Long-Term Clinical Outcomes of Treatment with Dental Implants with Acid Etched Surface
Abstract
1. Introduction
2. Material and Methods
2.1. Sample Description
2.1.1. Recruitment
2.1.2. Demographic Description
2.1.3. Inclusion and Exclusion Criteria
2.2. Diagnosis Records
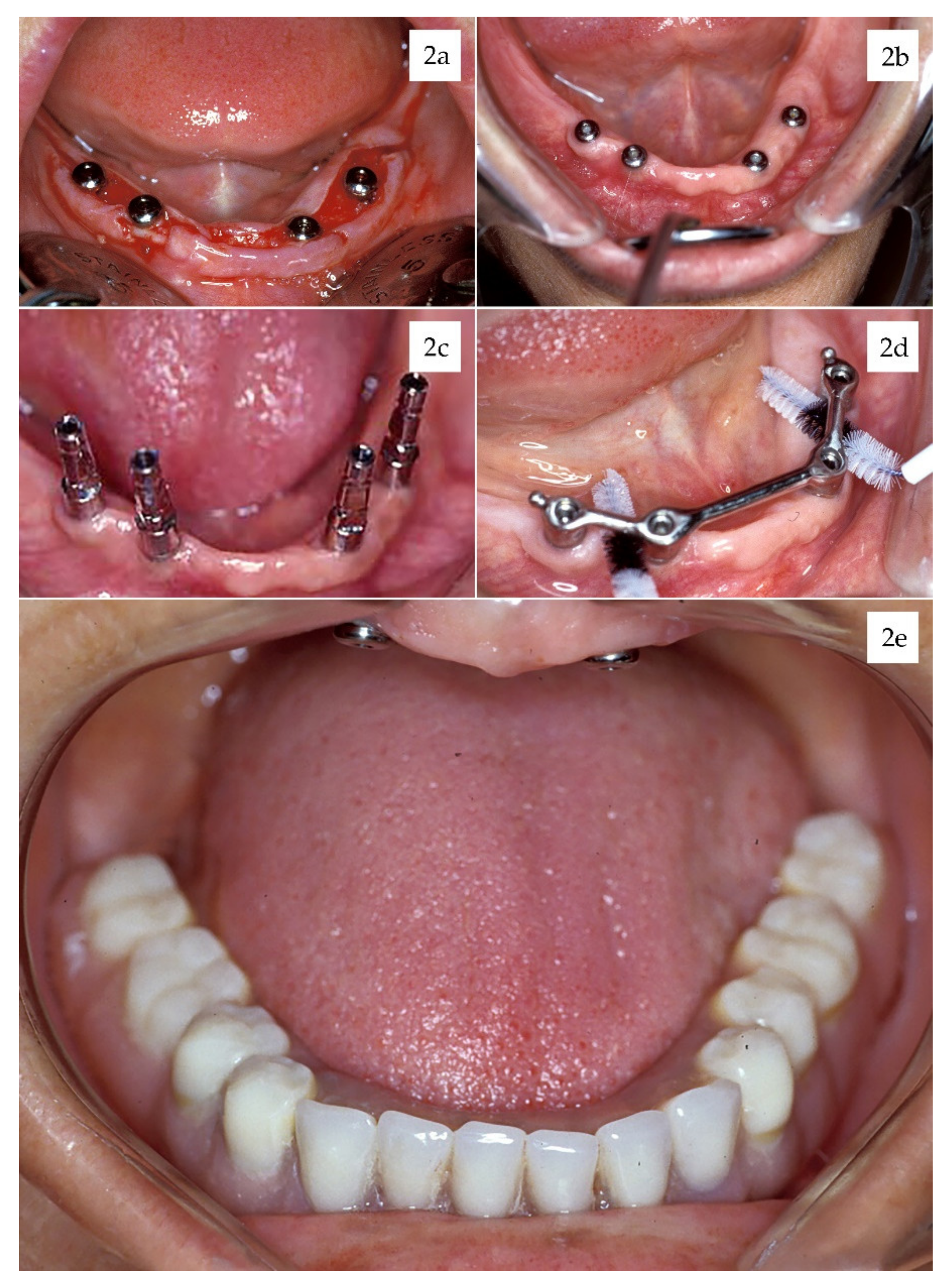
2.3. Surgery Protocol
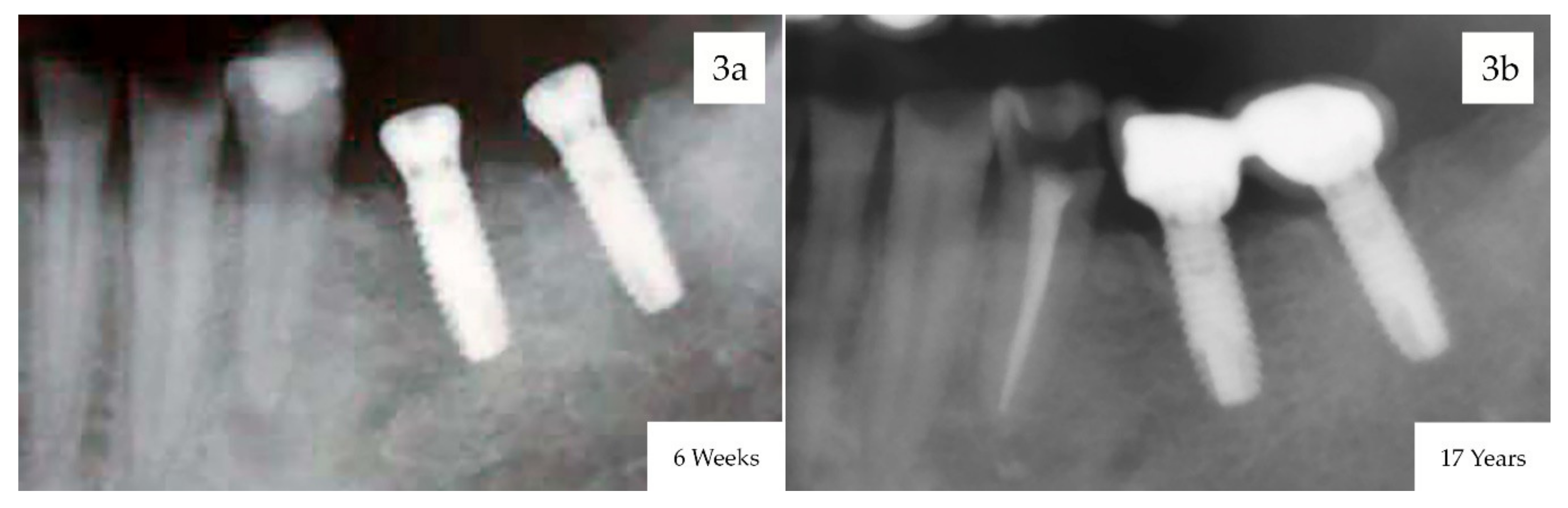
2.4. Follow-Up
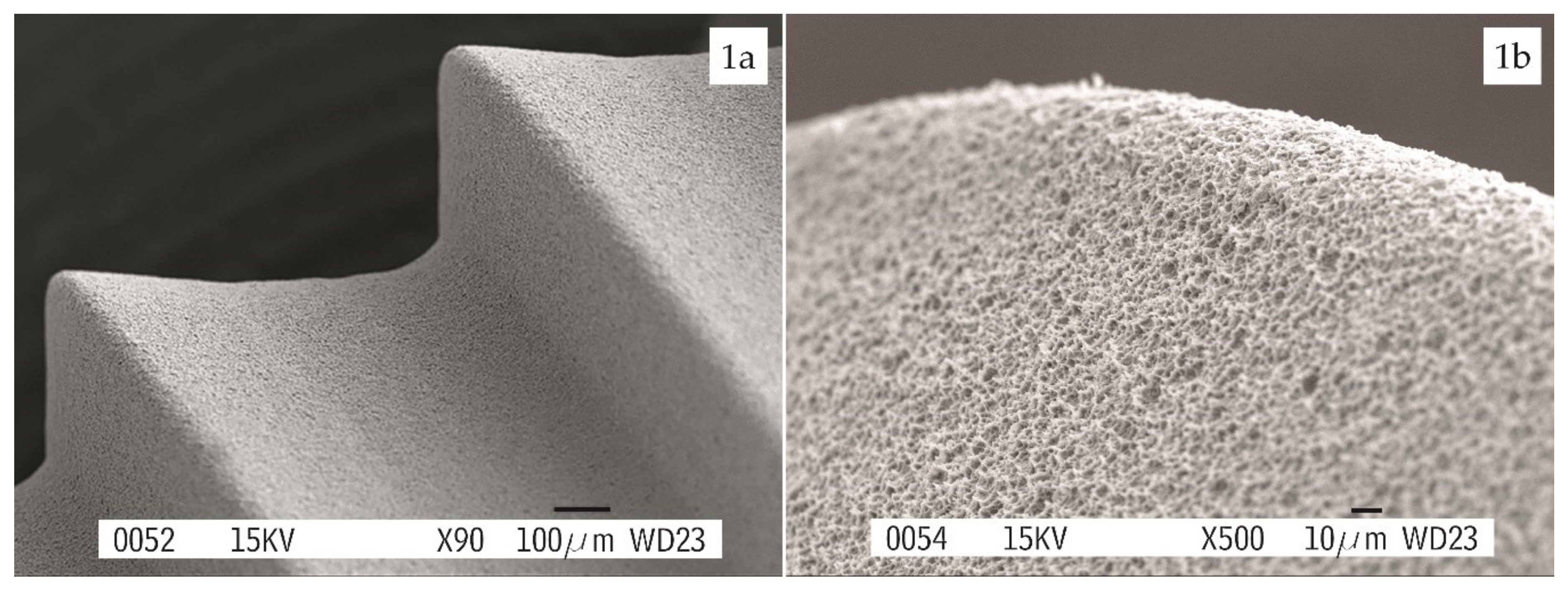
2.5. Implant Features
2.6. Success Criteria
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int J. Oral Maxillofac Implants. 1986, 1, 11–25. [Google Scholar]
- Del Fabbro, M.; Testori, T.; Kekovic, V.; Goker, F.; Tumedei, M.; Wang, H.L. Systematic review of survival rates of osseointegrated implants in fully and partially edentulous patients following immediate loading. J. Clin Med. 2019, 8, 2142. [Google Scholar] [CrossRef]
- Velasco-Ortega, E.; Ortiz-García, I.; Jiménez-Guerra, J.; Monsalve-Guil, L.; Muñoz-Guzón, F.; Perez, R.A.; Gil, F.J. Comparison between sandblasted-acid etched and oxidized titanium dental implants: In vivo study. Int J. Mol Sci. 2019, 20, 3267. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Cavalcanti de Lima, J.H.; Rodriguez, F.; Calvo-Guirado, J.L.; Aramburú Júnior, J.; Pérez-Díaz, L.; Mazón, P.; Aragoneses, J.M.; De Aza, P.N. Microgrooves and microrugosities in titanium implant surfaces: An in vitro and in vivo evaluation. Materials 2019, 12, 1287. [Google Scholar] [CrossRef] [PubMed]
- Nicolas-Silvente, A.I.; Velasco-Ortega, E.; Ortiz-Garcia, I.; Monsalve-Guil, L.; Gil, J.; Jiménez-Guerra, A. Influence of the titanium implant surface treatment on the surface roughness and chemical composition. Materials 2020, 13, 314. [Google Scholar] [CrossRef] [PubMed]
- Blatt, S.; Max Pabst, A.M.; Schiegnitz, E.; Hosang, M.; Ziebart, T.; Walter, C.; Al-Nawas, B.; Klein, M.O. Early cell response of osteogenic cells on differently modified implant surfaces: Sequences of cell proliferation, adherence and differentiation. J. Cranio Maxillo Fac Sur. 2018, 46, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Velasco-Ortega, E.; Alfonso-Rodriguez, C.; Monsalve-Guil, L.; España-López, A.; Jiménez-Guerra, A.; Garzón, I.; Alaminos, M.; Gil, F.J. Relevant aspects in the surface properties in titanium dental implants for the cellular viability. Mater. Sci Eng C Mater. Biol Appl. 2016, 64, 1–10. [Google Scholar] [CrossRef]
- Albrektsson, T.; Wennerberg, A. Oral implant surfaces: Part 1. Review focusing on topographic and chemical property surfaces and in vivo responses to them. Int J. Prosthodont. 2004, 17, 536–543. [Google Scholar]
- Albrektsson, T.; Wennerberg, A. Oral implant surfaces: Part 2. Review focusing on clinical knowledge of different surfaces. Int J. Prosthodont. 2004, 17, 544–564. [Google Scholar]
- Rupp, F.; Lianga, L.; Geis-Gerstorfer, J.; Scheideler, L.; Hüttig, F. Surface characteristics of dental implants: A review. Dent. Mater. 2018, 34, 40–57. [Google Scholar] [CrossRef]
- Velasco-Ortega, E.; Monsalve-Guil, L.; Jiménez, A.; Ortiz, I.; Moreno-Muñoz, J.; Nuñez-Márquez, E.; Pegueroles, M.; Perez, R.; Gil, F.J. Importance of the surface roughness and residual stress of dental implants on fatigue and osseointegration behavior in rabbits. J. Oral Implantol. 2016, 42, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, M.; Abe, Y.; Yoshida, Y.; Nakayama, Y.; Okazaki, M.; Akagawa, Y. Acid pretreatment of titanium implants. Biomaterials 2003, 24, 1821–1827. [Google Scholar] [CrossRef]
- Jemat, A.; Ghazali, M.J.; Razali, M.; Otsuka, Y. Surface modifications and their effects on titanium dental implants. BioMed Res. Int. 2015, 791725. [Google Scholar] [CrossRef] [PubMed]
- Ban, S.; Iwaya, Y.; Kono, H.; Sato, H. Surface modification of titanium by etching in concentrated sulfuric acid. Dent. Mater. 2006, 22, 1115–1120. [Google Scholar] [CrossRef] [PubMed]
- Klokkevold, P.R.; Nishimura, R.D.; Adachi, M.; Caputo, A. Osseointegration enhanced by chemical etching of the titanium surface: A torque removal study in the rabbit. Clin Oral Impl Res. 1997, 8, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Shayganpour, A.; Rebaudi, A.; Cortella, P.; Diaspro, A.; Salerno, M. Electrochemical coating of dental implants with anodic porous titania for enhanced osteointegration. Beilstein J. Nanotech. 2015, 6, 2183–2192. [Google Scholar] [CrossRef]
- Cho, S.A.; Park, K.T. The removal torque of titanium screw inserted in rabbit tibia treated by dual acid etching. Biomaterials 2003, 24, 3611–3617. [Google Scholar] [CrossRef]
- Mangano, F.G.; Pires, J.T.; Shibli, J.A.; Mijiritsky, E.; Iezzi, G.; Piattelli, A.; Mangano, C. Early bone response to dual acid-etched and machined dental implants placed in the posterior maxilla: A histologic and histomorphometric human study. Impl Dent. 2017, 26, 24–29. [Google Scholar] [CrossRef]
- Peñarrocha, M.; Carrillo, C.; Boronat, A.; Martí, E. Early loading of 642 Defcon implants: 1-year follow-up. J. Oral Maxillofac Surg. 2007, 65, 2317–2320. [Google Scholar] [CrossRef]
- Browaeys, H.; Defrancq, J.; Dierens, M.C.A.; Miremadi, R.; Vandeweghe, S.; van de Velde, T.; De Bruyn, H. A retrospective analysis of early and immediately loaded Osseotite implants in cross-arch rehabilitations in edentulous maxillas and mandibles up to 7 years. Clin Impl Dent. Relat Res. 2013, 15, 380–389. [Google Scholar] [CrossRef]
- Balshi, T.J.; Wolfinger, G.J.; Balshi, S.F.; Bidra, A.S. A 30-year follow-up of a patient with mandibular complete-arch fixed implant-supported prosthesis on 4 implants: A clinical report. J. Prosthodont. 2019, 28, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Simonis, P.; Dufour, T.; Tenenbaum, H. Long-term implant survival and success: A 10–16-year follow-up of non-submerged dental implants. Clin Oral Impl Res. 2010, 21, 772–777. [Google Scholar] [CrossRef]
- Su, M.Y.; Shi, B.; Zhu, Y.; Guo, Y.I.; Zhang, Y.; Xia, H.; Zhao, L. Comparison of implant success rates with different loading protocols: A meta-analysis. Int J. Oral Maxillofac Implants. 2014, 29, 344–352. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Papaspyridakos, P.; Mokti, M.; Chen, C.J.; Benic, G.I.; Gallucci, G.O.; Chronopoulos, V. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years:a systematic review. Clin Impl Dent. Relat Res. 2014, 16, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.G.; Millen, C.; Brägger, U. Clinical performance of screw-versus cement-retained fixed implant-supported reconstructions- a systematic review. Int J. Oral Maxillofac Implant. 2014, 29, 84–98. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Carrascal, N.; Salomó-Coll, O.; Gilabert-Cerdà, M.; Farré-Pagés, N.; Gargallo-Albiol, J.; Hernández-Alfaro, F. Effect of implant macro-design on primary stability: A prospective clinical study. Med. Oral Patol Oral Cir. Bucal. 2016, 21, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, M.V.; Vandamme, K.; Chaudhari, A.; De Rycker, J.; Van Meerbeek, B.; Naert, I.; Duyck, J. Dental implant macro-design features can impact the dynamics of osseointegration. Clin Implant. Dent. Relat Res. 2015, 17, 639–645. [Google Scholar] [CrossRef]
- Martínez-González, J.M.; Barona-Dorado, C.; Cano-Sánchez, J.; Fernández-Cáliz, F.; Sánchez-Turrión, A. Evaluation of 80 implants subjected to immediate loading in edentulous mandibles after two years of follow-up. Med. Oral Patol Oral Cir. Bucal. 2006, 11, 165–170. [Google Scholar]
- Lazzara, R.J.; Porter, S.S.; Testori, T.; Galante, J.; Zetterqvist, L. A prospective multicenter study evaluating loading of Osseotite implants two months after placement: One year results. J. Esthet Dent. 1998, 10, 280–289. [Google Scholar] [CrossRef]
- Sullivan, D.; Vincenzi, G.; Feldman, S. Early loading of Osseotite implants 2 months after placement in the maxilla and mandible: A 5-year report. Int J. Oral Maxillofac Implant. 2005, 20, 905–912. [Google Scholar]
- Peñarrocha, M.; Boronat, A.; García, B. Immediate loading of immediate mandibular implants with a full-arch fixed prosthesis: A preliminary study. J. Oral Maxillofac Surg. 2009, 67, 1286–1293. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Guirado, J.L.; Gómez-Moreno, G.; Delgado-Ruiz, R.A.; Maté Sánchez de Val, J.E.; Negri, B.; Ramírez-Fernández, M.P. Clinical and radiographic evaluation of osseotite-expanded platform implants related to crestal bone loss: A 10-year study. Clin Oral Implant. Res. 2014, 25, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, J.M.; García-Sabán, F.; Ferrándiz-Bernal, J.; Gonzalo-Lafuente, J.C.; Cano-Sánchez, J.; Barona-Dorado, C. Removal torque and physico-chemical characteristics of dental implants etched with hydro-fluoric and nitric acid. An experimental study in Beagle dogs. Med. Oral Patol Oral Cir. Bucal. 2006, 11, 281–285. [Google Scholar]
- Marenzi, G.; Impero, F.; Scherillo, F.; Sammartino, J.C.; Squillace, A.; Spagnuolo, G. Effect of different surface treatments on titanium dental implant micro-morphology. Materials 2019, 12, 733. [Google Scholar] [CrossRef] [PubMed]
- Shah, F.A.; Stenlund, P.; Martinelli, A.; Thomsen, P.; Palmquist, A. Direct communication between osteocytes and acid-etched titanium implants with a sub-micron topography. J. Mater. Sci. Mater. Med. 2016, 27, 167. [Google Scholar] [CrossRef]
- Carmo Filho, L.C.; Marcello-Machado, R.M.; Castilhos, E.D.; del bel Cury, A.A.; Faot, F. Can implant surfaces affect implant stability during osseointegration? A randomized clinical trial. Braz Oral Res. 2018, 32, 110. [Google Scholar] [CrossRef]
- Khang, W.; Feldman, S.; Hawley, C.E.; Gunsolley, J. A multi-center study comparing dual acid-etched and machined-surfaced implants in various bone qualities. J. Periodontol. 2001, 72, 1384–1390. [Google Scholar] [CrossRef]
- Nicoli, L.G.; de Oliveira, G.J.P.L.; Lopes, B.M.V.; Marcantonio, C.; Zandim-Barcelos, D.L.; Marcantonio Jr., E. Survival/success of dental implants with acid-etched surfaces: A retrospective evaluation after 8 to 10 years. Braz Dent. J. 2017, 28, 330–336. [Google Scholar] [CrossRef]
- Montero, J.; Fernández-Ruiz, J.; Pardal-Peláez, B.; Jiménez-Guerra, A.; Velasco-Ortega, E.; Nicolas-Silvente, A.I.; Monsalve-Guil, L. Effect of rough surface platforms on the mucosal attachment and the marginal bone loss of implants: A dog study. Materials 2020, 13, 802. [Google Scholar] [CrossRef]
- Palacios-Garzón, N.; Velasco-Ortega, E.; López-López, J. Bone loss in implants placed at subcrestal and crestal level: A systematic review and meta-analysis. Materials 2019, 12, 154. [Google Scholar] [CrossRef]
- Barona-Dorado, C.; Martínez-Rodríguez, N.; Torres-Lear, F.; Martínez- González, J.M. Observational study of 67 wide platform implants treated with avantblast surface. Results at three years. Med. Oral Patol Oral Cir. Bucal. 2009, 14, 183–187. [Google Scholar]
- Nobre, M.A.; Maló, P. Prevalence of periodontitis, dental caries, and peri-implant pathology and their relation with systemic status and smoking habits: Results of an open cohort study with 22009 patients in a private rehabilitation center. J. Dent. 2017, 67, 36–42. [Google Scholar] [CrossRef] [PubMed]
| Total Patients | n = 48 (100%) | Age | 52.4 yrs (Ranged 30–72) |
|---|---|---|---|
| Gender | Male | Female | |
| n = 48 (100%) | n = 26 (51.4%) | n = 22 (48.6%) | |
| SmokingHabit | Smoker | Nonsmoker | |
| n = 48 (100%) | n = 26 (51.4%) | n = 26 (51.4%) | |
| Periodontitis History | Yes | No | |
| n = 48 (100%) | n = 11 (22.9%) | n = 37 (77.1%) | |
| Edentulism | Totally | Partially | |
| n = 48 (100%) | n = 11 (22.9%) | n = 37 (77.1%) |
| Implant Characteristics | N = 169 (100%) | |
|---|---|---|
| Diameter | 4 mm | 3.4 mm |
| 99 implants (58.7%) | 70 implants (41.3%) | |
| Length | 13 mm | 10 mm |
| 50 implants (29.6%) | 119 implants (70.4%) | |
| Location | Maxilla | Mandible |
| 79 implants (46.7%) | 90 implants (53.3%) | |
| Area | Anterior | Posterior |
| 82 implants (48.5%) | 87 implants (51.5%) | |
| Percentage of Failure/Success | Failure | Success |
| 12 implants (7.1%) | 157 implants (92.9%) | |
| Number of Implants | Single Crown | Fixed Bridge | Overdenture | Fixed Full-Arch |
|---|---|---|---|---|
| 1 | 30 (46.1%) | -- | -- | -- |
| 2 | -- | 13 (20.0%) | -- | -- |
| 3 | -- | 7 (10.7%) | 1 (1.5%) | -- |
| 4 | -- | 1 (1.5%) | 8 (12.3%) | -- |
| 9 | -- | -- | -- | 2 (3.1%) |
| 10 | -- | -- | -- | 3 (4.6%) |
| Total Prostheses | ||||
| 65 (100%) | 30 (46.1%) | 21 (32.3%) | 9 (13.8%) | 5 (87.6%) |
| Screwed /Cemented | ||||
| 65 (100%) | 44 (67.6%) Screwed | 21 (32.4%) Cemented | ||
| Complications | + | - |
|---|---|---|
| Patients Showing Complications | 22 patients (48.6%) | 26 patients (51.4%) |
| Early Implant Loss | 3 patients (6.2%) | 45 patients (93.8%) |
| Delayed Implant Loss | 5 patients (10.4%) | 43 patients (89.6%) |
| Peri-Implantitis | 10 patients (22.8%) | 38 patients (77.2%) |
| Technical Complications | 12 patients (26.6%) | 36 patients (73.4%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velasco-Ortega, E.; Jimenez-Guerra, A.; Monsalve-Guil, L.; Ortiz-Garcia, I.; Nicolas-Silvente, A.I.; Segura-Egea, J.J.; Lopez-Lopez, J. Long-Term Clinical Outcomes of Treatment with Dental Implants with Acid Etched Surface. Materials 2020, 13, 1553. https://doi.org/10.3390/ma13071553
Velasco-Ortega E, Jimenez-Guerra A, Monsalve-Guil L, Ortiz-Garcia I, Nicolas-Silvente AI, Segura-Egea JJ, Lopez-Lopez J. Long-Term Clinical Outcomes of Treatment with Dental Implants with Acid Etched Surface. Materials. 2020; 13(7):1553. https://doi.org/10.3390/ma13071553
Chicago/Turabian StyleVelasco-Ortega, Eugenio, Alvaro Jimenez-Guerra, Loreto Monsalve-Guil, Ivan Ortiz-Garcia, Ana I. Nicolas-Silvente, Juan J. Segura-Egea, and Jose Lopez-Lopez. 2020. "Long-Term Clinical Outcomes of Treatment with Dental Implants with Acid Etched Surface" Materials 13, no. 7: 1553. https://doi.org/10.3390/ma13071553
APA StyleVelasco-Ortega, E., Jimenez-Guerra, A., Monsalve-Guil, L., Ortiz-Garcia, I., Nicolas-Silvente, A. I., Segura-Egea, J. J., & Lopez-Lopez, J. (2020). Long-Term Clinical Outcomes of Treatment with Dental Implants with Acid Etched Surface. Materials, 13(7), 1553. https://doi.org/10.3390/ma13071553








