Biological Characteristics and Odontogenic Differentiation Effects of Calcium Silicate-Based Pulp Capping Materials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Preparation
2.2. Preparation of Various Direct Pulp Capping Material Eluates
2.3. Cell Proliferation Evaluation
2.4. Cell Morphology Evaluation
2.5. Cell Viability Evaluation
2.6. Alkaline Phosphatase Enzyme Activity Evaluation
2.7. Quantitative Real-Time Polymerase Chain Reaction Evaluation of Odontogenic Potential
2.8. Statistical Analyses
3. Results
3.1. Cell Proliferation Evaluation
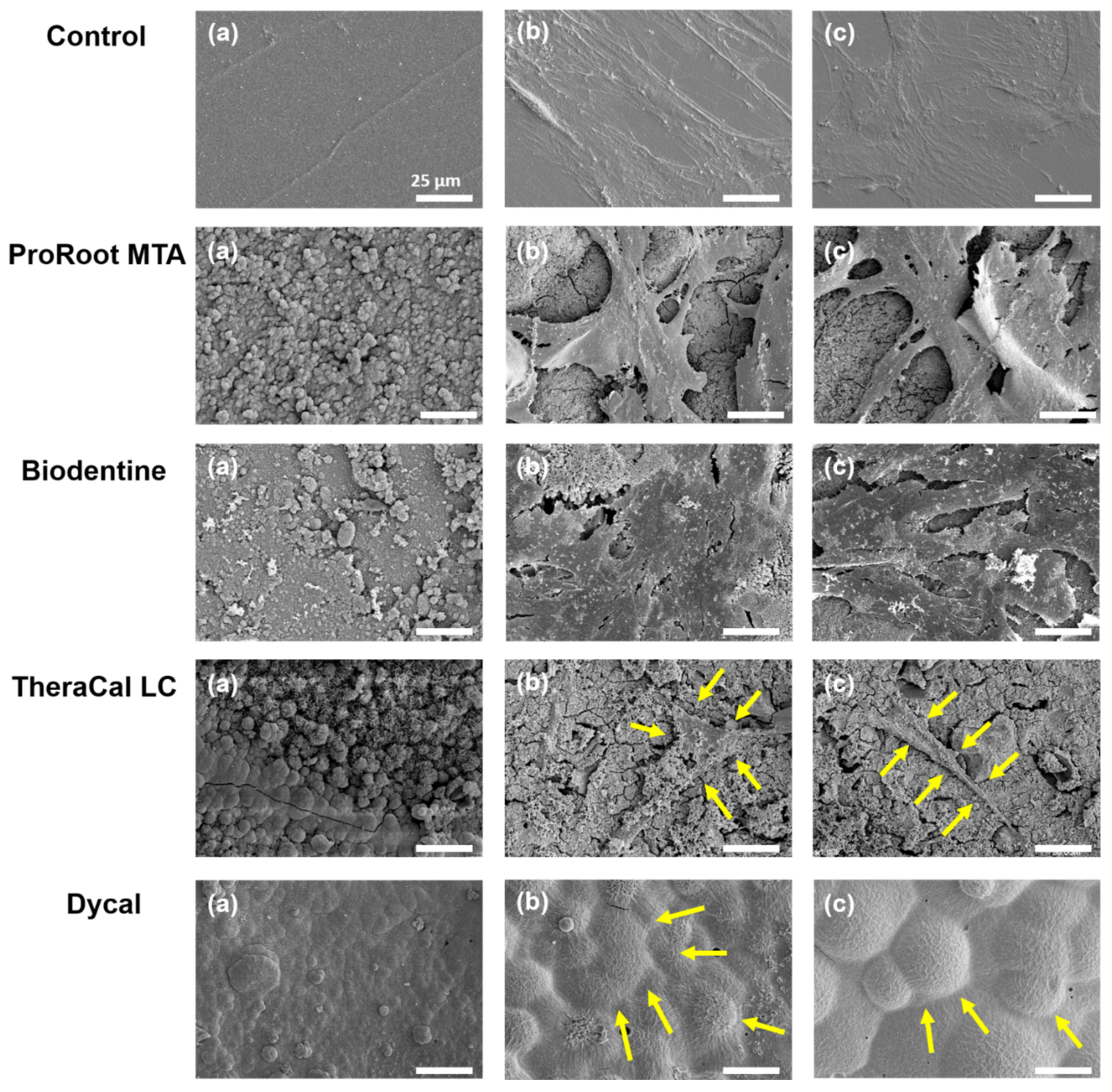
3.2. Cell Morphology Evaluation
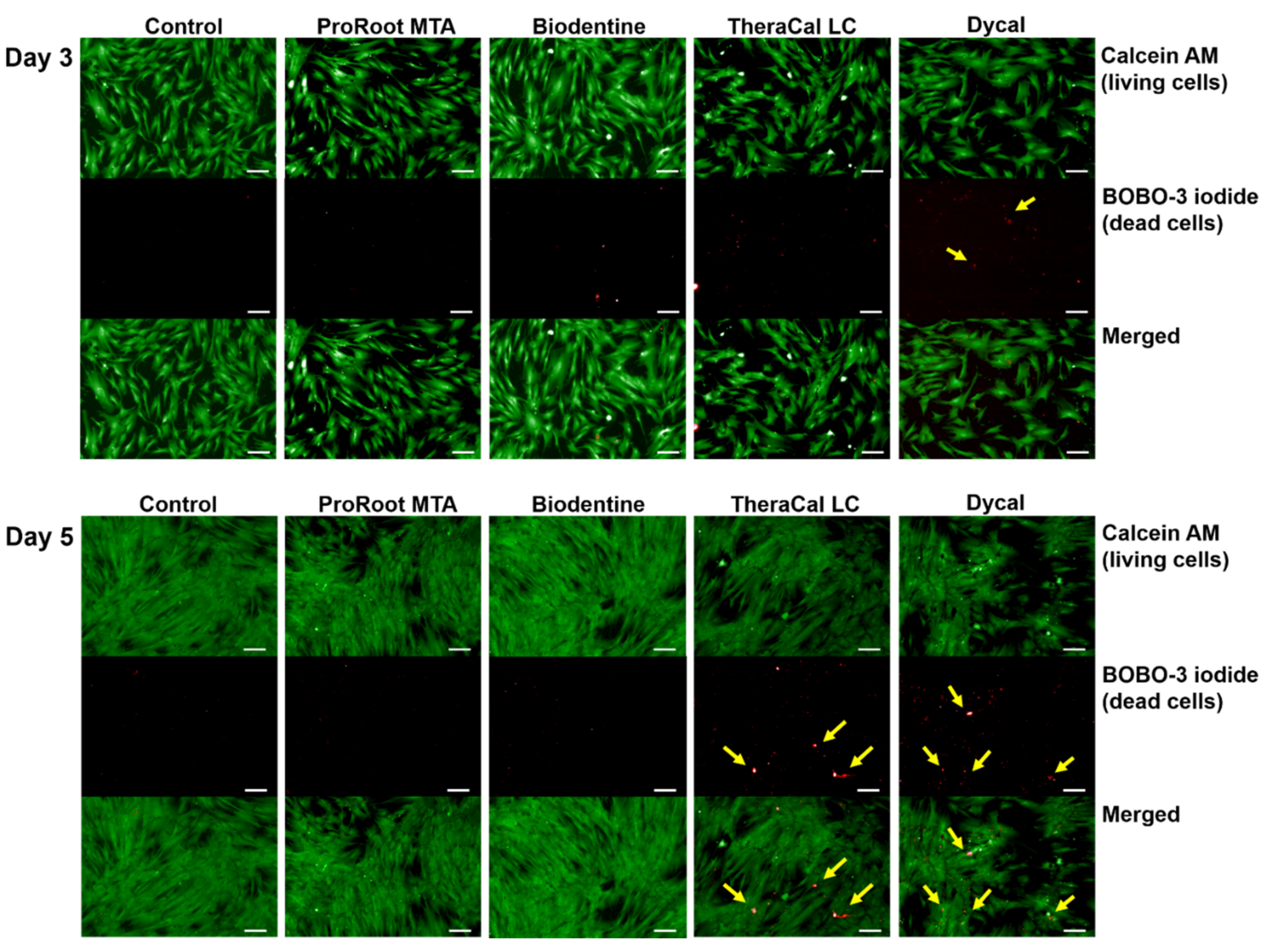
3.3. Cell Viability Evaluation
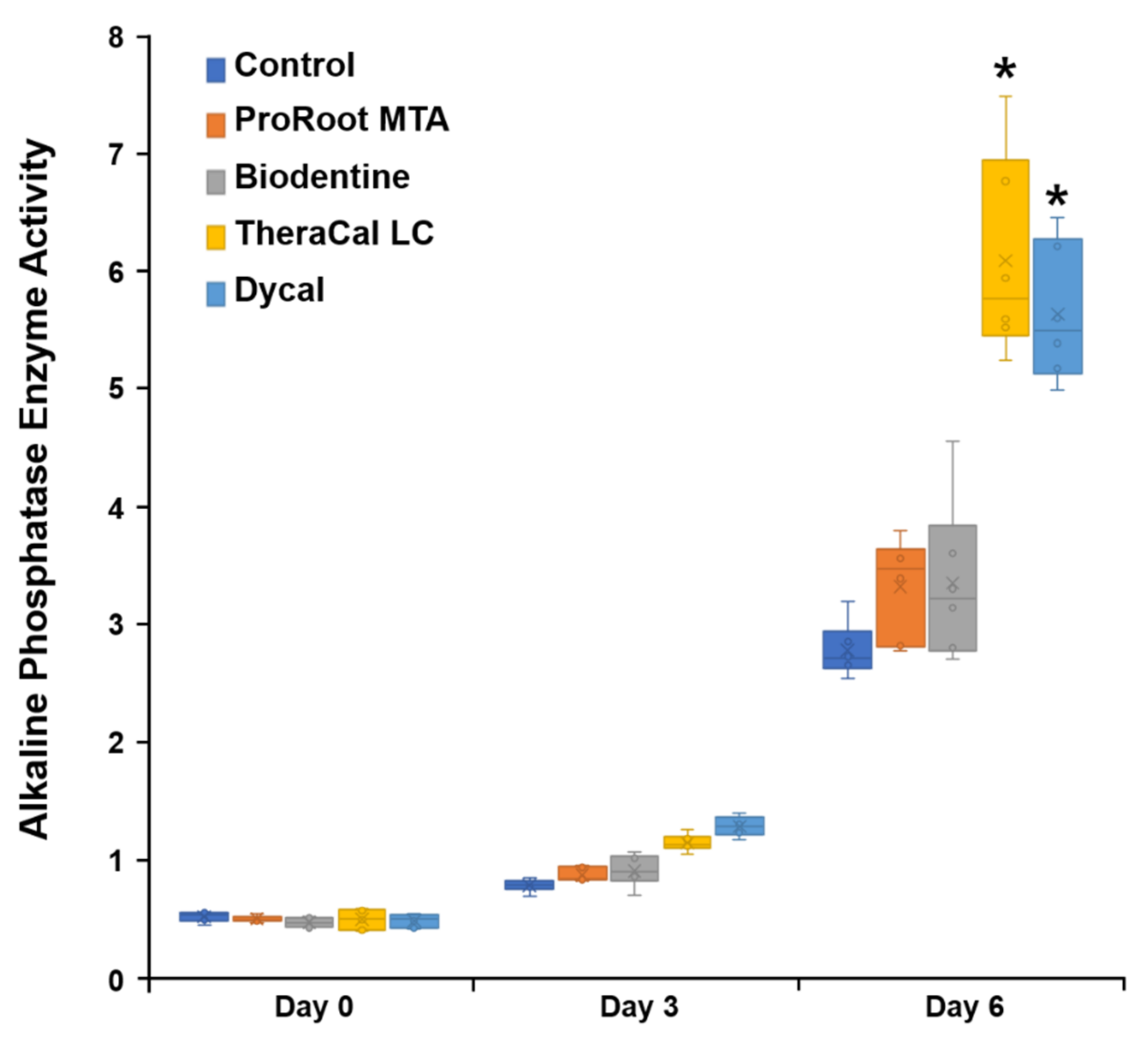
3.4. ALP Enzyme Activity Evaluation
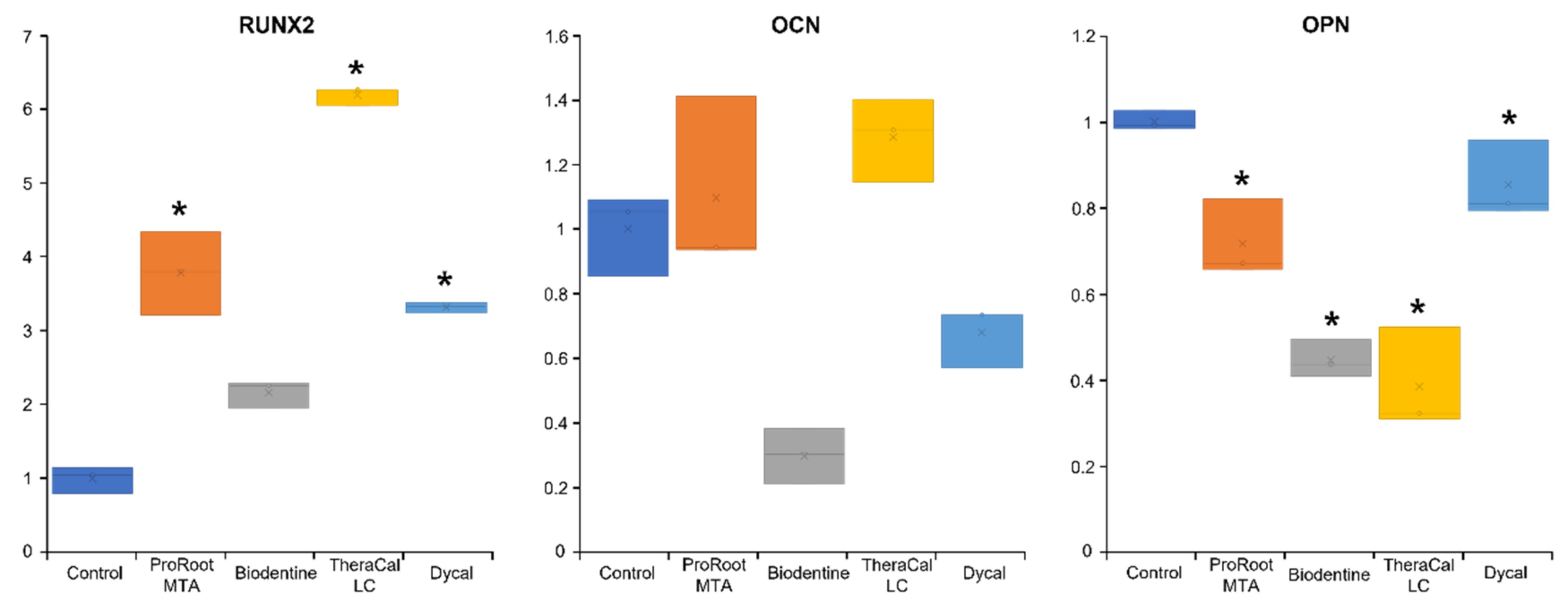
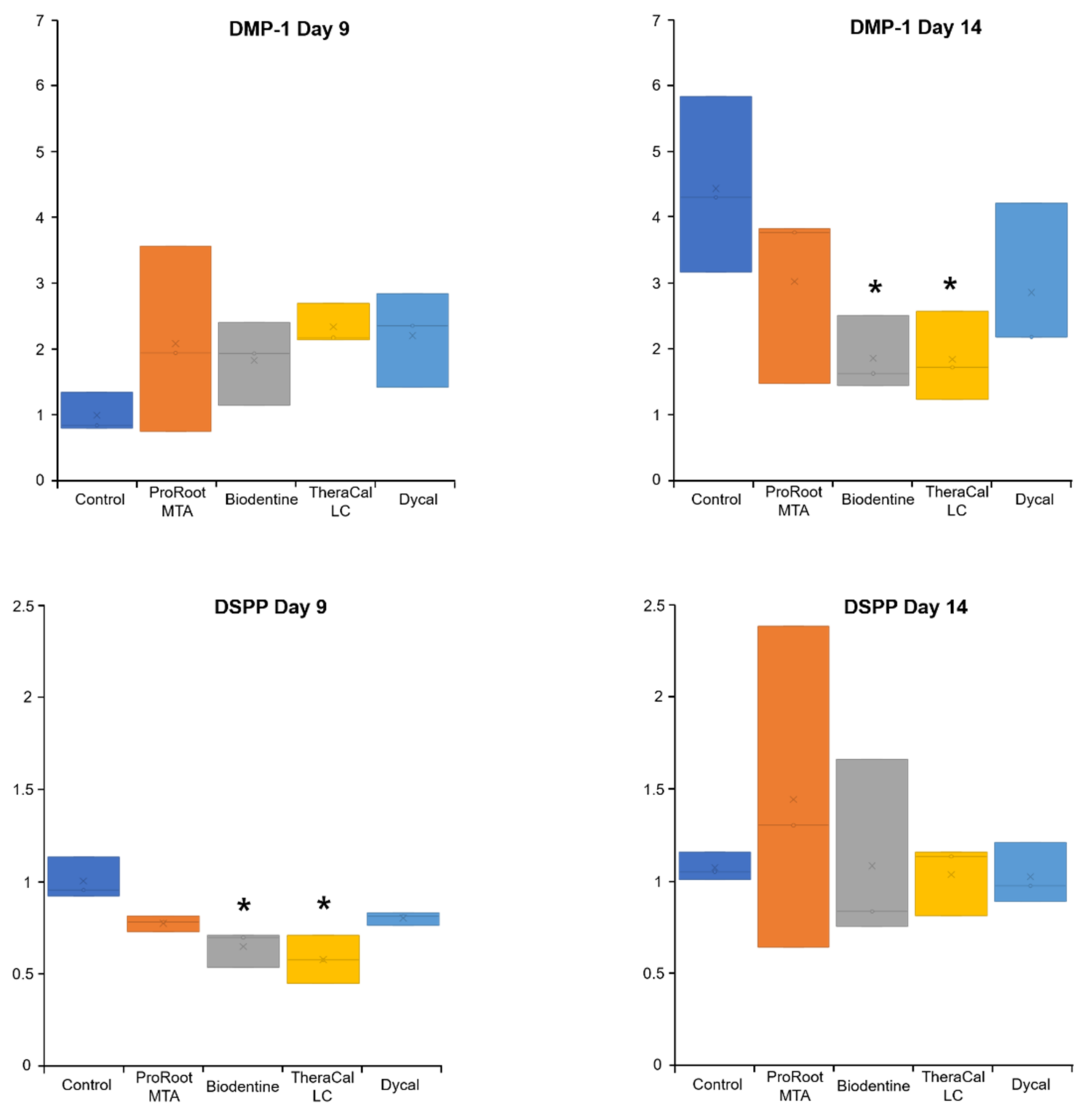
3.5. qPCR Evaluation of Odontogenic Potential
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, L.; Suh, B.I. Cytotoxicity and biocompatibility of resin-free and resin-modified direct pulp capping materials: A state-of-the-art review. Dent. Mater. J. 2017, 36, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Yu, F.; Dong, Y.; Yang, Y.W.; Lin, P.T.; Yu, H.H.; Sun, X.; Sun, X.F.; Zhou, H.; Huang, L.; Chen, J.H. Effect of an Experimental Direct Pulp-capping Material on the Properties and Osteogenic Differentiation of Human Dental Pulp Stem Cells. Sci. Rep. 2016, 6, 34713. [Google Scholar] [CrossRef]
- Komabayashi, T.; Zhu, Q.; Eberhart, R.; Imai, Y. Current status of direct pulp-capping materials for permanent teeth. Dent. Mater. J. 2016, 35, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Kitasako, Y.; Ikeda, M.; Tagami, J. Pulpal responses to bacterial contamination following dentin bridging beneath hard-setting calcium hydroxide and self-etching adhesive resin system. Dent. Traumatol. 2008, 24, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Parirokh, M. Mineral trioxide aggregate: A comprehensive literature review—Part II: Leakage and biocompatibility investigations. J. Endod. 2010, 36, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part III: Clinical applications, drawbacks, and mechanism of action. J. Endod. 2010, 36, 400–413. [Google Scholar] [CrossRef]
- Cho, S.Y.; Seo, D.G.; Lee, S.J.; Lee, J.; Lee, S.J.; Jung, I.Y. Prognostic factors for clinical outcomes according to time after direct pulp capping. J. Endod. 2013, 39, 327–331. [Google Scholar] [CrossRef]
- Mente, J.; Hufnagel, S.; Leo, M.; Michel, A.; Gehrig, H.; Panagidis, D.; Saure, D.; Pfefferle, T. Treatment outcome of mineral trioxide aggregate or calcium hydroxide direct pulp capping: Long-term results. J. Endod. 2014, 40, 1746–1751. [Google Scholar] [CrossRef] [PubMed]
- Caliskan, M.K.; Guneri, P. Prognostic factors in direct pulp capping with mineral trioxide aggregate or calcium hydroxide: 2- to 6-year follow-up. Clin. Oral Investig. 2017, 21, 357–367. [Google Scholar] [CrossRef]
- Brizuela, C.; Ormeño, A.; Cabrera, C.; Cabezas, R.; Silva, C.I.; Ramírez, V.; Mercade, M. Direct Pulp Capping with Calcium Hydroxide, Mineral Trioxide Aggregate, and Biodentine in Permanent Young Teeth with Caries: A Randomized Clinical Trial. J. Endod. 2017, 43, 1776–1780. [Google Scholar] [CrossRef]
- Parinyaprom, N.; Nirunsittirat, A.; Chuveera, P.; Na Lampang, S.; Srisuwan, T.; Sastraruji, T.; Bua-On, P.; Simprasert, S.; Khoipanich, I.; Sutharaphan, T.; et al. Outcomes of Direct Pulp Capping by Using Either ProRoot Mineral Trioxide Aggregate or Biodentine in Permanent Teeth with Carious Pulp Exposure in 6- to 18-Year-Old Patients: A Randomized Controlled Trial. J. Endod. 2018, 44, 341–348. [Google Scholar] [CrossRef]
- Katge, F.A.; Patil, D.P. Comparative Analysis of 2 Calcium Silicate-based Cements (Biodentine and Mineral Trioxide Aggregate) as Direct Pulp-capping Agent in Young Permanent Molars: A Split Mouth Study. J. Endod. 2017, 43, 507–513. [Google Scholar] [CrossRef]
- Paula, A.; Carrilho, E.; Laranjo, M.; Abrantes, A.M.; Casalta-Lopes, J.; Botelho, M.F.; Marto, C.M.; Ferreira, M.M. Direct Pulp Capping: Which is the Most Effective Biomaterial? A Retrospective Clinical Study. Materials 2019, 12, 3382. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, M.J.; Casey, J.A.; VanderWeele, R.A.; Vandewalle, K.S. Mechanical properties of new dental pulp-capping materials. Gen. Dent. 2016, 64, 44–48. [Google Scholar] [PubMed]
- Gandolfi, M.G.; Siboni, F.; Prati, C. Chemical-physical properties of TheraCal, a novel light-curable MTA-like material for pulp capping. Int. Endod. J. 2012, 45, 571–579. [Google Scholar] [CrossRef]
- Bortoluzzi, E.A.; Niu, L.N.; Palani, C.D.; El-Awady, A.R.; Hammond, B.D.; Pei, D.D.; Tian, F.C.; Cutler, C.W.; Pashley, D.H.; Tay, F.R. Cytotoxicity and osteogenic potential of silicate calcium cements as potential protective materials for pulpal revascularization. Dent. Mater. 2015, 31, 1510–1522. [Google Scholar] [CrossRef] [Green Version]
- Bakhtiar, H.; Nekoofar, M.H.; Aminishakib, P.; Abedi, F.; Naghi Moosavi, F.; Esnaashari, E.; Azizi, A.; Esmailian, S.; Ellini, M.R.; Mesgarzadeh, V.; et al. Human Pulp Responses to Partial Pulpotomy Treatment with TheraCal as Compared with Biodentine and ProRoot MTA: A Clinical Trial. J. Endod. 2017, 43, 1786–1791. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, D.; Song, D.; Kim, H.M.; Kim, S.Y. Biocompatibility and Bioactivity of Set Direct Pulp Capping Materials on Human Dental Pulp Stem Cells. Materials 2020, 13, 3925. [Google Scholar] [CrossRef]
- Kunert, M.; Lukomska-Szymanska, M. Bio-Inductive Materials in Direct and Indirect Pulp Capping-A Review Article. Materials 2020, 13, 1204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seo, D.G.; Lee, D.; Kim, Y.M.; Song, D.; Kim, S.Y. Biocompatibility and Mineralization Activity of Three Calcium Silicate-Based Root Canal Sealers Compared to Conventional Resin-Based Sealer in Human Dental Pulp Stem Cells. Materials 2019, 12, 2482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranjkesh, B.; Isidor, F.; Kraft, D.C.E.; Lovschall, H. In vitro cytotoxic evaluation of novel fast-setting calcium silicate cement compositions and dental materials using colorimetric methyl-thiazolyl-tetrazolium assay. J. Oral. Sci. 2018, 60, 82–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirschman, W.R.; Wheater, M.A.; Bringas, J.S.; Hoen, M.M. Cytotoxicity comparison of three current direct pulp-capping agents with a new bioceramic root repair putty. J. Endod. 2012, 38, 385–388. [Google Scholar] [CrossRef]
- Giraud, T.; Jeanneau, C.; Rombouts, C.; Bakhtiar, H.; Laurent, P.; About, I. Pulp capping materials modulate the balance between inflammation and regeneration. Dent. Mater. 2019, 35, 24–35. [Google Scholar] [CrossRef] [Green Version]
- Jeanneau, C.; Laurent, P.; Rombouts, C.; Giraud, T.; About, I. Light-cured Tricalcium Silicate Toxicity to the Dental Pulp. J. Endod. 2017, 43, 2074–2080. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, J. Hydration characteristics of Biodentine and Theracal used as pulp capping materials. Dent. Mater. 2014, 30, 709–715. [Google Scholar] [CrossRef]
- Lipski, M.; Nowicka, A.; Kot, K.; Postek-Stefańska, L.; Wysoczańska-Jankowicz, I.; Borkowski, L.; Andersz, P.; Jarząbek, A.; Grocholewicz, K.; Sobolewska, E.; et al. Factors affecting the outcomes of direct pulp capping using Biodentine. Clin. Oral. Investig. 2018, 22, 2021–2029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomas-Catala, C.J.; Collado-Gonzalez, M.; Garcia-Bernal, D.; Onate-Sanchez, R.E.; Forner, L.; Llena, C.; Lozano, A.; Moraleda, J.M.; Rodriguez-Lozano, F.J. Biocompatibility of New Pulp-capping Materials NeoMTA Plus, MTA Repair HP, and Biodentine on Human Dental Pulp Stem Cells. J. Endod. 2018, 44, 126–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Widbiller, M.; Lindner, S.R.; Buchalla, W.; Eidt, A.; Hiller, K.A.; Schmalz, G.; Galler, K.M. Three-dimensional culture of dental pulp stem cells in direct contact to tricalcium silicate cements. Clin. Oral Investig. 2016, 20, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, S.H.; El-Negoly, S.A.; Zaen El-Din, A.M.; El-Zekrid, M.H.; Grawish, L.M.; Grawish, H.M.; Grawish, M.E. Biodentine versus mineral trioxide aggregate as a direct pulp capping material for human mature permanent teeth—A systematic review. J. Conserv. Dent. 2018, 21, 466–473. [Google Scholar] [CrossRef]
- De Rossi, A.; Silva, L.A.; Gaton-Hernandez, P.; Sousa-Neto, M.D.; Nelson-Filho, P.; Silva, R.A.; de Queiroz, A.M. Comparison of pulpal responses to pulpotomy and pulp capping with biodentine and mineral trioxide aggregate in dogs. J. Endod. 2014, 40, 1362–1369. [Google Scholar] [CrossRef]
- Nowicka, A.; Lipski, M.; Parafiniuk, M.; Sporniak-Tutak, K.; Lichota, D.; Kosierkiewicz, A.; Kaczmarek, W.; Buczkowska-Radlinska, J. Response of human dental pulp capped with biodentine and mineral trioxide aggregate. J. Endod. 2013, 39, 743–747. [Google Scholar] [CrossRef] [PubMed]
- Prati, C.; Gandolfi, M.G. Calcium silicate bioactive cements: Biological perspectives and clinical applications. Dent. Mater. 2015, 31, 351–370. [Google Scholar] [CrossRef]
- Bielby, R.C.; Christodoulou, I.S.; Pryce, R.S.; Radford, W.J.; Hench, L.L.; Polak, J.M. Time- and concentration-dependent effects of dissolution products of 58S sol-gel bioactive glass on proliferation and differentiation of murine and human osteoblasts. Tissue Eng. 2004, 10, 1018–1026. [Google Scholar] [CrossRef]
- Mathieu, S.; Jeanneau, C.; Sheibat-Othman, N.; Kalaji, N.; Fessi, H.; About, I. Usefulness of controlled release of growth factors in investigating the early events of dentin-pulp regeneration. J. Endod. 2013, 39, 228–235. [Google Scholar] [CrossRef]
- Howard, C.; Murray, P.E.; Namerow, K.N. Dental pulp stem cell migration. J. Endod. 2010, 36, 1963–1966. [Google Scholar] [CrossRef] [PubMed]
- Bègue-Kirn, C.; Smith, A.J.; Ruch, J.V.; Wozney, J.M.; Purchio, A.; Hartmann, D.; Lesot, H. Effects of dentin proteins, transforming growth factor beta 1 (TGF beta 1) and bone morphogenetic protein 2 (BMP2) on the differentiation of odontoblast in vitro. Int. J. Dev. Biol. 1992, 36, 491–503. [Google Scholar]
- Laurent, P.; Camps, J.; About, I. Biodentine(TM) induces TGF-β1 release from human pulp cells and early dental pulp mineralization. Int. Endod. J. 2012, 45, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Hume, W.R.; Gerzina, T.M. Bioavailability of components of resin-based materials which are applied to teeth. Crit. Rev. Oral Biol. Med. 1996, 7, 172–179. [Google Scholar] [CrossRef]
- Ratanasathien, S.; Wataha, J.C.; Hanks, C.T.; Dennison, J.B. Cytotoxic interactive effects of dentin bonding components on mouse fibroblasts. J. Dent. Res. 1995, 74, 1602–1606. [Google Scholar] [CrossRef]
- Diamanti, E.; Mathieu, S.; Jeanneau, C.; Kitraki, E.; Panopoulos, P.; Spyrou, G.; About, I. Endoplasmic reticulum stress and mineralization inhibition mechanism by the resinous monomer HEMA. Int. Endod. J. 2013, 46, 160–168. [Google Scholar] [CrossRef]


| Product | Manufacturer | Components | Lot Number |
|---|---|---|---|
| ProRoot MTA | Dentsply Tulsa Dental Specialties, Tulsa, OK, USA | Portland cement (tricalcium silicate, dicalcium silicate, and tricalcium aluminate) 75%, calcium sulfate dihydrate (gypsum) 5%, Bismuth oxide 20%. | 0000186484 |
| Biodentine | Septodont, Saint- Maur-des-Fossés, France | Tricalcium silicate, dicalcium silicate, calcium carbonate, calcium oxide, and zirconium oxide, in powder form. Water, calcium chloride, and soluble polymer, in aqueous liquid form. | B24553 |
| TheraCal LC | Bisco, Schamberg, IL, USA, | Portland cement (calcium silicates), fumed silica, Bis-GMA, polyglycol dimethacrylate. | 1900004558 |
| Dycal | Dentsply Tulsa Dental, Johnson City, TN, USA | Base paste: calcium phosphate, calcium tungstate, zinc oxide, iron oxide pigments, 1,3-butylene glycol disalicylate. Catalyst paste: calcium hydroxide, zinc oxide, zinc stearate, titanium oxide, iron oxide pigments, N-ethyl-o/p-toluene sulphonamide. | 160801 |
| Gene | Primer Sequence |
|---|---|
| runt-related transcription factor 2 (Runx2) | Forward 5′-AAG TGC GGT GCA AAC TTT CT-3′ Reverse 5′-TCT CGG TGG CTG CTA GTG A-3′ |
| osteocalcin (OCN) | Forward 5′-GTG CAG AGT CCA GCA AAG GT-3′ |
| Reverse 5′-TCA GCC AAC TCG TCA CAG TC-3′ | |
| osteopontin (OPN) | Forward 5′-TGA AAC GAG TCA GCT GGA TG-3′ |
| Reverse 5′-TGA AAT TCA TGG CTG TGG AA-3 | |
| dentin matrix protein-1 (DMP-1) | Forward 5′-TGG TCC CAG CAG TGA GTC CA-3′ |
| Reverse 5′-TGT GTG CGA GCT GTC CTC CT-3′ | |
| dentin sialophosphoprotein (DSPP) | Forward 5′-GGG AAT ATT GAG GGC TGG AA-3′ |
| Reverse 5′-TCA TTG TGA CCT GCA TCG CC-3′ | |
| GAPDH | Forward 5′-TGT CAT CAA CGG GAA GCC-3′ |
| Reverse 5′-TTG TCA TGG ATG ACC TTG-3′ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.; Lee, D.; Kim, H.-M.; Kye, M.; Kim, S.-Y. Biological Characteristics and Odontogenic Differentiation Effects of Calcium Silicate-Based Pulp Capping Materials. Materials 2021, 14, 4661. https://doi.org/10.3390/ma14164661
Kim Y, Lee D, Kim H-M, Kye M, Kim S-Y. Biological Characteristics and Odontogenic Differentiation Effects of Calcium Silicate-Based Pulp Capping Materials. Materials. 2021; 14(16):4661. https://doi.org/10.3390/ma14164661
Chicago/Turabian StyleKim, Yemi, Donghee Lee, Hye-Min Kim, Minjoo Kye, and Sin-Young Kim. 2021. "Biological Characteristics and Odontogenic Differentiation Effects of Calcium Silicate-Based Pulp Capping Materials" Materials 14, no. 16: 4661. https://doi.org/10.3390/ma14164661
APA StyleKim, Y., Lee, D., Kim, H.-M., Kye, M., & Kim, S.-Y. (2021). Biological Characteristics and Odontogenic Differentiation Effects of Calcium Silicate-Based Pulp Capping Materials. Materials, 14(16), 4661. https://doi.org/10.3390/ma14164661







