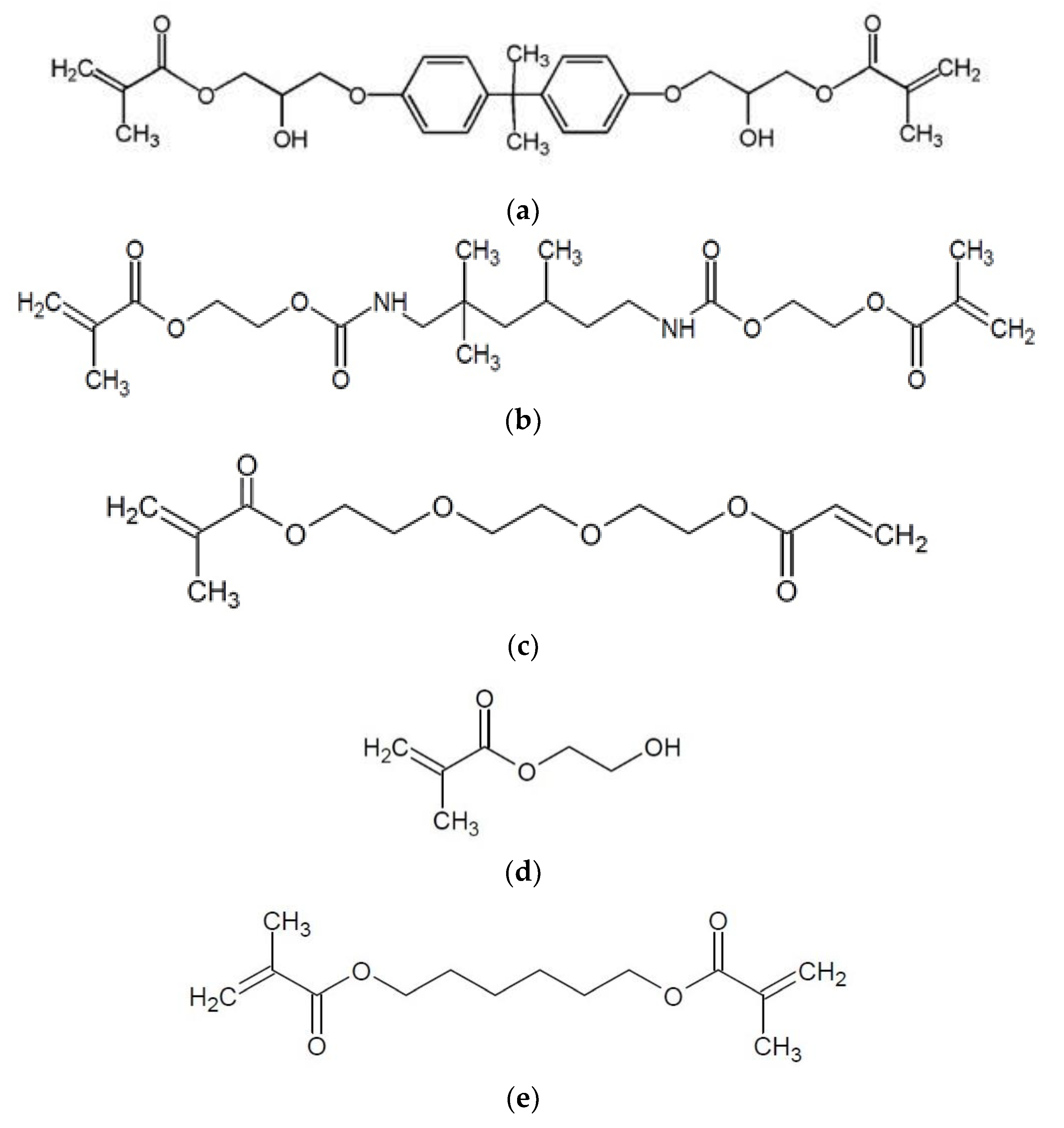
The Influence of Low-Molecular-Weight Monomers (TEGDMA, HDDMA, HEMA) on the Properties of Selected Matrices and Composites Based on Bis-GMA and UDMA
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Resin Materials
- UDMA/bis-GMA/TEGDMA/HEMA vs. UDMA/bis-GMA/HDDMA (p-value = 0.000130); UDMA/bis-GMA/TEGDMA/HDDMA (p-value = 0.0052); UDMA/bis-GMA/TEGDMA (p-value = 0.0007); UDMA/bis-GMA/HEMA (p-value = 0.0002);
- UDMA/bis-GMA/HDDMA vs. UDMA/bis-GMA/TEGDMA/HDDMA (p-value = 0.0187).
- UDMA/bis-GMA/HEMA vs. UDMA/bis-GMA/HDDMA (p-value = 0.0015) and UDMA/bis-GMA/TEGDMA (p-value = 0.0179).
- UDMA/bis-GMA/TEGDMA/HDDMA vs. UDMA/bis-GMA/TEGDMA/HEMA (p-value = 0.0281).
3.2. Composite Materials
- UDMA/bis-GMA/TEGDMA/HEMA vs. UDMA/bis-GMA/HDDMA (p-value = 0.0047), UDMA/bis-GMA/TEGDMA/HDDMA (p-value = 0.0348), and UDMA/bis-GMA/TEGDMA (p-value = 0.0070);
- UDMA/bis-GMA/HEMA vs. UDMA/bis-GMA/HDDMA (p-value = 0.0051), UDMA/bis-GMA/TEGDMA/HDDMA (p-value = 0.0380), and UDMA/bis-GMA/TEGDMA (p-value = 0.0077).
- UDMA/bis-GMA/HDDMA vs. UDMA/bis-GMA/HEMA (p-value = 0.0075).
- UDMA/bis-GMA/TEGDMA vs. UDMA/bis-GMA/TEGDMA/HEMA (p-value = 0.0071).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ozdemir, D. Dental Caries: The Most Common Disease Worldwide and Preventive Strategies. Int. J. Biol. 2013, 5, 55–61. [Google Scholar] [CrossRef]
- Pitts, N.B.; Twetman, S.; Fisher, J.; Marsh, P.D. Understanding dental caries as a non-communicable disease. Br. Dent. J. 2021, 231, 749–753. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Huang, X.; Li, M.; Peng, X.; Wang, S.; Zhou, X.; Cheng, L. Development and status of resin composite as dental restorative materials. J. Appl. Polym. Sci. 2019, 136, 48180. [Google Scholar] [CrossRef]
- Szczesio-Wlodarczyk, A.; Sokolowski, J.; Kleczewska, J.; Bociong, K. Ageing of dental composites based on methacrylate resins-A critical review of the causes and method of assessment. Polymers 2020, 12, 882. [Google Scholar] [CrossRef]
- Cramer, N.B.B.; Stansbury, J.W.W.; Bowman, C.N.N. Recent advances and developments in composite dental restorative materials. J. Dent. Res. 2011, 90, 402–416. [Google Scholar] [CrossRef] [PubMed]
- Barszczewska-Rybarek, I.M. Structure-property relationships in dimethacrylate networks based on Bis-GMA, UDMA and TEGDMA. Dent. Mater. 2009, 25, 1082–1089. [Google Scholar] [CrossRef] [PubMed]
- Gajewski, V.E.S.; Pfeifer, C.S.; Fróes-Salgado, N.R.G.; Boaro, L.C.C.; Braga, R.R. Monomers used in resin composites: Degree of conversion, mechanical properties and water sorption/solubility. Braz. Dent. J. 2012, 23, 508–514. [Google Scholar] [CrossRef]
- Tauscher, S.; Angermann, J.; Catel, Y.; Moszner, N. Evaluation of alternative monomers to HEMA for dental applications. Dent. Mater. 2017, 33, 857–865. [Google Scholar] [CrossRef]
- Van Landuyt, K.L.; Snauwaert, J.; Peumans, M.; De Munck, J.; Lambrechts, P.; Van Meerbeek, B. The role of HEMA in one-step self-etch adhesives. Dent. Mater. 2008, 24, 1412–1419. [Google Scholar] [CrossRef]
- van Dijken, J.W.V.; Pallesen, U. Durability of a low shrinkage TEGDMA/HEMA-free resin composite system in Class II restorations. A 6-year follow up. Dent. Mater. 2017, 33, 944–953. [Google Scholar] [CrossRef]
- Sunarintyas, S.; Siswomihardjo, W.; Irnawati, D.; Matinlinna, J.P. Evaluation on residual monomer of HDDMA matrix system on fider reinforced condosites (FRC). Dentika Dent. J. 2014, 18, 153–157. [Google Scholar] [CrossRef]
- International Organization for Standardization. ISO 4049:2019: Dentistry—Polymer-Based Restorative Materials; ISO Publishing: Geneve, Switzerland, 2019; pp. 1–29. [Google Scholar]
- Ilie, N.; Hilton, T.J.; Heintze, S.D.; Hickel, R.; Watts, D.C.; Silikas, N.; Stansbury, J.W.; Cadenaro, M.; Ferracane, J.L. Academy of Dental Materials guidance—Resin composites: Part I—Mechanical properties. Dent. Mater. 2017, 33, 880–894. [Google Scholar] [CrossRef] [PubMed]
- Penn, R.; Craig, R.; Tesk, J. Diametral tensile strength and dental composites. Dent. Mater. 1987, 3, 46–48. [Google Scholar] [CrossRef]
- Bona, D.A.; Benetti, P.; Borba, M.; Cecchetti, D. Flexural and diametral tensile strength of composite resins. Restor. Dent. Braz. Oral Res. 2008, 22, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Szczesio-Wlodarczyk, A.; Domarecka, M.; Kopacz, K.; Sokolowski, J.; Bociong, K. An evaluation of the properties of urethane dimethacrylate-based dental resins. Materials 2021, 14, 2727. [Google Scholar] [CrossRef]
- Bociong, K.; Nowak, J.; Szczesio, A.; Sokołowski, K.; Sokołowski, J. Selected mechanical properties of a light-curable experimental dental composites. Part 1 Naprężenia skurczowe generowane podczas fotoutwardzania eksperymentalnego kompozytu stomatologicznego. Cz. I. Przem. Chem. 2017, 1, 72–74. [Google Scholar] [CrossRef]
- Domarecka, M.; Sokołowski, K.; Krasowski, M.; Szczesio, A.; Bociong, K.; Sokołowski, J.; Łukomska-Szymańska, M. Influence of water sorption on the shrinkage stresses of dental composites. J. Stoma. 2016, 64, 476–483. [Google Scholar]
- Timoshenko, S.; Goodier, J.N. Theory of Elasticity, 2nd ed.; McGraw-Hill: New York, NY, USA, 1951. [Google Scholar]
- Aminoroaya, A.; Neisiany, R.E.; Khorasani, S.N.; Panahi, P.; Das, O.; Madry, H.; Cucchiarini, M.; Ramakrishna, S. A review of dental composites: Challenges, chemistry aspects, filler influences, and future insights. Compos. Part B Eng. 2021, 216, 108852. [Google Scholar] [CrossRef]
- Raskin, A.; Michotte-Theall, B.; Vreven, J.; Wilson, N.H.F. Clinical evaluation of a posterior composite 10-year report. J. Dent. 1999, 27, 13–19. [Google Scholar] [CrossRef]
- Loguércio, A.D.; Demarco, F.F.; da Rosa Rodolpho, P.A.; Cenci, M.S.; Donassollo, T.A. A clinical evaluation of posterior composite restorations: 17-year findings. J. Dent. 2005, 34, 427–435. [Google Scholar] [CrossRef]
- Leinfelder, K.F.; May, K.N.; Wilder, A.D.; Bayne, S.C.; Taylor, D.F. Seventeen-Year Clinical Study of Ultraviolet-Cured Posterior Composite Class I and II Restorations. J. Esthet. Restor. Dent. 2007, 11, 135–142. [Google Scholar] [CrossRef]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguércio, A.D.; Moraes, R.R.; Bronkhorst, E.M.; Opdam, N.J.M.; Demarco, F.F. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef]
- Heymann, H.; Swift, E.J.; Ritter, A.V.; Sturdevant, C.M. Sturdevant’s Art and Science of Operative Dentistry; Elsevier/Mosby: Amsterdam, The Netherlands, 2013; ISBN -9780323170604. [Google Scholar]
- Anusavice, K.; Shen, C.; Rawls, H.R. (Eds.) Phillips’ Science of Dental Materials, 12th ed.; Saunders: Philadelphia, PA, USA, 2012. [Google Scholar]
- Ferracane, J.L. Resin-based composite performance: Are there some things we can’t predict? Dent. Mater. 2013, 29, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Ersoy, M.; Civelek, A.; L’Hotelier, E.; Say, E.C.; Soyman, M. Physical Properties of Different Composites. Dent. Mater. J. 2004, 23, 278–283. [Google Scholar] [CrossRef][Green Version]
- Yap, A.U.J.; Teoh, S.H. Comparison of flexural properties of composite restoratives using the iso and mini-flexural tests. J. Oral Rehabil. 2003, 30, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Peutzfeldt, A.; Asmussen, E. Modulus of resilience as predictor for clinical wear of restorative resins. Dent. Mater. 1992, 8, 146–148. [Google Scholar] [CrossRef]
- Arcís, R.W.; López-Macipe, A.; Toledano, M.; Osorio, E.; Rodríguez-Clemente, R.; Murtra, J.; Fanovich, M.A.; Pascual, C.D. Mechanical properties of visible light-cured resins reinforced with hydroxyapatite for dental restoration. Dent. Mater. 2002, 18, 49–57. [Google Scholar] [CrossRef]
- Sideridou, I.; Tserki, V.; Papanastasiou, G. Effect of chemical structure on degree of conversion in light-cured dimethacrylate-based dental resins. Biomaterials 2002, 23, 1819–1829. [Google Scholar] [CrossRef]
- Antonucci, J.M.; Icenogle, T.B.; Regnault, W.; Liu, D.W.; O’Donnell, J.N.R.; Skrtic, D. Polymerization shrinkage and stress development in bioactive urethane acrylic resin composites. Polym. Prepr. 2006, 47, 498–499. [Google Scholar]
- Park, C.; Robertson, R.E. Mechanical properties of resin composites with filler particles aligned by an electric field. Dent. Mater. 1998, 14, 385–393. [Google Scholar] [CrossRef]
- Ling, L.; Xu, X.; Choi, G.Y.; Billodeaux, D.; Guo, G.; Diwan, R.M. Novel F-releasing composite with improved mechanical properties. J. Dent. Res. 2009, 88, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Perras, M.A.; Diederichs, M.S. A Review of the Tensile Strength of Rock: Concepts and Testing. Geotech. Geol. Eng. 2014, 32, 525–546. [Google Scholar] [CrossRef]
- AlAwad, M.N.J. Modification of the Brazilian indirect tensile strength formula for better estimation of the tensile strength of rocks and rock-like geomaterials. J. King Saud Univ. Eng. Sci. 2020. [Google Scholar] [CrossRef]
- Craig, R.G. Materiały Stomatologiczne, 12th ed.; Powers, J.M., Sakaguchi, R.L., Shaw, H., Shaw, J.G., Eds.; Edra Urban & Partner: Wrocław, Poland, 2008; ISBN -9780323081085. [Google Scholar]
- American Dental Association. ADA Specification No. 27: Resin-Based Filling Material; American Dental Association: Chicago, IL, USA, 1993. [Google Scholar]
- Zidan, O.; Asmussen, E.; Jørgensen, K.D. Tensile strength of restorative resins. Eur. J. Oral Sci. 1980, 88, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Musanje, L.; Ferracane, J.L. Effects of resin formulation and nanofiller surface treatment on the properties of experimental hybrid resin composite. Biomaterials 2004, 25, 4065–4071. [Google Scholar] [CrossRef]
- Stencel, R.; Pakieła, W.; Barszczewska-Rybarek, I.; Żmudzki, J.; Kasperski, J.; Chladek, G. Effects of Different Inorganic Fillers on Mechanical Properties and Degree of Conversion of Dental Resin Composites. Arch. Metall. Mater. 2018, 63, 1361–1369. [Google Scholar] [CrossRef]
- Bucuta, S.; Ilie, N. Light transmittance and micro-mechanical properties of bulk fill vs. conventional resin based composites. Clin. Oral Investig. 2014, 18, 1991–2000. [Google Scholar] [CrossRef]
- Poggio, C.; Lombardini, M.; Gaviati, S.; Chiesa, M. Evaluation of Vickers hardness and depth of cure of six composite resins photo-activated with different polymerization modes. J. Conserv. Dent. 2012, 15, 237–241. [Google Scholar] [CrossRef]
- Chinelatti, M.A.; Chimello, D.T.; Ramos, R.P.; Palma-Dibb, R.G. Evaluation of the surface hardness of composite resins before and after polishing at different times. J. Appl. Oral Sci. 2006, 14, 188–192. [Google Scholar] [CrossRef]
- Aung, S.Z.; Takagaki, T.; Ikeda, M.; Nozaki, K.; Burrow, M.F.; Abdou, A.; Nikaido, T.; Tagami, J. The effect of different light curing units on vickers microhardness and degree of conversion of flowable resin composites. Dent. Mater. J. 2021, 40, 44–51. [Google Scholar] [CrossRef]
- Łukomska-Szymańska, M.; Kleczewska, J.; Nowak, J.; Pryliński, M.; Szczesio, A.; Podlewska, M.; Sokołowski, J.; Łapińska, B. Mechanical Properties of Calcium Fluoride-Based Composite Materials. Biomed Res. Int. 2016, 2016, 2752506. [Google Scholar] [CrossRef] [PubMed]
- Bociong, K.; Szczesio, A.; Krasowski, M.; Sokolowski, J. The influence of filler amount on selected properties of new experimental resin dental composite. Open Chem. 2018, 16, 905–911. [Google Scholar] [CrossRef]
- Schmidt, C.; Ilie, N. The mechanical stability of nano-hybrid composites with new methacrylate monomers for matrix compositions. Dent. Mater. 2012, 28, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Randolph, L.D.; Palin, W.M.; Leloup, G.; Leprince, J.G. Filler characteristics of modern dental resin composites and their influence on physico-mechanical properties. Dent. Mater. 2016, 32, 1586–1599. [Google Scholar] [CrossRef] [PubMed]
- Domarecka, M.; Sokołowska, A.; Szynkowska, M.I.; Sokołowski, K.; Sokołowski, J.; Łukomska-Szymańska, M. Wybrane właściwości materiałów kompozytowych typu flow o niskim skurczu polimeryzacyjnym. Przem. Chem. 2014, 93, 775–778. [Google Scholar] [CrossRef]
- Oliveira, K.M.C.; Consani, S.; Gonçalves, L.S.; Brandt, W.C.; Ccahuana-Vásquez, R.A. Photoelastic evaluation of the effect of composite formulation on polymerization shrinkage stress. Braz. Oral Res. 2012, 26, 202–208. [Google Scholar] [CrossRef][Green Version]
- Münchow, E.A.; Meereis, C.T.W.; de Oliveira da Rosa, W.L.; da Silva, A.F.; Piva, E. Polymerization shrinkage stress of resin-based dental materials: A systematic review and meta-analyses of technique protocol and photo-activation strategies. J. Mech. Behav. Biomed. Mater. 2018, 82, 77–86. [Google Scholar] [CrossRef]
- Schneider, L.F.J.; Cavalcante, L.M.; Silikas, N. Shrinkage stresses generated during resin-composite applications: A review. J. Dent. Biomech. 2010, 1, 131630. [Google Scholar] [CrossRef]
- Braga, R.R.; Ferracane, J.L. Alternatives in polymerization contraction stress management. Crit. Rev. Oral Biol. Med. 2004, 15, 176–184. [Google Scholar] [CrossRef]
- Ferracane, J.L. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent. Mater. 2005, 21, 36–42. [Google Scholar] [CrossRef]
- Al Sunbul, H.; Silikas, N.; Watts, D.C. Polymerization shrinkage kinetics and shrinkage-stress in dental resin-composites. Dent. Mater. 2016, 32, 998–1006. [Google Scholar] [CrossRef] [PubMed]
- Robles-Moreno, M. Polymerization Shrinkage Stresses of Different Flowable and Universal Bulk-Fill Composites. Adv. Dent. Oral Health 2019, 10, 555794. [Google Scholar] [CrossRef]
- Ernst, C.P.; Meyer, G.R.; Klucker, K.; Willershausen, B. Determination of polymerization shrinkage stress by means of a photoelastic investigation. Dent. Mater. 2004, 20, 313–321. [Google Scholar] [CrossRef]
- Bociong, K.; Szczesio, A.; Sokolowski, K.; Domarecka, M.; Sokolowski, J.; Krasowski, M.; Lukomska-Szymanska, M. The Influence of Water Sorption of Dental Light-Cured Composites on Shrinkage Stress. Materials 2017, 10, 1142. [Google Scholar] [CrossRef] [PubMed]
- Gonalves, F.; Azevedo, C.L.N.; Ferracane, J.L.; Braga, R.R. BisGMA/TEGDMA ratio and filler content effects on shrinkage stress. Dent. Mater. 2011, 27, 520–526. [Google Scholar] [CrossRef]
- Love, B.J.; Piguet Ruinet, F.; Teyssandier, F. Chemorheology of Photopolymerizable Acrylates Using a Modified Boltzmann Sigmoidal Model. J. Polym. Sci. Part B Polym. Phys. 2004, 46, 2319–2325. [Google Scholar] [CrossRef][Green Version]
- Watts, D.C.; Hindi, A. Al Intrinsic “soft-start” polymerisation shrinkage-kinetics in an acrylate-based resin-composite. Dent. Mater. 1999, 15, 39–45. [Google Scholar] [CrossRef]
| Matrix | Percentage of Individual Monomers (wt.%) | ||||
|---|---|---|---|---|---|
| bis-GMA | UDMA | TEGDMA | HEMA | HDDMA | |
| UDMA/bis-GMA/HDDMA | 40 | 40 | - | - | 20 |
| UDMA/bis-GMA/TEGDMA/HDDMA | 40 | 40 | 10 | - | 10 |
| UDMA/bis-GMA/TEGDMA | 40 | 40 | 20 | - | - |
| UDMA/bis-GMA/TEGDMA/HEMA | 40 | 40 | 10 | 10 | - |
| UDMA/bis-GMA/HEMA | 40 | 40 | - | 20 | - |
| Test | Result Type | UDMA/bis-GMA/HDDMA 40/40/20 | UDMA/bis-GMA/TEGDMA/HDDMA 40/40/10/10 | UDMA/bis-GMA/TEGDMA 40/40/20 | UDMA/bis-GMA/TEGDMA/HEMA 40/40/10/10 | UDMA/bis-GMA/HEMA 40/40/20 |
|---|---|---|---|---|---|---|
| FS | M (SD) | 73.4 a,e (7.2) | 83.4 b,e (4.7) | 81.2 c (2.6) | 92.9 a,b,c,d (3.8) | 79.2 d (2.7) |
| FM | M (SD) | 1514 (250) | 1603 (321) | 1585 (241) | 1828 (281) | 1798 (139) |
| DTS | MD (QD) | 42.2 a (9.6) | 49.7 (4.8) | 48.6 b (1.6) | 55.5 (5.4) | 64.3 a,b (3.7) |
| HV | MD (QD) | 14 (1) | 16 a (1) | 15 (0) | 14 a (0) | 15 (1) |
| Test | Result Type | UDMA/bis-GMA/HDDMA 40/40/20 | UDMA/bis-GMA/TEGDMA/HDDMA 40/40/10/10 | UDMA/bis-GMA/TEGDMA 40/40/20 | UDMA/bis-GMA/TEGDMA/HEMA 40/40/10/10 | UDMA/bis-GMA/HEMA 40/40/20 |
|---|---|---|---|---|---|---|
| FS | M (SD) | 81.5 (10.9) | 79.3 (11.1) | 81.7 (5.0) | 95.7 (10.5) | 82.5 (13.4) |
| FM | M (SD) | 3673 a,d (172) | 3782 b,e (78) | 3695 c,f (364) | 4173 a,b,c (237) | 4168 d,e,f, (122) |
| DTS | M (SD) | 29.0 a (3.6) | 31.8 (5.4) | 33.6 (2.4) | 32.8 (6.2) | 37.4 a (5.8) |
| HV | MD (QD) | 25 (1) | 25 (0) | 25 a (1) | 26 a (1) | 26 (1) |
| PSS | M (SD) | 9.8 (1.6) | 10.4 (0.9) | 9.2 (0.9) | 7.8 (0.6) | 9.9 (0.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szczesio-Wlodarczyk, A.; Polikowski, A.; Krasowski, M.; Fronczek, M.; Sokolowski, J.; Bociong, K. The Influence of Low-Molecular-Weight Monomers (TEGDMA, HDDMA, HEMA) on the Properties of Selected Matrices and Composites Based on Bis-GMA and UDMA. Materials 2022, 15, 2649. https://doi.org/10.3390/ma15072649
Szczesio-Wlodarczyk A, Polikowski A, Krasowski M, Fronczek M, Sokolowski J, Bociong K. The Influence of Low-Molecular-Weight Monomers (TEGDMA, HDDMA, HEMA) on the Properties of Selected Matrices and Composites Based on Bis-GMA and UDMA. Materials. 2022; 15(7):2649. https://doi.org/10.3390/ma15072649
Chicago/Turabian StyleSzczesio-Wlodarczyk, Agata, Aleksander Polikowski, Michał Krasowski, Magdalena Fronczek, Jerzy Sokolowski, and Kinga Bociong. 2022. "The Influence of Low-Molecular-Weight Monomers (TEGDMA, HDDMA, HEMA) on the Properties of Selected Matrices and Composites Based on Bis-GMA and UDMA" Materials 15, no. 7: 2649. https://doi.org/10.3390/ma15072649
APA StyleSzczesio-Wlodarczyk, A., Polikowski, A., Krasowski, M., Fronczek, M., Sokolowski, J., & Bociong, K. (2022). The Influence of Low-Molecular-Weight Monomers (TEGDMA, HDDMA, HEMA) on the Properties of Selected Matrices and Composites Based on Bis-GMA and UDMA. Materials, 15(7), 2649. https://doi.org/10.3390/ma15072649






