Effect of Titanium-Base Abutment Height on Optical Properties of Monolithic Anterior Zirconia Crowns
Abstract
1. Introduction
2. Material and Methods
3. Results
4. Discussion
5. Conclusions
- Using a 5.5 mm-height ti-base abutment may produce a clinically unacceptable outcome (ΔEab > 2) in A1/0 and A2/3 shades of monolithic translucent zirconia.
- When restoring A1/0 and A2/3 shades of monolithic anterior zirconia restorations using high ti-base abutments, the final color may be largely affected.
- If possible, using a short ti-base abutment may be favorable when restoring a monolithic anterior A1/0 and A2/3 shade zirconia, providing that the retention forces must be considered, depending on the length of the restored crown.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zarauz, C.; Pitta, J.; Pradíes, G.; Sailer, I. Clinical Recommendations for Implant Abutment Selection for Single-Implant Reconstructions: Customized vs Standardized Ceramic and Metallic Solutions. Int. J. Periodontics Restor. Dent. 2020, 40, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Gou, M.; Chen, H.; Fu, M.; Wang, H. Fracture of Zirconia Abutments in Implant Treatments: A Systematic Review. Implant Dent. 2019, 4, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Pitta, J.; Hjerppe, J.; Burkhardt, F.; Fehmer, V.; Mojon, P.; Sailer, I. Mechanical stability and technical outcomes of monolithic CAD/CAM fabricated abutment-crowns supported by titanium bases: An in vitro study. Clin. Oral Implants Res. 2021, 32, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Nouh, I.; Kern, M.; Sabet, A.E.; Aboelfadl, A.K.; Hamdy, A.M.; Chaar, M.S. Mechanical behavior of posterior all-ceramic hybrid-abutment-crowns versus hybrid-abutments with separate crowns—A laboratory study. Clin. Oral Implants Res. 2019, 30, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Conejo, J.; Kobayashi, T.; Anadioti, E.; Blatz, M.B. Performance of CAD/CAM monolithic ceramic Implant-supported restorations bonded to titanium inserts: A systematic review. Eur. J. Oral Implantol. 2017, 10, 139–146. [Google Scholar] [PubMed]
- López-Píriz, R.; Cabal, B.; Goyos-Ball, L.; Fernandez, A.; Bartolomé, J.F.; Moya, J.S.; Torrecillas, R. Current state-of-the-art and future perspectives of the three main modern implant-dentistry concerns: Aesthetic requirements, mechanical properties, and peri-implantitis prevention. J. Biomed. Mater. Res. A 2019, 107, 1466–1475. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.E.; Soares, S.; Machado, C.M.; Bergamo, E.T.P.; Coelho, P.G.; Witek, L.; Ramalho, I.S.; Jalkh, E.B.B.; Bonfante, E.A. Effect of CAD/CAM abutment height and cement type on the retention of zirconia crowns. Implant Dent. 2018, 27, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Ghinea, R.; Pérez, M.M.; Herrera, L.J.; Rivas, M.J.; Yebra, A.; Paravina, R.D. Color difference thresholds in dental ceramics. J. Dent. 2010, 38, e57–e64. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.J.; Trushkowsky, R.D.; Paravina, R.D. Dental color matching instruments and systems. Review of clinical and research aspects. J. Dent. 2010, 38, e2–e16. [Google Scholar] [CrossRef] [PubMed]
- Kim-Pusateri, S.; Brewer, J.D.; Davis, E.L.; Wee, A.G. Reliability and accuracy of four dental shade-matching devices. J. Prosthet. Dent. 2009, 101, 193–199. [Google Scholar] [CrossRef]
- Westland, S. Review of the CIE system of colorimetry and its use in dentistry. J. Esthet. Restor. Dent. 2003, 15, 5–12. [Google Scholar] [CrossRef] [PubMed]
- CIE (Commission Internationale de l’Eclairage). Colorimetry-Technical Report, 2nd ed.; CIE Pub. No.15; Bureau Central de la CIE: Vienna, Austria, 1986; (corrected reprint 1996). [Google Scholar]
- Bayindir, F.; Koseoglu, M. The effect of restoration thickness and resin cement shade on the color and translucency of a high-translucency monolithic zirconia. J. Prosthet. Dent. 2020, 123, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Saito, O.; Fuyikawa, J.; Ishigaki, S. Influence of abutment substrate and ceramic thickness on the colour of heat-pressed ceramic crowns. J. Oral Rehabil. 2002, 29, 805–809. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y. Making yttria-stabilized tetragonal zirconia translucent. Dent. Mater. 2014, 30, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.-E.; Lim, Y.-J.; Han, J.-S.; Yeo, I.L.; Yoon, H.I. Effect of Yttria Content on the Translucency and Masking Ability of Yttria-Stabilized Tetragonal Zirconia Polycrystal. Materials 2020, 13, 4726. [Google Scholar] [CrossRef] [PubMed]
- Khashayar, G.; Bain, P.A.; Salari, S.; Dozic, A.; Kleverlaan, C.J.; Feilzer, A.J. Perceptibility and acceptability thresholds for colour differences in dentistry. J. Dent. 2014, 42, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Kontonasaki, E.; Rigos, A.E.; Ilia, C.; Istantsos, T. Monolithic Zirconia: An Update to Current Knowledge. Optical Properties, Wear, and Clinical Performance. Dent. J. 2019, 7, 90. [Google Scholar] [CrossRef] [PubMed]
- Hardan, L.; Bourgi, R.; Cuevas-Suárez, C.E.; Lukomska-Szymanska, M.; Monjarás-Ávila, A.J.; Zarow, M.; Jakubowicz, N.; Jorquera, G.; Ashi, T.; Mancino, D.; et al. Novel Trends in Dental Color Match Using Different Shade Selection Methods: A Systematic Review and Meta-Analysis. Materials 2022, 15, 468. [Google Scholar] [CrossRef] [PubMed]
- Al-Zordk, W.; Saker, S. Impact of sintering procedure and clinical adjustment on color stability and translucency of translucent zirconia. J. Prosthet. Dent. 2020, 124, 788.e1–788.e9. [Google Scholar] [CrossRef] [PubMed]


| Group (n = 20) | Crown Color Shade | Ti-Base Abutment Height |
|---|---|---|
| A | A0/1 | 3.5 |
| B | 5.5 | |
| C | A2/3 | 3.5 |
| D | 5.5 | |
| E | A3.5/A4 | 3.5 |
| F | 5.5 | |
| G | B2/3 | 3.5 |
| H | 5.5 |
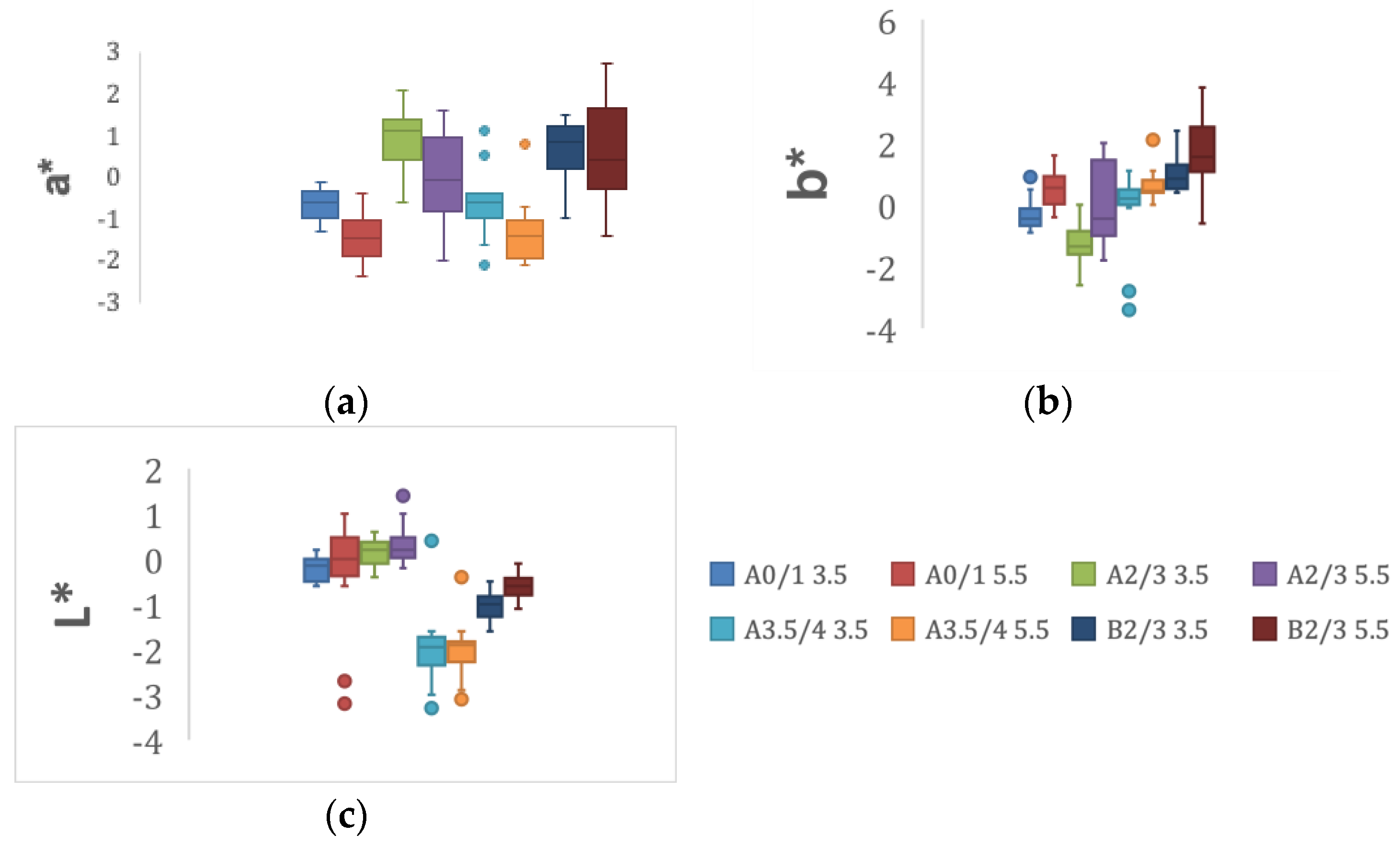
| Color Group/Abutment Height | L* | a* | b* |
|---|---|---|---|
| A 0/1 | |||
| 3.5 mm | −0.25 (0.27) | −0.64 (0.38) | −0.34 (0.45) |
| 5.5 mm | −0.16 (1.05) | −1.38 (0.60) | 0.47 (0.55) |
| A 2/3 | |||
| 3.5 mm | 0.12 (0.28) | 0.88 (0.72) | −1.30 (0.63) |
| 5.5 mm | 0.29 (0.38) | 0.04 (0.97) | 0.09 (1.26) |
| A 3.5/4 | |||
| 3.5 mm | −2.00 (0.73) | −0.59 (0.83) | −0.005 (1.11) |
| 5.5 mm | −2.02 (0.54) | −1.36 (0.67) | 0.60 (0.45) |
| B 2/3 | |||
| 3.5 mm | −1.04 (0.32) | 0.60 (0.77) | 1.03 (0.59) |
| 5.5 mm | −0.61 (0.23) | 0.54 (1.13) | 1.72 (1.12) |
| Dependent Variable: | |||||
|---|---|---|---|---|---|
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
| Corrected Model | 4.025 a | 7 | 0.575 | 3.349 | 0.002 |
| Intercept | 266.501 | 1 | 266.501 | 1551.878 | 0.000 |
| COLOR | 0.632 | 3 | 0.211 | 1.227 | 0.302 |
| HT | 1.398 | 1 | 1.398 | 8.142 | 0.005 |
| COLOR * HT | 1.995 | 3 | 0.665 | 3.873 | 0.011 |
| Error | 26.103 | 152 | 0.172 | ||
| Total | 296.629 | 160 | |||
| Corrected Total | 30.128 | 159 |
| ΔL* | Δa* | Δb* | ΔE CIE76* | ΔE CIEDE2000 | ||
|---|---|---|---|---|---|---|
| Color group | Abutment height | |||||
| A0/1 | 3.5 | 0.22450 | 0.48050 | 0.47850 | 0.96 ± 0.51 | 1.04 ± 0.61 |
| 5.5 | 2.02450 | 1.49700 | 2.25750 | 2.52 ± 0.65 | 2.18 ± 1.00 | |
| p value | 0.01 | 0.005 | 0.002 | 0.001 | <0.001 | |
| A2/3 | 3.5 | 0.37700 | 1.12500 | 1.01750 | 1.40 ± 0.75 | 1.57 ± 0.91 |
| 5.5 | 0.70600 | 1.90900 | 3.19800 | 2.23 ± 0.92 | 2.47 ± 1.02 | |
| p value | 0.155 | 0.074 | 0.003 | 0.003 | 0.004 | |
| A3.5/4 | 3.5 | 0.65200 | 1.24850 | 2.78950 | 1.82 ± 1.20 | 1.90 ± 1.28 |
| 5.5 | 1.21400 | 2.00900 | 3.75850 | 2.04 ± 1.71 | 2.15 ± 1.77 | |
| p value | 0.198 | 0.291 | 0.600 | 0.965 | 0.799 | |
| B2/3 | 3.5 | 0.25000 | 1.38150 | 2.94000 | 1.73 ± 1.27 | 1.91 ± 1.42 |
| 5.5 | 0.07700 | 1.03550 | 1.13200 | 1.34 ± 0.66 | 1.58 ± 0.79 | |
| p value | 0.004 | 0.578 | 0.096 | 0.393 | 0.465 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biadsee, A.; Özcan, M.; Masarwa, L.; Haddad, M.; Al-Haj Husain, N.; Ormianer, Z. Effect of Titanium-Base Abutment Height on Optical Properties of Monolithic Anterior Zirconia Crowns. Materials 2022, 15, 7643. https://doi.org/10.3390/ma15217643
Biadsee A, Özcan M, Masarwa L, Haddad M, Al-Haj Husain N, Ormianer Z. Effect of Titanium-Base Abutment Height on Optical Properties of Monolithic Anterior Zirconia Crowns. Materials. 2022; 15(21):7643. https://doi.org/10.3390/ma15217643
Chicago/Turabian StyleBiadsee, Ameer, Mutlu Özcan, Lubaba Masarwa, Mishel Haddad, Nadin Al-Haj Husain, and Zeev Ormianer. 2022. "Effect of Titanium-Base Abutment Height on Optical Properties of Monolithic Anterior Zirconia Crowns" Materials 15, no. 21: 7643. https://doi.org/10.3390/ma15217643
APA StyleBiadsee, A., Özcan, M., Masarwa, L., Haddad, M., Al-Haj Husain, N., & Ormianer, Z. (2022). Effect of Titanium-Base Abutment Height on Optical Properties of Monolithic Anterior Zirconia Crowns. Materials, 15(21), 7643. https://doi.org/10.3390/ma15217643








