Evaluating the Wear of Resin Teeth by Different Opposing Restorative Materials
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Specimens
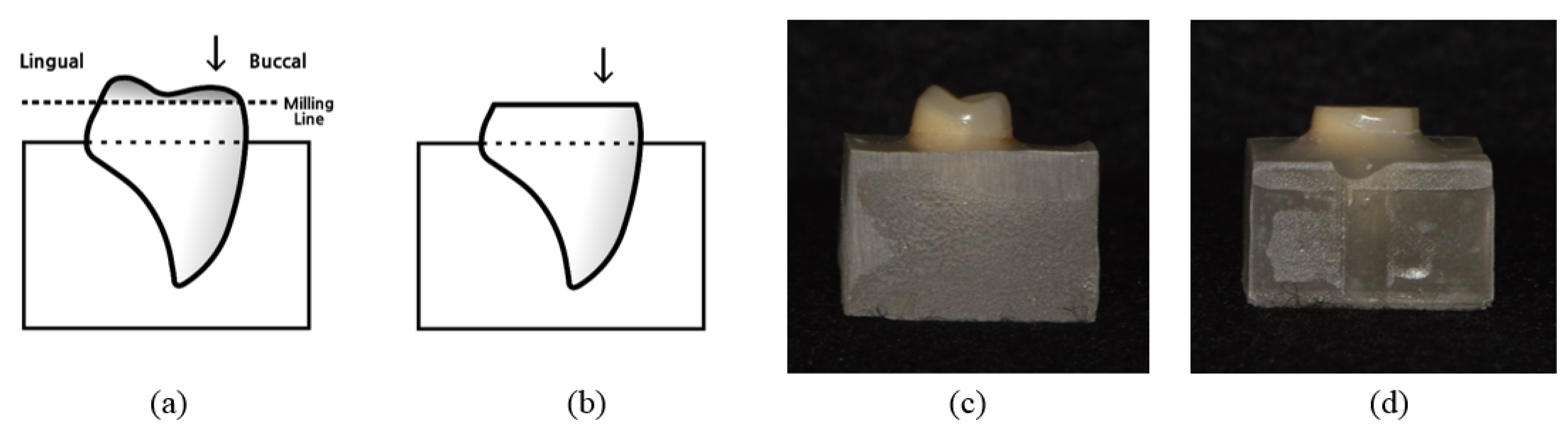
2.2.1. Fabrication of Specimens of Resin Teeth
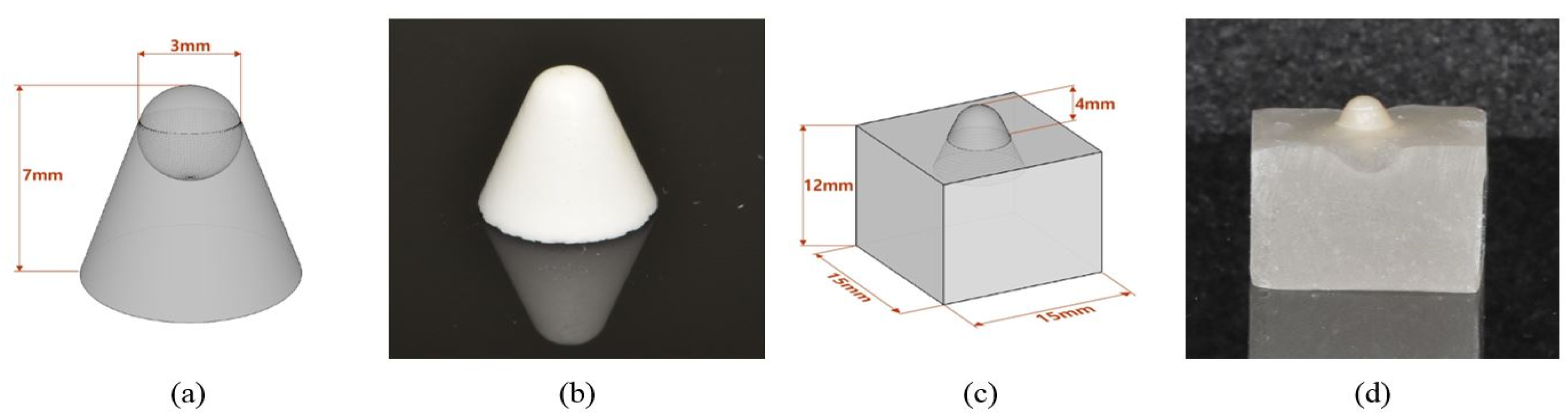
2.2.2. Fabrication of Restorative Material Specimens
2.3. Methods
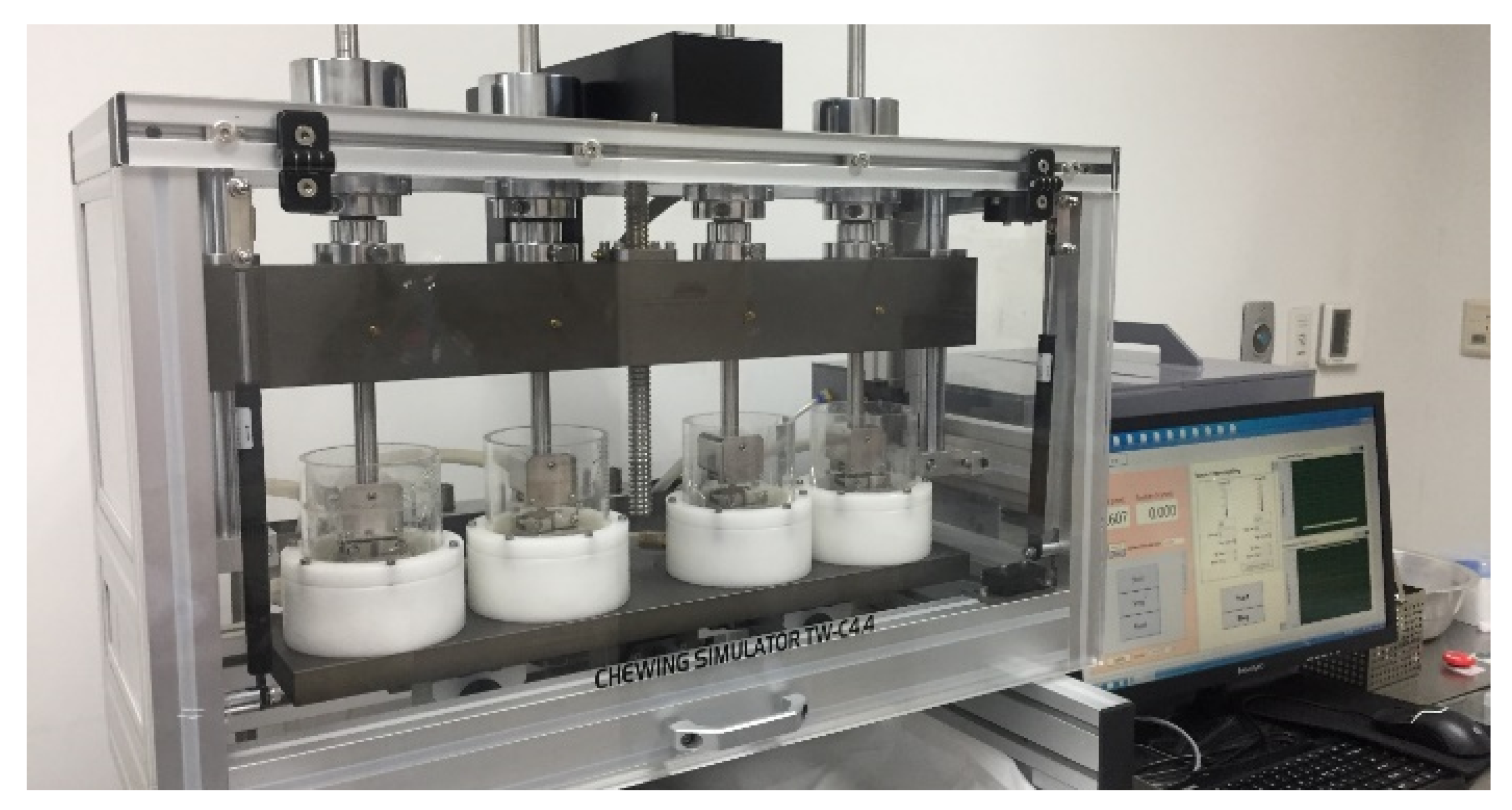
2.3.1. Wear Test
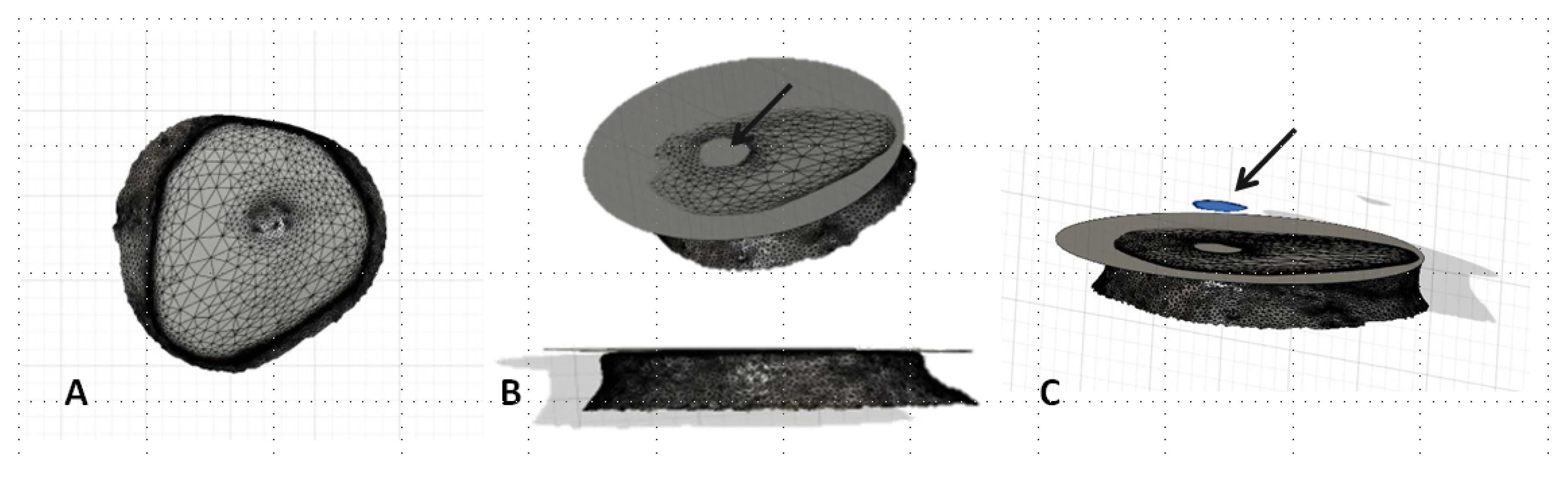
2.3.2. Wear Measurement
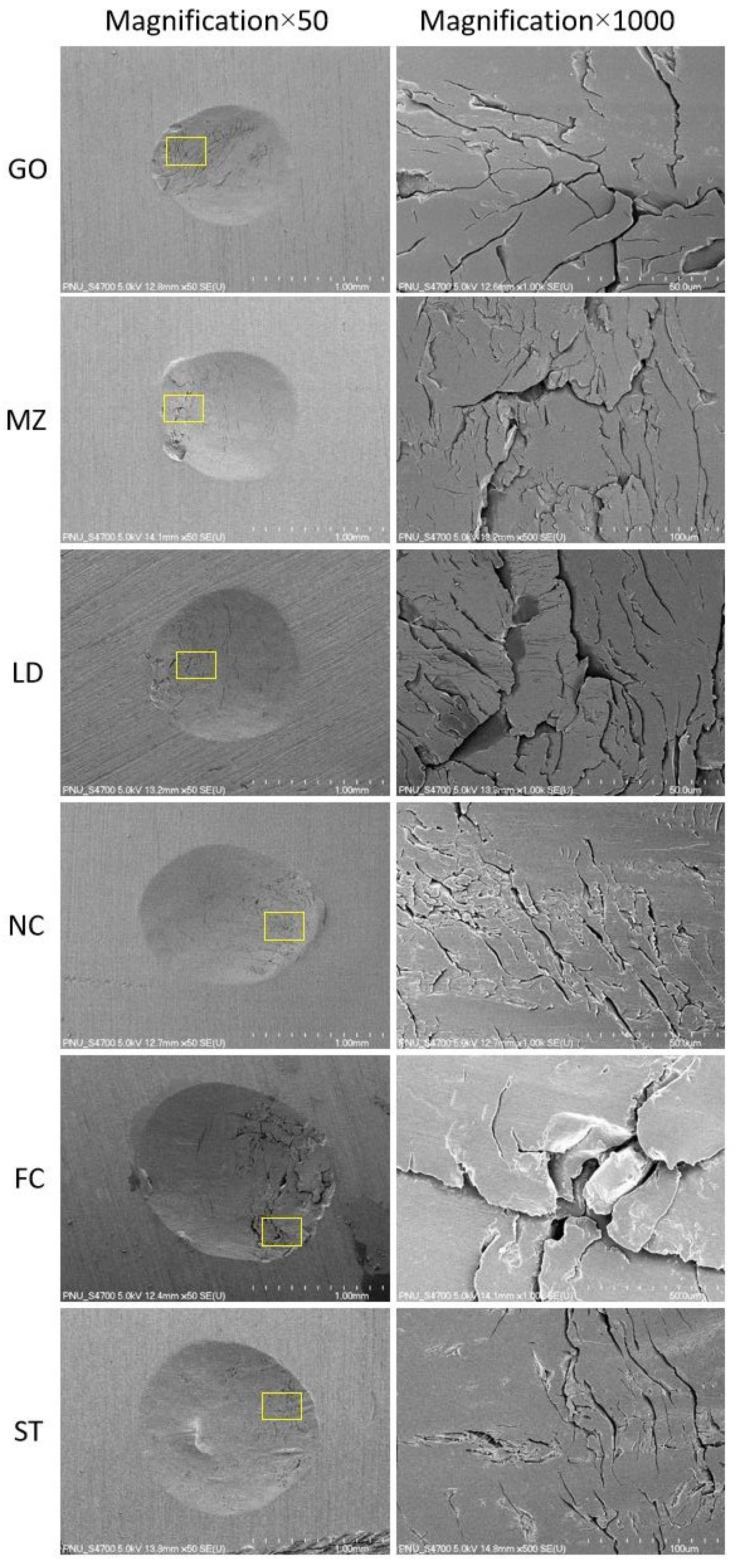
2.3.3. Scanning Electron Microscopy Evaluation (SEM) Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hayakawa, I.; Hirano, S.; Takahashi, Y.; Keh, E.S. Changes in the masticatory function of complete denture wearers after relining the mandibular denture with a soft denture liner. Int. J. Prosthodont. 2000, 13, 227–231. [Google Scholar] [PubMed]
- Wenz, H.J.; Hertrampf, K.; Lehmann, K.M. Clinical longevity of removable partial dentures retained by telescopic crowns: Outcome of the double crown with clearance fit. Int. J. Prosthodont. 2001, 14, 207–213. [Google Scholar] [PubMed]
- Bani, D.; Bani, T.; Bergamini, M. Morphologic and biochemical changes of the masseter muscles induced by occlusal wear: Studies in a rat model. J. Dent. Res. 1999, 78, 1735–1744. [Google Scholar] [CrossRef] [PubMed]
- Wedel, A.; Borrman, H.; Carlsson, G.E. Tooth wear and temporomandibular joint morphology in a skull material from the 17th century. Swed. Dent. J. 1998, 22, 85–95. [Google Scholar]
- Ghazal, M.; Hedderich, J.; Kern, M. Wear of feldspathic ceramic, nano-filled composite resin and acrylic resin artificial teeth when opposed to different antagonists. Eur. J. Oral Sci. 2008, 116, 585–592. [Google Scholar] [CrossRef]
- Sambataro, S.; Cervino, G.; Bocchieri, S.; La Bruna, R.; Cicciù, M. TMJ Dysfunctions Systemic Implications and Postural Assessments: A Review of Recent Literature. J. Funct. Morphol. Kinesiol. 2019, 4, 58. [Google Scholar] [CrossRef]
- Zeng, J.; Sato, Y.; Ohkubo, C.; Hosoi, T. In vitro wear resistance of three types of composite resin denture teeth. J. Prosthet. Dent. 2005, 94, 453–457. [Google Scholar] [CrossRef]
- Kamonwanon, P.; Yodmongkol, S.; Chantarachindawong, R.; Thaweeboon, S.; Thaweeboon, B.; Srikhirin, T. Wear resistance of a modified polymethyl methacrylate artificial tooth compared to five commercially available artificial tooth materials. J. Prosthet. Dent. 2015, 114, 286–292. [Google Scholar] [CrossRef]
- Munshi, N.; Rosenblum, M.; Jiang, S.; Flinton, R. In Vitro Wear Resistance of Nano-Hybrid Composite Denture Teeth. J. Prosthodont. 2017, 26, 224–229. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Vanini, L.; Rondoni, G.D.; Pirani, M.; Vadini, M.; Gattone, M.; De Angelis, F. Wear properties of a novel resin composite compared to human enamel and other restorative materials. Oper. Dent. 2014, 39, 612–618. [Google Scholar] [CrossRef]
- Ghazal, M.; Yang, B.; Ludwig, K.; Kern, M. Two-body wear of resin and ceramic denture teeth in comparison to human enamel. Dent. Mater. 2008, 24, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Ohlmann, B.; Rohstock, K.; Kugler, J.; Gilde, H.; Dreyhaupt, J.; Stober, T. Influences on clinical wear of acrylic denture teeth: A pilot study. Int. J. Prosthodont. 2007, 20, 496–498. [Google Scholar] [PubMed]
- Kim, S.K.; Kim, K.N.; Chang, I.T.; Heo, S.J. A study of the effects of chewing patterns on occlusal wear. J. Oral Rehabil. 2001, 28, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
- Ekfeldt, A.; øilo, G. Wear mechanisms of resin and porcelain denture teeth. Acta Odontol. Scand. 1989, 47, 391–399. [Google Scholar] [CrossRef]
- Oh, W.S.; DeLong, R.; Anusavice, K.J. Factors affecting enamel and ceramic wear: A literature review. J. Prosthet. Dent. 2002, 87, 451–459. [Google Scholar] [CrossRef]
- Gwon, B.; Bae, E.B.; Lee, J.J.; Cho, W.T.; Bae, H.Y.; Choi, J.W.; Huh, J.B. Wear Characteristics of Dental Ceramic CAD/CAM Materials Opposing Various Dental Composite Resins. Materials 2019, 12, E1839. [Google Scholar] [CrossRef]
- Ghazal, M.; Albashaireh, Z.S.; Kern, M. Wear resistance of nanofilled composite resin and feldspathic ceramic artificial teeth. J. Prosthet. Dent. 2008, 100, 441–448. [Google Scholar] [CrossRef]
- Kim, M.J.; Oh, S.H.; Kim, J.H.; Ju, S.W.; Seo, D.G.; Jun, S.H.; Ryu, J.J. Wear evaluation of the human enamel opposing different Y-TZP dental ceramics and other porcelains. J. Dent. 2012, 40, 979–988. [Google Scholar] [CrossRef]
- Stober, T.; Lutz, T.; Gilde, H.; Rammelsberg, P. Wear of resin denture teeth by two-body contact. Dent. Mater. 2006, 22, 243–249. [Google Scholar] [CrossRef]
- Jung, Y.S.; Lee, J.W.; Choi, Y.J.; Ahn, J.S.; Shin, S.W.; Huh, J.B. A study on the in-vitro wear of the natural tooth structure by opposing zirconia or dental porcelain. J. Adv. Prosthodont. 2010, 2, 111–115. [Google Scholar] [CrossRef]
- Hahnel, S.; Behr, M.; Handel, G.; Rosentritt, M. Two-body wear of artificial acrylic and composite resin teeth in relation to antagonist material. J. Prosthet. Dent. 2009, 101, 269–278. [Google Scholar] [CrossRef]
- Seghi, R.R.; Rosenstiel, S.F.; Bauer, P. Abrasion of human enamel by different dental ceramics in vitro. J. Dent. Res. 1991, 7, 221–225. [Google Scholar] [CrossRef] [PubMed]
- DeLong, R.; Douglas, W.H. An artificial oral environment for testing dental materials. IEEE Trans. Biomed. Eng. 1991, 38, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, C.H.; Mahan, P.E.; Lundeen, H.C.; Brehnan, K.; Walsh, E.K.; Holbrook, W.B. Occlusal forces during chewing and swallowing as measured by sound transmission. J. Prosthet. Dent. 1981, 46, 443–449. [Google Scholar] [CrossRef]
- Suzuki, S. In vitro wear of nano-composite denture teeth. J. Prosthodont. 2004, 13, 238–243. [Google Scholar] [CrossRef]
- Wassell, R.W.; McCabe, J.E.; Walls, A.W.G. A two-body frictional wear test. J. Dent. Res. 1994, 73, 1546–1553. [Google Scholar] [CrossRef]
- Kern, M.; Strub, J.R.; Lü, X.Y. Wear of composite resin veneering materials in a dual-axis chewing simulator. J. Oral Rehabil. 1999, 26, 372–378. [Google Scholar] [CrossRef]
- Krejci, I.; Lutz, F.; Reimer, M.; Heinzmann, J.L. Wear of ceramic inlays, their enamel antagonists, and luting cements. J. Prosthet. Dent. 1993, 69, 425–430. [Google Scholar] [CrossRef]
- Monasky, G.E.; Taylor, D.F. Studies on the wear of porcelain, enamel, and gold. J. Prosthet. Dent. 1971, 25, 299–306. [Google Scholar] [CrossRef]
- Schuh, C.; Kinast, E.J.; Mezzomo, E.; Kapczinski, M.P. Effect of glazed and polished surface finishes on the friction coefficient of two low-fusing ceramics. J. Prosthet. Dent. 2005, 93, 245–252. [Google Scholar] [CrossRef]
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef]
- Elkins, W.E. Gold occlusal surfaces and organic occlusion in denture construction. J. Prosthet. Dent. 1973, 30, 94–98. [Google Scholar] [CrossRef]
- Nedelcu, R.; Olsson, P.; Nyström, I.; Rydén, J.; Thor, A. Accuracy and precision of 3 intraoral scanners and accuracy of conventional impressions: A novel in vivo analysis method. J. Dent. 2018, 69, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Medina-Sotomayor, P.; Pascual, A.; Camps, I. Accuracy of four digital scanners according to scanning strategy in complete-arch impressions. PLoS ONE 2018, 13, e0202916. [Google Scholar] [CrossRef] [PubMed]
- Müller, P.; Ender, A.; Joda, T.; Katsoulis, J. Impact of digital intraoral scan strategies on the impression accuracy using the TRIOS Pod scanner. Quintessence Int. 2016, 47, 343–349. [Google Scholar]
- Giménez, B.; Özcan, M.; Martínez-Rus, F.; Pradies, G. Accuracy of a digital impression system based on parallel confocal laser technology for implants with consideration of operator experience and implant angulation and depth. Int. J. Oral Maxillofac. Implant. 2014, 29, 853–862. [Google Scholar] [CrossRef]
| Materials | Group (Sample Size) | Vickers Hardness (GPa) | Product Name | Manufacturer |
|---|---|---|---|---|
| Resin teeth | - | - | Trubyte Biotone | Dentsply, Philadelphia, PA, USA |
| Type III gold alloy | GO (n = 8) | 0.88–1.17 | Goldnian C-55 | Shinhung, Seoul, Korea |
| Monolithic zirconia | MZ (n = 8) | 13.24 | Luxen | Dentalmax, Seoul, Korea |
| Lithium disilicate | LD (n = 8) | 5.8 | Rosetta SM | HASS, Gangwondo, Korea |
| Ni–Cr alloy | NC (n = 8) | 3.7 | Verabond 2V | Albadent, Fairfield, CA, USA |
| Feldspathic ceramic | FC (n = 8) | 4.97 | Ceramco | Dentsply, Philadelphia, PA, USA |
| Steatite | ST (n = 8) | 5.8 | - | Yamamoto trading, Seoul, Korea |
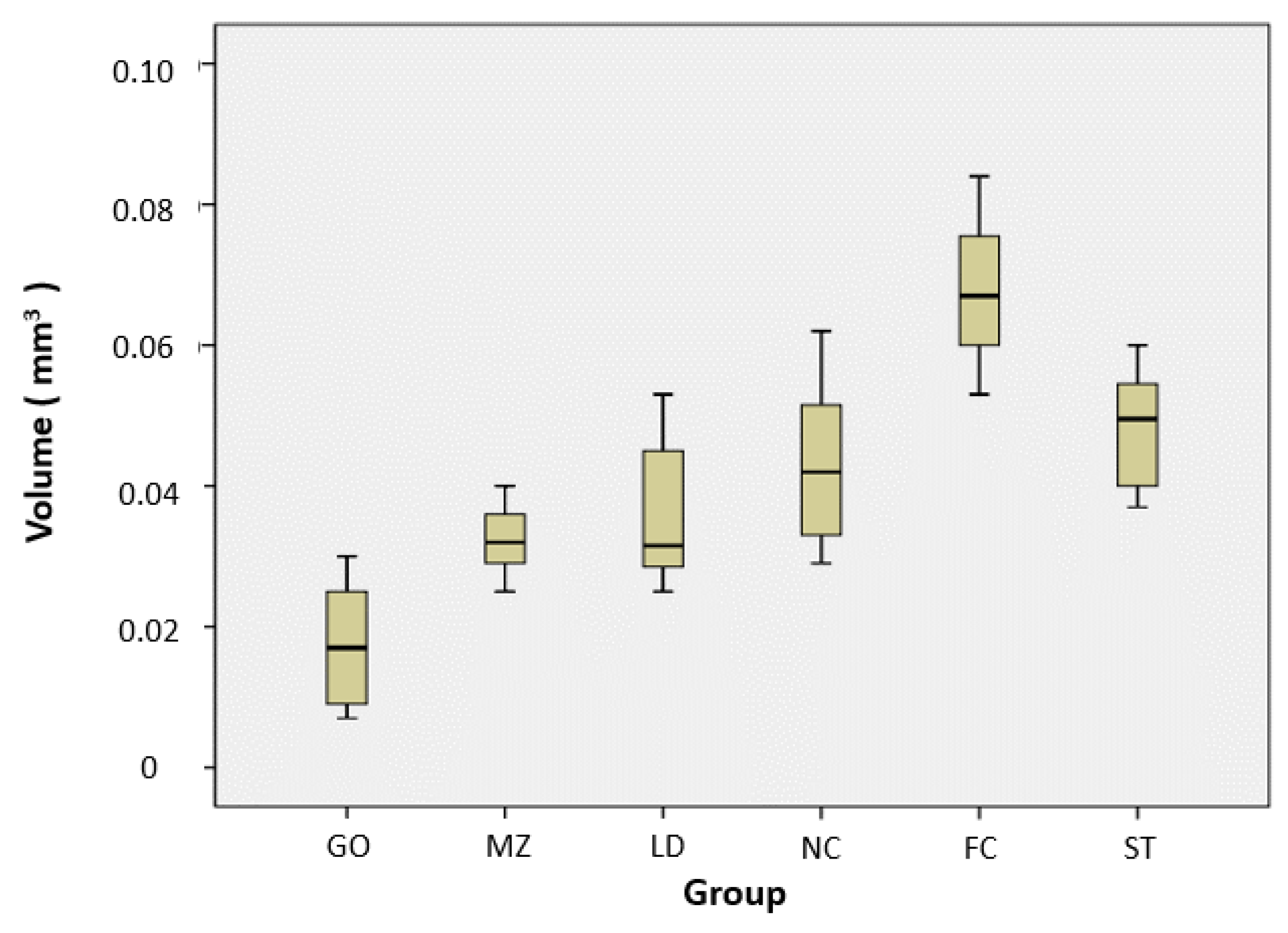
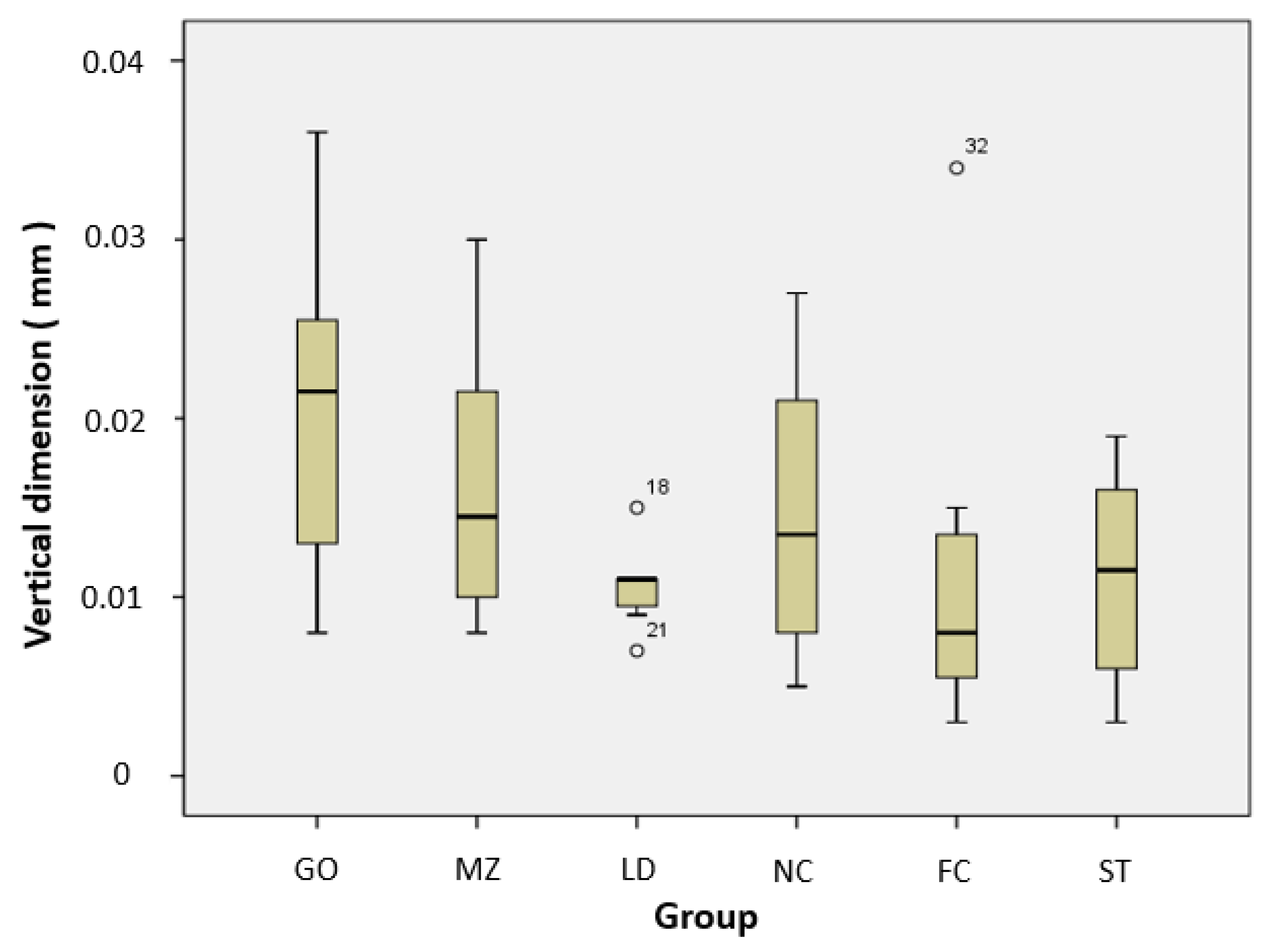
| Group | N | Volume Loss of Resin Teeth (mm3) | Vertical Loss of Restorative Materials (µm) |
|---|---|---|---|
| GO | 8 | 0.017 ± 0.009 a | 0.016 ± 0.008 a |
| MZ | 8 | 0.032 ± 0.005 b | 0.015 ± 0.008 a |
| LD | 8 | 0.036 ± 0.010 b c | 0.011 ± 0.002 a |
| NC | 8 | 0.043 ± 0.012 b c | 0.015 ± 0.011 a |
| FC | 8 | 0.068 ± 0.011 d | 0.020 ± 0.009 a |
| ST | 8 | 0.048 ± 0.009 c | 0.011 ± 0.006 a |
| p | - | <0.001 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, S.; Choi, J.-W.; Jeong, C.-M.; Huh, J.-B.; Lee, S.-H.; Lee, H.; Yun, M.-J. Evaluating the Wear of Resin Teeth by Different Opposing Restorative Materials. Materials 2019, 12, 3684. https://doi.org/10.3390/ma12223684
Jin S, Choi J-W, Jeong C-M, Huh J-B, Lee S-H, Lee H, Yun M-J. Evaluating the Wear of Resin Teeth by Different Opposing Restorative Materials. Materials. 2019; 12(22):3684. https://doi.org/10.3390/ma12223684
Chicago/Turabian StyleJin, Seunglee, Jae-Won Choi, Chang-Mo Jeong, Jung-Bo Huh, So-Hyoun Lee, Hyeonjong Lee, and Mi-Jung Yun. 2019. "Evaluating the Wear of Resin Teeth by Different Opposing Restorative Materials" Materials 12, no. 22: 3684. https://doi.org/10.3390/ma12223684
APA StyleJin, S., Choi, J.-W., Jeong, C.-M., Huh, J.-B., Lee, S.-H., Lee, H., & Yun, M.-J. (2019). Evaluating the Wear of Resin Teeth by Different Opposing Restorative Materials. Materials, 12(22), 3684. https://doi.org/10.3390/ma12223684





