Micromorphology of the Adhesive Interface of Self-Adhesive Resin Cements to Enamel and Dentin
Abstract
1. Introduction
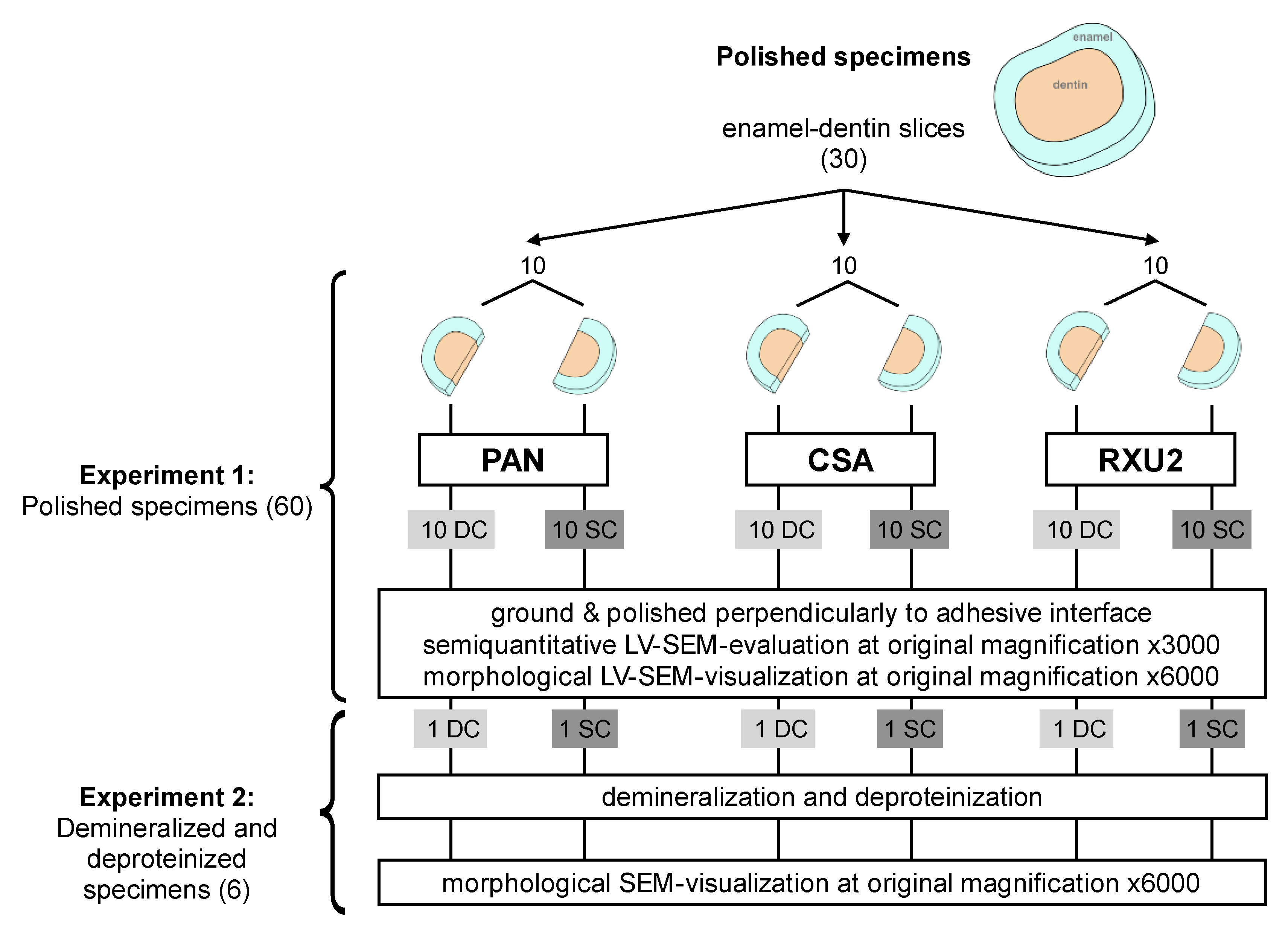
2. Materials and Methods
2.1. Specimen Selection
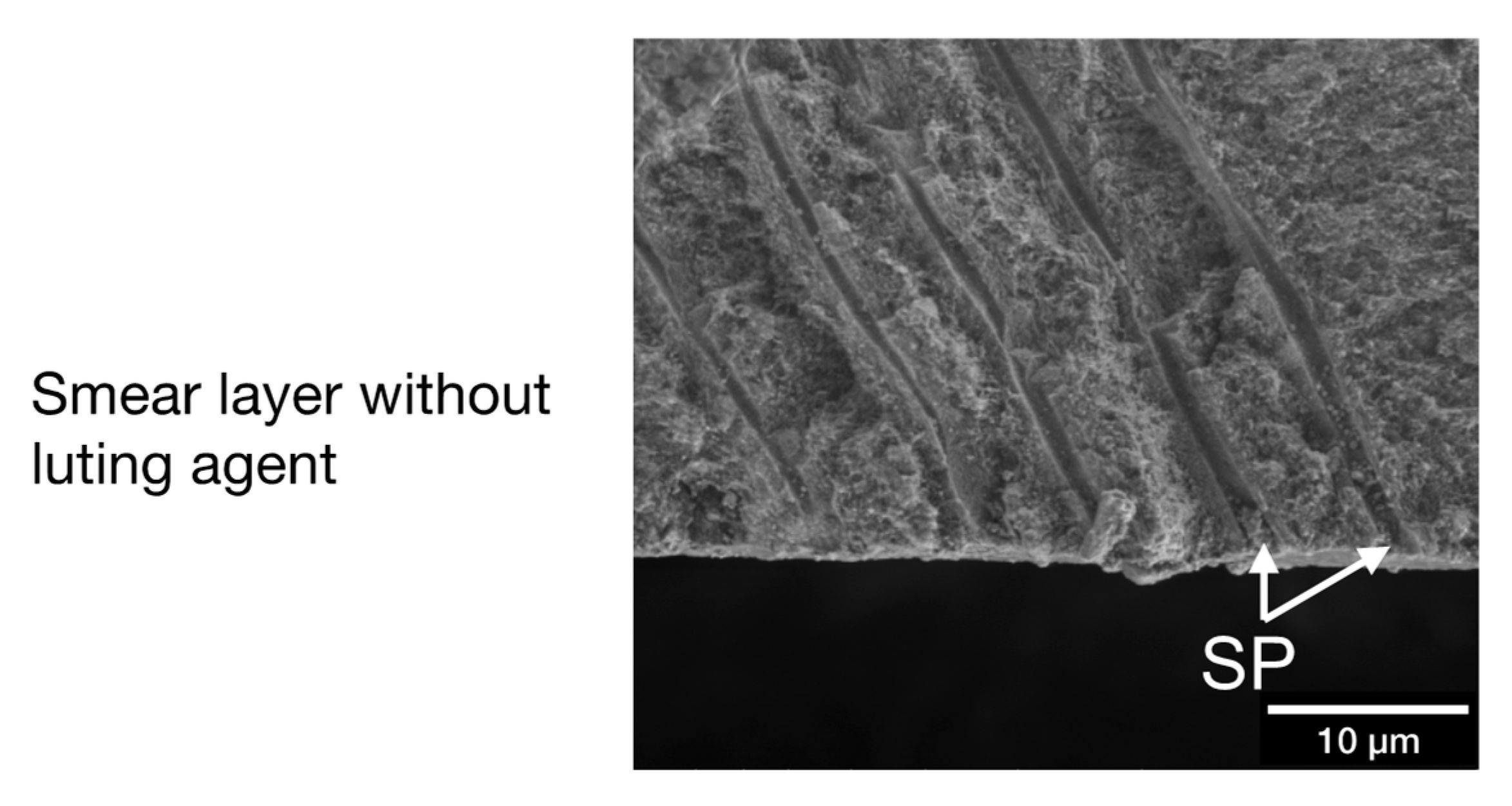
2.2. Smear Layer Creation and Measurement on Fractured Specimens
2.3. LV-SEM Smear Layer Examination of Fractured Specimens
2.4. Luting Agents and Curing Modes
Experiment 1: Semiquantitative Analyses of the Polished Interface
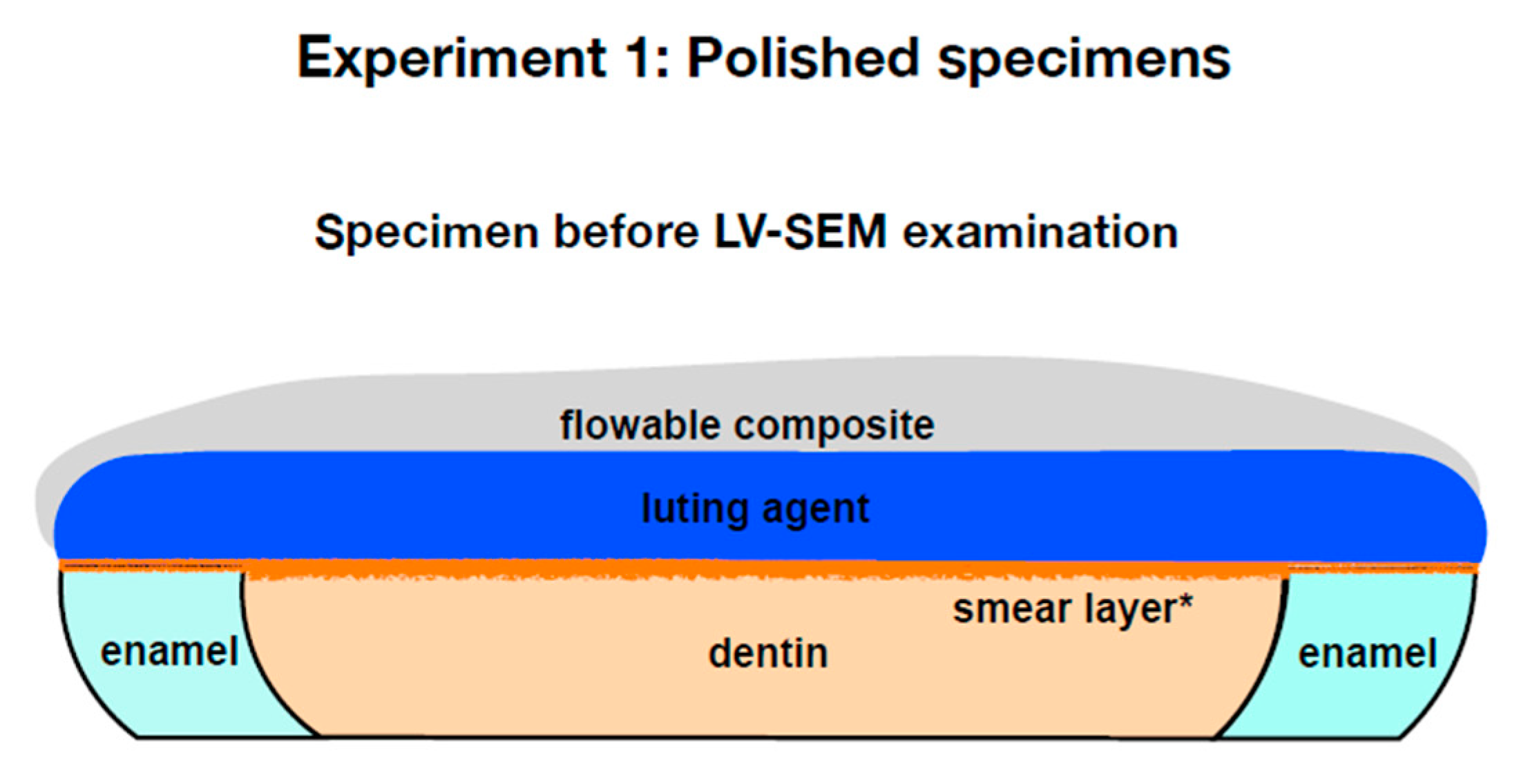
2.5. LV-SEM of Polished Specimens (Experiment 1)
Experiment 2: Morphological Analysis of the Polished Interface after Demineralization and Deproteinization
2.6. LV-SEM of Demineralized and Deproteinized Specimens (Experiment 2)
2.7. Data Analysis
3. Results
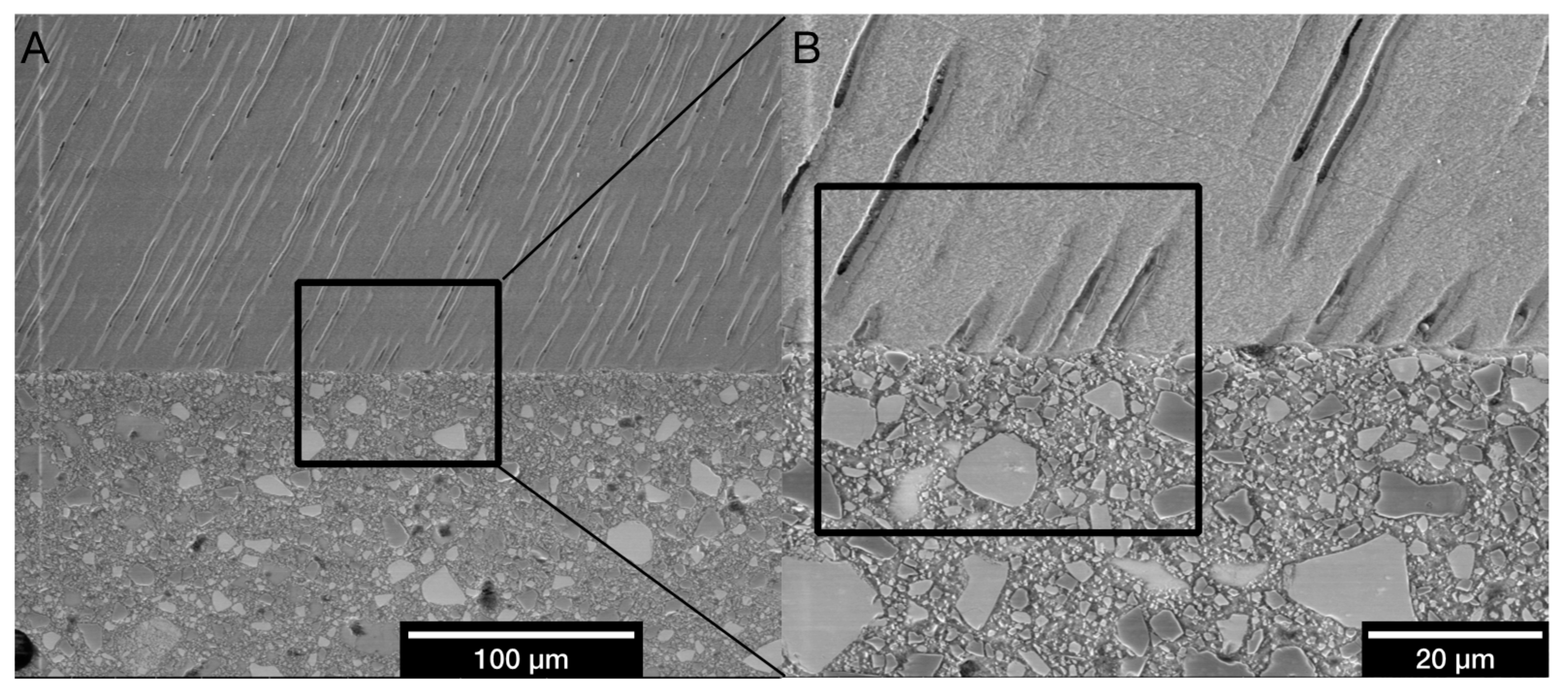
3.1. Measurement of Smear Layer Thickness Using Fractured Specimens
3.2. Micromorphological Interactions
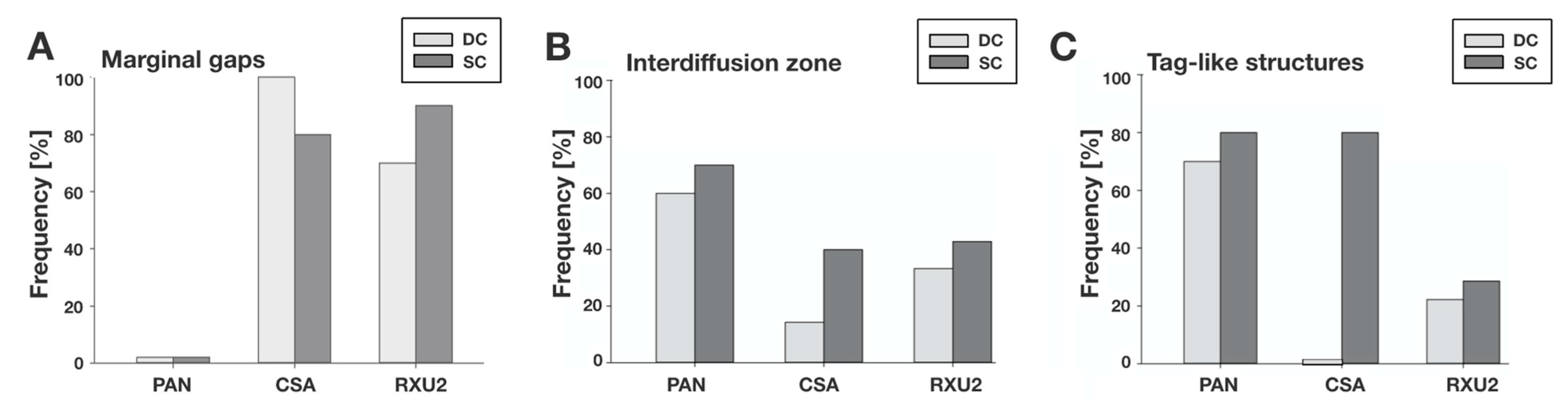
3.2.1. Experiment 1: Semiquantitative Evaluation of Polished Specimens
3.2.2. Experiment 2: Demineralized and Deproteinized Specimens, Morphological Characteristics
4. Discussion
4.1. Discussion of the Method
4.1.1. LV-SEM
4.1.2. Smear Layer Creation
4.1.3. Seating Pressure
4.2. Discussion of the Results
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Piemjai, M.; Nakabayashi, N. Direct Tensile Strength and Characteristics of Dentin Restored with All-Ceramic, Resin-Composite, and Cast Metal Prostheses Cemented with Resin Adhesives. BioMed. Res. Int. 2015, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J. Dent. Res. 2018, 97, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Brondani, L.P.; Pereira-Cecni, T.; Wandsher, V.F.; Pereira, G.K.; Valandro, L.F.; Bergoli, C.D. Longevity of metal-ceramic crowns cemented with self-adhesive resin cement: A prospective clinical study. Braz. Oral. Res. 2017, 31, 716. [Google Scholar] [CrossRef] [PubMed]
- Rauch, A.; Reich, S.; Dalchau, L.; Schierz, O. Clinical survival of chair-side generated monolithic lithium disilicate crowns: 10-year results. Clin. Oral Investig. 2017, 22, 1763–1769. [Google Scholar] [CrossRef]
- Manso, A.P.; Carvalho, R.M. Dental Cements for Luting and Bonding Restorations: Self-Adhesive Resin Cements. Dent. Clin. North. Am. 2017, 61, 821–834. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Stansbury, J.W.; Burke, F.J.T. Self-adhesive resin cements - chemistry, properties and clinical considerations. J. Oral. Rehabil. 2010, 38, 295–314. [Google Scholar] [CrossRef]
- Miotti, L.L.; Follak, A.C.; Montagner, A.F.; Pozzobon, R.T.; Da Silveira, B.L.; Susin, A.H. Is Conventional Resin Cement Adhesive Performance to Dentin Better Than Self-adhesive? A Systematic Review and Meta-Analysis of Laboratory Studies. Oper. Dent. 2020, 45, 484–495. [Google Scholar] [CrossRef]
- Brännström, M.; Johnson, G. Effects of various conditioners and cleaning agents on prepared dentin surfaces: A scanning electron microscopic investigation. J. Prosthet. Dent. 1974, 31, 422–430. [Google Scholar] [CrossRef]
- Pashley, D.H. Smear Layer: Removal and Bonding Considerations. Oper. Dent. Suppl. 1984, 3, 13–29. [Google Scholar]
- Mine, A.; De Munck, J.; Cardoso, M.V.; Van Landuyt, K.; Poitevin, A.; Kuboki, T.; Yoshida, Y.; Suzuki, K.; Van Meerbeek, B. Enamel-Smear Compromises Bonding by Mild Self-Etch Adhesives. J. Dent Res. 2010, 89, 1505–1509. [Google Scholar] [CrossRef]
- Mine, A.; De Munck, J.; Cardoso, M.V.; Van Landuyt, K.L.; Poitevin, A.; Van Ende, A.; Matsumoto, M.; Yoshida, Y.; Kuboki, T.; Yatani, H.; et al. Dentin-smear remains at self-etch adhesive interface. Dent. Mater. 2014, 30, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Suyama, Y.; De Munck, J.; Cardoso, M.V.; Yamada, T.; Van Meerbeek, B. Bond durability of self-adhesive composite cements to dentine. J. Dent. 2013, 41, 908–917. [Google Scholar] [CrossRef] [PubMed]
- Latta, M.A.; Radniecki, S.M. Bond Strength of Self-Adhesive Restorative Materials Affected by Smear Layer Thickness but not Dentin Desiccation. J. Adhes. Dent. 2020, 22, 79–84. [Google Scholar]
- Semeraro, S.; Mezzanzanica, D.; Spreafico, D.; Gagliani, M.; Re, D.; Tanaka, T.; Sidhu, S.K.; Sano, H. Effect of Different Bur Grinding on the Bond Strength of Self–etching Adhesives. Oper. Dent. 2006, 31, 317–323. [Google Scholar] [CrossRef]
- Ermis, R.B.; De Munck, J.; Cardoso, M.V.; Coutinho, E.; Van Landuyt, K.L.; Poitevin, A.; Laumbrechts, P.; Van Meerbeek, B. Bond strength of self-etch adhesives to dentin prepared with three different diamond burs. Dent. Mater. 2008, 24, 978–985. [Google Scholar] [CrossRef]
- Armstrong, S.; Breschi, L.; Özcan, M.; Pfefferkorn, F.; Ferrari, M.; Van Meerbeek, B. Academy of Dental Materials guidance on in vitro testing of dental composite bonding effectiveness to dentin/enamel using micro-tensile bond strength (μTBS) approach. Dent. Mater. 2017, 33, 133–143. [Google Scholar] [CrossRef]
- Joy, D.C.; Joy, C.S. Low voltage scanning electron microscopy. Micron 1996, 27, 247–263. [Google Scholar] [CrossRef]
- Pawley, J. Low voltage scanning electron microscopy. J. Microsc. 1984, 136, 45–68. [Google Scholar] [CrossRef]
- Turp, V.; Sen, D.; Tuncell, B.; Oezcan, M. Adhesion of 10-MDP containing resin cements to dentin with and without the etch-and-rinse technique. J. Adv. Prosthodont. 2013, 5, 226–233. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Inokoshi, S.; Braem, M.; Lambrechts, P.; Vanherle, G. Morphological aspects of the resin-dentin interdiffusion zone with different dentin adhesive systems. J. Dent. Res. 1992, 71, 1530–1540. [Google Scholar] [CrossRef]
- Goracci, C.; Cury, A.H.; Cantoro, A.; Papacchini, F.; Tay, F.R.; Ferrari, M. Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J. Adhes. Dent. 2006, 8, 327–335. [Google Scholar] [PubMed]
- De Munck, J.; Vargas, M.; Van Landuyt, K.; Hikita, K.; Lambrechts, P.; Van Meerbeek, B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater. 2004, 20, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Vargas, M.; Inoue, S.; Yoshida, Y.; Perdigão, J.; Lambrechts, P.; Guido, V. Microscopy investigations. Techniques, results, limitations. Am. J. Dent. 2000, 13, 3D–18D. [Google Scholar] [PubMed]
- Aschenbrenner, C.M.; Lang, R.; Handel, G.; Behr, M. Analysis of marginal adaptation and sealing to enamel and dentin of four self-adhesive resin cements. Clin. Oral. Invest. 2012, 16, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.N.D.B.; Daleprane, B.; Barbosa, P.F.; Moreira, A.N.; De Magalhães, C.S. Qualitative Evaluation of Scanning Electron Microscopy Methods in a Study of the Resin Cement/Dentine Adhesive Interface. Microsc. Microanal. 2014, 20, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Aguiar, T.R.; Vermelho, P.M.; André, C.B.; Giannini, M. Interfacial ultramorphology evaluation of resin luting cements to dentin: A correlative scanning electron microscopy and transmission electron microscopy analysis. Microsc. Res. Tech. 2013, 76, 1234–1239. [Google Scholar] [CrossRef]
- Oliveira, S.S.A.; Pugach, M.K.; Hilton, J.F.; Watanabe, L.G.; Marshall, S.J.; Marshall, G.W. The influence of the dentin smear layer on adhesion: A self-etching primer vs. a total-etch system. Dent. Mater. 2003, 19, 758–867. [Google Scholar] [CrossRef]
- El-Guindy, J.; Selim, M.; El-Agroudi, M. Alternative Pretreatment Modalities with a Self-Adhesive System to Promote Dentin/Alloy Shear Bond Strength. J. Prosthodont. 2010, 19, 205–211. [Google Scholar] [CrossRef]
- Radovic, I.; Monticelli, F.; Goracci, C.; Vulicevic, Z.R.; Ferrari, M. Self-adhesive resin cements: A literature review. J. Adhes. Dent. 2008, 10, 251–258. [Google Scholar]
- Temel, U.B.; Van Ende, A.; Van Meerbeek, B.; Ermis, R.B. Bond strength and cement-tooth interfacial characterization of self-adhesive composite cements. Am. J. Dent. 2017, 30, 205–211. [Google Scholar]
- Abo-Hamar, S.; Federlin, M.; Hiller, K.; Friedl, K.; Schmalz, G. Effect of temporary cements on the bond strength of ceramic luted to dentin. Dent. Mater. 2005, 21, 794–803. [Google Scholar] [CrossRef] [PubMed]
- Zortuk, M.; Bolpaca, P.; Kilic, K.; Ozdemir, E.; Aguloglu, S. Effects of Finger Pressure Applied by Dentists during Cementation of All-Ceramic Crowns. Eur. J. Dent. 2010, 4, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Shinya, A.; Gomi, H.; Shinya, A. Bonding of self-adhesive resin cements to enamel using different surface treatments: Bond strength and etching pattern evaluations. Dent. Mater. J. 2010, 29, 425–432. [Google Scholar] [CrossRef][Green Version]
- Baader, K.; Hiller, K.; Buchalla, W.; Schmalz, G.; Federlin, M. Self-adhesive Luting of Partial Ceramic Crowns: Selective Enamel Etching Leads to Higher Survival after 6.5 Years In Vivo. J. Adhes. Dent. 2016, 18, 69–79. [Google Scholar] [PubMed]
- Mazzitelli, C.; Monticelli, F.; Osorio, R.; Casucci, A.; Toledano, M.; Ferrari, M. Effect of simulated pulpal pressure on self-adhesive cements bonding to dentin. Dent. Mater. 2008, 24, 1156–1163. [Google Scholar] [CrossRef] [PubMed]
- Risnes, S.; Li, C. Aspects of the final phase of enamel formation as evidenced by observations of superficial enamel of human third molars using scanning electron microscopy. Arch. Oral. Biol. 2018, 86, 72–79. [Google Scholar] [CrossRef]
- Shafiei, F.; Kamran, S.; Memarpour, M.; Aghaei, T. Bond strength and adhesive interfacial micromorphology of self-adhesive resin cements: Effect of reduced times of pre-etching. J. Clin. Exp. Dent. 2019, 11, e984–e990. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; De Munck, J.; Yoshida, Y.; Inoue, S.; Vargas, M.; Vijay, P.; Van Landuyt, K.; Lambrechts, P.; Vanherle, G. Buonocore Memorial Lecture-Adhesion to enamel and dentin: Current status and future challenges. Oper. Dent. 2003, 28, 215–235. [Google Scholar]
- Tay, F.R.; Kwong, S.M.; Itthagarun, A.; King, N.M.; Yip, H.K.; Moulding, K.M.; Keith, M.; Pashley, D.H. Bonding of a self-etching primer to non-carious cervical sclerotic dentin: Interfacial ultrastructure and microtensile bond strength evaluation. J. Adhes. Dent. 2000, 2, 9–28. [Google Scholar]
- Burey, A.; Reis dos, P.J.; Vicentin, B.L.S.; Garbelini, C.C.D.; Hoeppner, M.G.; Appoloni, C.R. Polymerization shrinkage and porosity profile of dual cure dental resin cements with different adhesion to dentin mechanisms. Microsc. Res. Tech. 2018, 81, 88–96. [Google Scholar] [CrossRef]


| Material | LOT-No. | Ingredients |
|---|---|---|
| Panavia F 2.0 (PAN) | 041304 | PAN Paste A: 10-methacryloyloxydecyl dihydrogen phosphate, hydrophobic aromatic dimethacrylate, hydrophobic aliphatic dimethacrylate, hydrophilic aliphatic dimethacrylate, silanized glass powder, silanated colloidal silica, di-camphorquinone, catalysts, initiators PAN Paste B: hydrophobic aromatic dimethacrylate, hydrophobic aliphatic dimethacrylate, hydrophilic aliphatic dimethacrylate, Silanated barium glass filler, catalysts, accelerators, pigments, sodium fluoride ED Primer Liquid A: 2-hydroxyethyl methacrylate, 10-methacryloyloxydecyl dihydrogen phosphate, N-methacryloyl-5-aminosalicylic acid, water, accelerators ED Primer Liquid B: N-methacryloyl-5-aminosalicylic acid, water, catalysts, accelerators |
| Clearfil SA Cement (CSA) | 023AAB | Silanated barium glass filler, silanated colloidal silica, hydrophilic aliphatic dimethacrylates, triethylene glycol dimethacrylate, bisphenol A-glycidyl methacrylate, catalysts, initiators, di-camphorquinone, 10-methacryloyloxydecyl dihydrogen phosphate, pigments |
| RelyX Unicem 2 (RXU2) | 404603 | Silanized glass powder, silane treated silica, 1,12-dodecanedimethacrylate substituted dimethacrylate, methacrylated aliphatic amine, 2,6-di-tert-butyl-p-cresol, sodium P-toluenesulfinate, calcium hydroxyde, barbituric acid derivate, titanium oxide, sodium fluoride |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scholz, K.J.; Bittner, A.; Cieplik, F.; Hiller, K.-A.; Schmalz, G.; Buchalla, W.; Federlin, M. Micromorphology of the Adhesive Interface of Self-Adhesive Resin Cements to Enamel and Dentin. Materials 2021, 14, 492. https://doi.org/10.3390/ma14030492
Scholz KJ, Bittner A, Cieplik F, Hiller K-A, Schmalz G, Buchalla W, Federlin M. Micromorphology of the Adhesive Interface of Self-Adhesive Resin Cements to Enamel and Dentin. Materials. 2021; 14(3):492. https://doi.org/10.3390/ma14030492
Chicago/Turabian StyleScholz, Konstantin Johannes, Aleksandra Bittner, Fabian Cieplik, Karl-Anton Hiller, Gottfried Schmalz, Wolfgang Buchalla, and Marianne Federlin. 2021. "Micromorphology of the Adhesive Interface of Self-Adhesive Resin Cements to Enamel and Dentin" Materials 14, no. 3: 492. https://doi.org/10.3390/ma14030492
APA StyleScholz, K. J., Bittner, A., Cieplik, F., Hiller, K.-A., Schmalz, G., Buchalla, W., & Federlin, M. (2021). Micromorphology of the Adhesive Interface of Self-Adhesive Resin Cements to Enamel and Dentin. Materials, 14(3), 492. https://doi.org/10.3390/ma14030492






