Functionalization and Surface Modifications of Bioactive Glasses (BGs): Tailoring of the Biological Response Working on the Outermost Surface Layer
Abstract
1. Introduction
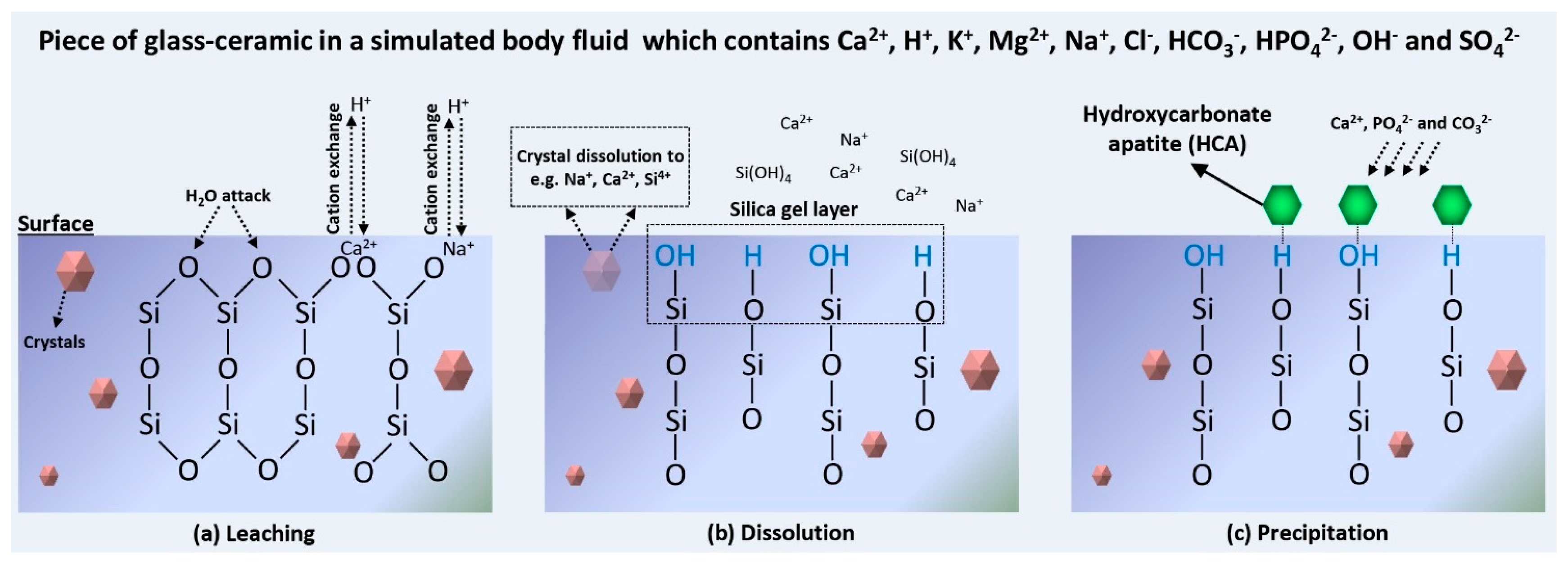
2. Mechanisms of Surface Modification of BGs
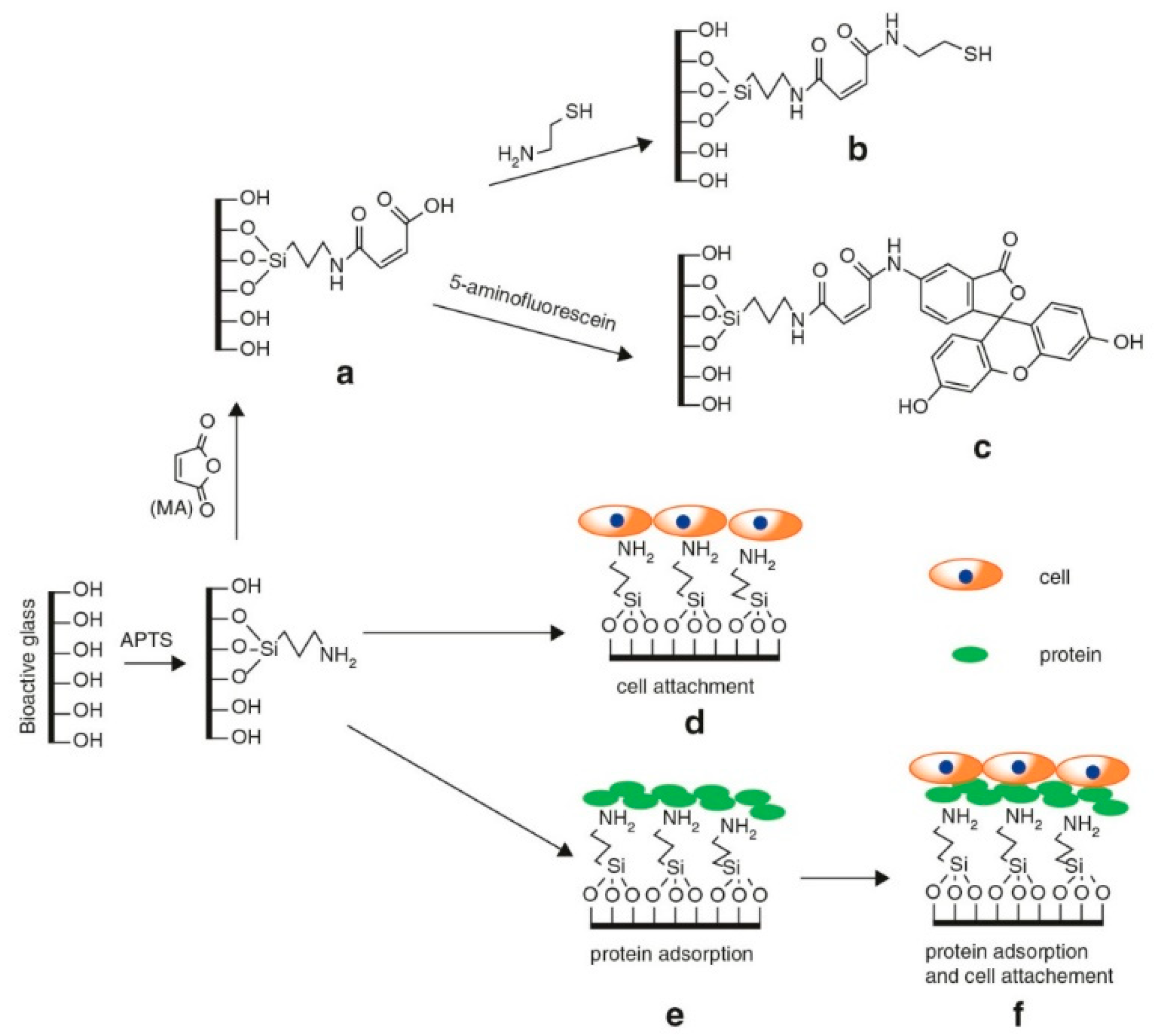
2.1. Surface Modification by Chemical Agents
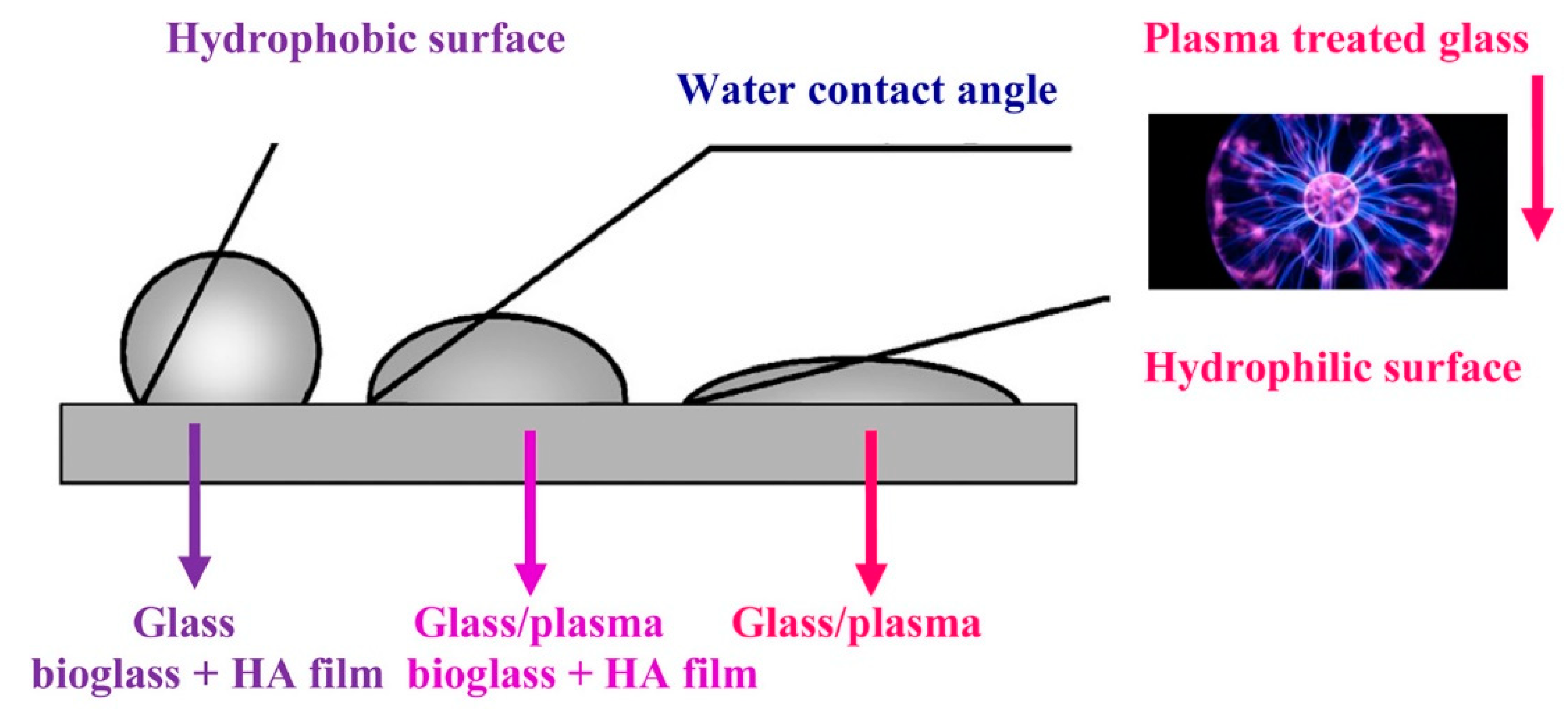
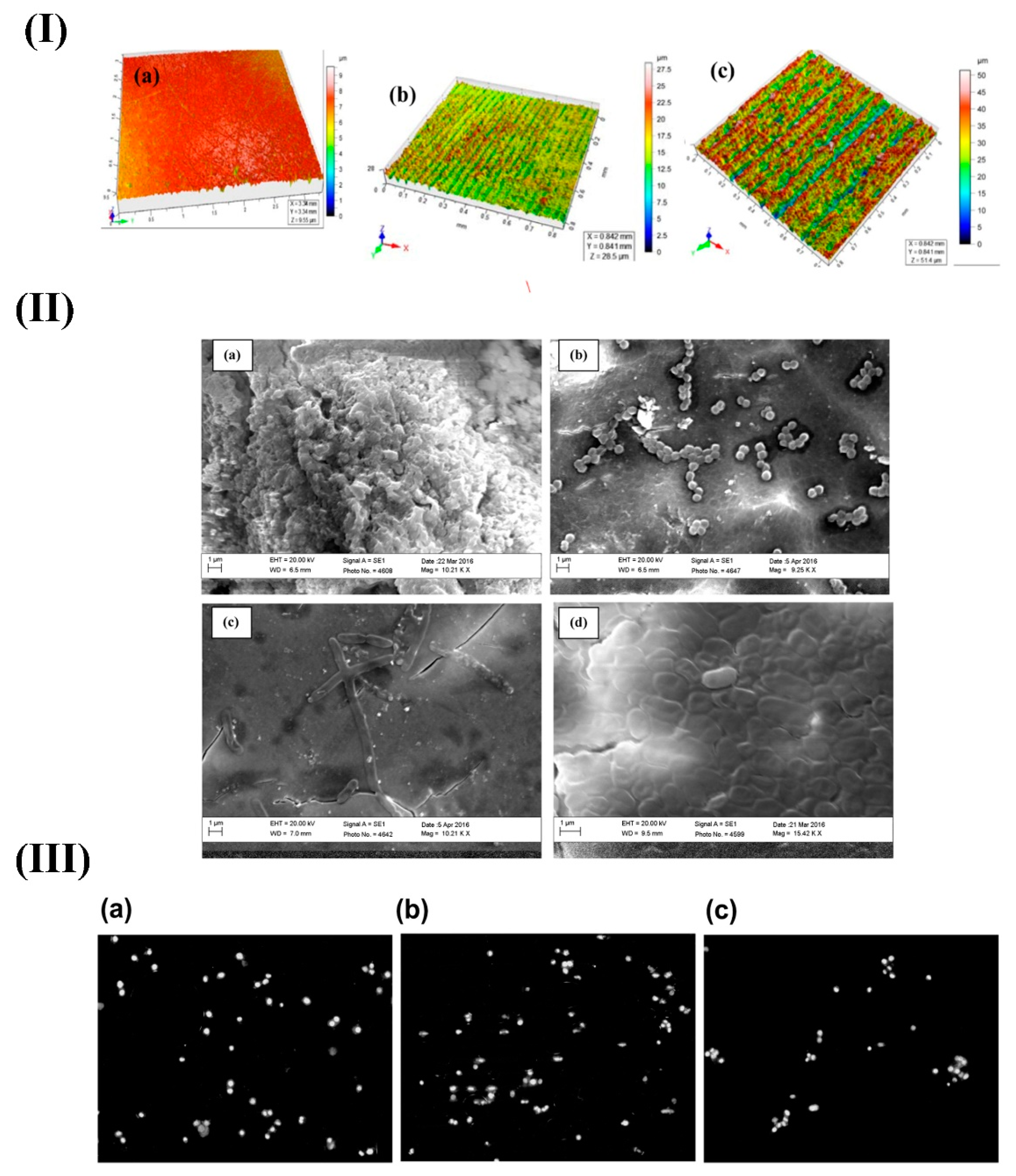
2.2. Physico-Chemical Techniques
2.3. Radiation-Based Methods
3. Biological Improvements Carried by Surface Functionalization
4. Concluding Remarks
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kargozar, S.; Mozafari, M.; Hamzehlou, S.; Baino, F. Using Bioactive Glasses in the Management of Burns. Front. Bioeng. Biotechnol. 2019, 7, 62. [Google Scholar] [CrossRef] [PubMed]
- Kargozar, S.; Mozafari, M.; Hamzehlou, S.; Kim, H.-W.; Baino, F. Mesoporous bioactive glasses (MBGs) in cancer therapy: Full of hope and promise. Mater. Lett. 2019, 251, 241–246. [Google Scholar] [CrossRef]
- Miola, M.; Pakzad, Y.; Banijamali, S.; Kargozar, S.; Vitale-Brovarone, C.; Yazdanpanah, A.; Bretcanu, O.; Ramedani, A.; Vernè, E.; Mozafari, M. Glass-ceramics for cancer treatment: So close, or yet so far? Acta Biomater. 2019, 83, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Rahaman, M.; Bal, B.; Bonewald, L.; Kuroki, K.; Brown, R. Bioactive glass scaffolds with controllable degradation rates for bone tissue engineering applications, II: In vitro and in vivo biological evaluation. J. Biomed. Mater. Res. Part A 2010, 95, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Fan, W.; Zhu, Y.; Gelinsky, M.; Chang, J.; Cuniberti, G.; Albrecht, V.; Friis, T.; Xiao, Y. Multifunctional magnetic mesoporous bioactive glass scaffolds with a hierarchical pore structure. Acta Biomater. 2011, 7, 3563–3572. [Google Scholar] [CrossRef] [PubMed]
- Bi, L.; Rahaman, M.N.; Day, D.E.; Brown, Z.; Samujh, C.; Liu, X.; Mohammadkhah, A.; Dusevich, V.; Eick, J.D.; Bonewald, L.F. Effect of bioactive borate glass microstructure on bone regeneration, angiogenesis, and hydroxyapatite conversion in a rat calvarial defect model. Acta Biomater. 2013, 9, 8015–8026. [Google Scholar] [CrossRef]
- Wu, C.; Fan, W.; Chang, J. Functional mesoporous bioactive glass nanospheres: Synthesis, high loading efficiency, controllable delivery of doxorubicin and inhibitory effect on bone cancer cells. J. Mater. Chem. B 2013, 1, 2710–2718. [Google Scholar] [CrossRef]
- Kargozar, S.; Montazerian, M.; Hamzehlou, S.; Kim, H.-W.; Baino, F. Mesoporous bioactive glasses: Promising platforms for antibacterial strategies. Acta Biomater. 2018, 81, 1–19. [Google Scholar] [CrossRef]
- Kargozar, S.; Baino, F.; Hamzehlou, S.; Hill, R.G.; Mozafari, M. Bioactive glasses: Sprouting angiogenesis in tissue engineering. Trends Biotechnol. 2018, 36, 430–444. [Google Scholar] [CrossRef]
- Kargozar, S.; Baino, F.; Hamzehlou, S.; Hill, R.G.; Mozafari, M. Bioactive glasses entering the mainstream. Drug Discov. Today 2018, 23, 1700–1704. [Google Scholar] [CrossRef]
- Oyane, A.; Onuma, K.; Ito, A.; Kim, H.M.; Kokubo, T.; Nakamura, T. Formation and growth of clusters in conventional and new kinds of simulated body fluids. J. Biomed. Mater. Res. Part A Off. J. Soc. Biomater. Jpn. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2003, 64, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- Bohner, M.; Lemaitre, J. Can bioactivity be tested in vitro with SBF solution? Biomaterials 2009, 30, 2175–2179. [Google Scholar] [CrossRef] [PubMed]
- Dorozhkin, S.V.; Dorozhkina, E.I. Crystallization from a milk-based revised simulated body fluid. Biomed. Mater. 2007, 2, 87. [Google Scholar] [CrossRef]
- Macon, A.L.; Kim, T.B.; Valliant, E.M.; Goetschius, K.; Brow, R.K.; Day, D.E.; Hoppe, A.; Boccaccini, A.R.; Kim, I.Y.; Ohtsuki, C. A unified in vitro evaluation for apatite-forming ability of bioactive glasses and their variants. J. Mater. Sci. Mater. Med. 2015, 26, 115. [Google Scholar] [CrossRef]
- Mozafari, M.; Banijamali, S.; Baino, F.; Kargozar, S.; Hill, R.G. Calcium carbonate: Adored and ignored in bioactivity assessment. Acta Biomater. 2019, 91, 35–47. [Google Scholar] [CrossRef]
- Hench, L.L. Bioceramics: From concept to clinic. J. Am. Ceram. Soc. 1991, 74, 1487–1510. [Google Scholar] [CrossRef]
- Rehman, I.; Hench, L.; Bonfield, W.; Smith, R. Analysis of surface layers on bioactive glasses. Biomaterials 1994, 15, 865–870. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, L.; Shi, M.; Zhai, D.; Zhu, H.; Chang, J.; Wu, C.; Zheng, X.; Yin, J. Mesoporous bioactive glass nanolayer-modified zirconia coatings on Ti-6Al-4V with improved in vitro bioactivity. Int. J. Appl. Glass Sci. 2016, 7, 216–228. [Google Scholar] [CrossRef]
- Omar, S.A.; Ballarre, J.; Ceré, S. Protection and functionalization of AISI 316 L stainless steel for orthopedic implants: Hybrid coating and sol gel glasses by spray to promote bioactivity. Electrochim. Acta 2016, 203, 309–315. [Google Scholar] [CrossRef]
- Kuo, P.H.; Joshi, S.S.; Lu, X.; Ho, Y.H.; Xiang, Y.; Dahotre, N.B.; Du, J. Laser coating of bioactive glasses on bioimplant titanium alloys. Int. J. Appl. Glass Sci. 2019, 10, 307–320. [Google Scholar] [CrossRef]
- Baino, F.; Verné, E. Glass-based coatings on biomedical implants: A state-of-the-art review. Biomed. Glasses 2017, 3, 1–17. [Google Scholar] [CrossRef]
- Duan, K.; Wang, R. Surface modifications of bone implants through wet chemistry. J. Mater. Chem. 2006, 16, 2309–2321. [Google Scholar] [CrossRef]
- Gruian, C.; Vanea, E.; Simon, S.; Simon, V. FTIR and XPS studies of protein adsorption onto functionalized bioactive glass. Biochim. Biophys. Acta (BBA)-Proteins Proteomics 2012, 1824, 873–881. [Google Scholar] [CrossRef] [PubMed]
- Filippini, P.; Rainaldi, G.; Ferrante, A.; Mecheri, B.; Gabrielli, G.; Bombace, M.; Indovina, P.L.; Santini, M.T. Modulation of osteosarcoma cell growth and differentiation by silane-modified surfaces. J. Biomed. Mater. Res. 2001, 55, 338–349. [Google Scholar] [CrossRef]
- Ferraris, S.; Vernè, E. Surface Functionalization of Bioactive Glasses: Reactive Groups, Biomolecules and Drugs on Bioactive Surfaces for Smart and Functional Biomaterials. In Bioactive Glasses: Fundamental, Technology and Applications; RSC: Cambridge UK, 2016; pp. 221–235. [Google Scholar]
- Baino, F.; Ferraris, S.; Miola, M.; Verné, E.; Evans, I.; Bretcanu, O. Multifunctional Bioactive Glasses and Glass-Ceramics: Beyond ‘Traditional’ Bioactivity. In Biomedical, Therapeutic and Clinical Applications of Bioactive Glasses; Elsevier: Duxford, UK, 2019; pp. 35–67. [Google Scholar]
- Chang, J.; Zhou, Y. Surface modification of bioactive glasses. In Bioactive Glasses, 2nd ed.; Elsevier: Duxford, UK, 2017; pp. 119–143. [Google Scholar]
- Wu, C.; Zhang, Y.; Ke, X.; Xie, Y.; Zhu, H.; Crawford, R.; Xiao, Y. Bioactive mesopore-glass microspheres with controllable protein-delivery properties by biomimetic surface modification. J. Biomed. Mater. Res. Part A 2010, 95, 476–485. [Google Scholar] [CrossRef]
- Lee, W.-H.; Loo, C.-Y.; Rohanizadeh, R. A review of chemical surface modification of bioceramics: Effects on protein adsorption and cellular response. Colloids Surf. B Biointerfaces 2014, 122, 823–834. [Google Scholar] [CrossRef]
- Spriano, S.; Yamaguchi, S.; Baino, F.; Ferraris, S. A critical review of multifunctional titanium surfaces: New frontiers for improving osseointegration and host response, avoiding bacteria contamination. Acta Biomater. 2018, 79, 1–22. [Google Scholar] [CrossRef]
- Izquierdo-Barba, I.; Vallet-Regí, M. Mesoporous bioactive glasses: Relevance of their porous structure compared to that of classical bioglasses. Biomed. Glasses 2015, 1, 140–150. [Google Scholar] [CrossRef]
- Wu, C.; Chang, J. Mesoporous bioactive glasses: Structure characteristics, drug/growth factor delivery and bone regeneration application. Interface Focus 2012, 2, 292–306. [Google Scholar] [CrossRef]
- Baino, F.; Fiume, E.; Miola, M.; Verné, E. Bioactive sol-gel glasses: Processing, properties, and applications. Int. J. Appl. Ceram. Technol. 2018, 15, 841–860. [Google Scholar] [CrossRef]
- Baino, F.; Fiume, E.; Barberi, J.; Kargozar, S.; Marchi, J.; Massera, J.; Verné, E. Processing methods for making porous bioactive glass-based scaffolds—A state-of-the-art review. Int. J. Appl. Ceram. Technol. 2019, 16, 1762–1796. [Google Scholar] [CrossRef]
- Baino, F. Bioactive glasses—When glass science and technology meet regenerative medicine. Ceram. Int. 2018, 44, 14953–14966. [Google Scholar] [CrossRef]
- Kargozar, S.; Hamzehlou, S.; Baino, F. Can bioactive glasses be useful to accelerate the healing of epithelial tissues? Mater. Sci. Eng. C 2019, 97, 1009–1020. [Google Scholar] [CrossRef]
- Baino, F.; Hamzehlou, S.; Kargozar, S. Bioactive Glasses: Where Are We and Where Are We Going? J. Funct. Biomater. 2018, 9, 25. [Google Scholar] [CrossRef]
- Kargozar, S.; Hamzehlou, S.; Baino, F. Potential of Bioactive Glasses for Cardiac and Pulmonary Tissue Engineering. Materials 2017, 10, 1429. [Google Scholar] [CrossRef]
- Verné, E.; Vitale-Brovarone, C.; Bui, E.; Bianchi, C.; Boccaccini, A. Surface functionalization of bioactive glasses. J. Biomed. Mater. Res. Part A Off. J. Soc. Biomater. Jpn. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2009, 90, 981–992. [Google Scholar] [CrossRef]
- Verné, E.; Ferraris, S.; Vitale-Brovarone, C.; Cochis, A.; Rimondini, L. Bioactive glass functionalized with alkaline phosphatase stimulates bone extracellular matrix deposition and calcification in vitro. Appl. Surf. Sci. 2014, 313, 372–381. [Google Scholar] [CrossRef]
- Verné, E.; Ferraris, S.; Cassinelli, C.; Boccaccini, A. Surface functionalization of Bioglass® with alkaline phosphatase. Surf. Coat. Technol. 2015, 264, 132–139. [Google Scholar] [CrossRef]
- Hum, J.; Boccaccini, A. Collagen as coating material for 45S5 bioactive glass-based scaffolds for bone tissue engineering. Int. J. Mol. Sci. 2018, 19, 1807. [Google Scholar] [CrossRef]
- Chen, Q.; Rezwan, K.; Armitage, D.; Nazhat, S.; Boccaccini, A. The surface functionalization of 45S5 Bioglass®-based glass-ceramic scaffolds and its impact on bioactivity. J. Mater. Sci. Mater. Med. 2006, 17, 979–987. [Google Scholar] [CrossRef] [PubMed]
- Gruian, C.; Boehme, S.; Simon, S.; Steinhoff, H.-J.; Klare, J. Assembly and function of the tRNA-modifying GTPase MnmE adsorbed to surface functionalized bioactive glass. ACS Appl. Mater. Interfaces 2014, 6, 7615–7625. [Google Scholar] [CrossRef] [PubMed]
- Lusvardi, G.; Malavasi, G.; Menabue, L.; Shruti, S. Gallium-containing phosphosilicate glasses: Functionalization and in-vitro bioactivity. Mater. Sci. Eng. C 2013, 33, 3190–3196. [Google Scholar] [CrossRef] [PubMed]
- Larranaga, A.; Petisco, S.; Sarasua, J. Improvement of thermal stability and mechanical properties of medical polyester composites by plasma surface modification of the bioactive glass particles. Polym. Degrad. Stab. 2013, 98, 1717–1723. [Google Scholar] [CrossRef]
- Lopes, J.H.; Fonseca, E.M.B.; Mazali, I.O.; Magalhães, A.; Landers, R.; Bertran, C.A. Facile and innovative method for bioglass surface modification: Optimization studies. Mater. Sci. Eng. C 2017, 72, 86–97. [Google Scholar] [CrossRef]
- Li, X.; Cai, S.; Zhang, W.; Xu, G.; Zhou, W. Effect of pH values on surface modification and solubility of phosphate bioglass-ceramics in the CaO–P2O5–Na2O–SrO–ZnO system. Appl. Surf. Sci. 2009, 255, 9241–9243. [Google Scholar] [CrossRef]
- Zhu, H.; Hu, C.; Zhang, F.; Feng, X.; Li, J.; Liu, T.; Chen, J.; Zhang, J. Preparation and antibacterial property of silver-containing mesoporous 58S bioactive glass. Mater. Sci. Eng. C 2014, 42, 22–30. [Google Scholar] [CrossRef]
- Mishra, M.; Muthuprasanna, P.; Prabha, K.S.; Rani, P.S.; Babu, I.A.S.; Chandiran, I.S.; Arunachalam, G.; Shalini, S. Basics and potential applications of surfactants—A review. Int. J. PharmTech Res. 2009, 1, 1354–1365. [Google Scholar]
- Sagnella, S.; Mai-Ngam, K. Chitosan based surfactant polymers designed to improve blood compatibility on biomaterials. Colloids Surf. B Biointerfaces 2005, 42, 147–155. [Google Scholar] [CrossRef]
- Mitchell, M.J.; Castellanos, C.A.; King, M.R. Surfactant functionalization induces robust, differential adhesion of tumor cells and blood cells to charged nanotube-coated biomaterials under flow. Biomaterials 2015, 56, 179–186. [Google Scholar] [CrossRef]
- Bonici, A.; Lusvardi, G.; Malavasi, G.; Menabue, L.; Piva, A. Synthesis and characterization of bioactive glasses functionalized with Cu nanoparticles and organic molecules. J. Eur. Ceram. Soc. 2012, 32, 2777–2783. [Google Scholar] [CrossRef]
- Aina, V.; Marchis, T.; Laurenti, E.; Diana, E.; Lusvardi, G.; Malavasi, G.; Menabue, L.; Cerrato, G.; Morterra, C. Functionalization of sol gel bioactive glasses carrying Au nanoparticles: Selective Au affinity for amino and thiol ligand groups. Langmuir 2010, 26, 18600–18605. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Li, Y.; Li, L.; Zhao, W.; Li, L.; Gao, J.; Ruan, M.; Shi, J. Functionalization and bioactivity in vitro of mesoporous bioactive glasses. J. Non-Cryst. Solids 2008, 354, 3799–3805. [Google Scholar] [CrossRef]
- Chen, Q.-Z.; Rezwan, K.; Françon, V.; Armitage, D.; Nazhat, S.N.; Jones, F.H.; Boccaccini, A.R. Surface functionalization of Bioglass®-derived porous scaffolds. Acta Biomater. 2007, 3, 551–562. [Google Scholar] [CrossRef]
- El-Fiqi, A.; Lee, J.H.; Lee, E.-J.; Kim, H.-W. Collagen hydrogels incorporated with surface-aminated mesoporous nanobioactive glass: Improvement of physicochemical stability and mechanical properties is effective for hard tissue engineering. Acta Biomater. 2013, 9, 9508–9521. [Google Scholar] [CrossRef]
- Manzano, M.; Aina, V.; Arean, C.; Balas, F.; Cauda, V.; Colilla, M.; Delgado, M.; Vallet-Regi, M. Studies on MCM-41 mesoporous silica for drug delivery: Effect of particle morphology and amine functionalization. Chem. Eng. J. 2008, 137, 30–37. [Google Scholar] [CrossRef]
- Aina, V.; Malavasi, G.; Magistris, C.; Cerrato, G.; Martra, G.; Viscardi, G.; Menabue, L.; Lusvardi, G. Conjugation of amino-bioactive glasses with 5-aminofluorescein as probe molecule for the development of pH sensitive stimuli-responsive biomaterials. J. Mater. Sci. Mater. Med. 2014, 25, 2243–2253. [Google Scholar] [CrossRef][Green Version]
- Aina, V.; Ghigo, D.; Marchis, T.; Cerrato, G.; Laurenti, E.; Morterra, C.; Malavasi, G.; Lusvardi, G.; Menabue, L.; Bergandi, L. Novel bio-conjugate materials: Soybean peroxidase immobilized on bioactive glasses containing Au nanoparticles. J. Mater. Chem. 2011, 21, 10970–10981. [Google Scholar] [CrossRef]
- Schickle, K.; Zurlinden, K.; Bergmann, C.; Lindner, M.; Kirsten, A.; Laub, M.; Telle, R.; Jennissen, H.; Fischer, H. Synthesis of novel tricalcium phosphate-bioactive glass composite and functionalization with rhBMP-2. J. Mater. Sci. Mater. Med. 2011, 22, 763–771. [Google Scholar] [CrossRef]
- Chen, Q.; Ahmed, I.; Knowles, J.; Nazhat, S.; Boccaccini, A.; Rezwan, K. Collagen release kinetics of surface functionalized 45S5 Bioglass®-based porous scaffolds. J. Biomed. Mater. Res. Part A Off. J. Soc. Biomater. Jpn. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2008, 86, 987–995. [Google Scholar] [CrossRef]
- Verné, E.; Ferraris, S.; Vitale-Brovarone, C.; Spriano, S.; Bianchi, C.L.; Naldoni, A.; Morra, M.; Cassinelli, C. Alkaline phosphatase grafting on bioactive glasses and glass ceramics. Acta Biomater. 2010, 6, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Ferraris, S.; Vitale-Brovarone, C.; Bretcanu, O.; Cassinelli, C.; Vernè, E. Surface functionalization of 3D glass—Ceramic porous scaffolds for enhanced mineralization in vitro. Appl. Surf. Sci. 2013, 271, 412–420. [Google Scholar] [CrossRef]
- adhesion of tumor cells and blood cells to charged nanotube-coated biomaterials under flow. Biomaterials 2015, 56, 179–186. [CrossRef]
- Wang, S.; Wen, S.; Shen, M.; Guo, R.; Cao, X.; Wang, J.; Shi, X. Aminopropyltriethoxysilane-mediated surface functionalization of hydroxyapatite nanoparticles: Synthesis, characterization, and in vitro toxicity assay. Int. J. Nanomed. 2011, 6, 3449–3459. [Google Scholar]
- Magyari, K.; Baia, L.; Vulpoi, A.; Simon, S.; Popescu, O.; Simon, V. Bioactivity evolution of the surface functionalized bioactive glasses. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015, 103, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Guo, C.; Zhao, N. Preparation and characterization of the sol—Gel nano-bioactive glasses modified by the coupling agent gamma—Aminopropyltriethoxysilane. Appl. Surf. Sci. 2008, 255, 466–468. [Google Scholar] [CrossRef]
- Curran, J.M.; Chen, R.; Hunt, J.A. Controlling the phenotype and function of mesenchymal stem cells in vitro by adhesion to silane-modified clean glass surfaces. Biomaterials 2005, 26, 7057–7067. [Google Scholar] [CrossRef]
- Stanić, V. Variation in properties of bioactive glasses after surface modification. In Clinical Applications of Biomaterials; Springer: Berlin, Germany, 2017; pp. 35–63. [Google Scholar]
- Massera, J.; Mishra, A.; Guastella, S.; Ferraris, S.; Verné, E. Surface functionalization of phosphate-based bioactive glasses with 3-aminopropyltriethoxysilane (APTS). Biomed. Glasses 2016, 2, 51–62. [Google Scholar] [CrossRef]
- Ferraris, S.; Nommeots-Nomm, A.; Spriano, S.; Vernè, E.; Massera, J. Surface reactivity and silanization ability of borosilicate and Mg-Sr-based bioactive glasses. Appl. Surf. Sci. 2019, 475, 43–55. [Google Scholar] [CrossRef]
- Ozmen, M.; Can, K.; Akin, I.; Arslan, G.; Tor, A.; Cengeloglu, Y.; Ersoz, M. Surface modification of glass beads with glutaraldehyde: Characterization and their adsorption property for metal ions. J. Hazard. Mater. 2009, 171, 594–600. [Google Scholar] [CrossRef]
- Gruian, C.; Vulpoi, A.; Steinhoff, H.-J.; Simon, S. Structural changes of methemoglobin after adsorption on bioactive glass, as a function of surface functionalization and salt concentration. J. Mol. Struct. 2012, 1015, 20–26. [Google Scholar] [CrossRef]
- Leivo, J.; Virjula, S.; Vanhatupa, S.; Kartasalo, K.; Kreutzer, J.; Miettinen, S.; Kallio, P. A durable and biocompatible ascorbic acid-based covalent coating method of polydimethylsiloxane for dynamic cell culture. J. R. Soc. Interface 2017, 14, 20170318. [Google Scholar] [CrossRef] [PubMed]
- Gruian, C.; Vulpoi, A.; Vanea, E.; Oprea, B.; Steinhoff, H.-J.; Simon, S. The attachment affinity of hemoglobin toward silver-containing bioactive glass functionalized with glutaraldehyde. J. Phys. Chem. B 2013, 117, 16558–16564. [Google Scholar] [CrossRef] [PubMed]
- Wiącek, A.E.; Gozdecka, A.; Jurak, M.; Przykaza, K.; Terpiłowski, K. Wettability of plasma modified glass surface with bioglass layer in polysaccharide solution. Colloids Surf. A Physicochem. Eng. Asp. 2018, 551, 185–194. [Google Scholar] [CrossRef]
- Araújo, M.; Viveiros, R.; Philippart, A.; Miola, M.; Doumett, S.; Baldi, G.; Perez, J.; Boccaccini, A.R.; Aguiar-Ricardo, A.; Verné, E. Bioactivity, mechanical properties and drug delivery ability of bioactive glass-ceramic scaffolds coated with a natural-derived polymer. Mater. Sci. Eng. C 2017, 77, 342–351. [Google Scholar] [CrossRef]
- Srdić, V.V.; Mojić, B.; Nikolić, M.; Ognjanović, S. Recent progress on synthesis of ceramics core/shell nanostructures. Matrix 2013, 13, 14. [Google Scholar] [CrossRef]
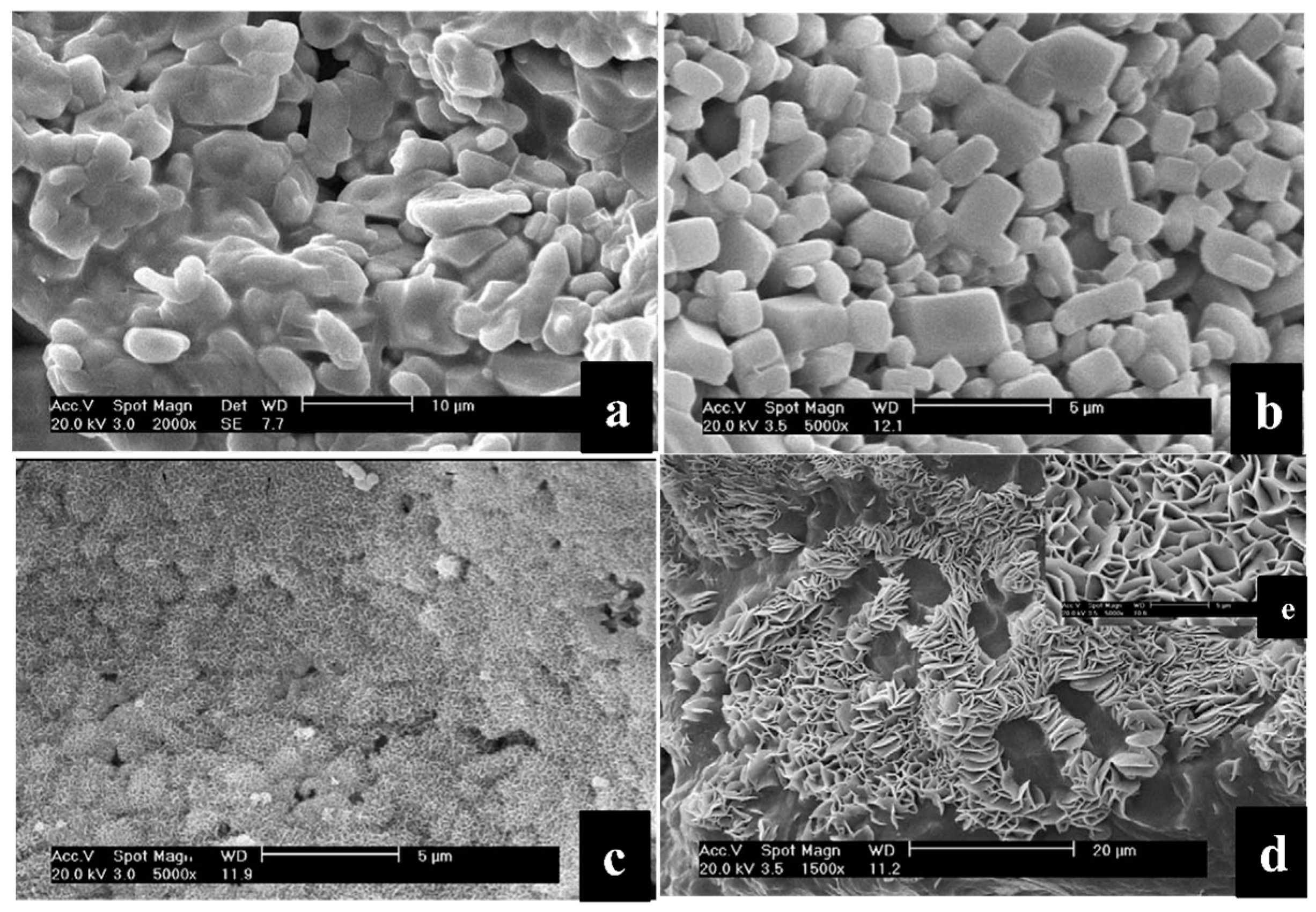
- Verné, E.; Ferraris, S.; Miola, M.; Fucale, G.; Maina, G.; Martinasso, G.; Canuto, R.A.; Di Nunzio, S.; Vitale-Brovarone, C. Synthesis and characterisation of bioactive and antibacterial glass–ceramic Part 1–Microstructure, properties and biological behaviour. Adv. Appl. Ceram. 2008, 107, 234–244. [Google Scholar] [CrossRef]
- Verné, E.; Miola, M.; Brovarone, C.V.; Cannas, M.; Gatti, S.; Fucale, G.; Maina, G.; Massé, A.; Di Nunzio, S. Surface silver-doping of biocompatible glass to induce antibacterial properties. Part I: Massive glass. J. Mater. Sci. Mater. Med. 2009, 20, 733–740. [Google Scholar] [CrossRef]
- Vernè, E.; Di Nunzio, S.; Bosetti, M.; Appendino, P.; Brovarone, C.V.; Maina, G.; Cannas, M. Surface characterization of silver-doped bioactive glass. Biomaterials 2005, 26, 5111–5119. [Google Scholar] [CrossRef]
- Miola, M.; Ferraris, S.; Di Nunzio, S.; Robotti, P.; Bianchi, G.; Fucale, G.; Maina, G.; Cannas, M.; Gatti, S.; Massé, A. Surface silver-doping of biocompatible glasses to induce antibacterial properties. Part II: Plasma sprayed glass-coatings. J. Mater. Sci. Mater. Med. 2009, 20, 741. [Google Scholar] [CrossRef]
- Verné, E.; Ferraris, S.; Miola, M.; Fucale, G.; Maina, G.; Robotti, P.; Bianchi, G.; Martinasso, G.; Canuto, R.A.; Vitale-Brovarone, C. Synthesis and characterisation of bioactive and antibacterial glass-ceramic Part 2—Plasma spray coatings on metallic substrates. Adv. Appl. Ceram. 2008, 107, 245–253. [Google Scholar] [CrossRef]
- Farag, M.; Abd-Allah, W.; Ahmed, H.Y. Study of the dual effect of gamma irradiation and strontium substitution on bioactivity, cytotoxicity, and antimicrobial properties of 45S5 bioglass. J. Biomed. Mater. Res. Part A 2017, 105, 1646–1655. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.; Kedia, S.; Singh, A.K.; Sharma, K.; Sinha, S. Surface treatment of 45S5 Bioglass using femtosecond laser to achieve superior growth of hydroxyapatite. J. Laser Appl. 2017, 29, 022004. [Google Scholar] [CrossRef]
- Pou, P.; Riveiro, A.; del Val, J.; Comesaña, R.; Penide, J.; Arias-González, F.; Soto, R.; Lusquiños, F.; Pou, J. Laser surface texturing of Titanium for bioengineering applications. Procedia Manuf. 2017, 13, 694–701. [Google Scholar] [CrossRef]
- Zhao, S.; Zhang, J.; Zhu, M.; Zhang, Y.; Liu, Z.; Ma, Y.; Zhu, Y.; Zhang, C. Effects of functional groups on the structure, physicochemical and biological properties of mesoporous bioactive glass scaffolds. J. Mater. Chem. B 2015, 3, 1612–1623. [Google Scholar] [CrossRef]
- Shaikh, S.; Singh, D.; Subramanian, M.; Kedia, S.; Singh, A.K.; Singh, K.; Gupta, N.; Sinha, S. Femtosecond laser induced surface modification for prevention of bacterial adhesion on 45S5 bioactive glass. J. Non-Cryst. Solids 2018, 482, 63–72. [Google Scholar] [CrossRef]
- Zheng, K.; Lu, M.; Liu, Y.; Chen, Q.; Taccardi, N.; Hüser, N.; Boccaccini, A.R. Monodispersed lysozyme-functionalized bioactive glass nanoparticles with antibacterial and anticancer activities. Biomed. Mater. 2016, 11, 035012. [Google Scholar] [CrossRef]
- Lin, H.-M.; Lin, H.-Y.; Chan, M.-H. Preparation, characterization, and in vitro evaluation of folate-modified mesoporous bioactive glass for targeted anticancer drug carriers. J. Mater. Chem. B 2013, 1, 6147–6156. [Google Scholar] [CrossRef]
- Vernè, E.; Miola, M.; Ferraris, S.; Bianchi, C.L.; Naldoni, A.; Maina, G.; Bretcanu, O. Surface activation of a ferrimagnetic glass—Ceramic for antineoplastic drugs grafting. Adv. Eng. Mater. 2010, 12, B309–B319. [Google Scholar] [CrossRef]
- Cazzola, M.; Verné, E.; Cochis, A.; Sorrentino, R.; Azzimonti, B.; Prenesti, E.; Rimondini, L.; Ferraris, S. Bioactive glasses functionalized with polyphenols: In vitro interactions with healthy and cancerous osteoblast cells. J. Mater. Sci. 2017, 52, 9211–9223. [Google Scholar] [CrossRef]
- Cazzola, M.; Corazzari, I.; Prenesti, E.; Bertone, E.; Vernè, E.; Ferraris, S. Bioactive glass coupling with natural polyphenols: Surface modification, bioactivity and anti-oxidant ability. Appl. Surf. Sci. 2016, 367, 237–248. [Google Scholar] [CrossRef]
- Dziadek, M.; Dziadek, K.; Zagrajczuk, B.; Menaszek, E.; Cholewa-Kowalska, K. Poly (ε-caprolactone)/bioactive glass composites enriched with polyphenols extracted from sage (Salvia officinalis L.). Mater. Lett. 2016, 183, 386–390. [Google Scholar] [CrossRef]
- Schuhladen, K.; Roether, J.A.; Boccaccini, A.R. Bioactive glasses meet phytotherapeutics: The potential of natural herbal medicines to extend the functionality of bioactive glasses. Biomaterials 2019, 217, 119288. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhao, L.; Liang, Q.; Ye, J.; Komatsu, N.; Zhang, Q.; Gao, W.; Xu, M.; Chen, X. Cationic polyarginine conjugated mesoporous bioactive glass nanoparticles with polyglycerol coating for efficient DNA delivery. J. Biomed. Nanotechnol. 2017, 13, 280–289. [Google Scholar] [CrossRef] [PubMed]


| Glass/Composition | Agent | Techniques | Remarks | Ref (s) |
|---|---|---|---|---|
| 45S5 BG (46.1SiO2-24.4Na2O-26.9CaO-2.6P2O5 mol.%) | Alkaline phosphatase (ALP) | Immersed in solution | Increased enzymatic activity | [40,41,42] |
| 45S5 BG (46.1SiO2-24.4Na2O-26.9CaO-2.6P2O5 mol.%) | (3-aminopropyl) triethoxysilane (APTS) | Immersed in solution | Improving the mechanical stability Promoting the formation of spherical HCA layer on the surface of BGs Increasing the kinetics of the release of collagen Increasing the surface roughness | [43] |
| 45S5 BG (46.1SiO2-24.4Na2O-26.9CaO-2.6P2O5 mol.%) | APTS/GA | Immersed in solution | Enhancing the protein adsorption and collagen release Reducing the aggressiveness of the adsorption process of proteins Improving the stability of the protein attachment onto BGs | [44,45] |
| 45Ca30 BG (45.7SiO2-24.1Na2O-26.6CaO-2.6P2O5-1.0Ga2O3 mol.%) | Tetraethoxysilane (TEOS) | Immersed in solution | Facilitating the formation of silica layer with negativity charge around BGs Increasing the surface roughness | [46] |
| 45S5 BG (46.1SiO2-24.4Na2O-26.9CaO-2.6P2O5 mol.%) | - | plasma | A rapid and clean method | [47] |
| 45S5 BG (46.1SiO2-24.4Na2O-26.9CaO-2.6P2O5 mol.%) | - | Core-shell based system | Accelerating HCA layer formation | [48] |
| Phosphate glass-ceramics (CaO-P2O5-Na2O-SrO-ZnO) | HF, HCl, NH3 | Immersed in solutions with various pH values | Showing critical role of pH on the surface morphology of the materials | [49] |
| Mesoporous 58S BG (60SiO2-36CaO-4P2O5 mol.%) | KH550 | Immersed in solution | Improving the loading Enhancing the antibacterial effect | [50] |
| Functional Group | Method of Introduction | Function | Ref (s) |
|---|---|---|---|
| SH | 2-mercapto-1 ethanol or 6 mercapto-1hexanol grafting | Improve further protein and drug grafting | [54,55] |
| COOH/OH | Triethoxysilylpropyl succinic anhydride or tetraethoxysilane grafting | Improve further protein and drug grafting | [56,57] |
| NH2 | 3-aminopropyl-triethoxysilane grafting (most used), 2-amino-1 ethanol, 6 amino-1 hexanol, 2 ethanolamine or Cysteamine grafting (occasionally reported) | [24,40,41,42,46,54,55,56,57,58,59,60,61,62,63,64,65] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kargozar, S.; Kermani, F.; Mollazadeh Beidokhti, S.; Hamzehlou, S.; Verné, E.; Ferraris, S.; Baino, F. Functionalization and Surface Modifications of Bioactive Glasses (BGs): Tailoring of the Biological Response Working on the Outermost Surface Layer. Materials 2019, 12, 3696. https://doi.org/10.3390/ma12223696
Kargozar S, Kermani F, Mollazadeh Beidokhti S, Hamzehlou S, Verné E, Ferraris S, Baino F. Functionalization and Surface Modifications of Bioactive Glasses (BGs): Tailoring of the Biological Response Working on the Outermost Surface Layer. Materials. 2019; 12(22):3696. https://doi.org/10.3390/ma12223696
Chicago/Turabian StyleKargozar, Saeid, Farzad Kermani, Sahar Mollazadeh Beidokhti, Sepideh Hamzehlou, Enrica Verné, Sara Ferraris, and Francesco Baino. 2019. "Functionalization and Surface Modifications of Bioactive Glasses (BGs): Tailoring of the Biological Response Working on the Outermost Surface Layer" Materials 12, no. 22: 3696. https://doi.org/10.3390/ma12223696
APA StyleKargozar, S., Kermani, F., Mollazadeh Beidokhti, S., Hamzehlou, S., Verné, E., Ferraris, S., & Baino, F. (2019). Functionalization and Surface Modifications of Bioactive Glasses (BGs): Tailoring of the Biological Response Working on the Outermost Surface Layer. Materials, 12(22), 3696. https://doi.org/10.3390/ma12223696







