1. Introduction
Recent events associated with the coronavirus disease (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-COV-2), indicate the failure of modern scientists, experts, and artificial intelligence [
1,
2] to properly predict the probability of such a medical surge. No country could predict or was fully prepared for the socio-economic impacts of the outbreak, particularly the economic consequences. Moreover, no measures were initially taken to prevent its spread. The consequences emanating from such unpreparedness has already tangibly impacted all sectors of the economy in regions that have recorded substantial human morbidity and mortality from the disease.
Measures taken by countries to prevent the spread of COVID-19 are unprecedented [
3]. For the first time in many years, the civilised world faced strict restrictions on freedom, such as the closing of international and domestic borders, imposition of a state of emergency, and ban on movement between cities, among others.
These measures are designed to minimise the impact on the health and well-being of society, but their cost is enormous, which remains to be estimated. However, there are certain assumptions and estimates of the losses affecting the global economy, and they are impressive. Even without accurate calculations, it is easy to observe and comprehend the number of people who have lost their jobs, the volume of unproduced goods and of services not provided, the unrealised income, and the sentiments formed among individuals and businesses. Each sector of the global economy has faced losses, and the production, sale, and purchase of non-essential goods (which largely generates the highest incomes and the most value added) have declined.
However, there is no method for predicting events of such magnitudes and their consequences. While there are a number of techniques for future events forecasting and scenario modelling, all of them are based on the dynamics of processes that have already begun. Events whose first-stage processes have not yet started cannot be predicted, as forecasts are built on trends and fixed metrics.
The healthcare sector is at the epicentre of the pandemic. However, other population groups involved in all branches of the economy are also focusing their efforts towards fighting the disease. Therefore, there is also a significant burden on the police, military, teachers, government officials, and other professionals to fulfil the functional responsibilities of individuals in the society.
I believe that economists should also be involved in addressing the problem of ‘black swans’ or ‘gray rhinos’, especially those who specialise in issues such as resource allocation. They should participate in developing economic mechanisms to prevent the negative effects of global disasters.
There are four key categories of resources that contribute to effective responses to surge and are essential for the successful realisation of hospitals’ potential during medical surges [
4]:
- -
Space;
- -
Staff;
- -
Supplies;
- -
Specific resources (to meet the needs of patients, for example, with burns, airborne diseases, paediatrics, etc.).
According to scientists, ‘the medical community has faced and undoubtedly will face choices of how we can best steward the resources available to us’ [
4] (p. 177). Moreover, ‘augmentation of medical surge capacity for disaster response can be achieved through several measures: (1) release of internal capacity through precision launching or through upgrading the levels of response, (2) precision support for medical surge capacity from external efforts, (3) centralised response and (4) altering standards of care’ [
5] (p. 1). Another tactic to increase the capacity of a healthcare facility is to reduce the use of limited resources [
6,
7,
8].
Thus, most studies on preparing for a medical surge have highlighted that resources are limited and always will be. Hence, the staff and management of healthcare institutions need to make managerial and ethical decisions about who wins and who loses. To avoid the need for such decisions, it is necessary to either introduce various lockdowns to reduce the number of patients in the case of human-to-human diseases, or to invent a medical way to reduce the number of patients (e.g., a vaccine), or to increase the capacity of health care facilities, in particular, by economic mechanisms. However, the first two options will not work if, for example, a man-made disaster occurs rather than an outbreak of a contagious disease. Therefore, the most universal way is to use mechanisms to increase health care capacity.
In general, resource constraints are not a problem for economists, since the problem of their replenishment or increase may be in the high level of prices, a replacement for counterparts or an increase in efficiency through the latest technology. However, resources alone are not enough for the well-coordinated functioning of a system. There must be energy, since ‘the flow of energy through a system acts to organise that system’ [
9].
The purpose of this article is to highlight the versatility of the concept of ‘energy’ by attributing it to money or financial resources, which are absolutely essential in dealing with surges as the healthcare system adopts the appropriate capacity level and to utilise the concept of resource allocation as an economic means of refining the medical surge capacity.
2. Background
Preparedness for medical surges is key as events like war and pandemics cannot be predicted. It becomes essential to be prepared, especially economically, to deal with the level, scope and depth of any problem. Thus, this study focuses on the mechanisms that can and should be used to enhance preparedness.
Both unpreparedness as well as preparation for contending with global upheavals (such as diseases and wars) involve enormous societal costs. Therefore, an important economic question is whether it is cheaper to be prepared or not prepared for cataclysms, and this involves a choice between spending money to prevent a crisis or to overcome its effects.
The pandemic consequences for economies will be assessed after overcoming it. However, preparation for the future and minimisation of negative consequences, drawing relevant conclusions and correcting known mistakes should begin today, as the next pandemic can strike at any time.
By issuing an order to stay at home, the governments of many countries made a difficult choice, prioritising the lives and health of people over economic welfare. Several other measures have been taken in various countries to prevent the spread of COVID-19 [
3], such as:
- -
Restriction on movement between settlements;
- -
Restrictions on or cancellation of public transport;
- -
Encouraging workers to work remotely wherever possible;
- -
Prohibition of entry for foreign citizens and stateless persons (with the exception of certain categories).
Not implementing such restrictive measures could subsequently crowd the healthcare system because of a substantial increase in the number of infected cases.
Figure 1 portrays the curve, which has become ubiquitous, to explain the reasons for the introduction of restrictive measures in countries. The section in green depicts the number of patients that the healthcare system can manage if protective (restrictive) measures are enforced. The part under the curve in red denotes the conditional dynamics of patient growth, as some of them will be unable to receive proper treatment because of the limitations of the healthcare system.
One of the most important indicators that characterises the reliability of the healthcare system, especially during a pandemic, is the efficiency of the medical staff. The different stages of dealing with the infection can be observed through the following:
- -
The number of admitted patients and their initial diagnosis;
- -
The number of treated patients (who received care, specific or symptomatic);
- -
The number of recovered patients.
Each stage is determined by the capacity of the medical facility, number of staff, number of technical facilities (space, beds, diagnostic tools, life support techniques, etc.,) and availability of medication. Each of these elements of the healthcare system requires proper financing to ensure availability in sufficient quantities, which will determine the probability of the healthcare system overcoming the disease.
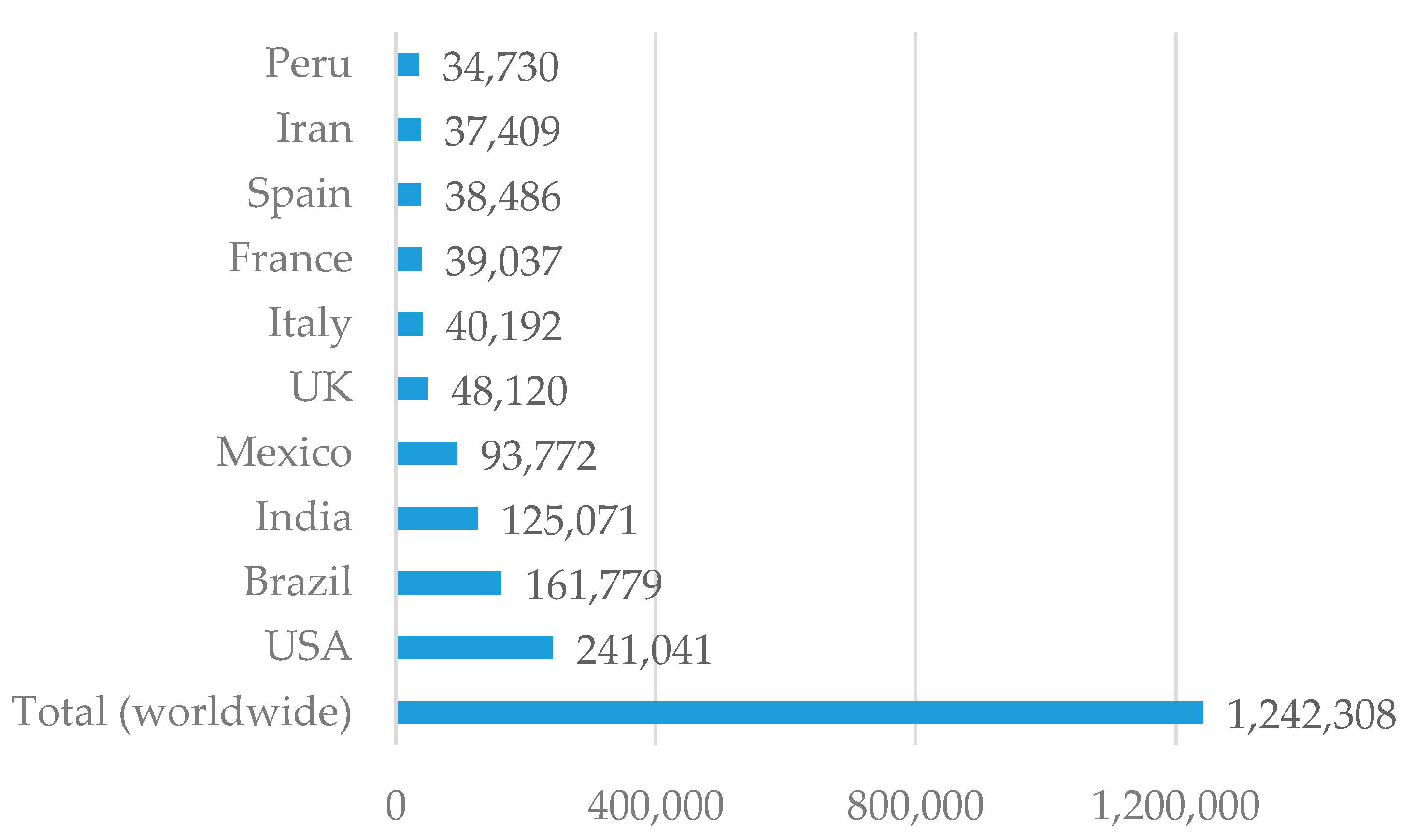
Despite the aforementioned measures taken by various governments, the number of COVID-19 deaths is constantly growing (
Figure 2), as it is impossible to increase the capacity of the healthcare system in a short time. Hospitals and other healthcare institutions have not been able to provide high-quality medical services to all patients, whose numbers are increasing exponentially.
There arises a problem in any system increasingly burdened with processing requests—the establishment of an interdependence between the number of service units and the quality of service. That is, the capacity of the healthcare system should be determined in such a way that medical staff does not remain unoccupied with professional work during periods of normalcy. Meanwhile, in times of a crisis, when the need for treatment with the highest efficiency and quality is high, patients should not be refused admission and treatment due to insufficient capacity.
An important issue is regarding the economic feasibility of maintaining a healthcare system at the highest capacity, such that it could accept the maximum number of patients during periods when there are no epidemics or natural disasters. In England, patient-to-nurse ratios in some hospitals is 5.6 and in others 11.5 [
11], and it would be inexpedient to increase this ratio to 1 patient-per-nurse with the aim that in the period of a probable (unlikely) medical surge, this ratio takes on significance (5.6 or 11.5). In such a case, it would be necessary to preserve the professional expertise of medical employees, as the skills and motivation to work could diminish because of the lack of practice during periods of low workload. For this, measures like additional training and internships should be adopted, which would, however, lead to additional costs.
3. Analysis of Recent Research
A study on the capabilities of the healthcare system [
12] testifies to the improvement in the qualitative characteristics of the system, as well as the permanent insufficiency of its quantitative indicators. Each health shock in history highlighted the lack of prevention measures and the insufficient capacity of the healthcare system. The discussions at a workshop on medical surge capacity (United States, 10–11 July 2009) [
13] led to a number of important conclusions regarding the significant burden on healthcare systems during outbreaks, epidemics, catastrophes or other mass casualties, which can cause a significantly excessive burden on healthcare facilities.
This implies that planning, which is aimed at the implementation of standards in medical treatment, involves more specific requirements, which in turn results in a more engaged and efficient use of funding. In emergency and disaster preparedness, the analysis of quantitative parameters is required; however, much of the recent research is qualitative rather than quantitative. The extent of planning, financing and achieving even the minimally adequate disaster response capabilities in the medical community is extremely unsatisfactory [
7]. Examining the economic component in the preparation and overcoming of the consequences of medical stress primarily needs quantitative parameters.
A 2009 study on hospital surges is one of the key publications that reflects the essence of the medical surge problem, which had been identified by the participants of the aforementioned workshop as a new field of science [
14]. The authors identified three levels of medical surges that affect hospital performance, depending on the degree of stress and workload with new patients, which have also been discussed in other scientific articles [
12,
15]. A brief description of hospital capacity levels is given below:
Conventional capacity: In this level of surge, the premises, staff, and supplies are consistent with the day-to-day practice of the organisation. Such level can be defined as an intense day, when everyone is working as usual, with only a limited amount of extra staff, space, or supplies. It may include retaining staff at the end of the shift, bringing in additional fans from other floors of the hospital, and keeping patients on beds in the rooms or other hospital offices near the emergency department. However, the traditional standard of care and treatment remains high for all patients. The occurrence of this level is possible during a large mass-casualty accident.
Contingency capacity: This level involves the use of medical space that is not typically used for patients in need of emergency, such as hospital conference halls. In this case, the space, staff, and supplies are not consistent with the day-to-day practice, but provide usual standard of care and treatment for all patients. It may involve minor changes that may be caused by the involvement of doctors with different specialties, who may not be accustomed to assisting acutely ill or critically injured patients (dermatologists, ophthalmologists, psychiatrists, etc.,). The most unpredictable limitation is the availability and access to the necessary goods, equipment and medicines.
Crisis capacity: It refers to the conditions under which the adapted hospital space, staff, and supplies do not meet conventional care standards, but provide sufficient care in a medical surge (i.e., provide the best care to patients given the circumstances and available resources). In such circumstances, the hospital is overcrowded, and its facilities are taken outside to tents in the spaces in front of the hospital, in adjacent offices, or other premises.
‘Hospitals usually work with a stockpile of equipment lasting roughly 14 days at normal demand’ [
16]. But what to do during a surge?
For example, in 2015, a group of researchers [
17] investigated the provision of artificial lung ventilation devices that can be used in large-scale respiratory health emergencies, as in the case of COVID-19. Their research showed that the ability of the US healthcare system to provide ventilation therapy may be limited by the various key components at each performance level. The number of emergency care physicians available was a key component at the usual capability level, limiting the maximum number of patients that could be connected to an artificial lung ventilation device. Other deterrents included the number of beds for emergency and intermediate health services as well as the number of available respiratory therapists.
Their findings revealed that even if the number of beds and some staffing capacity could be expanded by using non-specialty beds in general wards and involvement of non-core physicians and nurses without medical emergency experience, ventilation capacity in the US would still be limited by the number of trained respiratory therapists, which would make it impossible to utilise the full potential of the healthcare system [
17].
Research related to medical surges of a different nature—unexpected catastrophes leading to multiple requests for medical care—are devoted to important results in the search for sources of resources and their distribution. Thus, after the events of 11 September 2001, hospitals ‘established relationships with local supermarkets and merchants for short-term help in times of most need’ [
18].
Thus, most studies on preparing for a medical surge have highlighted that resources are limited and always will be. Hence, the staff and management of healthcare institutions need to make managerial and ethical decisions about how and whom to treat first with the available resources or use ‘facility-based surge capacity, public health-based surge capacity, and community-based surge capacity’ [
5] during periods of crisis capacity, making ethical crisis decisions about who wins and who loses: ‘Triage criteria include need (providing resources only to individuals who will not survive without them) and benefit (providing resources to individuals most likely to survive with their use)’ [
19]. Of course, such decisions do not pass without leaving a trace neither for patients, nor for their relatives, nor for medical personnel. The latter, in addition to a huge psychological burden, are also legally responsible for the decisions made on the allocation of resources [
20]. The issue of resource allocation during medical surges is especially acute for people with disabilities [
21].
The most recent publications related to research on the fight against COVID-19 are mainly focused on medical problems: protecting healthcare workers from COVID-19 [
22], providing quality care to older people in the era of COVID-19 [
23], the role of ECMO (a form of cardiopulmonary bypass) in COVID-19 [
24], patients required extracorporeal membrane oxygenation (ECMO) support in the context of the COVID-19 pandemic [
25], paediatric dentistry [
26], an obstetric critical care during pandemic [
27], risk of virus transmission via tears [
28], planning for nonemergent surgery [
29], ethical issues: stay and carry out their professional roles or to step back and decrease their own personal and family risks [
30]; and ‘how to distribute scarce, lifesaving medical resources’ [
31].
Nevertheless, some publications are also devoted to energy (this will be discussed below in this study), however, only in context of electrification [
32,
33,
34,
35].
Although some publications are focused on solving the problem of resource scarcity by external procurement of such resources, the results of such studies relate to management problems, and they also offer solutions from a management point of view, such as recruiting staff through staffing companies [
36,
37].
These and other publications on the issue of medical surges have focused on organisational questions of the functioning of healthcare institutions, replacement or redistribution of missing resources, while the economic component of such loads remains outside the scope of scientists and researchers.
Only a few publications are devoted to the socio-economic issues in the fight against COVID-19, but they are focused on the socio-economic factors of the spread of the disease in certain social groups such as African Americans, Asian Americans, Hispanics, and American Indians or Alaska Natives (compared to White Non-Hispanics) [
38].
4. The Problem Statement
Modern practice and scientific research related to medical surges emphasise the need for the distribution or redistribution of resources such as space, supplies and specific resources.
The problem raised in this study is that there is no universal, unambiguous and absolutely effective way of allocating these resources during medical surges in the world, especially of the magnitude that has been witnessed during the COVID-19 pandemic.
This is why lockdowns were imposed all over the world in the spring of 2020, in addition to actions related to mass quarantines, restricting the work of various institutions, free movement of people, and stopping the work of entire sectors of the economy. Its use is justified by the need to slow down the spread of the virus in order to prevent the collapse of medical institutions and to gain time to prepare the healthcare system for receiving patients. However, such a lockdown did not solve the problem in a complex way: doctors as well as administrative and other personnel in hospitals still have to operate with limited resources, often making ethical decisions such as who should continue to receive assistance with a connected ventilator, and who should be disconnected from it by transferring it to another patient.
Thus, we are faced with the task of proposing a mechanism for solving this problem in the economic plane. Of course, such a solution cannot be complex, since the problem also lies in other planes and is directly related to the sciences, including medicine and chemistry; however, within the framework of the problem formulated in this study and the goal set, we will present ways to solve it.
5. Theoretical Framework
It is necessary to elaborate on the concept of resources, which is multifaceted and inherent in almost every scientific field. It originated in the early seventeenth century but was of little importance until the early twentieth century [
39], when the renowned economics professor Erich Zimmermann published his work on the nature of resources [
40]. As a representative of the institutional theory of economics, he provided a classic definition of resources: ‘The word resource does not refer to a thing or a substance but to a function which a thing or a substance may perform or to an operation in which it may take part, namely, the function or operation of attaining a given end such as satisfying a want. In other words, the word resource is an abstraction reflecting human appraisal and relating to a function or operation’.
Human knowledge, wisdom, and technological innovation can turn neutral objects into precious resources. For example, oil was not considered a resource until 1859; earlier, man was ignorant of its use, but with the development of science and technology, it is now considered the basis for energy use. Therefore, ‘knowledge is the mother of all resources’ [
41,
42]. The process of economic development is directly proportional to the pace of turning a neutral object into a resource. With increasing knowledge, the function of the resource can be enhanced [
40].
In general, resource constraints are not a problem for economists, since the problem of their replenishment or increase may be in the high level of price, a replacement for counterparts or an increase in efficiency through the latest technology. Humanity will not run out of resources until it has ideas [
43].
Resource exhaustion depends on two aspects of technology: first, the likelihood of technical progress, and second, the ease with which other factors of production, especially labour and reproducible capital, can be substituted for exhaustible resources in production [
44].
Land (as a set of natural reserves) and labour (as the physical and mental abilities of the people) were referred to as economic resources that met human needs with goods by the classics of economic theory [
45]. This division seems logical considering the way of life in the past. Over time, capital (all manufactured means of production, i.e., all kinds of tools, machines, equipment, everyday and professional items) and entrepreneurial abilities (a special human resource needed in a market economy to combine all other resources in the process of production of goods and services) have become components of economic resources [
46]. Together, these four elements constitute the economic resources of society, enterprise or organisation.
Hence, the medical resources identified previously can be unreservedly attributed to economic resources, thereby warranting application of appropriate management principles. Thus, space, supplies and specific resources of a healthcare facility denote capital, while staff refers to labour in the context of modern economic theory.
The availability of resources and their concentration in the place of greatest need, however, will not allow us to successfully overcome a medical surge without the energy required to activate these resources and activities, and increase their quantities if necessary.
6. Results
In the framework of our study, the components of medical space, staff and supplies will be considered as economic resources (material and renewable), which are directly related to the fight against COVID-19.
Capital and labour have a clear monetary value. In hospitals or any other healthcare facility, the former shall be represented by the value of assets (buildings, equipment, supplies, etc.,), and the latter, by the amount of staff remuneration.
When it comes to limited resources and transition of hospitals to operating at the corresponding capacity level, one should consider not only the limited amount of resources available at the hospital, but also the opportunity factor by which that level can be increased at the appropriate time. It is clear that the profile and scope of healthcare organisations do not imply the availability of facilities for the production of consumables, which are key in the fight against illnesses and treatment of patients. The increase in consumables, along with the increase in staff and space also requires financial resources, with the help of which it is possible to solve the problem of limited resources that are directly involved in realising the potential of hospitals (
Figure 3).
There must be energy for the well-coordinated work of the healthcare system, since ‘the flow of energy through a system acts to organise that system’ [
9]. Actually, the formulation of the research topic focused on capacity, which provides the best evidence of the need to use energy to increase the power of the system.
The use of energy is understood here as a part of the doing or performing of many varied practices such as cooking, working, communicating or laundry [
47,
48,
49], and in particular, diagnosis, treatment, rehabilitation of patients. At an aggregate level, demand (for medical services, among others) is a product of the vast array of interwoven practices out of which the ordering of society is made [
50,
51].
Of course, today, most researchers in the energy domain (especially in the humanities) refer to electrical or thermal energy [
52], and its sources in fuels such as coal, gas, oil, timber, nuclear generation and ‘new’ renewables sources including technologies like solar photovoltaic energy, geothermal power, and wind power) [
53].
However, some physicists have pointed out that we do not know what energy is [
54]. Hence, it is erroneous to think that ‘energy is contained in fuel’ [
55], but ‘a dollar seems more real than a joule, because though value is subjective, we know what money can buy. A million dollars can feel more meaningful than a megajoule’ [
56].
Each of us, for sure, uses such expressions as ‘I do not have enough energy’, ‘I transfer my energy to someone’, certainly not referring to electrical or thermal energy. Moreover, a study on the history of the concept of energy has, however, shown that the discoverers did not find anything which is transformable and indestructible [
54]. Energy is a system of quantitative and qualitative indicators, the force that sets matter in motion and the source of its action [
57]. The scientist Espen Gaarder Haug says: ‘Get the money, take it out as energy, and sell the energy’ [
58,
59,
60].
Considering that in the modern world, in its civilised part, large purchases are more or less made using non-cash, electronic payments, we can express each monetary unit and transaction in joules (J) or kilowatt hour (kWh), representing the energy expended for its storage, transfer or liquidation. Some researchers do not rule out the scenario that ‘in the future, we could, for example, imagine all money being linked to energy, where the money transferred into your bank account would actually be in the form of energy transferred into a battery bank’ [
58].
In other words, ‘financial resources’ in the direct sense of this word can also be defined in terms of energy. Energy, in other respects, has nothing to do with the subject of our research, but this study aims to reveal the versatility of this concept and the possibility of its application in relation to financial resources.
If under the gold standard, money was gold and gold was money, and under the labour theory of value the monetary unit is equivalent to a unit of labour, then, in the modern world, money is energy. This is evidenced by the energy theory of value [
61], and some researchers have even derived the ‘energy value’ or the dollar exchange rate in Joules—1.4 × 10
5 J [
62].
According to popular wisdom, if a problem can be solved by money, it is not a problem anymore, but rather, a matter of the cost. Therefore, the problem should be solved by increasing funds and acquiring necessary resources in the relevant market. In the modern globalised world, it is not a problem to increase the volume of each of these medical resources for the corresponding, albeit high price, as a result of increased demand. Moreover, it can be done in a fairly short period of time; for example, the recall of retired clinicians or recruiting senior medical students [
31], recruiting and training nurses from other specialities, recruiting and training doctors from other specialties, qualifying nurses from regular ward to IMC and ICU and cooperating with other health-care institutions [
16]. Another urgent solution is to announce open vacancies for doctors and other medical staff from other countries, where their income levels are much lower [
63]. Given the significant number of migrants in the world (272 million in 2019) with a fairly tough immigration policy in developed countries, the opportunities for economic migration remain significant (only 3.4% of the world’s population are migrants) [
64] considering that there are about 50 million is the global health workforce [
65]. If the policy would be focused on promoting the immigration of doctors, medical staff would be appointed in countries that are significantly poor, thus increasing the capacity of the healthcare system. For immigrants, this step will not be devoid of meaning, since the moral and professional task of saving lives and risks will remain unchanged. However, financial compensation will significantly increase and add energy to solve daily tasks.
Moreover, there are examples of a quick solution to this problem when ‘after the Wenchuan earthquake, the Chinese Government mobilised the whole country, activated the emergency medical rescue system within 2 h and ordered 10,630 medical workers to the affected areas’ [
66]. This was despite the fact that ‘the Staff category is a considerable expensive resource’ [
67]. In addition, other solutions include telemedicine [
6,
68] and technology leveraging just-in-time (JIT) training [
12] or classic method of preparing medical students for a pandemic [
69], which, however, takes too long.
The initiation of the purchase of equipment or other materials will generate demand and, accordingly, supply in the market, which will lead to positive economic consequences through stimulation of business activity, in an environment of reasonable policy implementation, as well as physical and organisational access to the markets.
Sometimes managers of companies are invited to work for other firms, while football players, for other teams, at an appropriate, sometimes increased, remuneration. Similarly, medical staff can be found in the labour market and recruited in appropriate hospitals during medical surges.
The procurement of tents or containers for the proper organisation and enhancement of patients’ access to hospitals should not be an obstacle. This is crucial since there are no restrictions on the import of such goods or their manufacturing in the country, which would, besides increasing the medical capacity, provide additional employment and increase business activity.
Thus, the system capacity will increase and the graph will look as shown in
Figure 4, when even the surge shown in yellow is within the capabilities of the healthcare system.
The acquisition of fixed assets or the recruitment of staff at present and over time to increase the medical capacity for times of need is not an obligatory condition. It is worthwhile to consider the economic and legal mechanisms of temporary mobilisation of resources: lease, leasing, fixed-term contracts, etc.
7. Contributions, Limitations
This study has some limitations, in that its conclusions and suggestions are based on a review of the literature without using models, surveys and empirical data, the results section is conceptual.
Nevertheless, the paper presents evidence that the assessment of increasing the capacity of hospitals depends on the financial resources, which can be used to solve the problem of security of healthcare facilities. In addition, the use of the energy concept to denote financial resources in the context of increasing the capacity of medical institutions during medical surges is justified. This research and its conclusions are based on a literature review, logical conclusions. The absence of empirical data does not distort the results of the study, although their collection from various hospitals and geographies would increase its comprehensiveness and objectivity. However, their absence indicates not a lack of understanding of the problem of providing hospitals with financial resources, but rather, to a different way of data collection—through the personal involvement of the author in the described processes. In addition, research and analysis of empirical data would require considerable time and resources to investigate a truly relevant sample from all continents and enterprise groups. This requires a separate study that could not fit into the scope of this work, which can provide a theoretical basis for further research.
8. Discussion
This study emphasises the versatility of the ‘energy’ concept in a broad sense. This approach is a challenge because, on the one hand, recently scientists have focused more on energy and its sources in the utilitarian sense, and less attention has been paid to the philosophical concept and its use in applied sciences. On the other hand, in the pursuit of the resolution of specific economic problems, the connection between the economy and the fundamental sciences, as well as the values that they create, is weakening. Therefore, finance as an applied science is focused exclusively on the resolution of specific problems without regard to general scientific values and categories that are the fundamental sciences’ research subjects. Therefore, the versatility of the concept of ‘energy’ by attributing it to money or financial resources is absolutely essential in dealing with surges as the healthcare system adopts the appropriate capacity level to refining the medical surge capacity.
Preparedness for medical surges is as key as events like war and pandemics, which cannot be predicted. It becomes essential to be prepared, especially economically, to deal with the level, scope and depth of any problem. In addition, modern practice and scientific research related to medical surges emphasise the need for the distribution or redistribution of resources such as space, supplies and specific resources.
The problem raised in this study is that there is no universal, unambiguous and absolutely effective way of allocating these resources during medical surges in the world, especially of the magnitude that has been witnessed during the COVID-19 pandemic. Most studies on preparing for a medical surge have highlighted that resources (space, staff, supplies, and specific resources) are limited and always will be. Hence, the staff and management of healthcare institutions need to make managerial and ethical decisions about how and whom to treat first with the available resources.
This study considers the means at the disposal of healthcare institutions for the control of diseases as economic resources to identify ways to enhance their capacity, especially during periods of medical surges such as those caused by the coronavirus disease (COVID-19). The article, thus, points out that while limited resources are the norm in economic theory, a medical surge provides an opportunity to sufficiently extend the resources within the health system capacity through increased funding. However, resource constraints are not a problem for economists, since the problem of their replenishment or increase may be in the high level of prices, a replacement for counterparts or an increase in efficiency through the latest technology.
9. Conclusions and Future Research Directions
An appropriate level of treatment during periods of increased workload in the healthcare system can be ensured either by changing the organisation of the system and principles for using such resources (such as space, staff, and supplies), by their redistribution or by using financial resources that allow to increase or replenish the amount of such resources.
The article proposes considering the means (space, staff, supplies and specific resources) at the disposal of healthcare institutions as economic resources. The literature on the organisation of hospital activity during periods of medical surges, where it is recommended to use the limited resources available at the expense of their redistribution, is analysed. Such organisation intends to increase the capacity of healthcare institutions only through the redistribution of available resources and approaches regarding their use. This article also proposes taking into account the fact that medical resources are material and renewable, and more attention should be paid to increasing them during medical surges. Future studies in the proposed area should focus on identification of staffing, equipment and supplies needs using mathematical modelling tools (queueing theory), financing systems of healthcare to identify opportunities for improvement, analysis of financing systems of hospitals and other healthcare facilities to increase their capacity, estimation and analysis of the costs for increasing the healthcare system capacity and finding reserves to ensure the effective operation of healthcare facilities.
This study is a review article, therefore, data based on some experiment and input variables are not presented in the work. However, the need still remains for a more detailed study of this topic to test the findings. Therefore, in future research, a model of the energy concept to denote financial resources in the context of increasing the capacity of medical institutions during medical surges should be developed.
An important issue for future research is also the energy of finance cost. To increase the capacity of medical institutions during medical surges, a specific amount of energy is needed, whose cost should be calculated. Moreover, each type of cost can be calculated using its market value like any other energy in the appropriate market, as well as financial resources, which also have their own value in a capital market.