Reliability of Orthodontic Miniscrews: Bending and Maximum Load of Different Ti-6Al-4V Titanium and Stainless Steel Temporary Anchorage Devices (TADs)
Abstract
1. Introduction
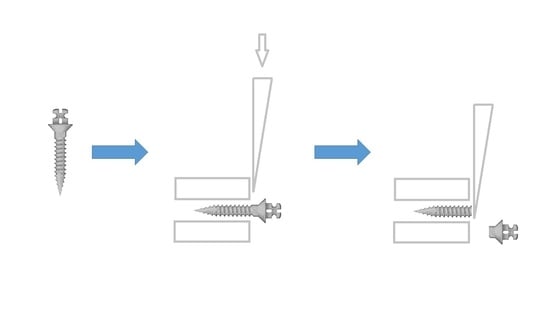
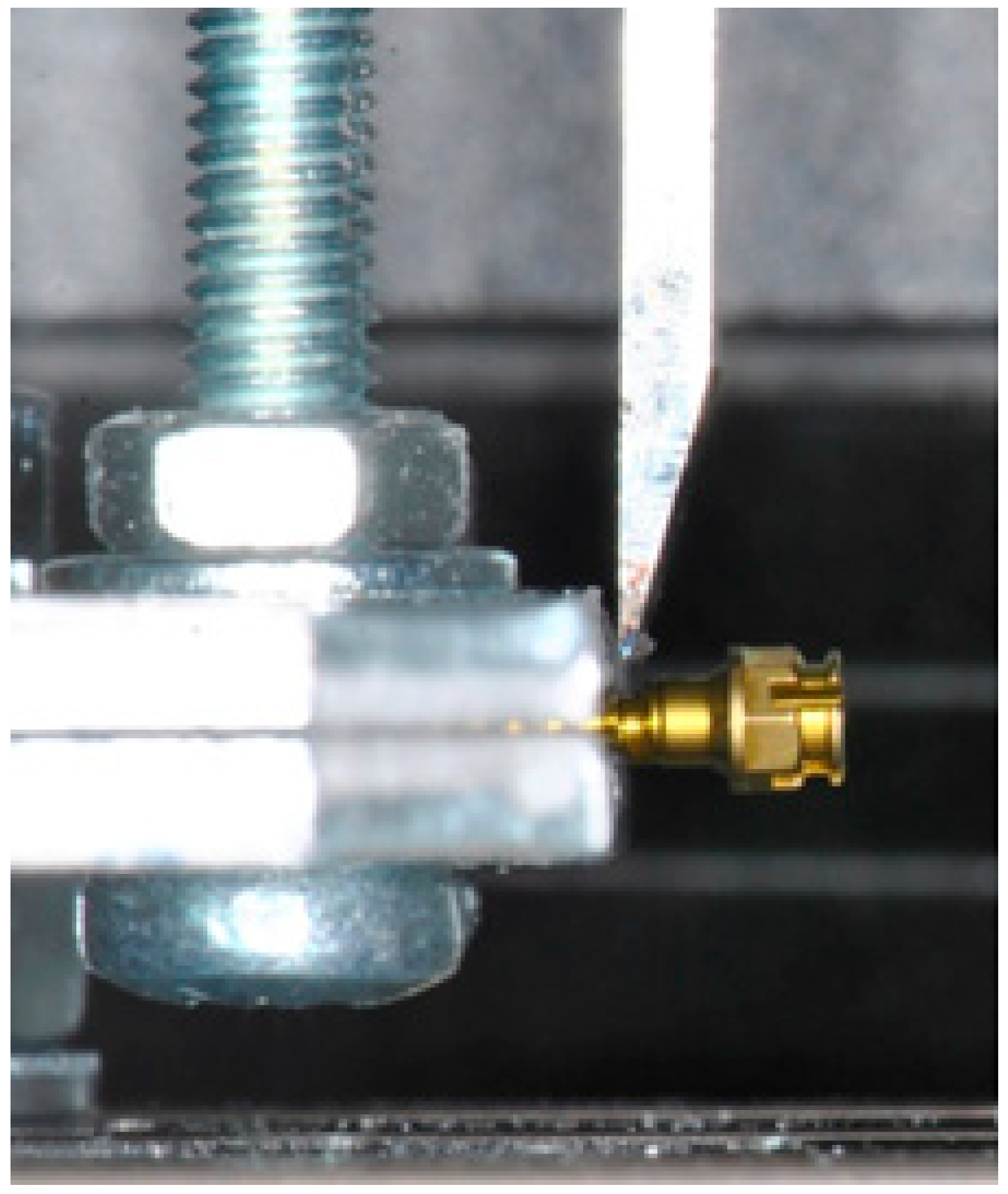
2. Materials and Methods
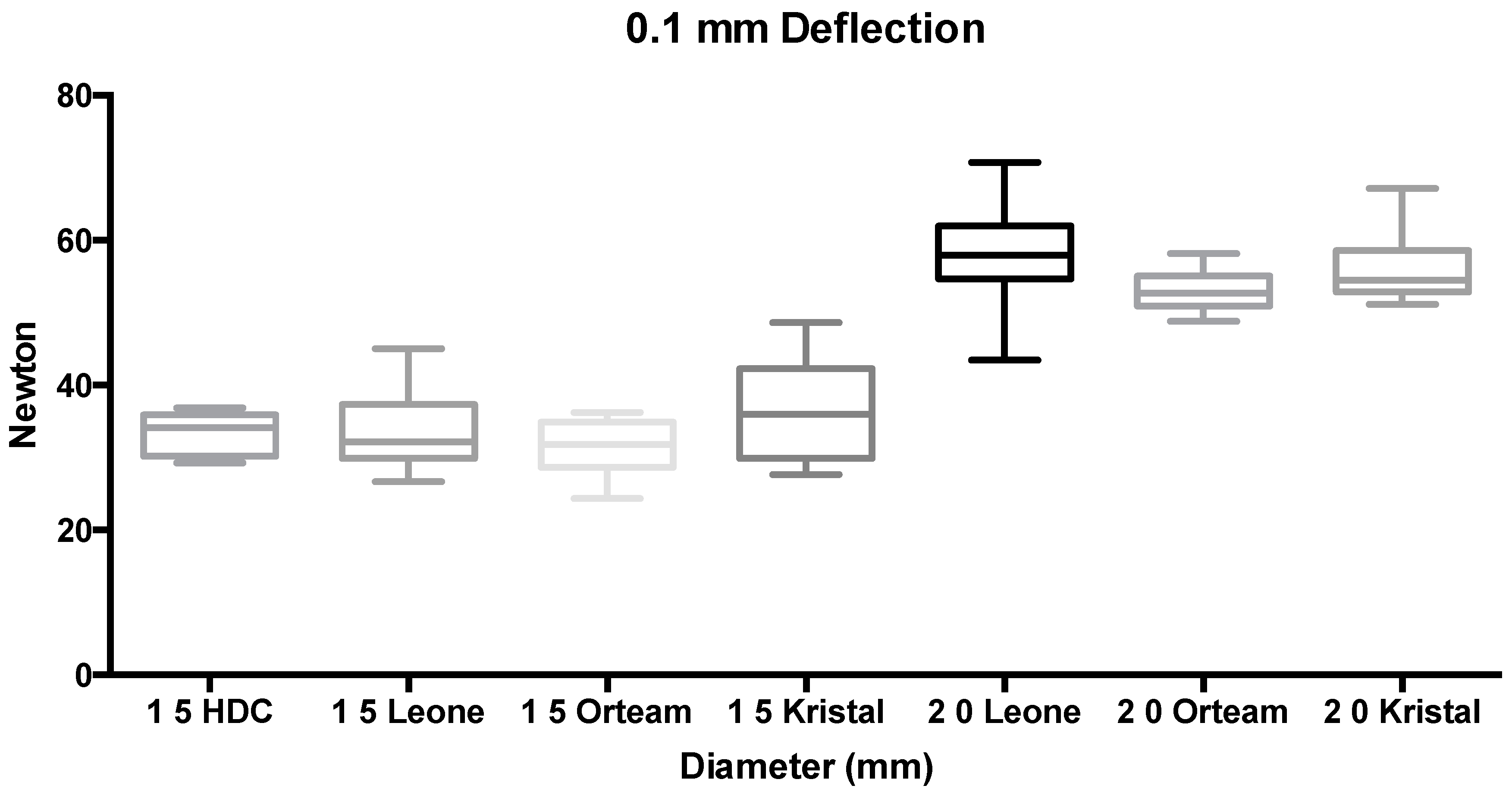
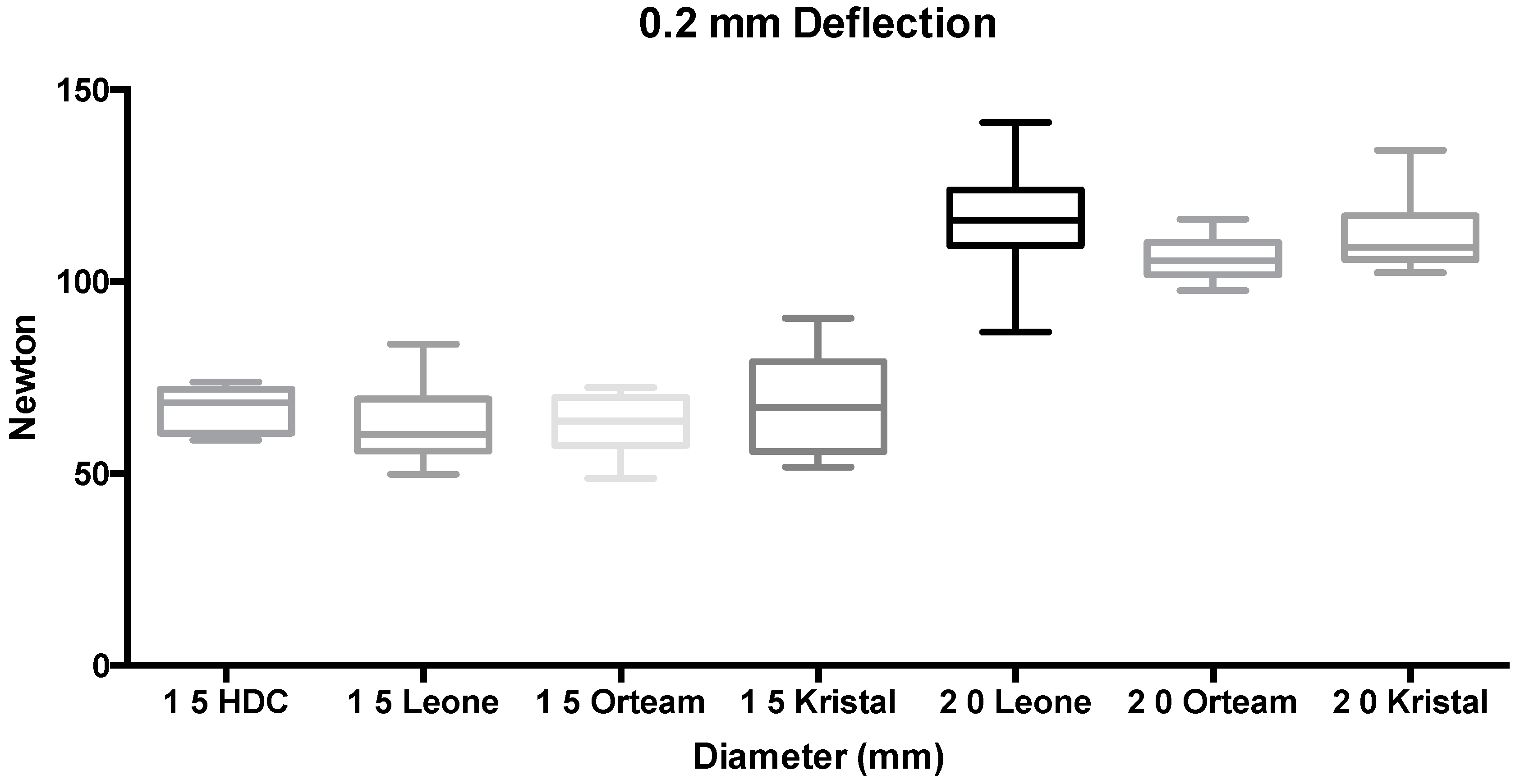
3. Results
4. Discussion
5. Conclusions
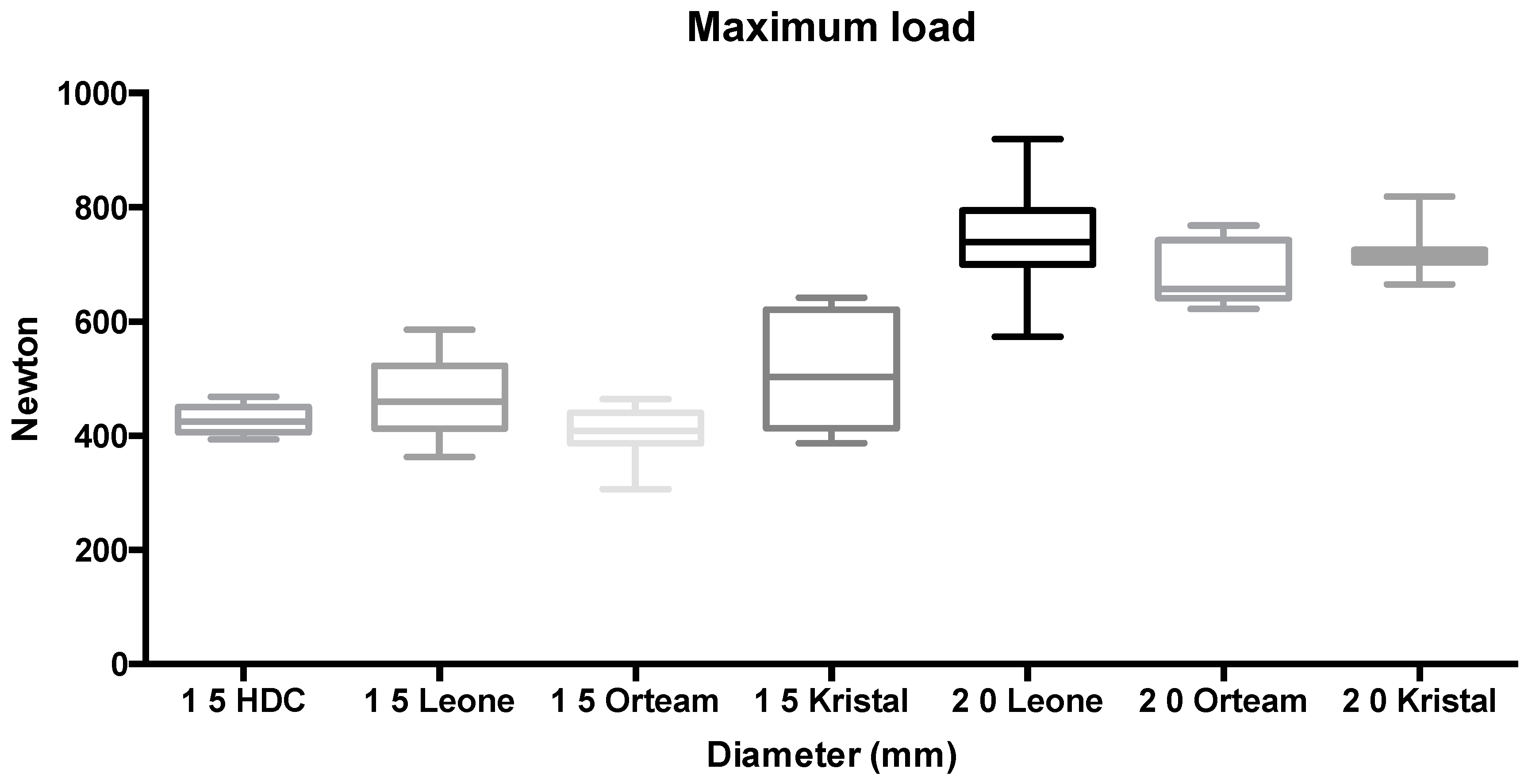
- Miniscrews of 2.0-mm diameter showed significantly higher bending and fracture resistance than 1.5-mm diameter TADs;
- No significant differences were reported between titanium and stainless steel miniscrews with the same diameter;
- Based on these results, when placing a miniscrew for non-conventional TADs’ applications, or when maximum bending and fracture resistance are needed, in order to reduce the risk of unwanted fracture due to tangential forces, a larger diameter is safer regardless of the miniscrew material.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Montasser, M.A.; Keilig, L.; El-Bialy, T.; Reimann, S.; Jäger, A.; Bourauel, C. Effect of archwire cross-section changes on force levels during complex tooth alignment with conventional and self-ligating brackets. Am. J. Orthod. Dentofac. Orthop. 2015, 147 (Suppl. S4), S101–S108. [Google Scholar] [CrossRef] [PubMed]
- Leung, M.T.; Lee, T.C.; Rabie, A.B.; Wong, R.W. Use of miniscrews and miniplates in orthodontics. J. Oral Maxillofac. Surg. 2008, 66, 1461–1466. [Google Scholar] [CrossRef] [PubMed]
- Mesko, M.E.; Skupien, J.A.; Valentini, F.; Pereira-Cenci, T. Can we close large prosthetic space with orthodontics? Int. J. Orthod. Milwaukee 2013, 24, 41–44. [Google Scholar] [PubMed]
- Dahiya, A.; Singh, G. Incisor Intrusion with a Miniscrew-Anchored Segmental Utility Arch. J. Clin. Orthod. 2016, 50, 375–376. [Google Scholar] [PubMed]
- Rodriguez, Y.; Baena, R.; Lupi, M.S.; Ceriana, G.; Sfondrini, M.F.; Scribante, A. Extrusion of severely impacted mandibular first molar using partial orthodontics and temporary anchorage miniscrews. Eur. J. Paediatr. Dent. 2016, 17, 310–314. [Google Scholar]
- Chung, K.; Kim, S.H.; Kook, Y. C-orthodontic microimplant for distalization of mandibular dentition in Class III correction. Angle Orthod. 2005, 75, 119–128. [Google Scholar] [PubMed]
- Wang, S.H.; Shih, Y.H.; Liaw, J.J. Correction of Unilateral Complete Buccal Crossbite with Miniscrew Anchorage. J. Clin. Orthod. 2016, 50, 493–502. [Google Scholar] [PubMed]
- Yamada, K.; Kuroda, S.; Deguchi, T.; Takano-Yamamoto, T.; Yamashiro, T. Distal movement of maxillary molars using miniscrew anchorage in the buccal interradicular region. Angle Orthod. 2009, 79, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Kircelli, B.H.; Pektaş, Z.O.; Uçkan, S. Orthopedic protraction with skeletal anchorage in a patient with maxillary hypoplasia and hypodontia. Angle Orthod. 2006, 76, 156–163. [Google Scholar] [PubMed]
- Pires, M.S.; Reinhardt, L.C.; Antonello G de, M.; Torres do Couto, R. Use of orthodontic mini-implants for maxillomandibular fixation in mandibular fracture. Craniomaxillofac. Trauma Reconstr. 2011, 4, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Moon, W.; Previdente, L.H.; Suzuki, S.S.; Garcez, A.S.; Consolaro, A. Miniscrew-assisted rapid palatal expander (MARPE): The quest for pure orthopedic movement. Dent. Press J. Orthod. 2016, 21, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Nienkemper, M.; Renger, S.; Drescher, D. Mini-implant-supported temporary pontics. J. Clin. Orthod. 2014, 48, 422–429. [Google Scholar] [PubMed]
- Morarend, C.; Qian, F.; Marshall, S.D.; Southard, K.A.; Grosland, N.M.; Morgan, T.A.; McManus, M.; Southard, T.E. Effect of screw diameter on orthodontic skeletal anchorage. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.A.; Cha, J.Y.; Hwang, C.J. Insertion torque of orthodontic miniscrews according to changes in shape, diameter and length. Angle Orthod. 2008, 78, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Tanaka, E. Risks and complications of miniscrew anchorage in clinical orthodontics. Jpn. Dent. Sci. Rev. 2014, 50, 79–85. [Google Scholar] [CrossRef]
- Mizrahi, E. The Use of Miniscrews in Orthodontics: A Review of Selected Clinical Applications. Prim. Dent. J. 2016, 5, 20–27. [Google Scholar] [PubMed]
- Galeotti, A.; Uomo, R.; Spagnuolo, G.; Paduano, S.; Cimino, R.; Valletta, R.; D’Antò, V. Effect of pH on in vitro biocompatibility of orthodontic miniscrew implants. Prog. Orthod. 2013, 14, 15. [Google Scholar] [CrossRef] [PubMed]
- Tuomi, J.T.; Björkstrand, R.V.; Pernu, M.L.; Salmi, M.V.; Huotilainen, E.I.; Wolff, J.E.; Vallittu, P.K.; Mäkitie, A.A. In vitro cytotoxicity and surface topography evaluation of additive manufacturing titanium implant materials. J. Mater. Sci. Mater. Med. 2017, 28, 53. [Google Scholar] [CrossRef] [PubMed]
- Sodor, A.; Ogodescu, A.S.; Petreuş, T.; Şişu, A.M.; Zetu, I.N. Assessment of orthodontic biomaterials’ cytotoxicity: An in vitro study on cell culture. Rom. J. Morphol. Embryol. 2015, 56, 1119–1125. [Google Scholar] [PubMed]
- Downarowicz, P.; Mikulewicz, M. Trace metal ions release from fixed orthodontic appliances and DNA damage in oral mucosa cells by in vivo studies: A literature review. Adv. Clin. Exp. Med. 2017, 26, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Cacciafesta, V.; Maffia, E.; Scribante, A.; Alberti, G.; Biesuz, R.; Klersy, C. Nickel release from new conventional stainless steel, recycled, and nickel-free orthodontic brackets: An in vitro study. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Cacciafesta, V.; Maffia, E.; Massironi, S.; Scribante, A.; Alberti, G.; Biesuz, R.; Klersy, C. Chromium release from new stainless steel, recycled and nickel-free orthodontic brackets. Angle Orthod. 2009, 79, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Seifi, M.; Matini, N.S. Evaluation of primary stability of innovated orthodontic miniscrew system (STS): An ex-vivo study. J. Clin. Exp. Dent. 2016, 8, e255–e259. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, V.K.; Krishnaswamy, N.R.; Thavarajah, R. Miniscrew implant fracture and effects of such retained tip on dentin-pulp complex: A histological report. Dent. Traumatol. 2016, 32, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Reicheneder, C.; Rottner, K.; Bokan, I.; Mai, R.; Lauer, G.; Richter, G.; Gedrange, T.; Proff, P. Mechanical loading of orthodontic miniscrews—Significance and problems: An experimental study. Biomed. Tech. 2008, 53, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.; Hosein, Y.K.; Dunning, C.E.; Tassi, A. Fracture resistance of commonly used self-drilling orthodontic mini-implants. Angle Orthod. 2015, 85, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Bayani, S.; Masoomi, F.; Aghaabbasi, S.; Farsinejad, A. Evaluation of the Effect of Platelet-Released Growth Factor and Immediate Orthodontic Loading on the Removal Torque of Miniscrews. Int. J. Oral Maxillofac. Implant. 2016, 31, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Cacciafesta, V.; Sfondrini, M.F.; Lena, A.; Scribante, A.; Vallittu, P.K.; Lassila, L.V. Force levels of fiber-reinforced composites and orthodontic stainless steel wires: A 3-point bending test. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 410–413. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Massironi, S.; Pieraccini, G.; Scribante, A.; Vallittu, P.K.; Lassila, L.V.; Gandini, P. Flexural strengths of conventional and nanofilled fiber-reinforced composites: A three-point bending test. Dent. Traumatol. 2014, 30, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Cacciafesta, V.; Sfondrini, M.F.; Lena, A.; Scribante, A.; Vallittu, P.K.; Lassila, L.V. Flexural strengths of fiber-reinforced composites polymerized with conventional light-curing and additional postcuring. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 524–527. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Massironi, S.; Pieraccini, G.; Vallittu, P.; Lassila, L.; Sfondrini, M.F.; Gandini, P. Effects of nanofillers on mechanical properties of fiber-reinforced composites polymerized with light-curing and additional postcuring. J. Appl. Biomater. Funct. Mater. 2015, 13, e296–e299. [Google Scholar] [CrossRef] [PubMed]
- Ajami, S.; Mina, A.; Nabavizadeh, S.A. Stress distributions of a bracket type orthodontic miniscrew and the surrounding bone under moment loadings: Three-dimensional finite element analysis. J. Orthod. Sci. 2016, 5, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.B.; Kusnoto, B.; Kim, E.J.; BeGole, E.A.; Hwang, H.S.; Lim, H.J. Prognostic factors associated with the success rates of posterior orthodontic miniscrew implants: A subgroup meta-analysis. Korean J. Orthod. 2016, 46, 111–126. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.L.; Yow, M.; Chew, M.T.; Foong, K.W.C.; Wong, H.C.A. study of success rate of miniscrew implants as temporary anchorage devices in Singapore. Int. J. Dent. 2015, 2015, 294670. [Google Scholar] [CrossRef] [PubMed]
- Melo, A.C.; Andrighetto, A.R.; Hirt, S.D.; Bongiolo, A.L.; Silva, S.U.; Silva, M.A. Risk factors associated with the failure of miniscrews—A ten-year cross sectional study. Braz. Oral Res. 2016, 30, e124. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.; Wu, Y.; Jiang, W.; Zhao, L.; Jing, D.; Zhang, N.; Cao, X.; Xu, Z.; Zhao, Z. Factors Affecting the Clinical Success Rate of Miniscrew Implants for Orthodontic Treatment. Int. J. Oral Maxillofac. Implant. 2016, 31, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Maltha, J.C.; Kuijpers-Jagtman, A.M. Optimum force magnitude for orthodontic tooth movement: A systematic literature review. Angle Orthod. 2003, 73, 86–92. [Google Scholar] [PubMed]
- Wilmes, B.; Panayotidis, A.; Drescher, D. Fracture resistance of orthodontic mini-implants: A biomechanical in vitro study. Eur. J. Orthod. 2011, 33, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.Y.; Chou, S.T.; Tseng, Y.C.; Yang, Y.H.; Wu, C.Y.; Lan, T.H.; Liu, P.H.; Chang, H.P. Influence of different implant materials on the primary stability of orthodontic mini-implants. Kaohsiung J. Med. Sci 2012, 28, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.N.; Sexton, B.E.; Chu, T.M.; Katona, T.R.; Stewart, K.T.; Kyung, H.M.; Liu, S.S. Comparison of stainless steel and titanium alloy orthodontic miniscrew implants: A mechanical and histologic analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Gritsch, K.; Laroche, N.; Bonnet, J.M.; Exbrayat, P.; Morgon, L.; Rabilloud, M.; Grosgogeat, B. In vivo evaluation of immediately loaded stainless steel and titanium orthodontic screws in a growing bone. PLoS ONE 2013, 8, e76223. [Google Scholar] [CrossRef] [PubMed]
- Carano, A.; Lonardo, P.; Velo, S.; Incorvati, C. Mechanical properties of three different commercially available miniscrews for skeletal anchorage. Prog. Orthod. 2005, 6, 82–97. [Google Scholar] [PubMed]
- Chang, J.Z.; Chen, Y.J.; Tung, Y.Y.; Chiang, Y.Y.; Lai, E.H.; Chen, W.P.; Lin, C.P. Effects of thread depth, taper shape, and taper length on the mechanical properties of mini-implants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Radwan, E.S.; Montasser, M.A.; Maher, A. Influence of geometric design characteristics on primary stability of orthodontic miniscrews. J. Orofac. Orthop. 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Xheka, E.; Scribante, A.; Gandini, P.; Sfondrini, G. Reconditioning of self-ligating brackets. Angle Orthod. 2012, 82, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Cacciafesta, V.; Sfondrini, M.F.; Melsen, B.; Scribante, A. A 12 month clinical study of bond failures of recycled versus new stainless steel orthodontic brackets. Eur. J. Orthod. 2004, 26, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Estelita, S.; Janson, G.; Chiqueto, K.; Ferreira, E.S. Effect of recycling protocol on mechanical strength of used mini-implants. Int. J. Dent. 2014, 2014, 424923. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.D.; Choi, S.H.; Cha, J.Y.; Yu, H.S.; Kim, K.M.; Kim, J.; Hwang, C.J. Effects of recycling on the biomechanical characteristics of retrieved orthodontic miniscrews. Korean J. Orthod. 2017, 47, 238–247. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.; Sandler, J. In the land of no evidence, is the salesman king? Am. J. Orthod. Dentofac. Orthop. 2010, 138, 247–249. [Google Scholar] [CrossRef] [PubMed]


| Name | Manufacturer | Diameter | Length | Material | n |
|---|---|---|---|---|---|
| Spider Screw | HDC | 1.5 mm | 10 mm | Titanium Ti-6Al-4V (Grade 5) | 10 |
| Mini Implants | Leone | 1.5 mm | 10 mm | Stainless Steel | 10 |
| Benefit | Orteam | 1.5 mm | 11 mm | Titanium Ti-6Al-4V (Grade 5) | 10 |
| Storm | Kristal | 1.5 mm | 10 mm | Titanium Ti-6Al-4V (Grade 5) | 10 |
| Mini Implants | Leone | 2.0 mm | 10 mm | Stainless Steel | 10 |
| Benefit | Orteam | 2.0 mm | 11 mm | Titanium Ti-6Al-4V (Grade 5) | 10 |
| Storm | Kristal | 2.0 mm | 10 mm | Titanium Ti-6Al-4V (Grade 5) | 10 |
| Group | Diameter | Deflection | Mean | SD | Min | Mdn | Max | Tukey * |
|---|---|---|---|---|---|---|---|---|
| 1 | 1.5 mm | 0.1 mm | 33.28 | 2.92 | 29.28 | 34.16 | 36.86 | A |
| 2 | 1.5 mm | 0.1 mm | 34.69 | 9.50 | 21.13 | 33.38 | 53.70 | A |
| 3 | 1.5 mm | 0.1 mm | 31.53 | 3.86 | 24.34 | 31.81 | 36.21 | A |
| 4 | 1.5 mm | 0.1 mm | 36.38 | 7.01 | 27.67 | 36.00 | 48.65 | A |
| 5 | 2.0 mm | 0.1 mm | 58.00 | 7.17 | 43.45 | 57.99 | 70.73 | B |
| 6 | 2.0 mm | 0.1 mm | 53.07 | 2.92 | 48.84 | 52.71 | 58.16 | B |
| 7 | 2.0 mm | 0.1 mm | 55.21 | 8.58 | 38.58 | 53.63 | 69.32 | B |
| 8 | 1.5 mm | 0.2 mm | 66.57 | 5.85 | 58.56 | 68.32 | 73.73 | B |
| 9 | 1.5 mm | 0.2 mm | 64.71 | 17.71 | 39.48 | 62.29 | 100.42 | B |
| 10 | 1.5 mm | 0.2 mm | 63.05 | 7.72 | 48.68 | 63.62 | 72.42 | B |
| 11 | 1.5 mm | 0.2 mm | 67.87 | 13.06 | 51.66 | 67.19 | 90.44 | B |
| 12 | 2.0 mm | 0.2 mm | 116.00 | 14.34 | 86.91 | 115.98 | 141.46 | C |
| 13 | 2.0 mm | 0.2 mm | 106.15 | 5.84 | 97.68 | 105.41 | 116.31 | C |
| 14 | 2.0 mm | 0.2 mm | 110.43 | 17.16 | 77.16 | 107.26 | 138.64 | C |
| 15 | 1.5 mm | Maximum load | 428.03 | 24.29 | 393.61 | 424.80 | 468.61 | D |
| 16 | 1.5 mm | Maximum load | 481.60 | 133.40 | 300.08 | 462.41 | 773.25 | D |
| 17 | 1.5 mm | Maximum load | 405.89 | 45.53 | 306.68 | 408.58 | 464.25 | D |
| 18 | 1.5 mm | Maximum load | 505.67 | 99.29 | 387.43 | 503.65 | 642.12 | D |
| 19 | 2.0 mm | Maximum load | 747.16 | 90.98 | 573.60 | 739.06 | 919.52 | E |
| 20 | 2.0 mm | Maximum load | 685.03 | 55.53 | 622.47 | 657.79 | 768.21 | E |
| 21 | 2.0 mm | Maximum load | 711.78 | 106.73 | 462.97 | 717.64 | 873.41 | E |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scribante, A.; Montasser, M.A.; Radwan, E.S.; Bernardinelli, L.; Alcozer, R.; Gandini, P.; Sfondrini, M.F. Reliability of Orthodontic Miniscrews: Bending and Maximum Load of Different Ti-6Al-4V Titanium and Stainless Steel Temporary Anchorage Devices (TADs). Materials 2018, 11, 1138. https://doi.org/10.3390/ma11071138
Scribante A, Montasser MA, Radwan ES, Bernardinelli L, Alcozer R, Gandini P, Sfondrini MF. Reliability of Orthodontic Miniscrews: Bending and Maximum Load of Different Ti-6Al-4V Titanium and Stainless Steel Temporary Anchorage Devices (TADs). Materials. 2018; 11(7):1138. https://doi.org/10.3390/ma11071138
Chicago/Turabian StyleScribante, Andrea, Mona A. Montasser, Eman Saad Radwan, Luisa Bernardinelli, Roberto Alcozer, Paola Gandini, and Maria Francesca Sfondrini. 2018. "Reliability of Orthodontic Miniscrews: Bending and Maximum Load of Different Ti-6Al-4V Titanium and Stainless Steel Temporary Anchorage Devices (TADs)" Materials 11, no. 7: 1138. https://doi.org/10.3390/ma11071138
APA StyleScribante, A., Montasser, M. A., Radwan, E. S., Bernardinelli, L., Alcozer, R., Gandini, P., & Sfondrini, M. F. (2018). Reliability of Orthodontic Miniscrews: Bending and Maximum Load of Different Ti-6Al-4V Titanium and Stainless Steel Temporary Anchorage Devices (TADs). Materials, 11(7), 1138. https://doi.org/10.3390/ma11071138