of Dental Models Fabricated Using Recycled Poly-Lactic Acid. Materials. 2023; 16(7):2620. https://doi.org/10.3390/ma16072620
Chicago/Turabian StyleNagata, Koudai, Keitaro Inaba, Katsuhiko Kimoto, and Hiromasa Kawana. 2023. "Accuracy of Dental Models Fabricated Using Recycled Poly-Lactic Acid" Materials 16, no. 7: 2620. https://doi.org/10.3390/ma16072620
APA StyleNagata, K., Inaba, K., Kimoto, K., & Kawana, H. (2023). Accuracy of Dental Models Fabricated Using Recycled Poly-Lactic Acid. Materials, 16(7), 2620. https://doi.org/10.3390/ma16072620







