Deformation of the Internal Connection of Narrow Implants after Insertion in Dense Bone: An in Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Bone Samples
2.2. Dental Implants and Experimental Groups
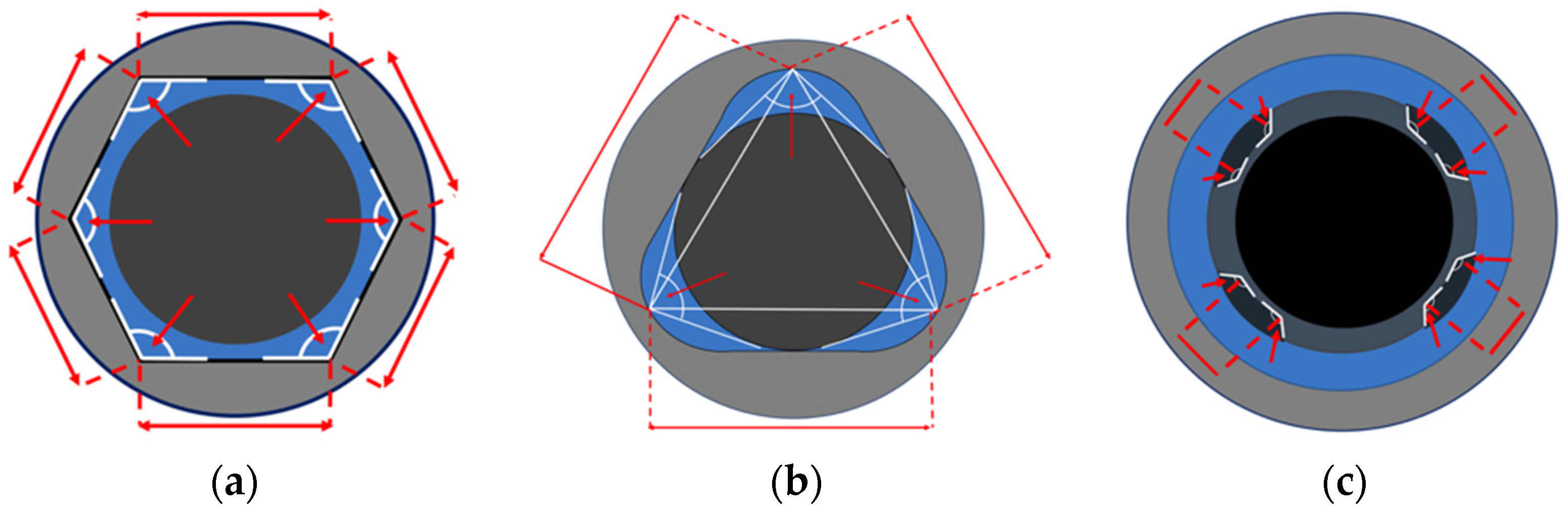
2.2.1. Group A (Internal Hexagonal Connection)
2.2.2. Group B (Internal Three-Channel Connection)
2.2.3. Group C (Internal Four-Channel Connection)
2.3. Standardization of the Implant Insertion
2.4. Experimental Procedures
2.4.1. Evaluation of the Insertion Torque
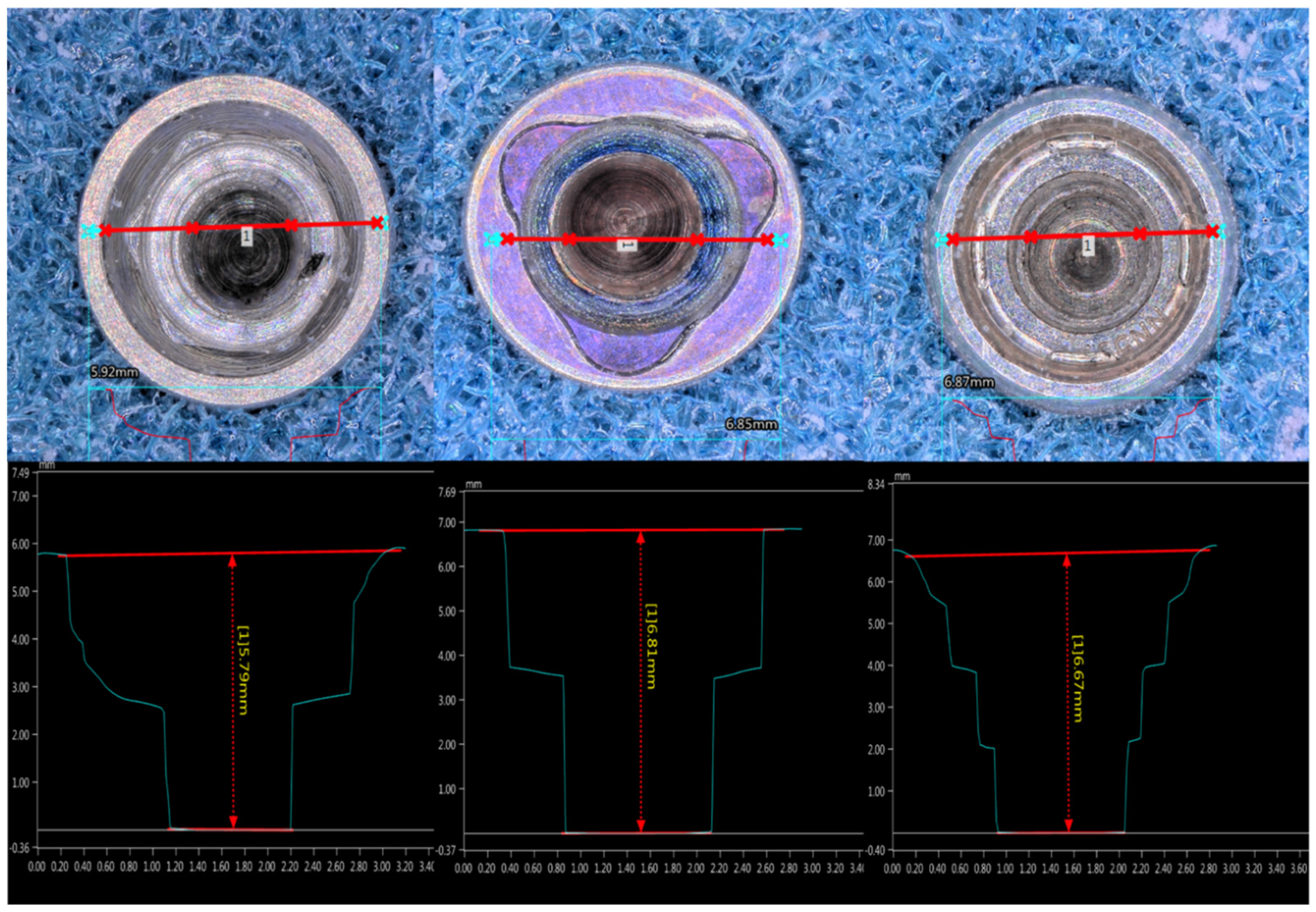
2.4.2. Evaluation of the Implant’s Geometry and Its Deformation
2.4.3. Measurement Procedure
2.5. Statistical Analysis
3. Results
3.1. Qualitative Findings
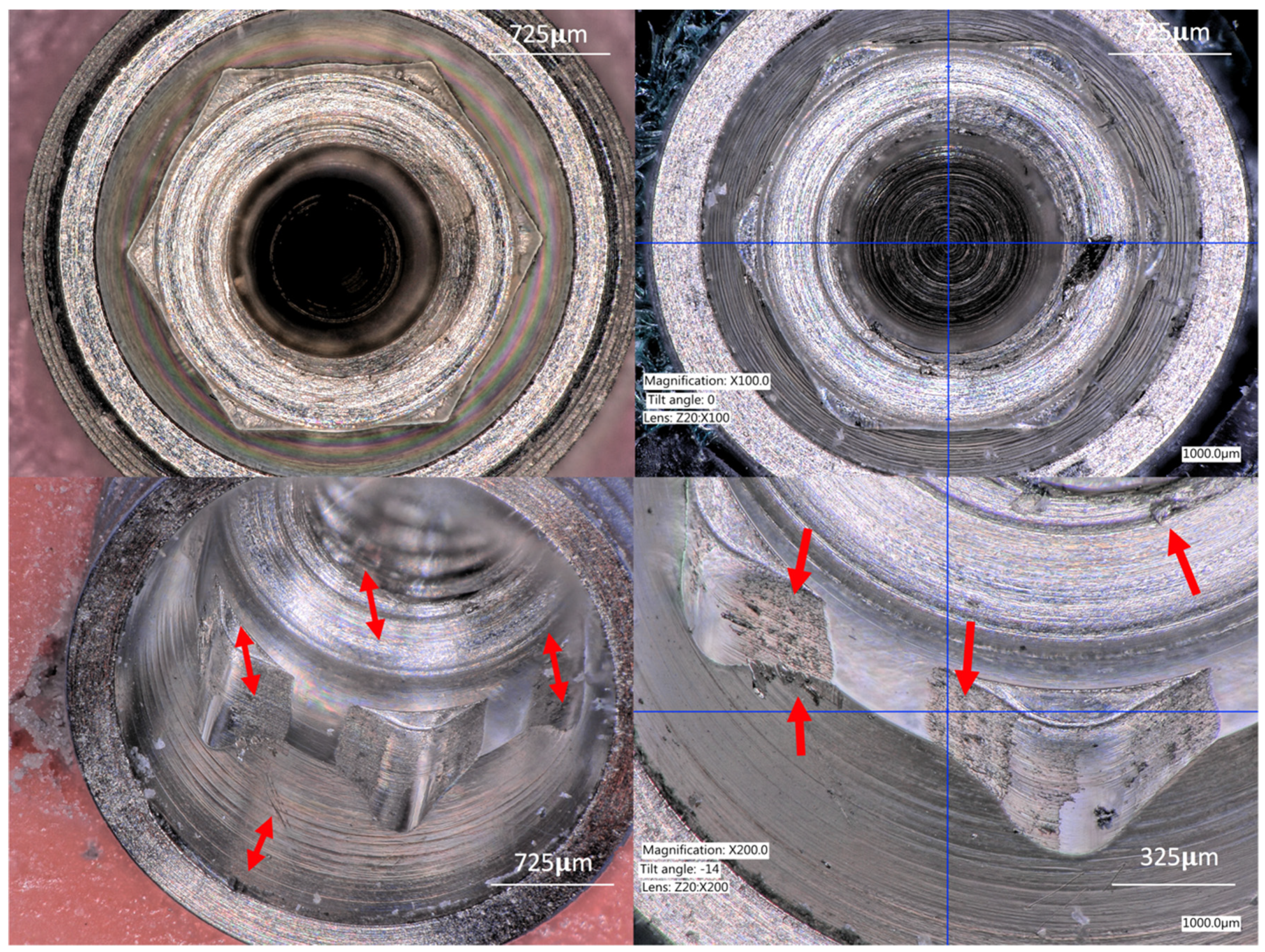
3.1.1. Group A (IC Hexagon)
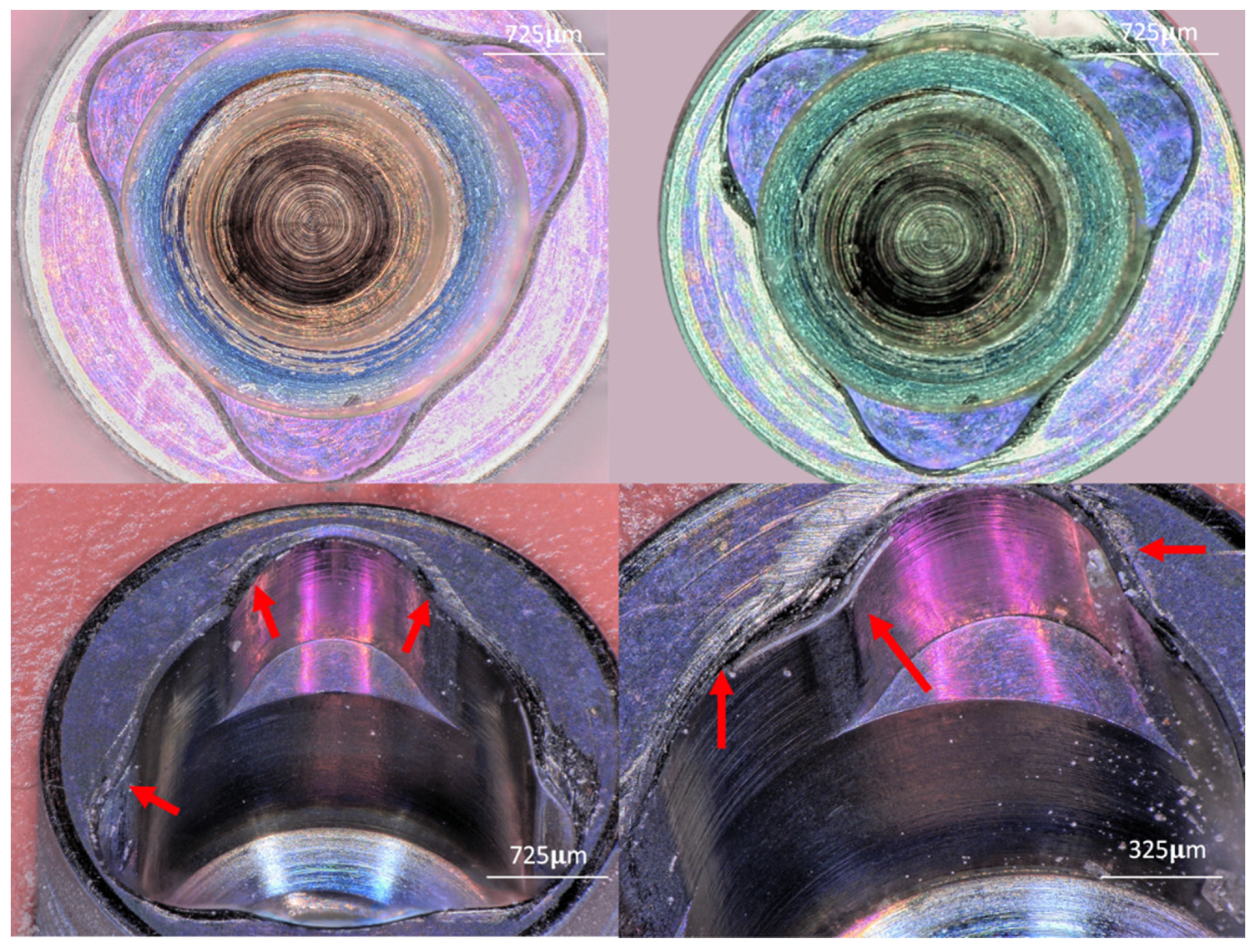
3.1.2. Group B (Three-Channel)
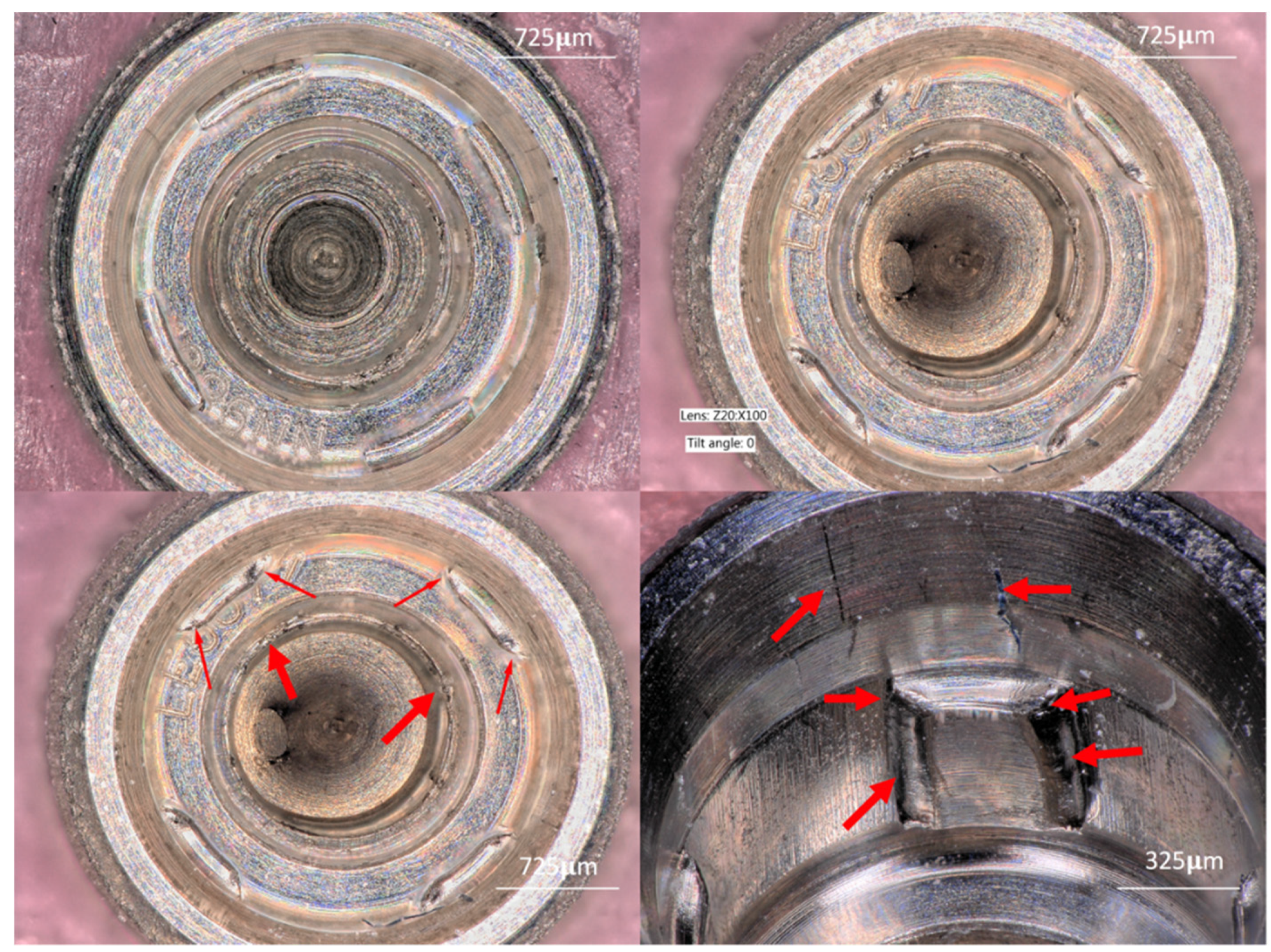
3.1.3. Group C (Four-Channel)
3.2. Quantitative Findings
3.2.1. IT values
3.2.2. Connection Depth
3.3. Geometry Changes
3.3.1. Group A (IC Hexagon)
3.3.2. Group B (IC Three-Channel)
3.3.3. Group C (IC Four-Channel)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- International Congress of Oral Implantologists (ICOI). Glossary of Implant Dentistry; ICOI Editorial: Fairfield, NJ, USA, 2017; p. 63. [Google Scholar]
- Yanase, R.T.; Preston, J.D. Considerations for screw/cylinder prosthetic components. In Reconstructive and Preprosthetic Oral and Maxillofacial Surgery, 2nd ed.; Fonseca, R., Davis, W.H., Eds.; WB Saunders Co.: Philadelphia, PA, USA, 1995; p. 251. [Google Scholar]
- Jalbout, Z.; Tabourian, G. Glossary of Implant Dentistry; ICOI and New York University: New York, NY, USA, 2004. [Google Scholar]
- Salvi, G.E.; Lang, N.P. Changing paradigms in implant dentistry. Crit. Rev. Oral Biol. Med. 2001, 12, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, R.; Gionso, L.; Quaglini, V.; Di Martino, E.; Simion, M. An in vitro study on compensation of mismatch of screw versus cement-retained implant supported fixed prostheses. Clin. Oral Implants Res. 2000, 11, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Binon, P. Evaluation of three slip fit hexagonal implants. Implant Dent. 1996, 5, 235–248. [Google Scholar] [CrossRef] [PubMed]
- The Academy of Prosthodontics; The Academy of Prosthodontics Foundation. The Glossary of Prosthodontic Terms, 9th ed.; Elsevier: St. Louis, MO, USA, 2017. [Google Scholar]
- Balfour, A.; O’Brien, G.R. Comparative study of antirotational single tooth abutments. J. Prosthet. Dent. 1995, 73, 36–43. [Google Scholar] [CrossRef]
- Aboyoussef, H.; Weiner, S.; Ehrenberg, D. Effect of an antirotation resistance form on screw loosening for single implant-supported crowns. J. Prosthet. Dent. 2000, 83, 450–455. [Google Scholar] [CrossRef]
- Teixeira, A.B.; Shimano, A.; Macedo, A.; Valente, M.; dos Reis, A. Influence of torsional strength on different types of dental implant platforms. Implant Dent. 2015, 24, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Dittmer, A.; Dittmer, M.; Kohorst, P.; Jendras, M.; Borchers, L.; Stiesch, M. Effect of implant-abutment connection design on load bearing capacity and failure mode of implants. J. Prosthodont. 2011, 20, 510–516. [Google Scholar] [CrossRef]
- Neto, R.T.; Moura, M.S.; Souza, E.A.; Rubo, J.H. Implant abutment deformation during prosthetic cylinder screw tightening: An in vitro study. Int. J. Prosthodont. 2009, 22, 391–395. [Google Scholar]
- Millington, N.D.; Leung, T. Inaccurate fit of implant superstructures. Part 1: Stresses generated on the superstructure relative to the size of fit discrepancy. Int. J. Prosthodont. 1995, 8, 511–516. [Google Scholar]
- Bordin, D.; Witek, L.; Fardin, V.P.; Bonfante, E.A.; Coelho, P.G. Fatigue Failure of Narrow Implants with Different Implant-Abutment Connection Designs. J. Prosthodont. 2018, 27, 659–664. [Google Scholar] [CrossRef]
- Hecker, D.M.; Eckert, S.E. Cyclic loading of implant-supported prostheses: Changes in component fit over time. J. Prosthet. Dent. 2003, 89, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, K.; Homma, S.; Takanashi, T.; Takemoto, S.; Furuya, F.; Yoshinari, M.; Yajima, Y. Influence of eccentric cyclic loading on implant components: Comparison between external joint system and internal joint system. Dent. Mater. J. 2016, 35, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Micarelli, C.; Canullo, L.; GIannello, L. Implant-abutment connection deformation after prosthetic procedures: An in vitro study. Int. J. Prosthodont. 2015, 28, 282–286. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, J.H.; Huh, Y.H.; Park, C.J.; Cho, L.R. Effect of the Coronal Wall Thickness of Dental Implants on the Screw Joint Stability in the Internal Implant-Abutment Connection. Int. J. Oral Maxillofac. Implants 2016, 31, 1058–1065. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.; Schmelzeisen, R.; Taylor, T.D.; Zabler, S.; Wiest, W.; Fretwurst, T. The Impact of Force Transmission on Narrow-Body Dental Implants Made of Commercially Pure Titanium and Titanium Zirconia Alloy with a Conical Implant-Abutment Connection: An Experimental Pilot Study. Int. J. Oral Maxillofac. Implants 2016, 31, 1066–1071. [Google Scholar] [CrossRef] [PubMed]
- Imam, A.Y.; Moshaverinia, A.; McGlumphy, E.A. Implant-abutment interface: A comparison of the ultimate force to failure among narrow diameter implant systems. J. Prosthet. Dent. 2014, 112, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.H.; Han, C.H.; Kim, S.J.; Chang, J.S. The change of rotational freedom following different insertion torques in three implant systems with implant driver. J. Adv. Prosthodont. 2009, 1, 37–40. [Google Scholar] [CrossRef]
- Gurgel-Juarez, N.C.; De Almeida, E.O.; Rocha, E.P.; Freitas, A.C.; Anchieta, R.B.; de Vargas, L.C.; Kina, S.; Franca, F.M. Regular and platform switching: Bone stress analysis varying implant type. J. Prosthodont. 2012, 21, 160–166. [Google Scholar] [CrossRef]
- Peñarrocha-Oltra, D.; Rossetti, P.; Covani, U.; Galluccio, F.; Canullo, L. Microbial Leakage at the Implant-Abutment Connection Due to Implant Insertion Maneuvers: Cross-Sectional Study 5 Years Postloading in Healthy Patients. J. Oral Implantol. 2015, 41, 292–296. [Google Scholar] [CrossRef]
- Calvert, K.L.; Trumble, K.P.; Webster, T.J.; Kirkpatrick, L.A. Characterization of commercial rigid polyurethane foams used as bone analogs for implant testing. J. Mater. Sci. Mater. Med. 2010, 21, 1453–1461. [Google Scholar] [CrossRef]
- Nary Filho, H.; Calvo Guirado, J.L.; Matsumoto, M.A.; Bresaola, M.D.; Aur, R. Biomechanical evaluation of resistance to insertion torque of different implant systems and insertion driver types. Implant Dent. 2015, 24, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Lee, S.W.; Leesungbok, R.; Ahn, S. Influence of the connection design and titanium grades of the implant complex on resistance under static loading. J. Adv. Prosthodont. 2016, 8, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Ruiz, R.A.; Romanos, G. Potential Causes of Titanium Particle and Ion Release in Implant Dentistry: A Systematic Review. Int. J. Mol. Sci. 2018, 19, 3585. [Google Scholar] [CrossRef] [PubMed]
- Suárez-López Del Amo, F.; Garaicoa-Pazmiño, C.; Fretwurst, T.; Castilho, R.; Squarize, C. Dental implants-associated release of titanium particles: A systematic review. Clin. Oral Implants Res. 2018, 29, 1085–1100. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, F.; Hiroyasu, K.; Ueda, K. The fracture strength by a torsion test at the implant-abutment interface. Int. J. Implant Dent. 2015, 1, 25. [Google Scholar] [CrossRef] [PubMed]
- English, C.E. Externally hexed implants, abutments, and transfer devices: A comprehensive overview. Implant Dent. 1992, 1, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Dahl, G. The importance of the modulus of elasticity and the rigid connection of dental implants. J. Oral Implantol. 1981, 9, 427–428. [Google Scholar]
| Connection Characteristics | Implant Manufacturer/Line | Coupling System | Implant Index Geometry | Composition | Insertion Device | External Geometry | Diameter | Length |
|---|---|---|---|---|---|---|---|---|
| Group A Straight walls n = 10 | Nobel Biocare Nobel Active | Conical Friction fit Angle 12° | Internal Hexagon Six abutment positions | Cold worked Titanium Grade IV | Implant Driver | Tapered | 3.5 mm | 10 mm |
| Group B Channeled walls n = 10 | Nobel Biocare Nobel Replace | Butt Joint Angle 0° | Three channels Three abutment positions | 3.5 mm | ||||
| Group C Channeled walls n = 10 | Straumann Bone Level | CrossFit Conical Friction fit Angle 15° | Four channels Four abutment positions | Pre-mounted/Transfer | 3.3 mm |
| Angular Deformation | Sample Size | Mean | Q1 | Median | Q3 | p-Value | |
|---|---|---|---|---|---|---|---|
| GROUP A | Vertex Angle Before | 60 | 119.261 | 119.109 | 119.29 | 119.673 | 0.087 |
| Vertex Angle After | 60 | 120.822 | 120.077 | 120.755 | 121.042 | ||
| GROUP B | Channel Angle Before | 30 | 95.254 | 95.056 | 95.21 | 95.369 | 0.092 |
| Channel Angle After | 30 | 96.829 | 95.68 | 96.48 | 97.83 | ||
| GROUP C | Channel Angle Before | 40 | 91.575 | 77.727 | 93.103 | 93.339 | 0.021 |
| Channel Angle After | 40 | 142.325 | 101.763 | 144.368 | 148.281 | ||
| Variable | Sample Size | Mean | Difference Before vs. After | Test Statistic | p-Value | |
|---|---|---|---|---|---|---|
| GROUP A Hexagon Wall Length | Before | 60 | 1005.77 µm | −0.25 | 0.08683 | 0.9511 |
| After | 60 | 1005.52 µm | ||||
| GROUP B Three-Channeled Wall Length | Before | 30 | 2646.90 µm | −22.76 | 2.49081 | 0.08351 |
| After | 30 | 2624.14 µm | ||||
| GROUP C Four-Channeled Wall Length | Before | 40 | 655.89 µm | −186.2140 | 36.18923 | 0.00006 |
| After | 40 | 469.68 µm | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delgado-Ruiz, R.; Silvente, A.N.; Romanos, G. Deformation of the Internal Connection of Narrow Implants after Insertion in Dense Bone: An in Vitro Study. Materials 2019, 12, 1833. https://doi.org/10.3390/ma12111833
Delgado-Ruiz R, Silvente AN, Romanos G. Deformation of the Internal Connection of Narrow Implants after Insertion in Dense Bone: An in Vitro Study. Materials. 2019; 12(11):1833. https://doi.org/10.3390/ma12111833
Chicago/Turabian StyleDelgado-Ruiz, Rafael, Ana Nicolas Silvente, and Georgios Romanos. 2019. "Deformation of the Internal Connection of Narrow Implants after Insertion in Dense Bone: An in Vitro Study" Materials 12, no. 11: 1833. https://doi.org/10.3390/ma12111833
APA StyleDelgado-Ruiz, R., Silvente, A. N., & Romanos, G. (2019). Deformation of the Internal Connection of Narrow Implants after Insertion in Dense Bone: An in Vitro Study. Materials, 12(11), 1833. https://doi.org/10.3390/ma12111833







