Early Short-Term Postoperative Mechanical Failures of Current Ceramic-on-Ceramic Bearing Total Hip Arthroplasties
Abstract
1. Introduction
2. Materials and Methods
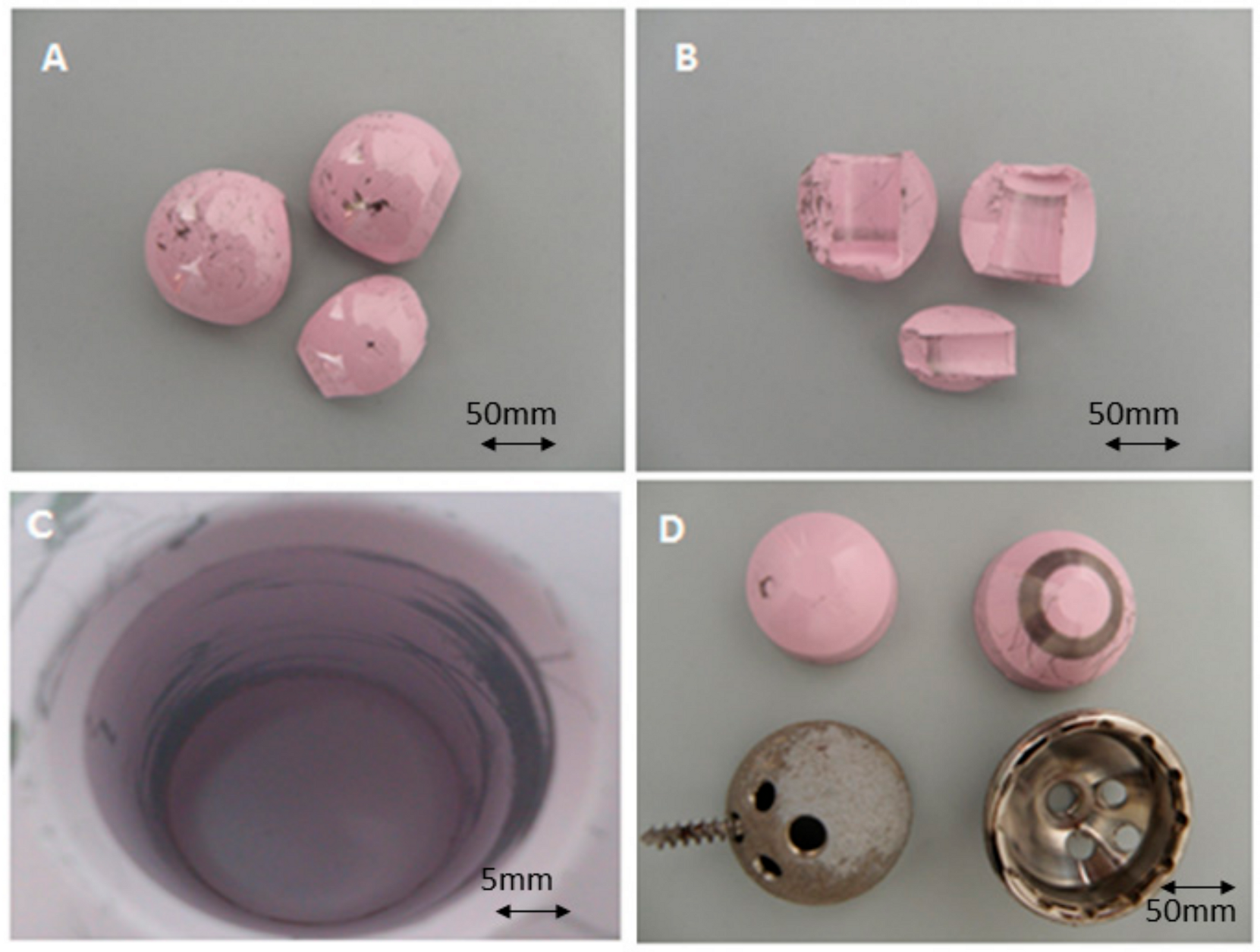
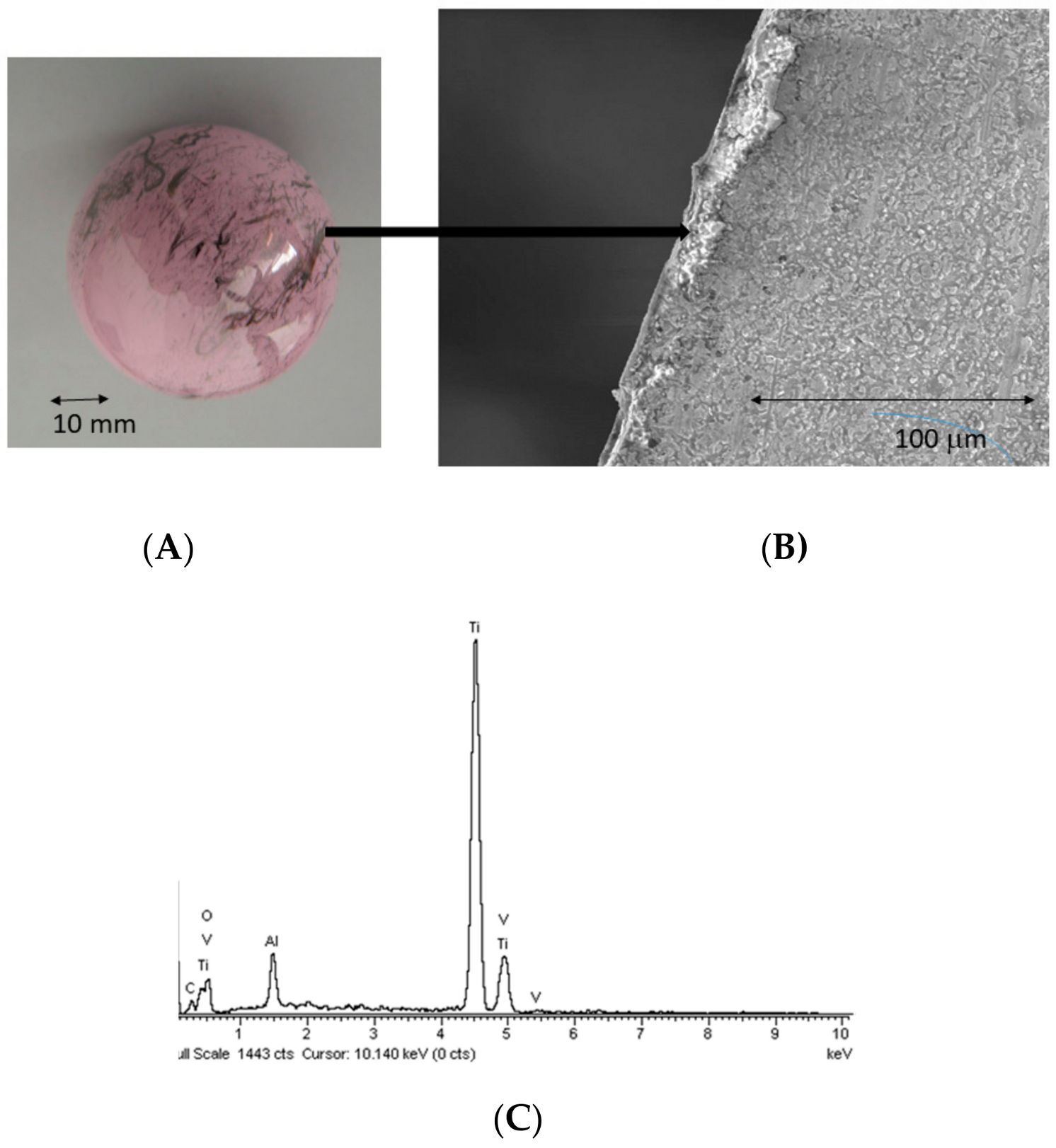
- A total of 4 out of the 6 showed chipping of the liner.
- One of these cases also presented fracture of the liner head. It corresponded to a 25-year-old woman suffering from dysplasic hip. She received an uncemented Trilogy acetabular cup (Zimmer, USA) with an uncemented Fitmore femoral stem (Zimmer, Warsaw, IN, USA), using a 28 mm diameter head in a 48 mm diameter liner and short neck.
- In two other cases of liner chipping, the acetabulum was vertically oriented and retroverted. One of them experienced dislocation and closed reduction in the immediate postoperative.
- The component orientation was judged radiologically perfect in the fourth case, and there was no trauma or instability.
- The remaining two cases operated using a Trinity cup (Corin, Cirencester, UK) and a MiniHip stem (Corin, Cirencester, UK). Both components were revised for disassembly of the ceramic insert from the metallic cup caused by the protruding head of fixation screws.
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kluge, F.A.; Goldstein, J.R.; Vogt, T.C. Transfers in an Aging European Union. J. Econ. Ageing 2018. [Google Scholar] [CrossRef]
- Stuart Melvin, J.; Karthikeyan, T.; Cope, R.; Fehring, T.K. Early Failures in Total Hip Arthroplasty—A Changing Paradigm. J. Arthroplast. 2014, 29, 1285–1288. [Google Scholar] [CrossRef] [PubMed]
- The Organization for Economic Cooperation and Development. Infant Health: Low Birth Weight. In Health at a Glance: Europe; OECD Publishing: Paris, France, 2012. [Google Scholar]
- Malem, D.; Nagy, M.T.; Ghosh, S.; Shah, B. Catastrophic Failure of Ceramic-on-Ceramic Total Hip Arthroplasty Presenting as Squeaking Hip. BMJ Case Rep. 2013. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y. What Are the Options for Better Outcomes of Total Hip Arthroplasty? Clin. Orthop. Surg. 2010, 2, 195. [Google Scholar] [CrossRef]
- Aprato, A.; Loddo, G.; Giaretta, S.; Di Benedetto, P.; Massè, A. Ceramic Bearings Fracture: A Literature Review on Risk Factors, Diagnosis, and Treatment. J. Surg. Trauma 2020, 8, 1–7. [Google Scholar] [CrossRef]
- Vendittoli, P.A.; Riviere, C.; Lavigne, M.; Lavoie, P.; Alghamdi, A.; Duval, N. Alumina on Alumina Versus Metal on Conventional Polyethylene: A Randomized Clinical Trial with 9 to 15 Years’ Follow-Up. Acta Orthop. Belg. 2013, 79, 181–190. [Google Scholar]
- D’Antonio, J.A.; Capello, W.N.; Naughton, M. Ceramic Bearings for Total Hip Arthroplasty Have High Survivorship at 10 Years. Clin. Orthop. Relat. Res. 2012, 470, 373–381. [Google Scholar] [CrossRef]
- Finkbone, P.R.; Severson, E.P.; Cabanela, M.E.; Trousdale, R.T. Ceramic-on-Ceramic Total Hip Arthroplasty in Patients Younger Than 20 Years. J. Arthroplast. 2012, 27, 213–219. [Google Scholar] [CrossRef]
- Kamath, A.F.; Sheth, N.P.; Hosalkar, H.H.; Babatunde, O.M.; Lee, G.C.; Nelson, C.L. Modern Total Hip Arthroplasty in Patients Younger Than 21 Years. J. Arthroplast. 2012, 27, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Faldini, C.; Miscione, M.T.; Chehrassan, M. Congenital Hip Dysplasia Treated by Total HIP Arthroplasty Using Cementless Tapered Stem in Patients Younger Than 50 Years Old: Results After 12-Years Follow-Up. J. Orthop. Traumatol. 2011, 12, 213–218. [Google Scholar] [CrossRef]
- Barrack, R.L.; Burak, C.; Skinner, H.B. Concerns About Ceramics in THA. Clin. Orthop. Relat. Res. 2004, 429, 73–79. [Google Scholar] [CrossRef]
- Bal, B.S.; Garino, J.; Ries, M.; Rahaman, M.N. A Review of Ceramic Bearing Materials in Total Joint Arthroplasty. HIP Int. 2007, 17, 21–30. [Google Scholar] [CrossRef]
- Tateiwa, T.; Clarke, I.C.; Williams, P.A.; Garino, J.; Manaka, M.; Shishido, T.; Yamamoto, K.; Imakiire, A. Ceramic Total Hip Arthroplasty in the United States: Safety and Risk Issues Revisited. Am. J. Orthop. 2008, 37, E26–E31. [Google Scholar]
- Allain, J.; Roudot-Thoraval, F.; Delecrin, J.; Anract, P.; Migaud, H.; Goutallier, D. Revision Total Hip Arthroplasty Performed After Fracture of a Ceramic Femoral Head. A Multicenter Survivorship Study. J. Bone Joint Surg. A 2003, 85, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Al-Saffar, N. Early Clinical Failure of Total Joint Replacement in Association with Follicular Proliferation of B-Lymphocytes: A Report of Two Cases. J. Bone Joint Surg. A 2002, 84, 2270–2273. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Ranawat, A.S.; Rasquinha, V.J.; Weiskopf, J.; Howard, H.; Ranawat, C.S. Revision Total Hip Arthroplasty for Ceramic Head Fracture: A Long-Term Follow-Up. J. Arthroplast. 2020, 25, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Lachiewicz, P.F.; Kleeman, L.T.; Seyler, T. Bearing Surfaces for Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. 2018, 26, 45–57. [Google Scholar] [CrossRef]
- Howard, D.P.; Wall, P.D.H.; Fernandez, M.A. Ceramic-on-Ceramic Bearing Fractures in Total Hip Arthroplasty: An Analysis of Data from the National Joint Registry. Bone Joint J. 2017, 99-B, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.C.; Kim, R.H. Incidence of Modern Alumina Ceramic and Alumina Matrix Composite Femoral Head Failures in Nearly 6 Million Hip Implants. J. Arthroplast. 2016, 32, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Levy, Y.D.; Walter, W.L. Complications of Ceramic-on-Ceramic Bearings: Fracture, Stripe Wear, and Squeaking. In Complications after Primary Total Hip Arthroplasty: A Comprehensive Clinical Guide; Abdel, M.P., Della Valle, C.J., Eds.; Springer International Publishing: Cham, Basel, Switzerland, 2017; pp. 137–150. [Google Scholar] [CrossRef]
- Brandt, J.M.; Gascoyne, T.C.; Guenther, L.E.; Allen, A.; Hedden, D.R.; Turgeon, T.R. Clinical Failure Analysis of Contemporary Ceramic-on-Ceramic Total Hip Replacements. Proc. Inst. Mech. Eng. H 2013, 227, 833–846. [Google Scholar] [CrossRef] [PubMed]
- Sipek, K.T.; Lyvers, M.E.; Mathew, M.T. Failure Causes in Total Hip Replacements: A Review. Austin J. Orthop. Rheumatol. 2018, 5, 1064. [Google Scholar]
- Pawar, E.D.; Yadav, A.K.; Sharma, A.; Harsoor, A. Ceramic Liner Fracture in Ceramic on Ceramic Total Hip Arthoplasty: A Case Report. Int. J. Surg. Case Rep. 2019, 65, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Anwar, I.; Bhatnagar, G.; Atrah, S. Delayed Catastrophic Failure of a Ceramic Head in Hybrid Total Hip Arthroplasty. J. Arthroplast. 2009, 24, 158.e5–158.e8. [Google Scholar] [CrossRef] [PubMed]
- Gallo, J.; Goodman, S.B.; Lostak, J.; Janout, M. Advantages and Disadvantages of Ceramic on Ceramic Total Hip Arthroplasty: A Review. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc Czech Repub. 2012, 156, 204–212. [Google Scholar] [CrossRef]
- Al-Hajjar, M.; Fisher, J.; Tipper, J.L.; Williams, S.; Jennings, L.M. Wear of 36-mm BIOLOX(R) Delta Ceramic-on-Ceramic Bearing in Total Hip Replacements under Edge Loading Conditions. Proc. Inst. Mech. Eng. H 2013, 227, 535–542. [Google Scholar] [CrossRef]
- Macdonald, N.; Bankes, M. Ceramic on Ceramic Hip Prostheses: A Review of Past and Modern Materials. Arch. Orthop. Trauma Surg. 2014, 134, 1325–1333. [Google Scholar] [CrossRef]
- Curran, S.; Hoskin, T.; Williams, S.; Scholes, S.C.; Kinbrum, A.; Unsworth, A. Does Surface Wettability Influence the Friction and Wear of Large-Diameter CoCrMo alloy Hip Resurfacings? Proc. Inst. Mech. Eng. H 2013, 227, 847–858. [Google Scholar] [CrossRef]
- Mesko, J.W.; D’Antonio, J.A.; Capello, W.N.; Bierbaum, B.E.; Naughton, M. Ceramic-on-Ceramic Hip Outcome at a 5- to 10-Year Interval: Has It Lived Up to Its Expectations? J. Arthroplast. 2011, 26, 172–177. [Google Scholar] [CrossRef]
- Hu, D.; Tie, K.; Yang, X.; Alaidaros, M.; Chen, L. Comparison of Ceramic-on-Ceramic to Metal-on-Polyethylene Bearing Surfaces in Total Hip Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. J. Orthop. Surg. Res. 2015, 10, 22. [Google Scholar] [CrossRef]
- Rodriguez, J.A.; Rathod, P.A. Large Diameter Heads: Is Bigger Always Better? J. Bone Joint Surg. Br. 2012, 94, 52–54. [Google Scholar] [CrossRef]
- Tsikandylakis, G.; Mohaddes, M.; Cnudde, P.; Eskelinen, A.; Kärrholm, J.; Rolfson, O. Head Size in Primary Total Hip Arthroplasty. EFORT Open Rev. 2018, 3, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, W.G.; McAuley, J.P.; Dennis, D.A.; Murphy, J.A.; Blumenfeld, T.J.; Politi, J. THA with Delta Ceramic on Ceramic: Results of a Multicenter Investigational Device Exemption Trial. Clin. Orthop. Relat. Res. 2010, 468, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Koo, K.H.; Ha, Y.C.; Jung, W.H.; Kim, S.R.; Yoo, J.J.; Kim, H.J. Isolated Fracture of the Ceramic Head After Third-Generation Alumina-on-Alumina Total Hip Arthroplasty. J. Bone Joint Surg. Am. 2008, 90, 329–336. [Google Scholar] [CrossRef]
- Park, Y.S.; Hwang, S.K.; Choy, W.S.; Kim, Y.S.; Moon, Y.W.; Lim, S.J. Ceramic Failure After Total Hip Arthroplasty with an Alumina-Onalumina Bearing. J. Bone Joint Surg. Am. 2006, 88, 780–787. [Google Scholar] [CrossRef]
- Rhoads, D.P.; Baker, K.C.; Israel, R.; Greene, P.W. Fracture of an Alumina Femoral Head Used in Ceramic-on-Ceramic Total Hip Arthroplasty. J. Arthroplast. 2008, 23, 1239.e25–1239.e30. [Google Scholar] [CrossRef] [PubMed]
- Capello, W.N.; D’Antonio, J.A.; Feinberg, J.R.; Manley, M.T.; Naughton, M. Ceramic-on-Ceramic Total Hip Arthroplasty: Update. J. Arthroplast. 2008, 23, 39–43. [Google Scholar] [CrossRef]
- Ha, Y.C.; Kim, S.Y.; Kim, H.J.; Yoo, J.J.; Koo, K.H. Ceramic Liner Fracture after Cementless Alumina-on-Alumina Total Hip Arthroplasty. Clin. Orthop. Relat. Res. 2007, 458, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Hamouche, D.; Nich, C.; Bizot, P.; Meunier, A.; Nizard, R.; Sedel, L. Fractures of Ceramic Bearings: History and Present Status. Clin. Orthop. Relat. Res. 2003, 417, 19–26. [Google Scholar] [CrossRef]
- Hwang, D.S.; Kim, Y.M.; Lee, C.H. Alumina Femoral Head Fracture in Uncemented Total Hip Arthroplasty with a Ceramic Sandwich Cup. J. Arthroplast. 2007, 22, 468–471. [Google Scholar] [CrossRef]
- Castagnini, F.; Bordini, B.; Tassinari, E. Delta-on-Delta Ceramic Bearing Surfaces in Revision Hip Arthroplasty. J. Arthroplast. 2019, 34, 2065–2071. [Google Scholar] [CrossRef]
- Jenabzadeh, A.R.; Pearce, S.J.; Walter, W.L. Total Hip Replacement: Ceramic-on-Ceramic. Semin. Arthroplast. 2012, 23, 232–240. [Google Scholar] [CrossRef]
- Christel, P.S. Biocompatibility of Surgical-Grade Dense Polycrystalline Alúmina. Clin. Orthop. Relat. Res. 1992, 282, 10–18. [Google Scholar] [CrossRef]
- Sentuerk, U.; von Roth, P.; Perka, C. Ceramic on Ceramic Arthroplasty of the Hip: New Materials Confirm Appropriate Use in Young Patients. Bone Joint J. 2016, 98, 14–17. [Google Scholar] [CrossRef]
- Lee, G. Ceramic Component Fracture: Getting Rarer, but When It Happens? Orthop. Proc. 2017, 99, 107. [Google Scholar]
- Chang, J.-D.; Kimm, I.-S.; Mansukhani, S.A.; Sharma, V.; Lee, S.-S.; Yoo, J.-H. Midterm Outcome of Fourth-Generation Ceramic-on-Ceramic Bearing Surfaces in Revision Total Hip Arthroplasty. J. Orthop. Surg. 2018, 26. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.J.; Halawa, M. Lining up the Liner: 2 Case Reports of Early Ceramic Liner Fragmentation. J. Arthroplast. 2007, 22, 1217–1222. [Google Scholar] [CrossRef] [PubMed]
- Min, B.-W.; Song, K.-S.; Kang, C.-H.; Bae, K.-C.; Won, Y.-Y.; Lee, K.-Y. Delayed Fracture of a Ceramic Insert with Modern Ceramic Total Hip Replacement. J. Arthroplast. 2007, 22, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Poggie, R.A.; Turgeon, T.R.; Coutts, R.D. Failure Analysis of a Ceramic Bearing Acetabular Component. J. Bone Joint Surg. Am. 2007, 89, 367–375. [Google Scholar] [CrossRef]
- Toran, M.M.; Cuenca, J.; Martinez, A.A.; Herrera, A.; Thomas, J.V. Fracture of a Ceramic Femoral Head after Ceramic-on-Ceramic Total Hip Arthroplasty. J. Arthroplast. 2006, 21, 1072–1073. [Google Scholar] [CrossRef] [PubMed]
- Willmann, G. Fiction and Facts Concerning the Reliability of Ceramics in THR. In Bioceramics in Joint Arthroplasty; Zippel, H., Dietrich, M., Eds.; Steinkopff Verlag: Berlin, Germany, 2003; pp. 193–196. [Google Scholar] [CrossRef]
- Ranawat, A.S.; Ranawat, C.S. The Squeaking Hip: A Cause for Concern—Agrees. Orthopedics 2007, 30, 738–743. [Google Scholar] [CrossRef]
- ISO. Retrieval and Analysis of Surgical Implants—Part 1: Retrieval and Handling; 12891–1:2015; ISO: Geneva, Switzerland, 2015; pp. 1–24. [Google Scholar]
- Walter, W.L.; O’Toole, G.C.; Walter, W.K.; Ellis, A.; Zicat, B.A. Squeaking in Ceramic-on-Ceramic Hips: The Importance of Acetabular Component Orientation. J. Arthroplast. 2007, 22, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, M.; Sudo, A.; Hirata, H.; Uchida, A. Ceramic Acetabular Liner Fracture in Total Hip Arthroplasty with a Ceramic Sandwich Cup. J. Arthroplast. 2003, 18, 658–661. [Google Scholar] [CrossRef]
- Lee, S.C.; Jung, K.A.; Nam, C.H.; Kim, T.H.; Ahn, N.K.; Hwang, S.H. Acetabular Screw Head-Induced Ceramic Acetabular Liner Fracture in Cementless Ceramic-on-Ceramic Total Hip Arthroplasty. Orthopedics 2010, 12, 33. [Google Scholar] [CrossRef]
- Michaud, R.J.; Rashad, S.Y. Spontaneous Fracture of the Ceramic Ball in a Ceramic-Polyethylene Total Hip Arthroplasty. J. Arthroplast. 1995, 10, 863–867. [Google Scholar] [CrossRef]
- Pulliam, I.T.; Trousdale, R.T. Fracture of a Ceramic Femoral Head after a Revision Operation. A Case Report. J. Bone Joint Surg. Am. 1997, 79, 118–121. [Google Scholar] [CrossRef]
- Manero, J.M.; Gil, F.J.; Padrós, E.; Planell, J.A. Applications of Environmental Scanning Electron Microscopy (ESEM) in Biomaterials Field. Microsc. Res. Tech. 2003, 61, 469–480. [Google Scholar] [CrossRef]
- Gil, F.J.; Solano, E.; Peña, J.; Engel, E.; Mendoza, A.; Planell, J.A. Microstructural, Mechanical and Citotoxicity Evaluation of Different NiTi and NiTiCu Shape Memory Alloys. J. Mater. Sci. Mater. Med. 2004, 15, 1181–1185. [Google Scholar] [CrossRef] [PubMed]
- Fernández, E.; Gil, F.J.; Best, S.; Ginebra, M.P.; Driessens, F.C.M.; Planell, J.A. The Cement Setting Reaction in the CaHPO4-αCa3(PO4)2 System: An X-ray Diffraction Study. J. Biomed. Mater. Res. 1998, 42, 403–406. [Google Scholar] [CrossRef]
- Salinas, A.J.; Merino, J.M.; Babonneau, F.; Gil, F.J.; Vallet-Regí, M. Microstructure and Macroscopic Properties of Bioactive CaO-SiO2-PDMS Hybrids. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 81, 274–282. [Google Scholar] [CrossRef]
- Taheriazam, A.; Mohajer, M.A.; Aboulghasemian, M.; Hajipour, B. Fracture of the Alumina-Bearing Couple Delta Ceramic Liner. Orthopedics 2012, 35, e91–e93. [Google Scholar] [CrossRef]
- Vallet-Regí, M.; San Rmán, J.; Padilla, S.; Doadrio, J.C.; Gil, F.J. Bioactivity and mechanical properties of SiO2-CaO-P2O5 glass-ceramics. J. Mater. Chem. 2005, 15, 1353–1359. [Google Scholar] [CrossRef]
- Traina, F.; Tassinari, E.; De Fine, M.; Bordini, B.; Toni, A. Revision of Ceramic Hip Replacements for Fracture of a Ceramic Component: AAOS Exhibit Selection. J. Bone Joint Surg. A 2011, 93, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Bizot, P.; Larrouy, M.; Witvoet, J.; Sedel, L.; Nizard, R. Press-Fit Metal-Backed Alumina Sockets: A Minimum 5-Year Follow Up Study. Clin. Orthop. Relat. Res. 2000, 379, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Urban, J.A.; Garvin, K.L.; Boese, C.K.; Bryson, L.; Pedersen, D.R.; Callaghan, J.J.; Miller, R.K. Ceramic-on-Polyethylene Bearing Surfaces in Total Hip Arthroplasty. Seventeen to Twenty-One-Year Results. J. Bone Joint Surg. Am. 2001, 83, 1688–1694. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.A.; Dayan, A.J.; Ergas, E.; Stuchin, S.A.; Di Cesare, P.E. Catastrophic Failure of the Acetabular Component in a Ceramic-Polyethylene Bearing Total Hip Arthroplasty. J. Arthroplast. 1998, 13, 108–113. [Google Scholar] [CrossRef]
- Willmann, G. Ceramic Femoral Head Retrieval Data. Clin. Orthop. Relat. Res. 2000, 379, 22–28. [Google Scholar] [CrossRef]
- Masson, B. Emergence of the Alumina Matrix Composite in Total Hip Arthroplasty. Int. Orthop. 2009, 33, 359–363. [Google Scholar] [CrossRef]
- De Aza, A.H.; Chevalier, J.; Fantozzi, G.; Schehl, M.; Torrecillas, R. Crack Growth Resistance of Alumina, Zirconia and Zirconia Toughened Alumina Ceramics for Joint Prostheses. Biomaterials 2002, 23, 937–945. [Google Scholar] [CrossRef]
- Chevalier, J.; Grandjean, S.; Kuntz, M.; Pezzotti, G. On the Kinetics and Impact of Tetragonal to Monoclinic Transformation in an Alumina/Zirconia Composite for Arthroplasty Applications. Biomaterials 2009, 30, 5279–5282. [Google Scholar] [CrossRef]
- Masonis, J.L.; Bourne, R.B.; Ries, M.D.; McCalden, R.W.; Salehi, A.; Kelman, D.C. Zirconia Femoral Head Fractures. J. Arthroplast. 2004, 19, 898–905. [Google Scholar] [CrossRef]
- Kraay, M.J.; Thomas, R.D.; Rimnac, C.M.; Fitzgerald, S.J.; Goldberg, V.M. Zirconia versus Co-Cr Femoral Heads in Total Hip Arthroplasty: Early Assessment of Wear. Clin. Orthop. Relat. Res. 2006, 453, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Sevilla, P.; Sandino, C.; Arciniegas, M.; Martinez-Gomis, J.; Peraire, M.; Gil, F.J. Evaluating mechanical properties and degradation. Mater. Sci. Eng. C 2010, 20, 14–19. [Google Scholar] [CrossRef]
- Garino, J.P. Modern Ceramic-on-Ceramic Total Hip Systems in the United States: Early Results. Clin. Orthop. Relat. Res. 2000, 41–47. [Google Scholar] [CrossRef]
- Hamadouche, M.; Boutin, P.; Daussange, J.; Bolander, M.E.; Sedel, L. Alumina-on-Alumina Total hip Arthroplasty: A Minimum 18.5-Year Follow-Up Study. J. Bone Joint Surg. Am. 2002, 84, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Callaway, G.H.; Flynn, W.; Ranawat, C.S.; Sculco, T.P. Fracture of the Femoral Head after Ceramic-on-Polyethylene Total Hip Arthroplasty. J. Arthroplast. 1995, 10, 855–859. [Google Scholar] [CrossRef]
- Langdown, A.J.; Pickard, R.J.; Hobbs, C.M.; Clarke, H.J.; Dalton, D.J.N.; Grover, M.L. Incomplete Seating of the Liner with the Trident Acetabular System: A Cause for Concern? J. Bone Joint Surg. Br. 2007, 89, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Jang, B.; Kanawati, A.; Brazil, D.; Bruce, W. Laser Etching Causing Fatigue Fracture at the Neck-Shoulder Junction of an Uncemented Femoral Stem: A Case Report. J. Orthop. 2013, 10, 95–98. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.W.; Kim, H.T. Early Fatigue Failures of Cemented, Forged, Cobalt-Chromium Femoral Stems at the Neck-Shoulder Junction. J. Arthroplast. 2001, 16, 236–238. [Google Scholar] [CrossRef]
- Fernández-Fairén, M.; Sala, P.; Gil, F.J. Failures of Yttria-Stabilised Tetragonal Zirconia: 52 Retrieved Ceramic Femoral Heads of Total Hip Prostheses. Biomed. Mater. Eng. 2006, 16, 415–422. [Google Scholar]
- Fernández-Fairén, M.; Blanco, A.; Murcia, A.; Sevilla, P.; Gil, F.J. Aging of Retrieved Zirconia Femoral Heads. Clin. Orthop. Relat. Res. 2007, 462, 122–129. [Google Scholar] [CrossRef]
- Chowdhury, S.; Vohra, Y.K.; Lemmons, J.E.; Ueno, M.; Ikeda, J. Accelerating Aging of Zirconia Femoral Head Implants: Change of Surface Structure and Mechanical Properties. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 81, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Poggio, C.; Lasagna, A.; Chiesa, M.; Scribante, A. Vickers Micro-Hardness of New Restorative CAD/CAM Dental Materials: Evaluation and Comparison after Exposure to Acidic Drink. Materials 2019, 12, 1246. [Google Scholar] [CrossRef] [PubMed]
- Iinuma, Y.; Hirota, M.; Hayakawa, T.; Ohkubo, C. Surrounding Tissue Response to Surface-Treated Zirconia Implants. Materials 2020, 13, 30. [Google Scholar] [CrossRef] [PubMed]



| Prosthesis Reference | Time of Implantation (Days) | Monoclinic Phase (%) | Roughness (nm) | Fracture Resistance (N) |
|---|---|---|---|---|
| Original | 0 | 14 (5) | 4 (2) | 978 (67) |
| 47-FJM | 372 | 25 (7) | 11 (4) | 934 (30) |
| 92-XGM | 398 | 38 (9) | 19 (3) | 925 (11) |
| 98-MSO | 410 | 42 (9) | 19 (7) | 910 (38) |
| 103-REQ | 500 | 45 (7) | 21 (5) | 901 (21) |
| 108-SAT | 587 | 50 (13) | 32 (3) | 889 (30) |
| 110-TAG | 639 | 75 (11) | 55(4) | 860 (40) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Fairén, M.; Torres-Perez, A.; Perez, R.; Punset, M.; Molmeneu, M.; Ortiz-Hernández, M.; Manero, J.M.; Gil, J. Early Short-Term Postoperative Mechanical Failures of Current Ceramic-on-Ceramic Bearing Total Hip Arthroplasties. Materials 2020, 13, 5318. https://doi.org/10.3390/ma13235318
Fernández-Fairén M, Torres-Perez A, Perez R, Punset M, Molmeneu M, Ortiz-Hernández M, Manero JM, Gil J. Early Short-Term Postoperative Mechanical Failures of Current Ceramic-on-Ceramic Bearing Total Hip Arthroplasties. Materials. 2020; 13(23):5318. https://doi.org/10.3390/ma13235318
Chicago/Turabian StyleFernández-Fairén, Mariano, Ana Torres-Perez, Roman Perez, Miquel Punset, Meritxell Molmeneu, Monica Ortiz-Hernández, José María Manero, and Javier Gil. 2020. "Early Short-Term Postoperative Mechanical Failures of Current Ceramic-on-Ceramic Bearing Total Hip Arthroplasties" Materials 13, no. 23: 5318. https://doi.org/10.3390/ma13235318
APA StyleFernández-Fairén, M., Torres-Perez, A., Perez, R., Punset, M., Molmeneu, M., Ortiz-Hernández, M., Manero, J. M., & Gil, J. (2020). Early Short-Term Postoperative Mechanical Failures of Current Ceramic-on-Ceramic Bearing Total Hip Arthroplasties. Materials, 13(23), 5318. https://doi.org/10.3390/ma13235318








