Mechanical Properties of Dental Alloys According to Manufacturing Process
Abstract
1. Introduction
2. Materials and Methods
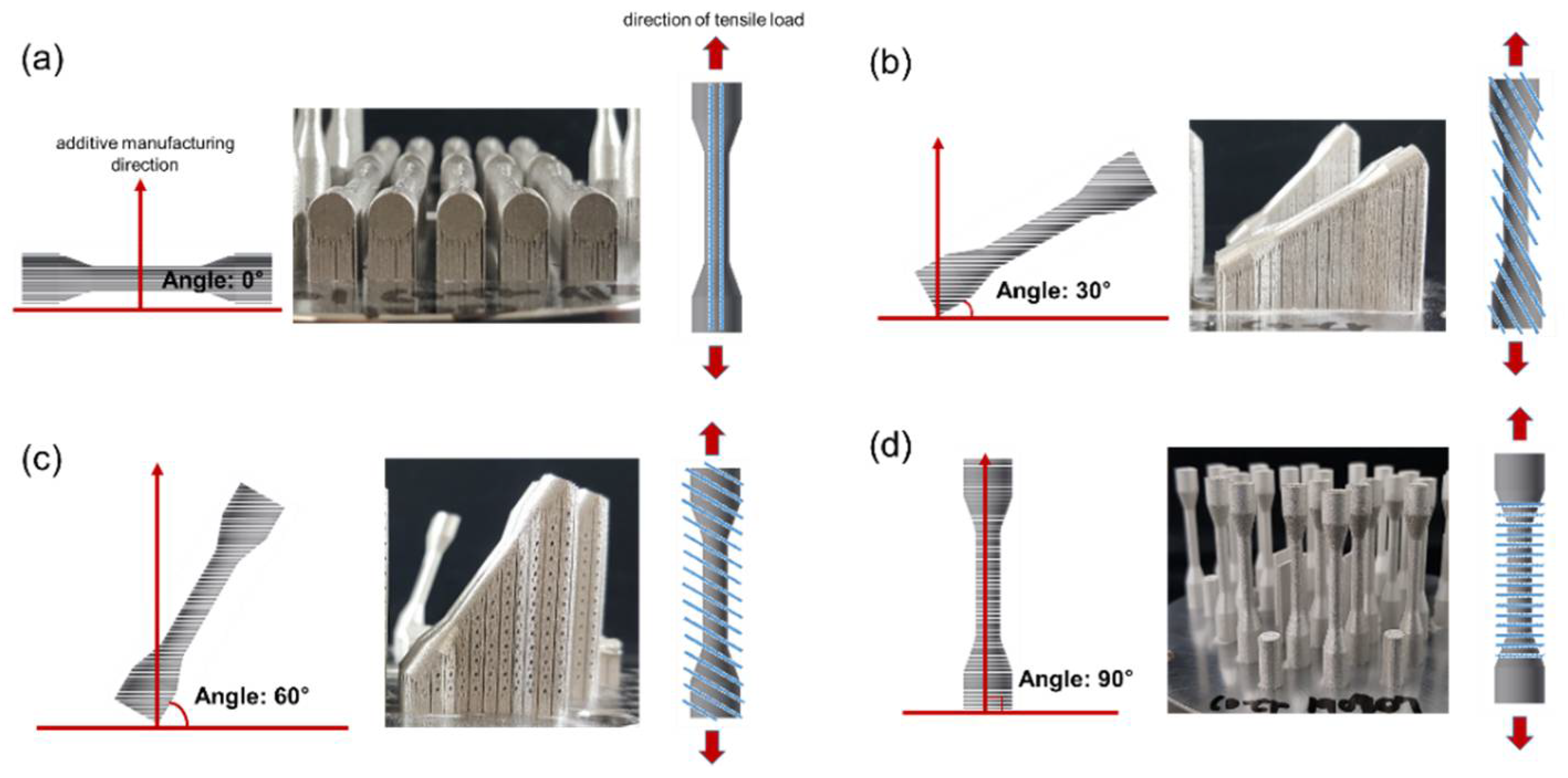
2.1. Specimen Production
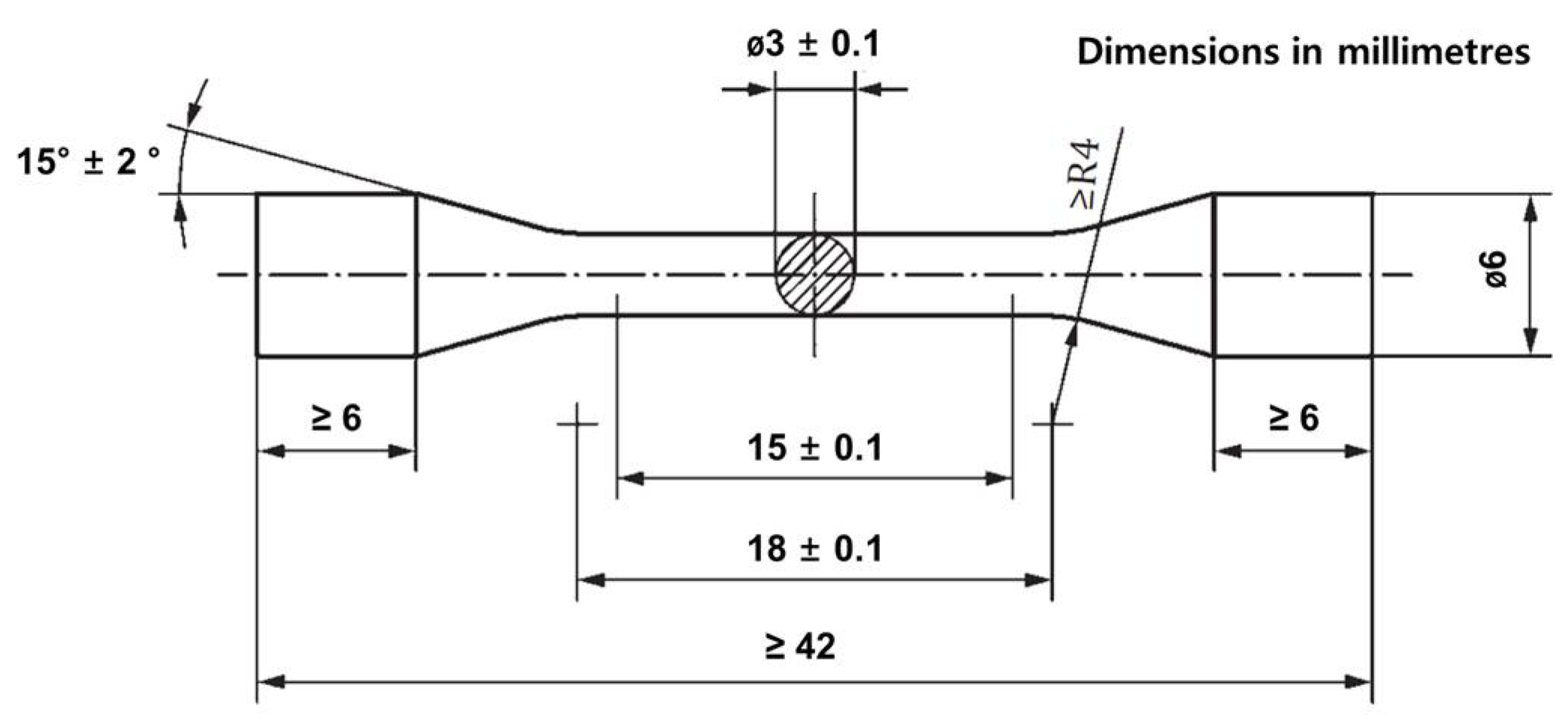
2.2. Mechanical Properties Test
Modulus of Elasticity Using Tensile Strain Method
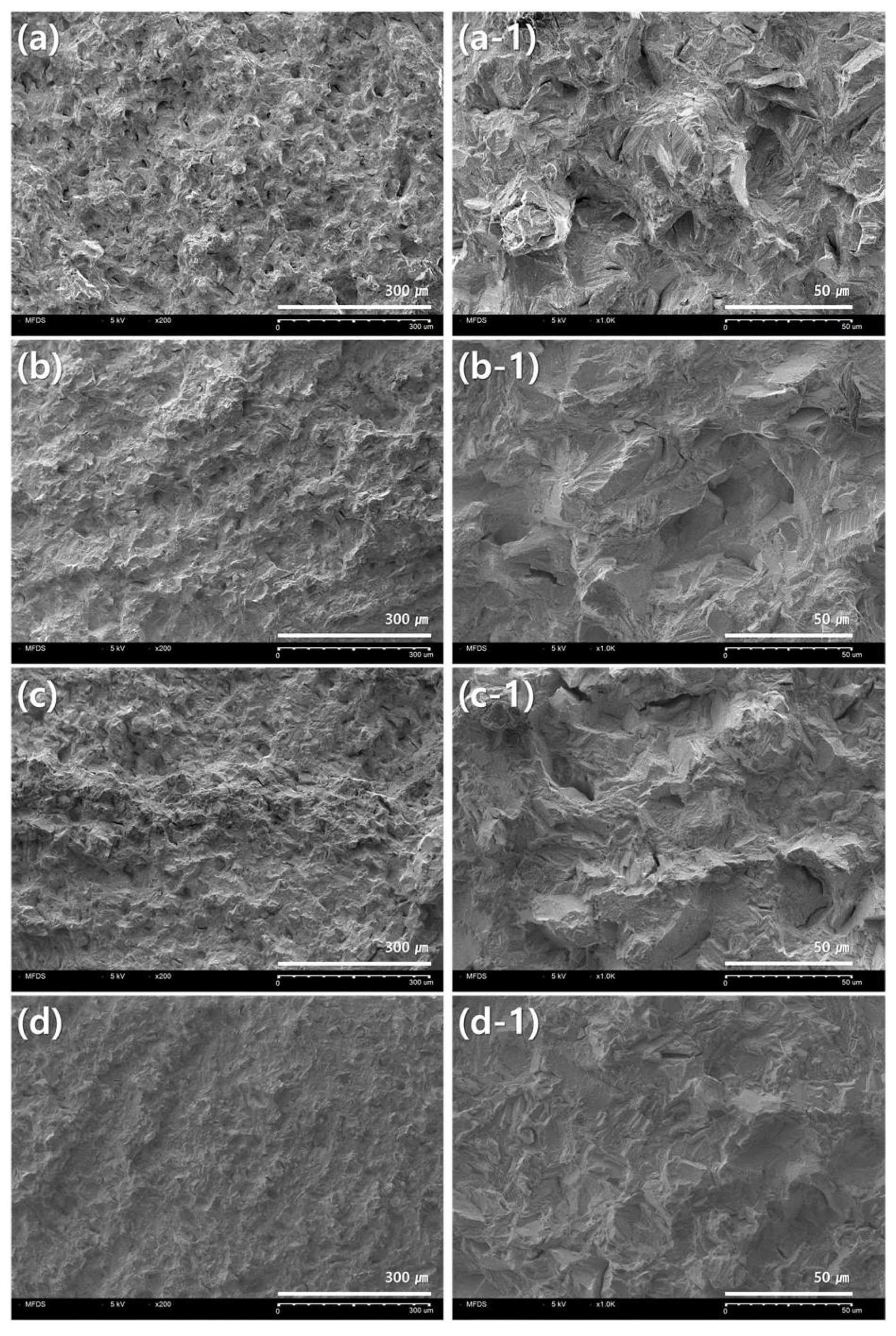
2.3. Observation of Fracture Surface and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bea, S.Y.; Park, J.Y.; Kim, J.H.; Kim, H.Y.; Kim, M.B.; Kim, W.C. The comparison of accuracy on three-unit fixed dental prosthesis made with CAD/CAM milling machines. J. Korean Acad. Dent. Technol. 2015, 37, 9–15. [Google Scholar]
- Kim, S.C.; Lee, H.H. Marginal accuracy of Three-unit bridge fabricated using dental Co-Cr CAM soft metal block. Korean J. Dent. Mater. 2016, 43, 177–184. [Google Scholar] [CrossRef]
- Kim, Y.H. A study of shrinkage and expansion for dental casting process. J. Korean Acad. Dent. Technol. 2020, 42, 107–112. [Google Scholar]
- Antanasova, M.; Kocjan, A.; Kovač, J.; Žužek, B.; Jevnikar, P. Influence of thermo-mechanical cycling on porcelain bonding to cobalt-chromium and titanim dental alloys fabricated by casting, milling and selective laser melting. J. Prosthod. Res. 2018, 62, 184–194. [Google Scholar] [CrossRef]
- Li, J.; Chen, C.; Liao, J.; Liu, L.; Ye, X.; Lin, S.; Ye, J. Bond strengths of porcelain to cobalt-chromium alloys made by casting, milling, and selective laser melting. J. Prosthet. Dent. 2016, 118, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Hitzler, L.; Alifui-Segbaya, F.; Williams, P.; Heine, B.; Heitzmann, M.; Hall, W.; Merkel, M.; Öchsner, A. Additive manufacturing of cobalt-based dental alloys: Analysis of microstructure and physicomechanical properties. Adv. Mater. Sci. Eng. 2018, 2018, 8213023. [Google Scholar] [CrossRef]
- Han, X.; Sawada, T.; Schille, C.; Schweizer, E.; Scheideler, L.; Geis-Gerstorfer, J.; Rupp, F.; Spintzuk, S. Comparative analysis of mechanical properties and metal-ceramic bond strength of Co-Cr dental alloy fabricated by different manufacturing processes. Materials 2018, 11, 1801. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive manufacturing technologies used for 3D metal printing in dentistry. Curr. Oral Health Rep. 2017, 4, 201–208. [Google Scholar] [CrossRef]
- Kim, W.S.; Kim, K.B. An evaluation of marginal and internal gap of fixed dental prostheses printed by selective laser sintering. Korean J. Dent. Mater. 2017, 44, 141–149. [Google Scholar] [CrossRef]
- Wu, L.; Zhu, H.; Gai, X.; Wang, Y. Evaluation of the mechanical properties and porcelain bond strength of cobalt-chromium dental alloy fabricated by selective laser melting. J. Prosthet. Dent. 2014, 111, 51–55. [Google Scholar] [CrossRef]
- Koutsoukis, T.; Zinelis, S.; Eliades, G.; Al-Wazzan, K.; Rifaiy, M.A.; Jabbari, Y.S.A. Selective laser melting technique of Co–Cr dental alloys: A review of structure and properties and comparative analysis with other available techniques. J. Prosthodont. 2015, 24, 303–312. [Google Scholar] [CrossRef]
- Kajima, Y.; Takaichi, A.; Nakamoto, T.; Kimura, T.; Yogo, Y.; Ashida, M.; Doi, H.; Nomura, N.; Tarahashi, H.; Hanawa, T.; et al. Fatigue strength of Co-Cr-Mo alloy clasps prepared by selective laser metling. J. Mech. Behav. Biomed. 2016, 59, 446–458. [Google Scholar] [CrossRef]
- Jang, S.H.; Min, B.K.; Hong, M.H.; Kwon, T.Y. Effect of different post-sintering temperatures on the microstructures and mechanical properties of a pre-sintered Co-Cr alloy. Metals 2018, 8, 1036. [Google Scholar] [CrossRef]
- Mergulhão, M.V.; Podestá, C.E.; Neves, M.D.M. Mechanical properties and microstructural characterization of cobalt-chromium (CoCr) obtained by casting and selective laser melting (SLM). Mater. Sci. Forum. 2017, 899, 534–539. [Google Scholar] [CrossRef]
- Mergulhão, M.V.; Neves, M.D.M. Characteristics of biometallic alloy to additive manufacturing using selective laser melting technology. J. Biomater. Nanobiotechnol. 2018, 9, 89–99. [Google Scholar] [CrossRef]
- Korean Society of Professors for Dental Materials. Korea Dental Materials Faculty Association, 8th ed.; Koonja Publisher: Yongin-si, Korea, 2020; pp. 315–337. [Google Scholar]
- Yoda, K.; Suyalatu; Takaichi, A.; Nomura, N.; Tsutsumi, Y.; Doi, H.; Kurosu, S.; Chiba, A.; Igarashi, Y.; Hanawa, T. Effects of chromium and nitrogen content on the microstructures and mechanical properties of as-cast Co-Cr-Mo alloys for dental applications. Acta Biomater. 2012, 8, 2856–2862. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Husain, M.A.H.; Nethani, M.M.; Özcan, M. Chemical composition, surface roughness, and ceramic bond strength of additively manufactured cobalt-chromium dental alloys. J. Prosthet. Dent. 2020, in press. [Google Scholar] [CrossRef]
- Kim, C.Y.; Chung, I.S. Evaluation of mechanical characteristic and biological stability of dental alloys by the manufacture method. J. Korea Contents Assoc. 2011, 11, 293–301. [Google Scholar] [CrossRef][Green Version]
- ISO 22674:2016. Dentistry—Metallic Materials for Fixed and Removable Restorations and Appliances; International Organization for Standardization: Geneva, Switzerland, 2016. [Google Scholar]
- Al Jabbari, Y.S.; Koutsoukis, T.; Barmpagadaki, X.; Zinelis, S. Metallurgical and interfacial characterization of PFM Co-Cr dental alloys fabricated via casting, milling or selective laser melting. Dent. Mater. 2014, 30, 79–88. [Google Scholar] [CrossRef]
- Liu, R.; Xi, S.Q.; Kapoor, S.; Wu, X.J. Effects of chemical composition on solidification, microstructure and hardness of Co-Cr-W-Ni and Co-Cr-Mo-Ni alloy systems. Int. J. Res. Rev. Appl. Sci. 2010, 5, 110–122. [Google Scholar]
- Dadbakhsh, S.; Hao, L. Effect of Al alloys on selective laser melting behaviour and microstructure of in situ formed particle reinforced composites. J. Alloys Comp. 2012, 541, 328–334. [Google Scholar] [CrossRef]
- Zhou, Y.; Li, N.; Yan, J.; Zeng, Q. Comparative analysis of the microstructures and mechanical properties of Co-Cr dental alloys fabricated by different methods. J. Prosthet. Dent. 2018, 120, 617–623. [Google Scholar] [CrossRef]
- Afkhami, S.; Piili, H.; Salminen, A.; Björk, T. Effective parameters on the fatigue life of metals processed by powder bed fusion technique: A short review. Procedia Manuf. 2019, 36, 3–10. [Google Scholar] [CrossRef]
- Aboulkhair, N.T.; Simonelli, M.; Parry, L.; Ashcroft, I.; Tuck, C.; Hague, R. 3D printing of aluminium alloys: Additive manufacturing of aluminium alloys using selective laser melting. Prog. Mater. Sci. 2019, 106, 100578. [Google Scholar] [CrossRef]
- Aarts, J.M.; Choi, J.J.E.; Metcalfe, S.; Bennani, V. Influence of build angulation on the mechanical properties of a direct-metal laser-sintered cobalt-chromium used for removable partial denture frameworks. J. Prosthet. Dent. 2020, in press. [Google Scholar] [CrossRef]
- Ma, P.; Prashanth, K.G.; Scudino, S.; Jia, Y.; Wang, H.; Zou, C.; Wei, Z.; Eckert, J. Influence of annealing on mechanical properties of Al-20Si processed by selective laser melting. Metals 2014, 4, 28–36. [Google Scholar] [CrossRef]
- Todaro, C.J.; Easton, M.A.; Qiu, D.; Zhang, D.; Bermingham, M.J.; Lui, E.W.; Brandt, M.; StJohn, D.H.; Qian, M. Grain structure control during metal 3D printing by high-intensity ultrasound. Nat. Commun. 2020, 11, 142. [Google Scholar] [CrossRef]
- Merdji, A.; Bouiadjra, B.B.; Chikh, B.O.; Mootanah, R.; Aminallah, L.; Serier, B.; Muslih, I.M. Stress distribution in dental prosthesis under an occlusal combined dynamic loading. Mater. Des. 2012, 36, 705–713. [Google Scholar] [CrossRef]
- Pieniak, D.; Walczak, A.; Walczak, M.; Przystupa, K.; Niewczas, A.M. Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures. Materials 2020, 13, 11255. [Google Scholar] [CrossRef]
- Scribante, A.; Vallittu, P.; Lassila, L.V.J.; Viola, A.; Tessera, P.; Gandini, P.; Sfondrini, M.F. Effect of Long-Term Brushing on Deflection, Maximum Load, and Wear of Stainless Steel Wires and Conventional and Spot Bonded Fiber-Reinforced Composites. Int. J. Mol. Sci. 2019, 20, 6043. [Google Scholar] [CrossRef] [PubMed]



| Group | Materials | Country | Composition | Manufacturer |
|---|---|---|---|---|
| Casting | Wirobond®C | Germany | Co: 63.3 wt.%, Cr: 24.8 wt.%, W: 5.3 wt.%, Mo: 5.1 wt.%, Si: 1 wt.% | Bego (Bremen) |
| Milling | Easymill | Korea | Co: >61 wt.%, Cr: >28 wt.%, Others | High dental (Gwang-ju) |
| 3D printing | Cobalt alloys | Sweden | Co: Balance, Cr: 28.7 wt.%, Mo: 6.1 wt.%, Mn: 0.69 wt.%, Si: 0.68 wt.%, C: 0.25 wt.%, Fe: 0.18 wt.%, Ni: 0.01 wt.% | SANDVIK (Stockholm) |
| Group | 0.2% Yield Strength (MPa) | Elongation (%) |
|---|---|---|
| Mean ± Standard Deviation | Mean ± Standard Deviation | |
| Casting | 501 ± 33 a | 11 ± 3 AB |
| Milling | 438 ± 15 a | 12 ± 5 B |
| 3D printing * | 1008 ± 59 * | 9 ± 2 * |
| 3D—0° | 1042 ± 102 b | 5 ± 1 C |
| 3D—30° | 1022 ± 86 b | 6 ± 1 AC |
| 3D—60° | 1002 ± 32 b | 9 ± 2 ABC |
| 3D—90° | 966 ± 47 b | 14 ± 2 B |
| Group | Yield Load (100%) | Yield Load (60%) | Yield Load (5%) | Elastic Modulus (GPa) | p-Value |
|---|---|---|---|---|---|
| Casting | 3500.45 | 2100.27 | 175.02 | 226 | p > 0.05 |
| Milling | 3152.41 | 1891.45 | 157.62 | 235 | |
| 3D—0° | 6905.63 | 4143.38 | 345.28 | 219 | |
| 3D—30° | 6760.25 | 4056.15 | 338.01 | 212 | |
| 3D—60° | 6617.40 | 3970.44 | 330.87 | 206 | |
| 3D—90° | 6387.27 | 3832.36 | 319.36 | 198 |
| Type | 0.2% Yield Strength (MPa) | Elongation (%) | Elastic Modulus (GPa) |
|---|---|---|---|
| 0 | - | - | - |
| 1 | 80 | 18 | - |
| 2 | 180 | 10 | - |
| 3 | 270 | 5 | - |
| 4 | 360 | 2 | - |
| 5 | 500 | 2 | 150 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, J.-M.; Kang, S.-Y.; Lee, J.-S.; Jeong, H.-S.; Lee, S.-Y. Mechanical Properties of Dental Alloys According to Manufacturing Process. Materials 2021, 14, 3367. https://doi.org/10.3390/ma14123367
Yu J-M, Kang S-Y, Lee J-S, Jeong H-S, Lee S-Y. Mechanical Properties of Dental Alloys According to Manufacturing Process. Materials. 2021; 14(12):3367. https://doi.org/10.3390/ma14123367
Chicago/Turabian StyleYu, Ji-Min, Seen-Young Kang, Jun-Seok Lee, Ho-Sang Jeong, and Seung-Youl Lee. 2021. "Mechanical Properties of Dental Alloys According to Manufacturing Process" Materials 14, no. 12: 3367. https://doi.org/10.3390/ma14123367
APA StyleYu, J.-M., Kang, S.-Y., Lee, J.-S., Jeong, H.-S., & Lee, S.-Y. (2021). Mechanical Properties of Dental Alloys According to Manufacturing Process. Materials, 14(12), 3367. https://doi.org/10.3390/ma14123367






