Chin IX: Unusual Soft Tissue Problems of the Lower Face
Abstract
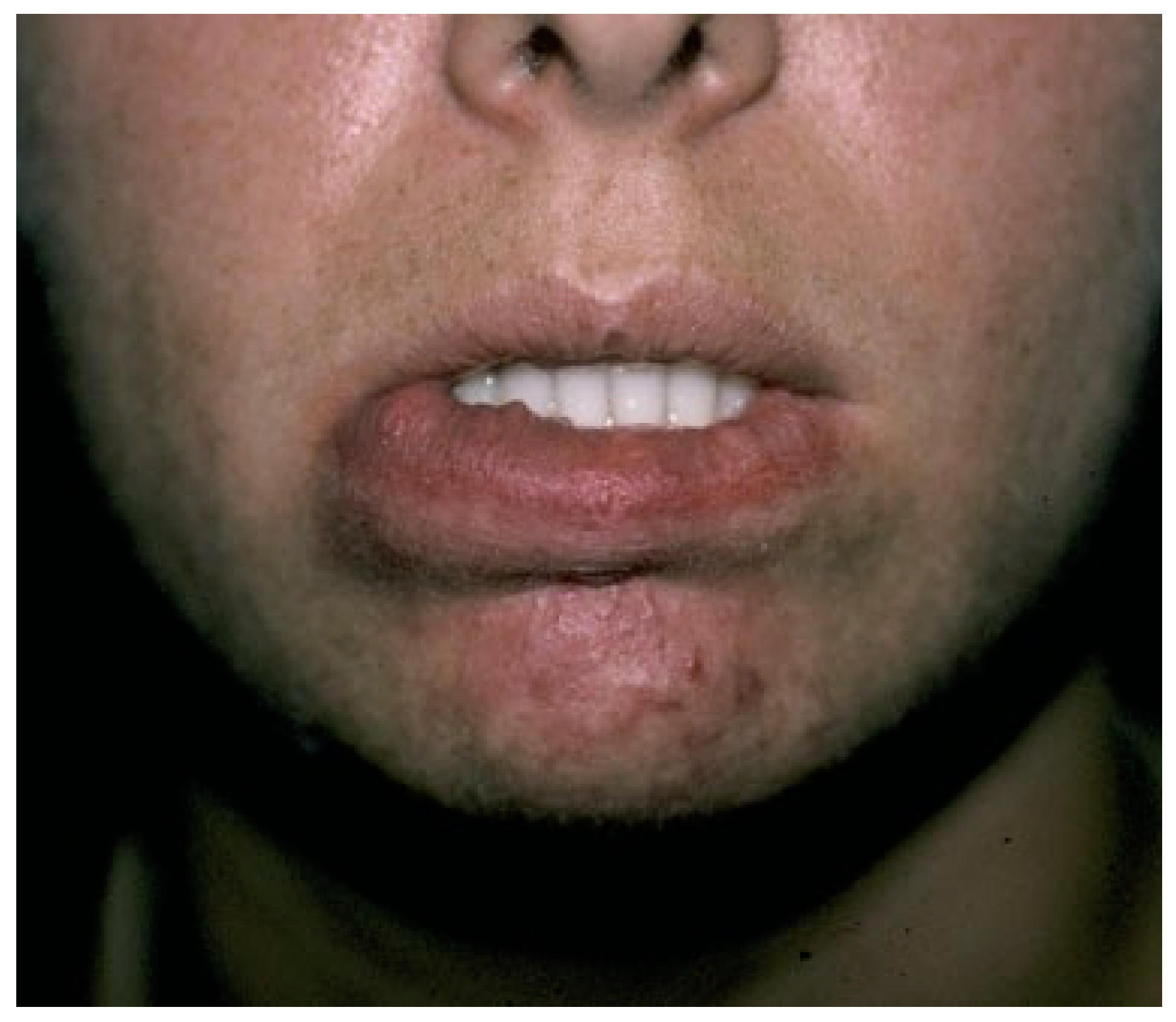
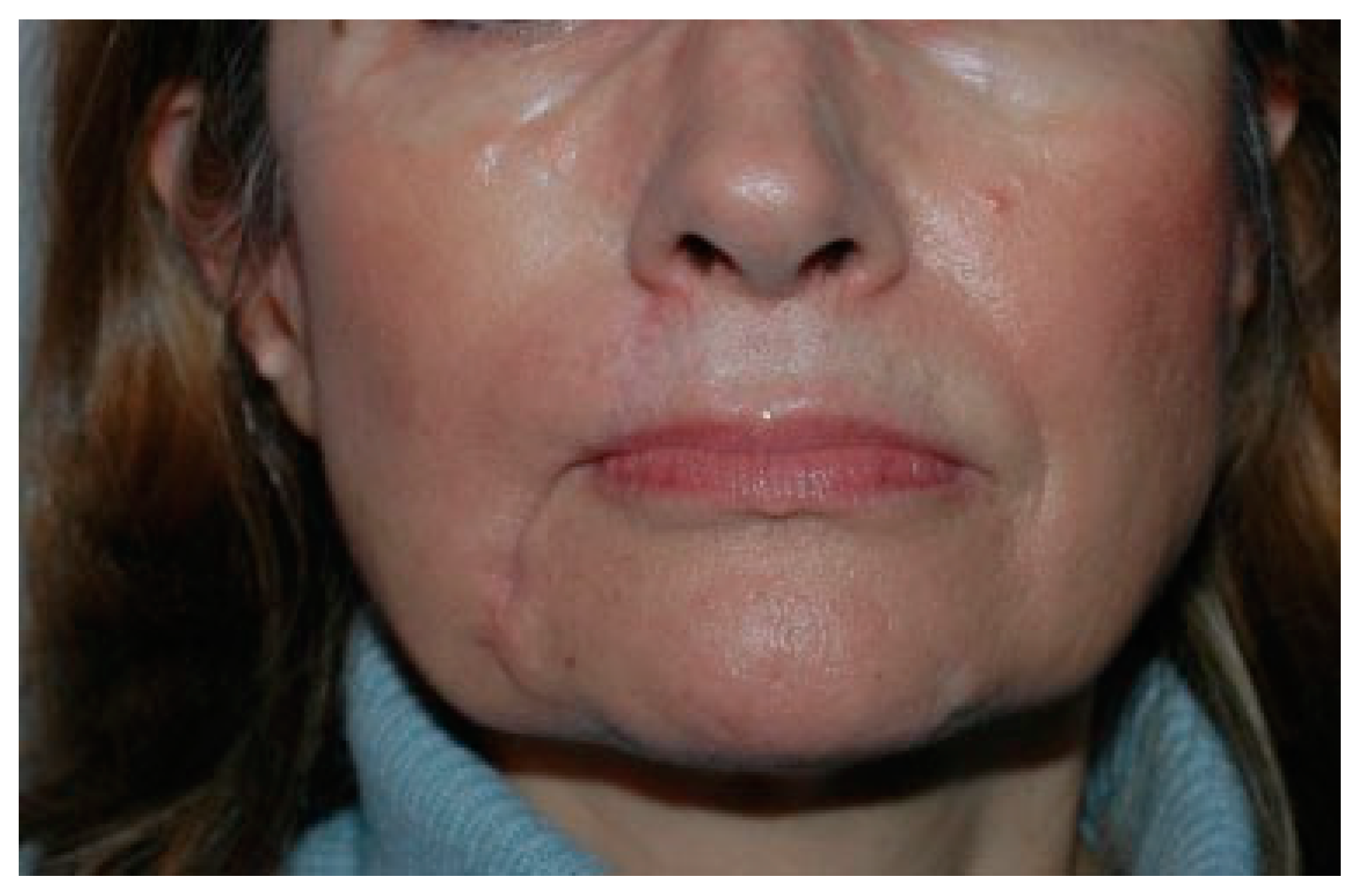
:Case 1: Port-Wine Stain Macrocheilia Overresected—Where do You Get Tissue?
Problems
- Deficiency of the vermillion on the left side of the lower lip.
- Excess horizontal length of the lower lip.
- Incisor show.
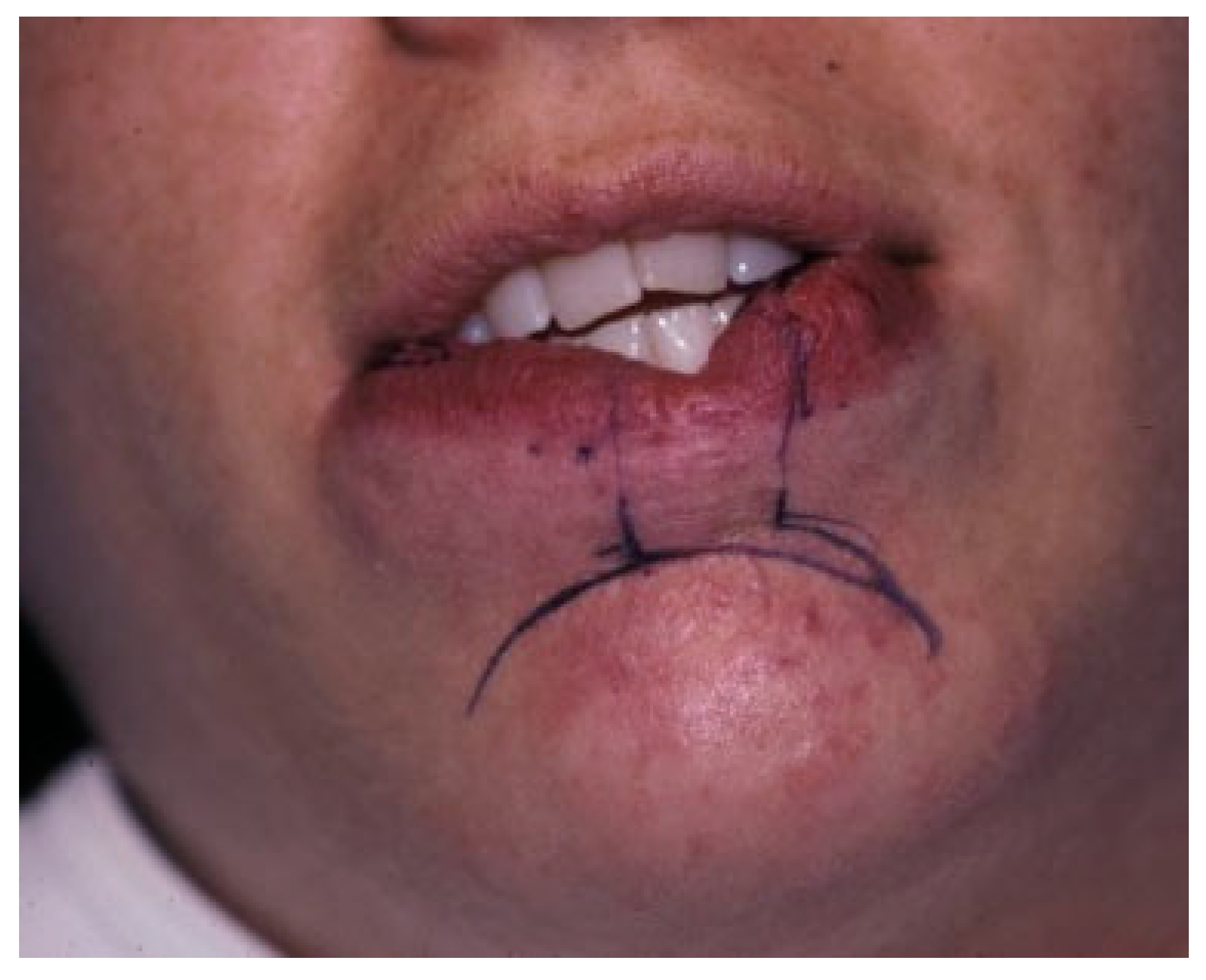
Reconstructive Plan
- 4.
- Restoration of the left lower-lip vermillion deficit with an ipsilateral, interior, Abbe flap transposed 90 degrees to the left.
- 5.
- Resection of excess horizontal lower lip and donor defect from Stage 1.
Stage 1
Stage 2
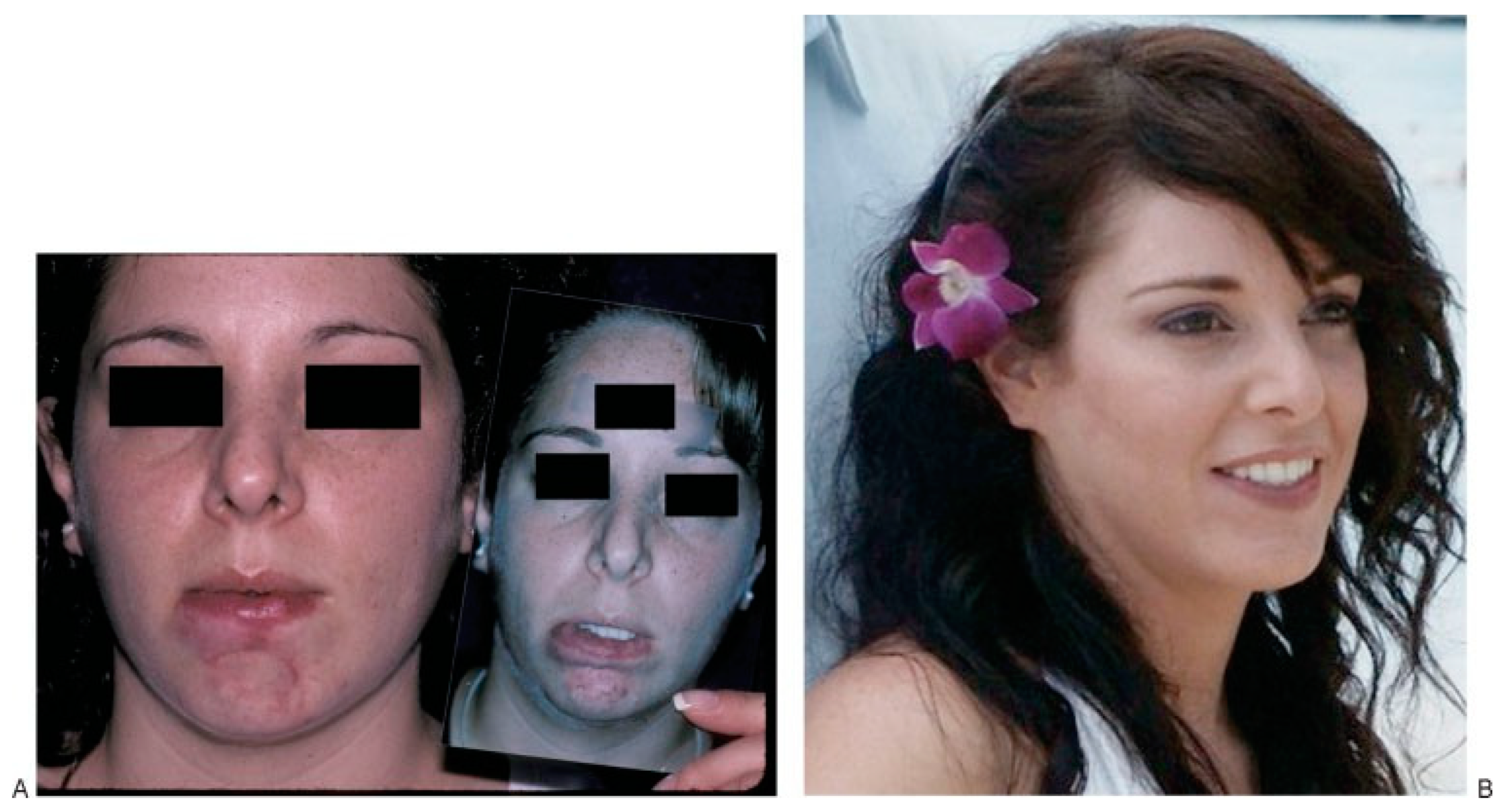
Result
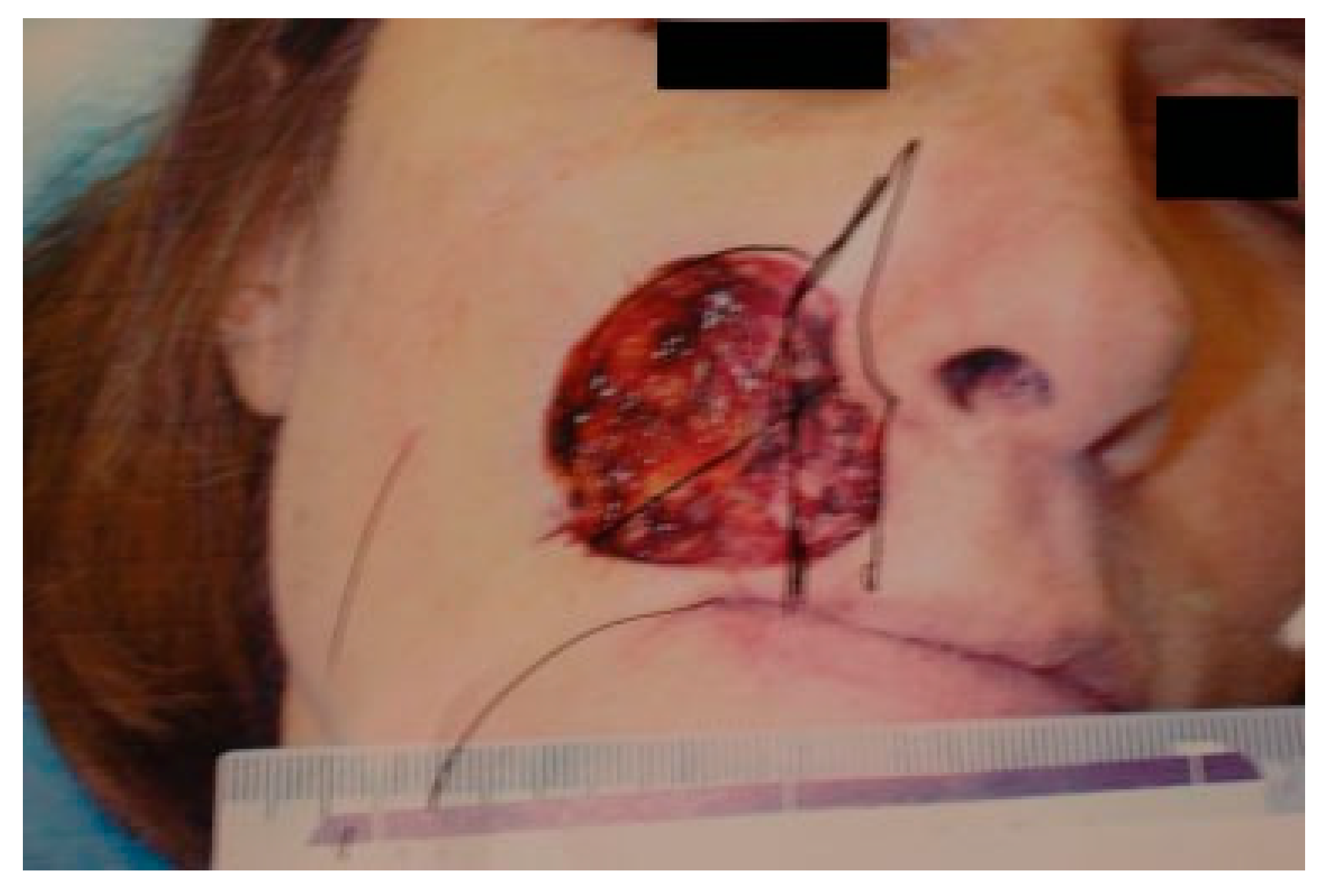
Case 2: Expanding the Reach of the Deep-Plane Schrudde Flap
Problems
- Large upper-lip soft tissue defect extending onto the cheek with mucosal and skin deficiency.
- Upper-lip retraction.
Reconstructive Plan
- Deep-plane angle-rotation flap to restore the upper- lip defect (Figure 7).
Stage 1
Stage 2
Result
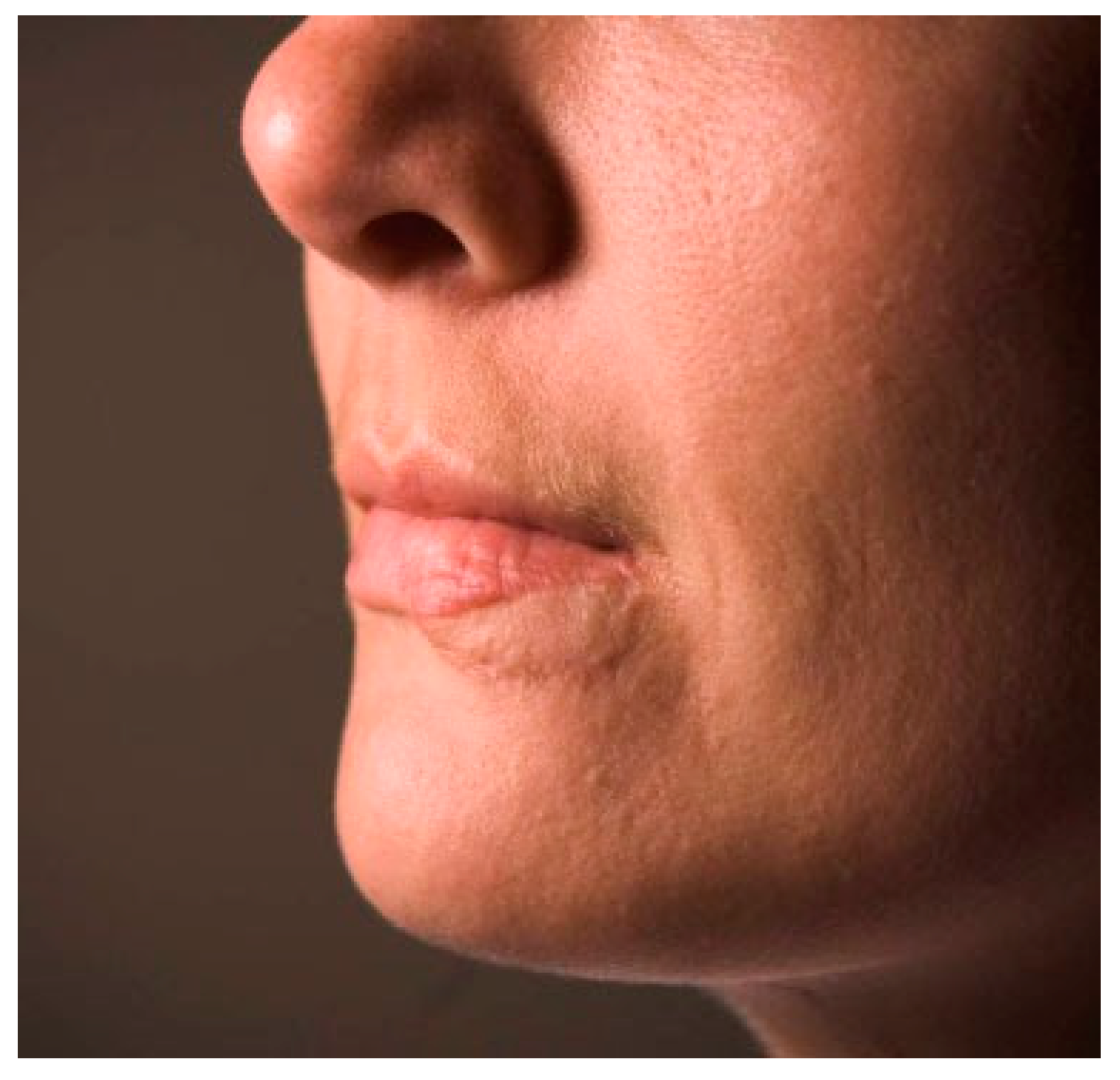
Cases 3 and 4: Precise Reconstruction of the White-Roll
Case 3
Problems
- Obliteration of the white roll.
- Advancement of the vermillion onto the lower-lip skin.
Reconstructive Plan
- Reconstruction of the vermillion/lower-lip skin bor- der exactly with a skin graft.
Stage 1
Stage 2
Result
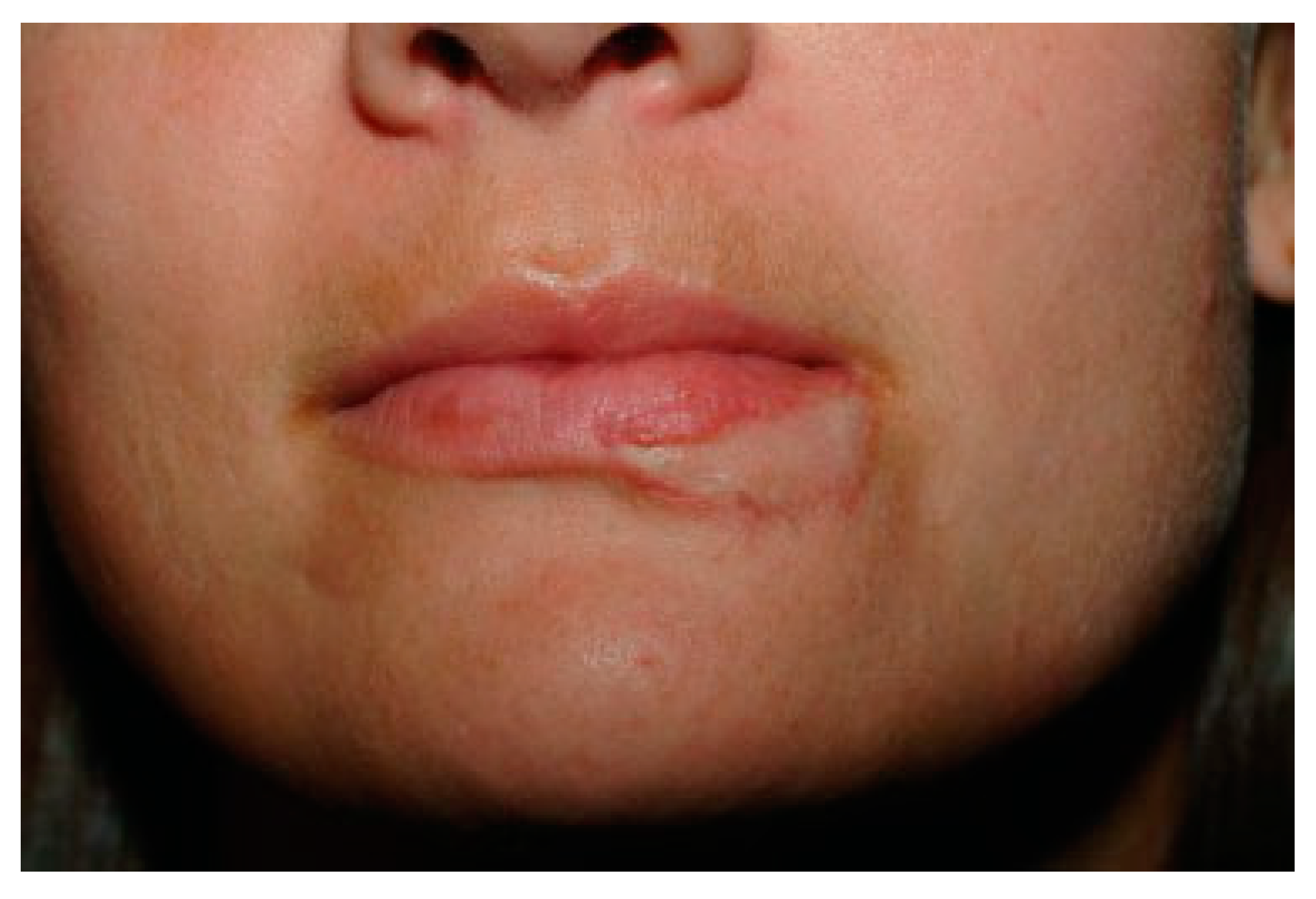
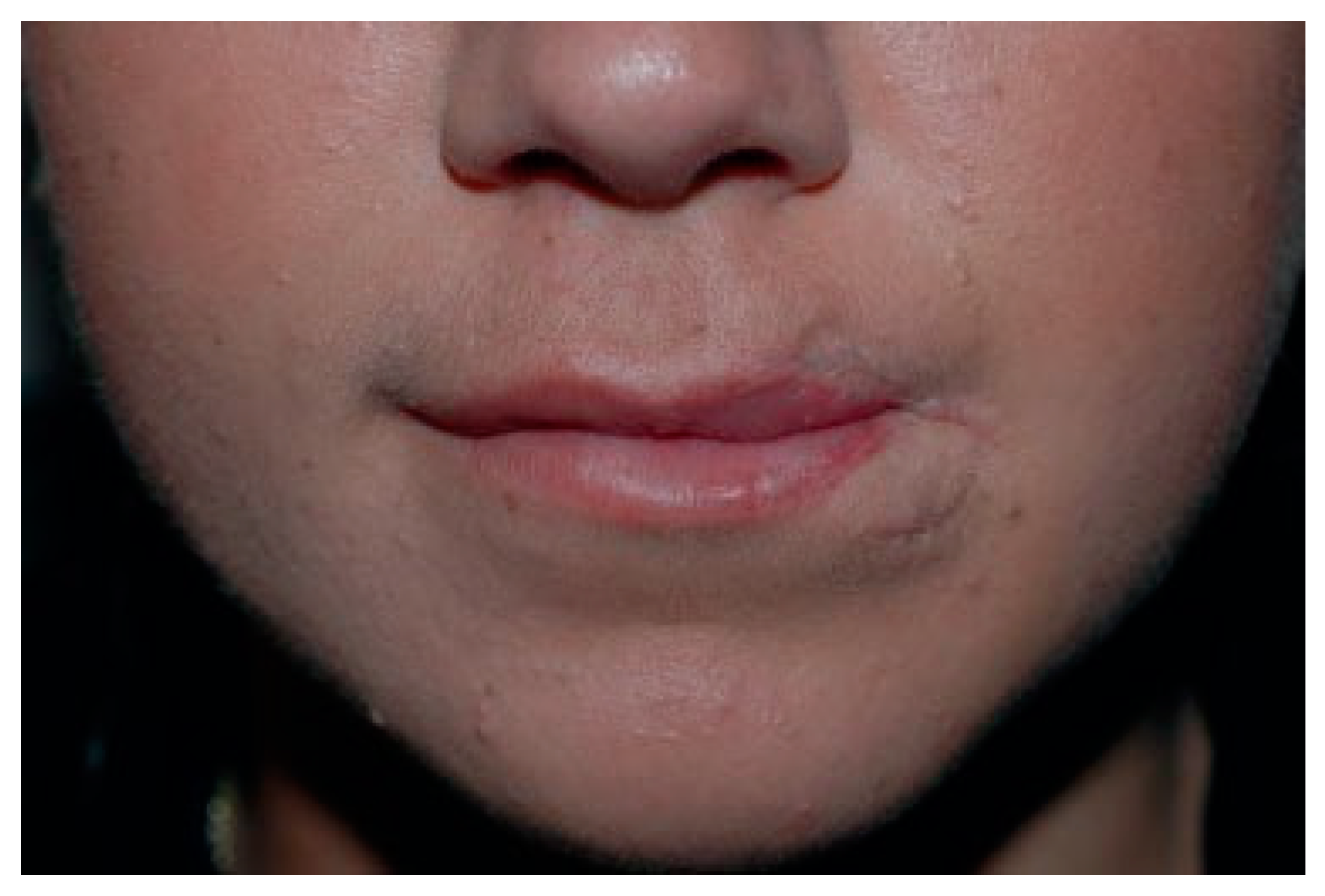
Case 4
Problems (Figure 14)
- Deficiency of upper-lip vermillion lateral to left Cupid’s peak.
- Left lower-lip white roll disrupted.
- Left lower-lip vermillion extending into rounded commissure.
- Contracture of left commissure.
- Tethering of the mucosa posterior to the left com- missure.
Reconstructive Plan
- Composite graft from right lower lip to left upper lip to equilibrate the vermillion.
- Excision of excess left upper-lip skin.
- Two-stage left lower-lip white roll reconstruction with an FTSG graft.
- Excision of scarred mucosa and commissure release followed by local flap reconstruction.
Stage 1 (Figure 15)
Stage 2
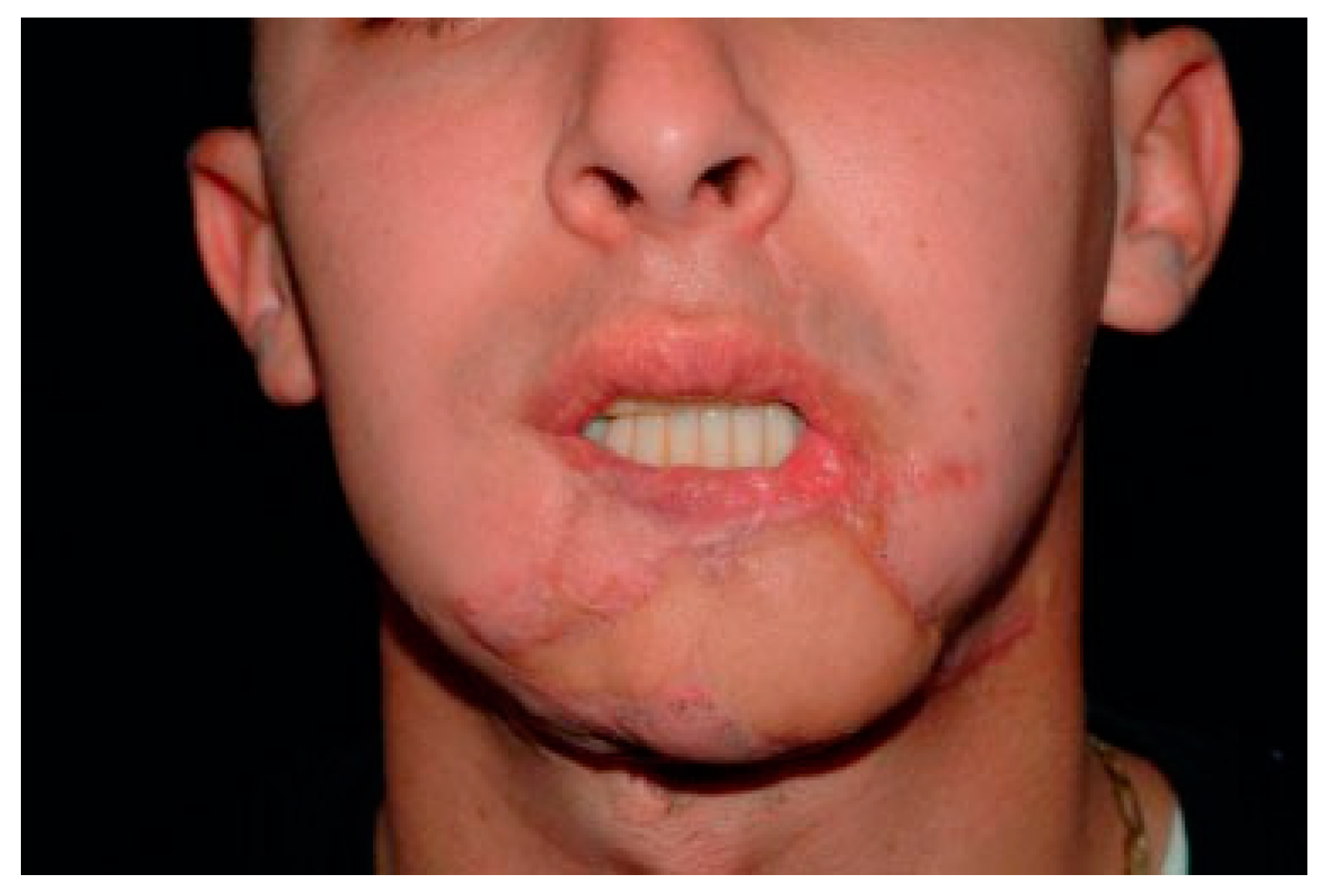
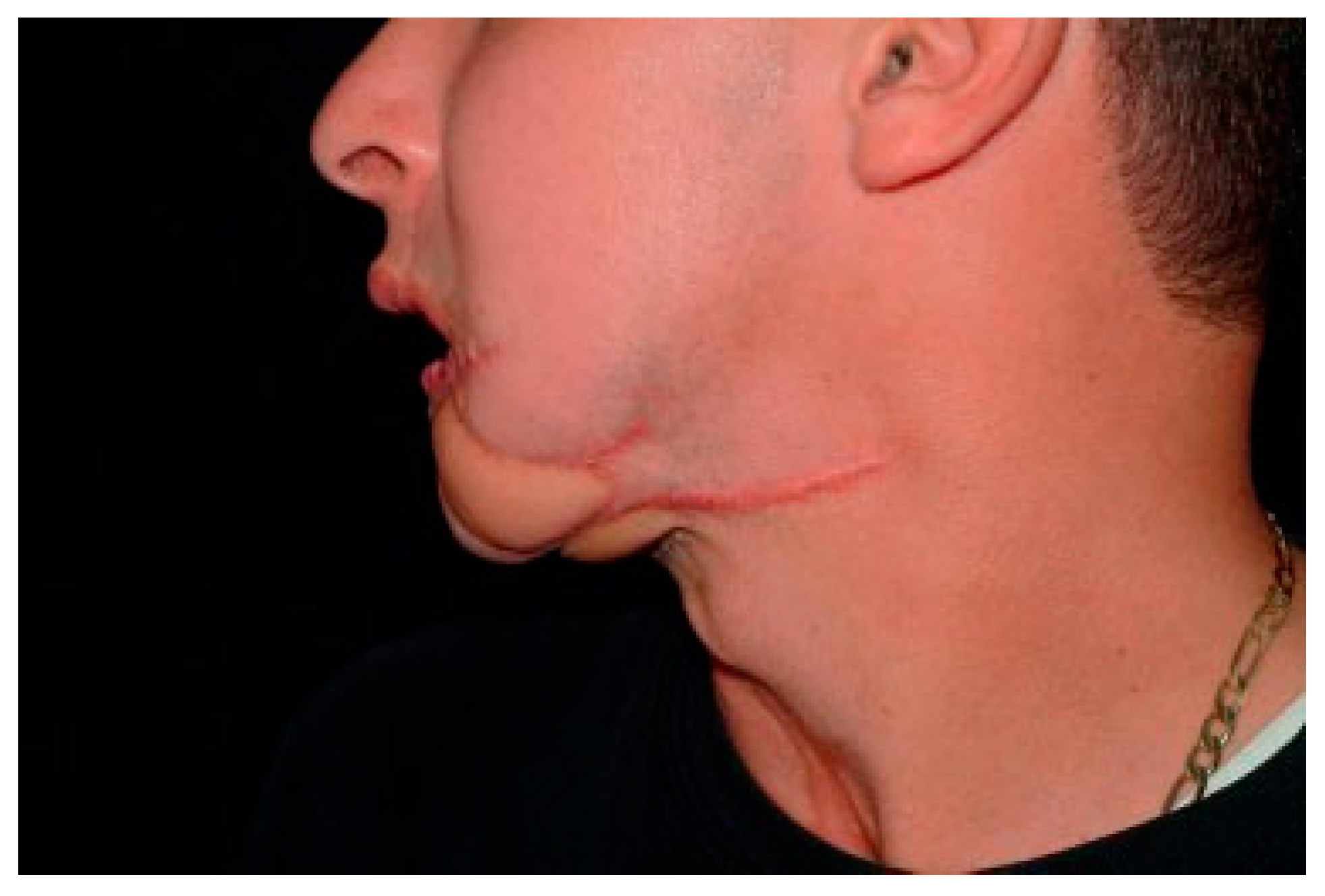
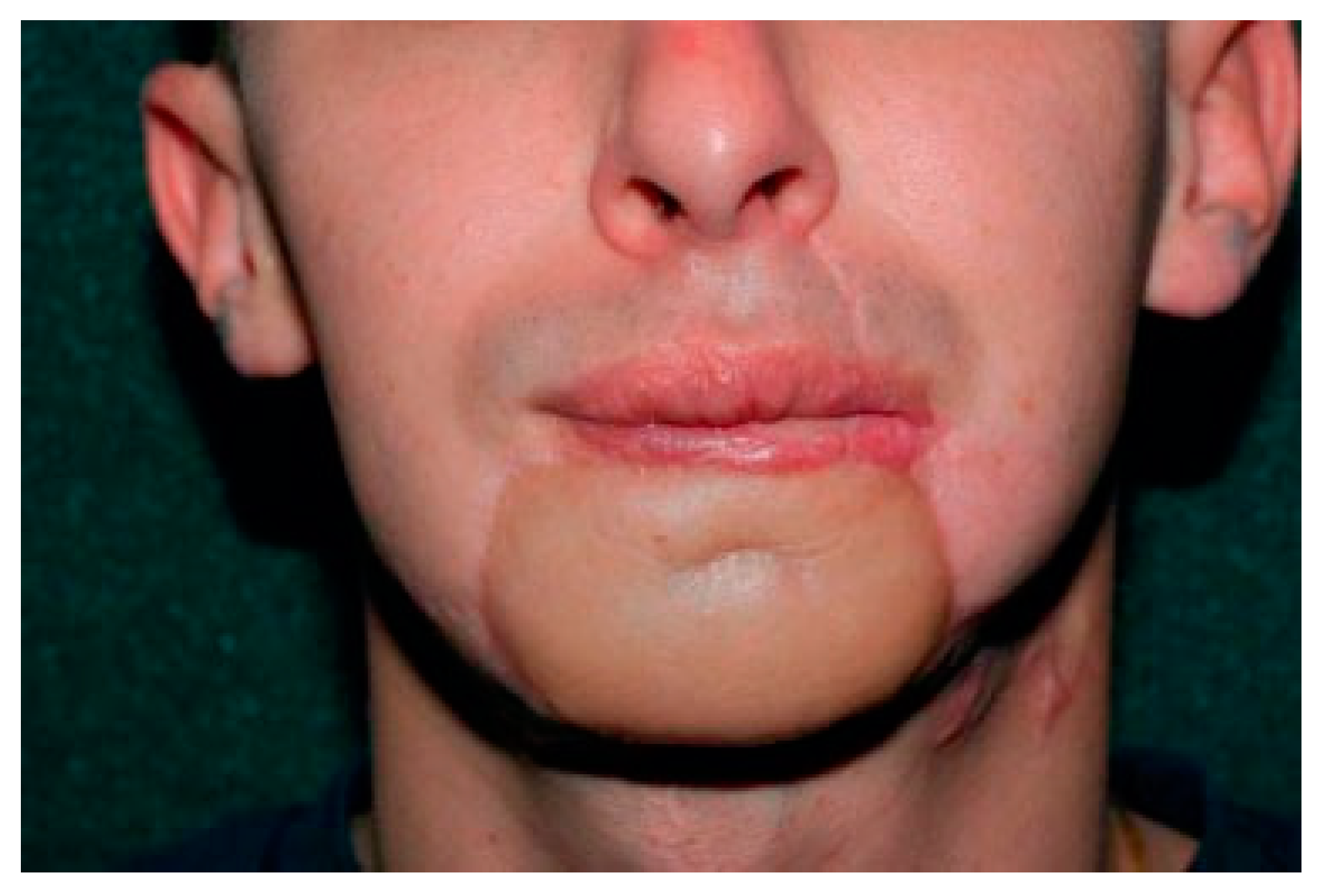
Case 5: Gunshot Loss to Lip and Chin
Problems
- Scarred lower gingivobuccal sulcus resulting in labial incompetence: excessive lower incisor show and per- sistent drooling, requiring him to wear a bib.
- No labiomental sulcus (Figure 20).
- Lack of a chin prominence (Figure 21).
- Subunits of the lower lip and chin disrupted by a patchwork appearance (Figure 19).
- Scarring on the neck and chin from prior flaps.
- Inadequate vermillion.
Reconstructive Plan
- Restoration of the sulcus lining with a thrice delayed extraoral to intraoral turnover flap from the lower-lip skin.
- Formation of a labiomental sulcus.
- Decreased bulking of the chin pad with advanced de- epithelialized submental tissue.
- Resurfacing the lower-lip skin with a second radial forearm flap.
- Restoration of vermillion bulk with a tongue flap.
Stage 1
Stage 2
Stage 3
Stage 4 (Several Procedures)
Stage 5A and B
Result
Summary
References
- Zide, B.M.; Glat, P.M.; Stile, F.L.; Longaker, M.T. Vascular lip enlargement: Part II Port-wine macrocheilia—Tenets of therapy based on normative values. Plast. Reconstr. Surg. 1997, 100, 1674–1681. [Google Scholar] [PubMed]
- Boutros, S.; Zide, B. Cheek and eyelid reconstruction: The resurrection of the angle rotation flap. Plast. Reconstr. Surg. 2005, 116, 1425–1430. [Google Scholar] [PubMed]
- Schrudde, J.; Beinhoff, U. Reconstruction of the face by means of the angle-rotation flap. Aesthetic Plast. Surg. 1987, 11, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Nakanishi, H.; Urano, Y.; Kubo, Y.; Nagae, H. Lower eyelid reconstruction with a cheek flap supported by fascia lata. Plast. Reconstr. Surg. 1999, 103, 1650–1654. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, T.; Yamada, A.; Ueda, K.; Asato, H.; Harii, K. Tissue expansion in facial reconstruction. Plast. Reconstr. Surg. 1994, 94, 944–950. [Google Scholar] [PubMed]
- Burget, G.C.; Menick, F.J. Aesthetic restoration of one-half the upper lip. Plast. Reconstr. Surg. 1986, 78, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Yotsuyanagi, T.; Yokoi, K.; Urushidate, S.; Sawada, Y. Functional and aesthetic reconstruction using a nasolabial orbicularis oris myocutaneous flap for large defects of the upper lip. Plast. Reconstr. Surg. 1998, 101, 1624–1629. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.C.; Celik, N.; Yang, W.G.; Chen, I.H.; Chang, Y.M.; Chen, H.C. Complications after reconstruction by plate and soft- tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap. Plast. Reconstr. Surg. 2003, 112, 37–42. [Google Scholar] [PubMed]















© 2008 by the author. The Author(s) 2008.
Share and Cite
Flores, R.L.; Zide, B.M. Chin IX: Unusual Soft Tissue Problems of the Lower Face. Craniomaxillofac. Trauma Reconstr. 2009, 2, 141-150. https://doi.org/10.1055/s-0029-1224776
Flores RL, Zide BM. Chin IX: Unusual Soft Tissue Problems of the Lower Face. Craniomaxillofacial Trauma & Reconstruction. 2009; 2(3):141-150. https://doi.org/10.1055/s-0029-1224776
Chicago/Turabian StyleFlores, Roberto L., and Barry M. Zide. 2009. "Chin IX: Unusual Soft Tissue Problems of the Lower Face" Craniomaxillofacial Trauma & Reconstruction 2, no. 3: 141-150. https://doi.org/10.1055/s-0029-1224776
APA StyleFlores, R. L., & Zide, B. M. (2009). Chin IX: Unusual Soft Tissue Problems of the Lower Face. Craniomaxillofacial Trauma & Reconstruction, 2(3), 141-150. https://doi.org/10.1055/s-0029-1224776


