Influence of Multiple Used Implant Drills on Their Cutting Performance and Fracture Resistance
Abstract
:1. Introduction
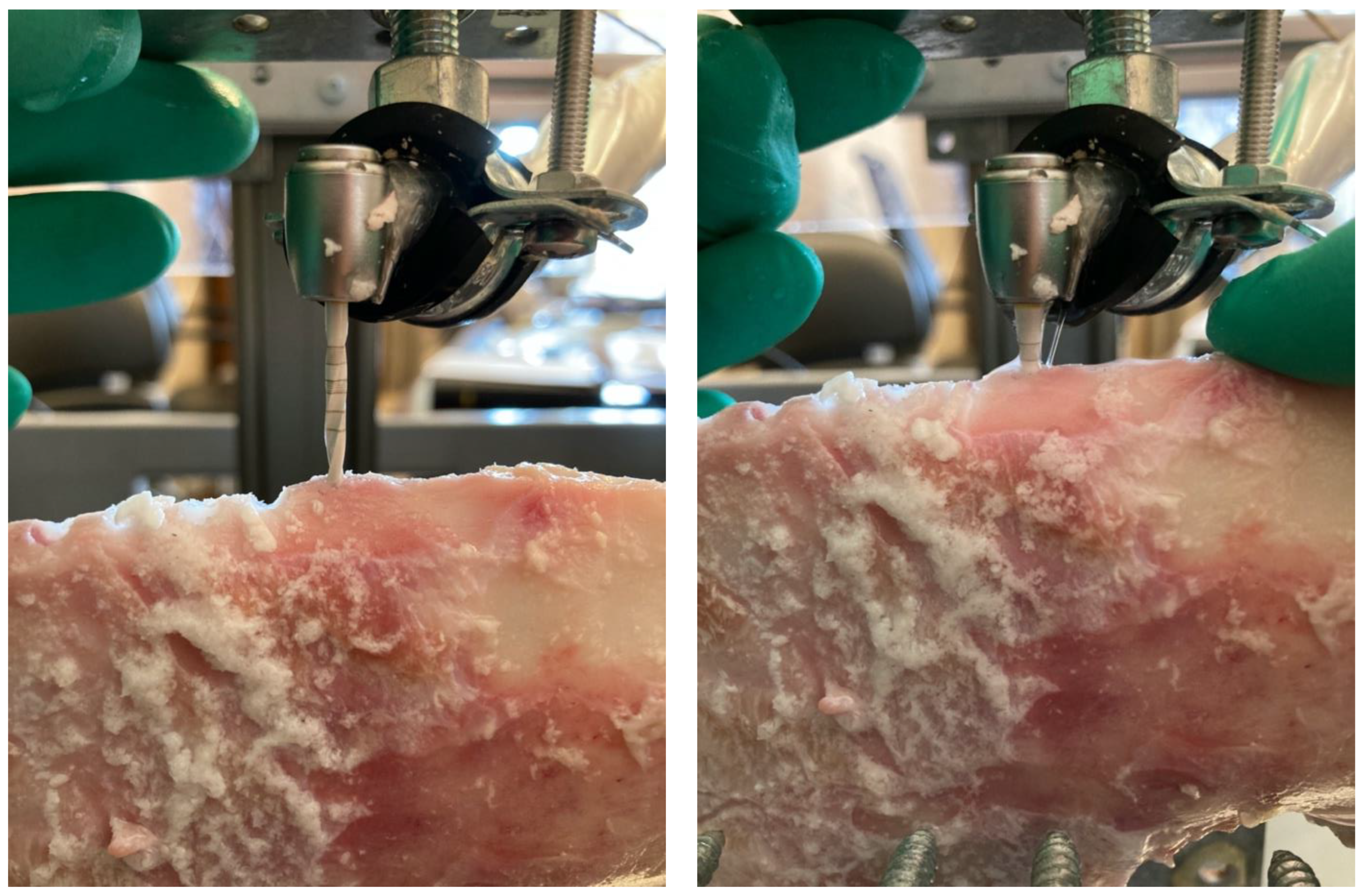
2. Materials and Methods
3. Results
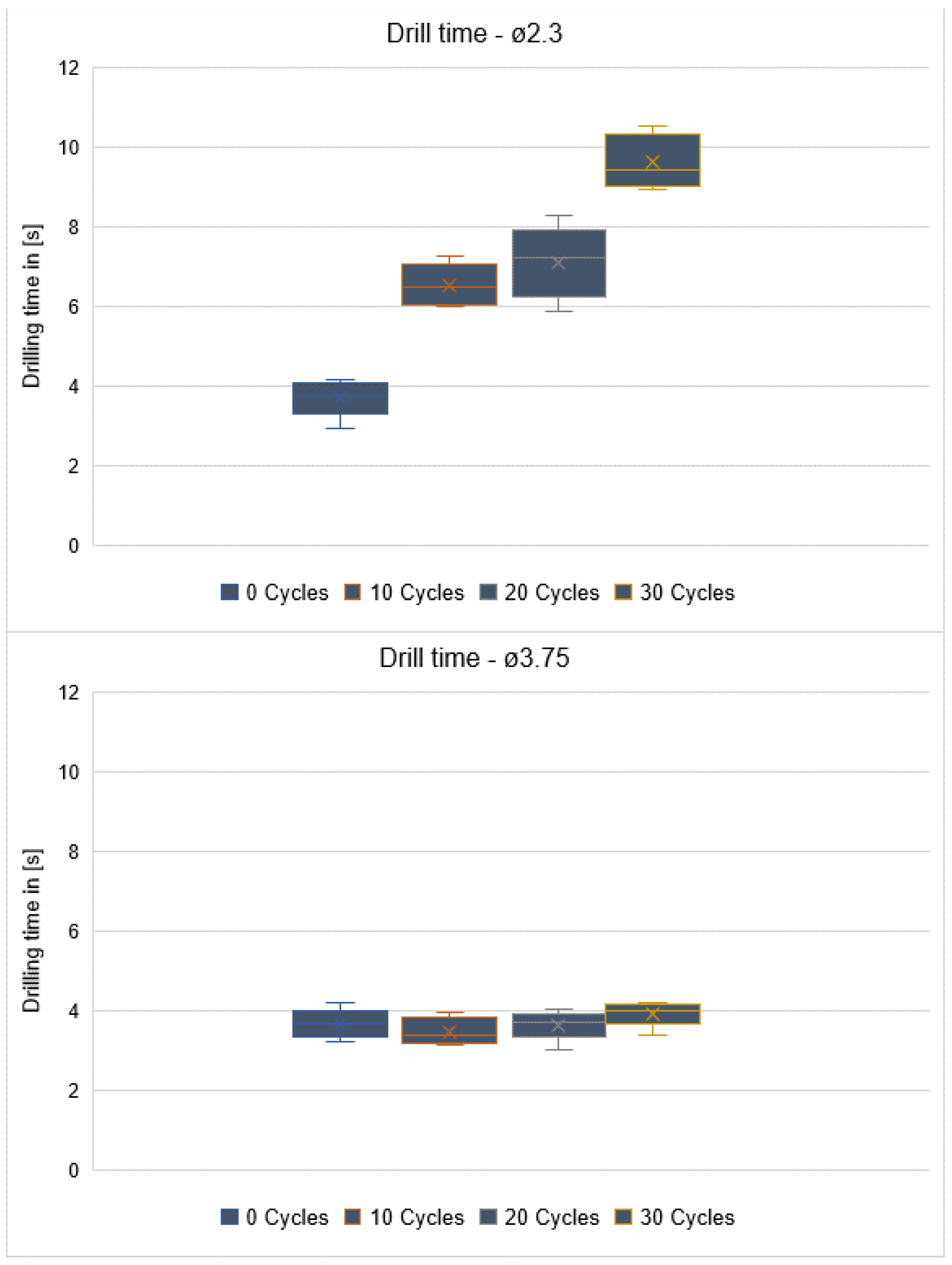
3.1. Drilling Time
3.1.1. Repetitive Usage
3.1.2. Diameter
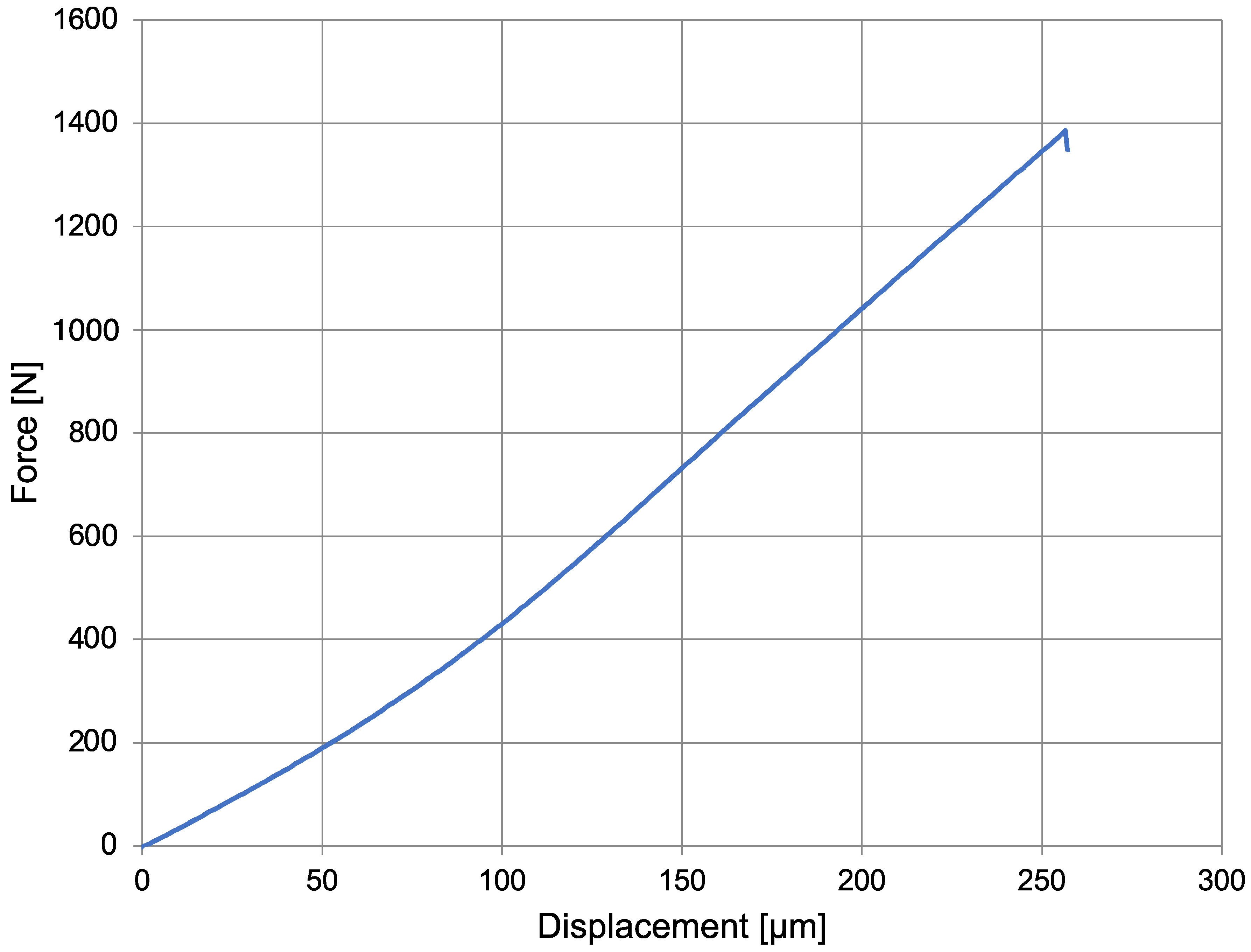
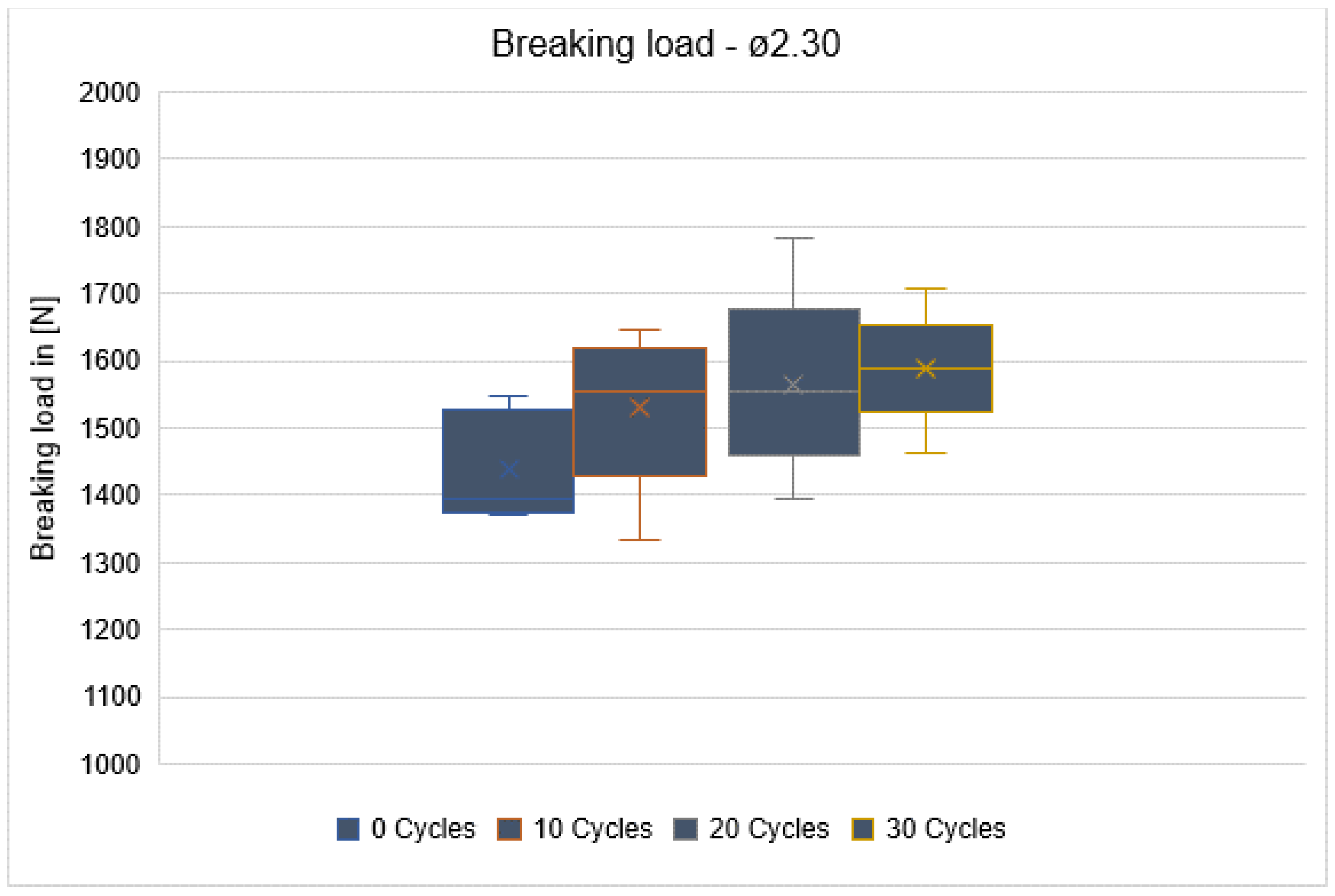
3.2. Flexural Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stacchi, C.; Troiano, G.; Montaruli, G.; Mozzati, M.; Lamazza, L.; Antonelli, A.; Giudice, A.; Lombardi, T. Changes in Implant Stability Using Different Site Preparation Techniques: Osseodensification Drills Versus Piezoelectric Surgery. A Multi-Center Prospective Randomized Controlled Clinical Trial. Clin. Implant Dent. Relat. Res. 2023, 25, 133–140. [Google Scholar] [PubMed]
- Guo, T.; Gulati, K.; Arora, H.; Han, P.; Fournier, B.; Ivanovski, S. Race to Invade: Understanding Soft Tissue Integration at the Transmucosal Region of Titanium Dental Implants. Dent. Mater. 2021, 37, 816–831. [Google Scholar]
- Lorusso, F.; Noumbissi, S.; Francesco, I.; Rapone, B.; Khater, A.G.A.; Scarano, A. Scientific Trends in Clinical Research on Zirconia Dental Implants: A Bibliometric Review. Materials 2020, 13, 5534. [Google Scholar]
- Giordano, R., II. Ceramics Overview. Br. Dent. J. 2022, 232, 658–663. [Google Scholar]
- Pieger, S.; Salman, A.; Bidra, A.S. Clinical Outcomes of Lithium Disilicate Single Crowns and Partial Fixed Dental Prostheses: A Systematic Review. J. Prosthet. Dent. 2014, 112, 22–30. [Google Scholar] [PubMed]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current Status on Lithium Disilicate and Zirconia: A Narrative Review. BMC Oral Health 2019, 19, 134. [Google Scholar]
- Schmitter, M.; Mussotter, K.; Rammelsberg, P.; Gabbert, O.; Ohlmann, B. Clinical Performance of Long-Span Zirconia Frameworks for Fixed Dental Prostheses: 5-Year Results. J. Oral Rehabil. 2012, 39, 552–557. [Google Scholar]
- Chiapasco, M.; Casentini, P.; Zaniboni, M.; Corsi, E.; Anello, T. Titanium-Zirconium Alloy Narrow-Diameter Implants (Straumann Roxolid(®)) for the Rehabilitation of Horizontally Deficient Edentulous Ridges: Prospective Study on 18 Consecutive Patients. Clin. Oral Implants Res. 2012, 23, 1136–1141. [Google Scholar]
- Roehling, S.; Schlegel, K.A.; Woelfler, H.; Gahlert, M. Performance and Outcome of Zirconia Dental Implants in Clinical Studies: A Meta-Analysis. Clin. Oral Implants Res. 2018, 29 (Suppl. S16), 135–153. [Google Scholar]
- Cahill, D.G.; Olson, J.R.; Fischer, H.E.; Watson, S.K.; Stephens, R.B.; Tait, R.H.; Ashworth, T.; Pohl, R.O. Thermal Conductivity and Specific Heat of Glass Ceramics. Phys. Rev. B Condens. Matter 1991, 44, 12226–12232. [Google Scholar]
- Wu, J.; Yu, P.; Lv, H.; Yang, S.; Wu, Z. Nanostructured Zirconia Surfaces Regulate Human Gingival Fibroblasts Behavior through Differential Modulation of Macrophage Polarization. Front. Bioeng. Biotechnol. 2020, 8, 611684. [Google Scholar] [PubMed]
- Eriksson, A.R.; Albrektsson, T. Temperature Threshold Levels for Heat-Induced Bone Tissue Injury: A Vital-Microscopic Study in the Rabbit. J. Prosthet. Dent. 1983, 50, 101–107. [Google Scholar] [PubMed]
- Eriksson, R.A.; Albrektsson, T. The Effect of Heat on Bone Regeneration: An Experimental Study in the Rabbit Using the Bone Growth Chamber. J. Oral Maxillofac. Surg. 1984, 42, 705–711. [Google Scholar] [PubMed]
- Möhlhenrich, S.C.; Modabber, A.; Steiner, T.; Mitchell, D.A.; Hölzle, F. Heat Generation and Drill Wear during Dental Implant Site Preparation: Systematic Review. Br. J. Oral Maxillofac. Surg. 2015, 53, 679–689. [Google Scholar]
- Chacon, G.E.; Bower, D.L.; Larsen, P.E.; McGlumphy, E.A.; Beck, F.M. Heat Production by 3 Implant Drill Systems after Repeated Drilling and Sterilization. J. Oral Maxillofac. Surg. 2006, 64, 265–269. [Google Scholar]
- Ercoli, C.; Funkenbusch, P.D.; Lee, H.-J.; Moss, M.E.; Graser, G.N. The Influence of Drill Wear on Cutting Efficiency and Heat Production during Osteotomy Preparation for Dental Implants: A Study of Drill Durability. Int. J. Oral Maxillofac. Implants 2004, 19, 335–349. [Google Scholar]
- Cordioli, G.; Majzoub, Z. Heat Generation during Implant Site Preparation: An in Vitro Study. Int. J. Oral Maxillofac. Implants 1997, 12, 186–193. [Google Scholar] [PubMed]
- Matthews, L.S.; Hirsch, C. Temperatures Measured in Human Cortical Bone When Drilling. J. Bone Jt. Surg. Am. 1972, 54, 297–308. [Google Scholar]
- Jochum, R.M.; Reichart, P.A. Influence of Multiple Use of Timedur-Titanium Cannon Drills: Thermal Response and Scanning Electron Microscopic Findings. Clin. Oral Implants Res. 2000, 11, 139–143. [Google Scholar] [PubMed]
- González-Alonso, J. Human Thermoregulation and the Cardiovascular System. Exp. Physiol. 2012, 97, 340–346. [Google Scholar]
- Harris, B.H.; Kohles, S.S. Effects of Mechanical and Thermal Fatigue on Dental Drill Performance. Int. J. Oral Maxillofac. Implants 2001, 16, 819–826. [Google Scholar] [PubMed]
- Elani, H.W.; Starr, J.R.; Da Silva, J.D.; Gallucci, G.O. Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026. J. Dent. Res. 2018, 97, 1424–1430. [Google Scholar] [PubMed]
- Alevizakos, V.; Mitov, G.; Ahrens, A.M.; von See, C. The Influence of Implant Site Preparation and Sterilization on the Performance and Wear of Implant Drills. Int. J. Oral Maxillofac. Implants 2021, 36, 546–552. [Google Scholar] [PubMed]
- Batista Mendes, G.C.; Padovan, L.E.M.; Ribeiro-Júnior, P.D.; Sartori, E.M.; Valgas, L.; Claudino, M. Influence of Implant Drill Materials on Wear, Deformation, and Roughness after Repeated Drilling and Sterilization. Implant Dent. 2014, 23, 188–194. [Google Scholar]
- Koo, K.-T.; Kim, M.-H.; Kim, H.-Y.; Wikesjö, U.M.E.; Yang, J.-H.; Yeo, I.-S. Effects of Implant Drill Wear, Irrigation, and Drill Materials on Heat Generation in Osteotomy Sites. J. Oral Implantol. 2015, 41, e19–e23. [Google Scholar]
- Fung, Y.C. Biomechanics: Mechanical Properties of Living Tissues, 2nd ed.; Springer: New York, NY, USA, 2010; p. 568. [Google Scholar]
- Watanabe, F.; Tawada, Y.; Komatsu, S.; Hata, Y. Heat Distribution in Bone during Preparation of Implant Sites: Heat Analysis by Real-Time Thermography. Int. J. Oral Maxillofac. Implants 1992, 7, 212–219. [Google Scholar]
- Parr, G.R. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. J. Prosthet. Dent. 1985, 54, 611–612. [Google Scholar]
- Chai, W.L.; Moharamzadeh, K.; Brook, I.M.; Emanuelsson, L.; Palmquist, A.; van Noort, R. Development of a Novel Model for the Investigation of Implant-Soft Tissue Interface. J. Periodontol. 2010, 81, 1187–1195. [Google Scholar]
- Misch, C.E.; Qu, Z.; Bidez, M.W. Mechanical Properties of Trabecular Bone in the Human Mandible: Implications for Dental Implant Treatment Planning and Surgical Placement. J. Oral Maxillofac. Surg. 1999, 57, 700–706, discussion 706–708. [Google Scholar]
- Msallem, B.; Sharma, N.; Cao, S.; Halbeisen, F.S.; Zeilhofer, H.-F.; Thieringer, F.M. Evaluation of the Dimensional Accuracy of 3D-Printed Anatomical Mandibular Models Using FFF, SLA, SLS, MJ, and BJ Printing Technology. J. Clin. Med. 2020, 9, 817. [Google Scholar]
- Heidari, B.; Khalesi, M.; Khodadoustan, A.; Kadkhodazadeh, M. The Influence of Cortical Width of Sheep Bone on the Primary Stability of Dental Implants: An in Vitro Study. J. Long Term Eff. Med. Implants 2013, 23, 87–91. [Google Scholar]
- Chakravarthy, C.; Malyala, S.K.; Aranha, D.; Suryadevara, S.S.; Sunder, V. Comparative Evaluation of Hybrid 3D-Printed Models versus Cadaveric Animal Jaws: A Student’s Perspective. J. Maxillofac. Oral Surg. 2022, 21, 1044–1051. [Google Scholar]
- Brisman, D.L. The Effect of Speed, Pressure, and Time on Bone Temperature during the Drilling of Implant Sites. Int. J. Oral Maxillofac. Implants 1996, 11, 35–37. [Google Scholar] [PubMed]
- Eriksson, R.A.; Adell, R. Temperatures during Drilling for the Placement of Implants Using the Osseointegration Technique. J. Oral Maxillofac. Surg. 1986, 44, 4–7. [Google Scholar]
- Hobkirk, J.A.; Rusiniak, K. Investigation of Variable Factors in Drilling Bone. J. Oral Surg. 1977, 35, 968–973. [Google Scholar]
- Lavelle, C.; Wedgwood, D. Effect of Internal Irrigation on Frictional Heat Generated from Bone Drilling. J. Oral Surg. 1980, 38, 499–503. [Google Scholar]
- Pallan, F.G. Histological Changes in Bone after Insertdon of Skeletal Fixation Pins. J. Oral Surg. Anesth. Hosp. Dent. Serv. 1960, 18, 400–408. [Google Scholar] [PubMed]
- Sutter, F.; Krekeler, G.; Schwammberger, A.E.; Sutter, F.J. Atraumatic Surgical Technique and Implant Bed Preparation. Quintessence Int. 1992, 23, 811–816. [Google Scholar]
- Thompson, H.C. Effect of Drilling into Bone. J. Oral Surg. 1958, 16, 22–30. [Google Scholar]
- Oh, H.J.; Wikesjö, U.M.E.; Kang, H.-S.; Ku, Y.; Eom, T.-G.; Koo, K.-T. Effect of Implant Drill Characteristics on Heat Generation in Osteotomy Sites: A Pilot Study. Clin. Oral Implants Res. 2011, 22, 722–726. [Google Scholar] [PubMed]
- Jung, O.; Lindner, C.; Pantermehl, S.; Barbeck, M. Heat Development during Medical Drilling: Influencing Factors and Examination Methods—Overview and First Results. In Vivo 2021, 35, 3011–3017. [Google Scholar] [PubMed]
- Badrfam, R.; Noorbala, A.A.; Vahabi, Z.; Zandifar, A. Creutzfeldt-Jakob Disease after Dental Procedure along with the Initial Manifestations of Psychiatric Disorder: A Case Report. Iran. J. Psychiatry 2021, 16, 106–110. [Google Scholar]
- Sushma, B.; Gugwad, S.; Pavaskar, R.; Malik, S.A. Prions in Dentistry: A Need to Be Concerned and Known. J. Oral Maxillofac. Pathol. 2016, 20, 111–114. [Google Scholar]
- Bertram, J.; Mielke, M.; Beekes, M.; Lemmer, K.; Baier, M.; Pauli, G. Inactivation and Removal of Prions in Producing Medical Products. A Contribution to Evaluation and Declaration of Possible Methods. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2004, 47, 36–40. [Google Scholar]
- Maccauro, G.; Bianchino, G.; Sangiorgi, S.; Magnani, G.; Marotta, D.; Manicone, P.F.; Raffaelli, L.; Rossi Iommetti, P.; Stewart, A.; Cittadini, A.; et al. Development of a New Zirconia-Toughened Alumina: Promising Mechanical Properties and Absence of in Vitro Carcinogenicity. Int. J. Immunopathol. Pharmacol. 2009, 22, 773–779. [Google Scholar] [PubMed]
- Nistor, L.; Grădinaru, M.; Rîcă, R.; Mărășescu, P.; Stan, M.; Manolea, H.; Ionescu, A.; Moraru, I. Zirconia Use in Dentistry—Manufacturing and Properties. Curr. Health Sci. J. 2019, 45, 28–35. [Google Scholar] [PubMed]
- Nakai, H.; Inokoshi, M.; Nozaki, K.; Komatsu, K.; Kamijo, S.; Liu, H.; Shimizubata, M.; Minakuchi, S.; Van Meerbeek, B.; Vleugels, J.; et al. Additively Manufactured Zirconia for Dental Applications. Materials 2021, 14, 3694. [Google Scholar]








Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alevizakos, V.; Mosch, R.; von See, C. Influence of Multiple Used Implant Drills on Their Cutting Performance and Fracture Resistance. Materials 2023, 16, 5271. https://doi.org/10.3390/ma16155271
Alevizakos V, Mosch R, von See C. Influence of Multiple Used Implant Drills on Their Cutting Performance and Fracture Resistance. Materials. 2023; 16(15):5271. https://doi.org/10.3390/ma16155271
Chicago/Turabian StyleAlevizakos, Vasilios, Richard Mosch, and Constantin von See. 2023. "Influence of Multiple Used Implant Drills on Their Cutting Performance and Fracture Resistance" Materials 16, no. 15: 5271. https://doi.org/10.3390/ma16155271
APA StyleAlevizakos, V., Mosch, R., & von See, C. (2023). Influence of Multiple Used Implant Drills on Their Cutting Performance and Fracture Resistance. Materials, 16(15), 5271. https://doi.org/10.3390/ma16155271





