Pilot Randomized Controlled Trial of iCanWork: Theory-Guided Return-to-Work Intervention for Individuals Touched by Cancer
Abstract
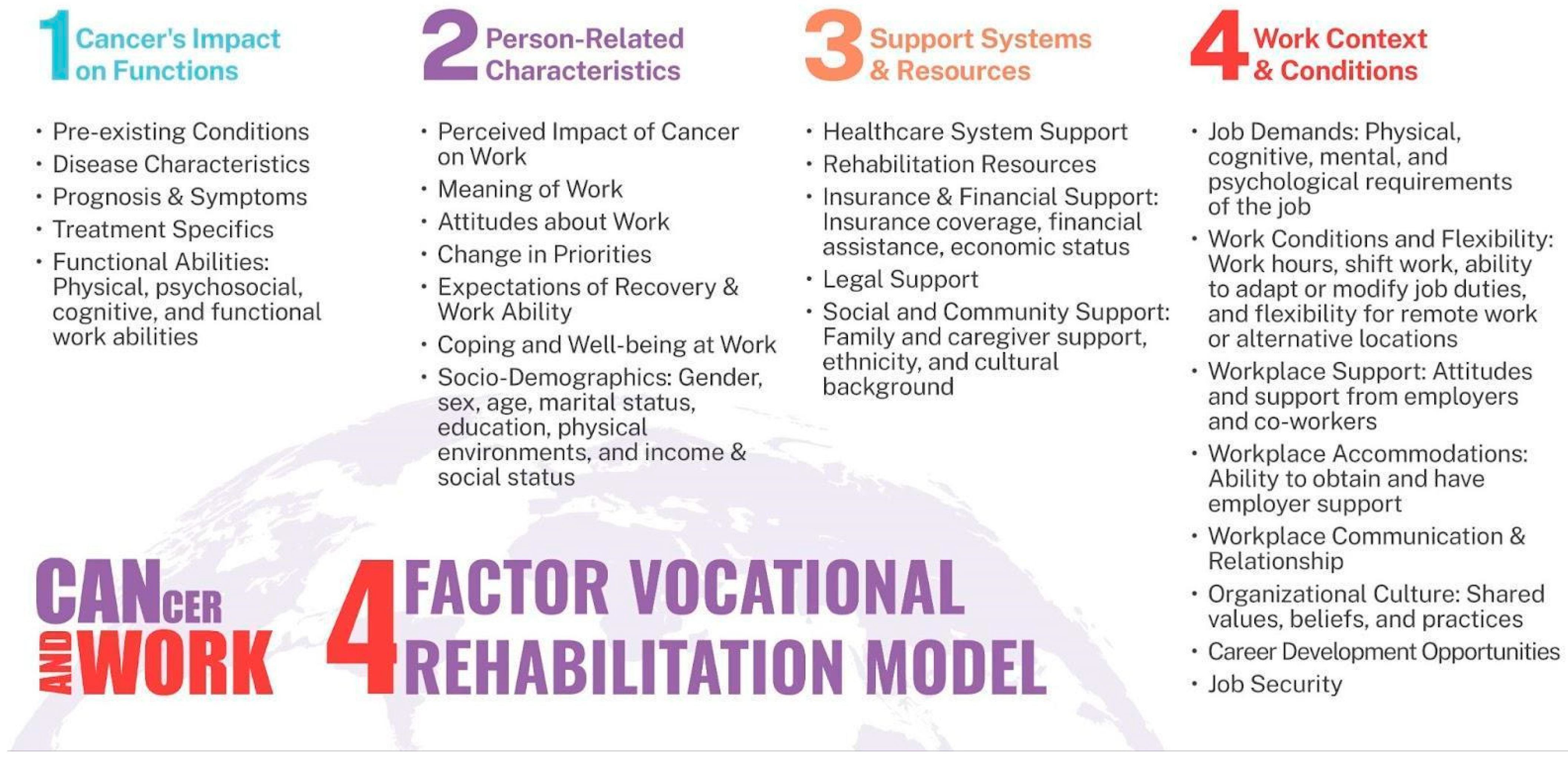
1. Introduction
2. Materials and Methods
2.1. Study and Intervention Design
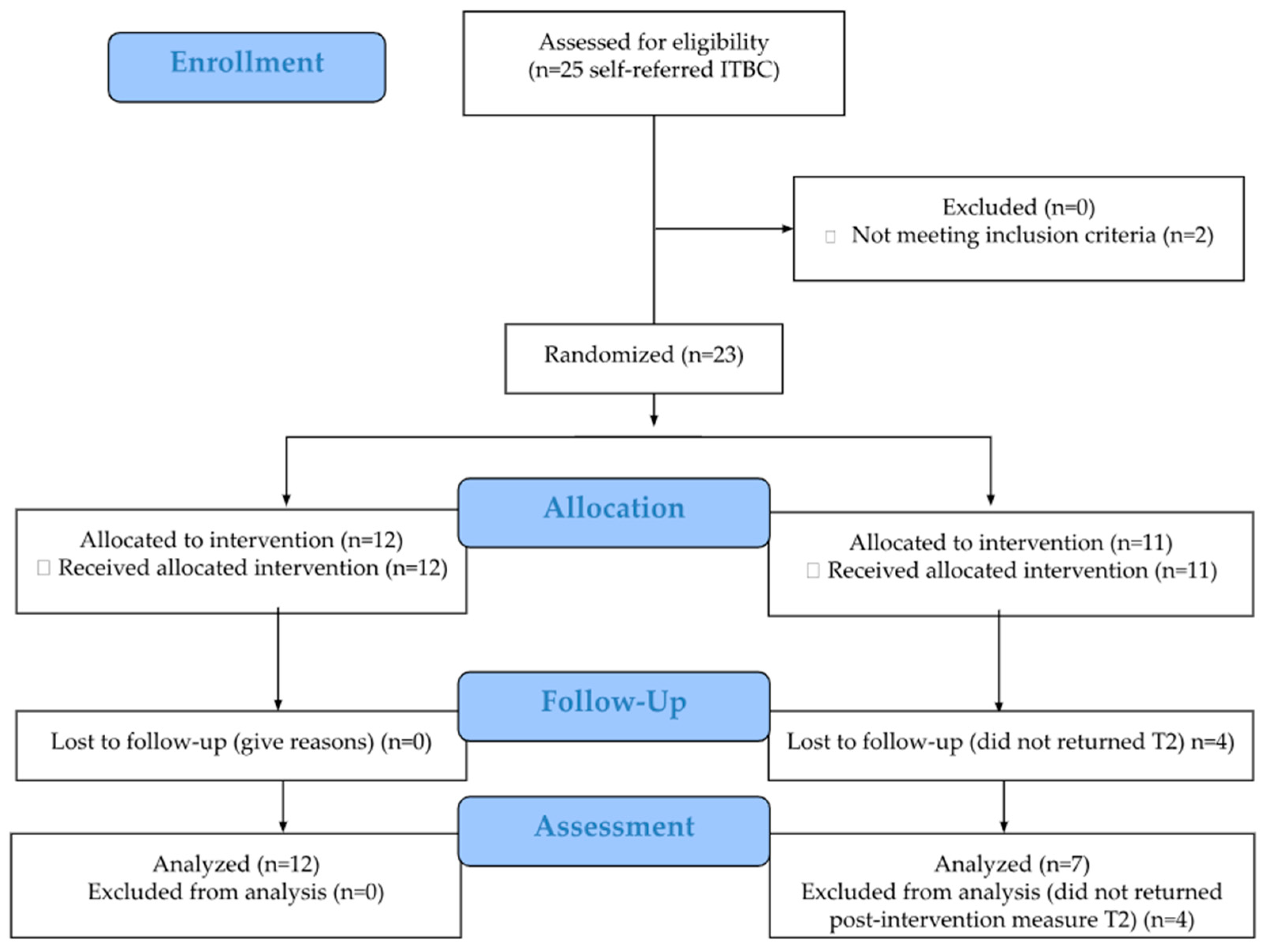
2.2. Setting, Recruitment, Participants, and Sample Size
2.3. Randomization and Blinding
2.4. Study Groups
2.5. Data Collection
2.6. Measurements of Study Outcomes
2.7. Data Analysis
3. Results
3.1. Participant Characteristics
3.2. Feasibility
Participant Engagement and Benchmark Adherence
3.3. Acceptability of the iCanWork Intervention
3.4. Preliminary Work-Health Related Outcomes
Return to Work Status
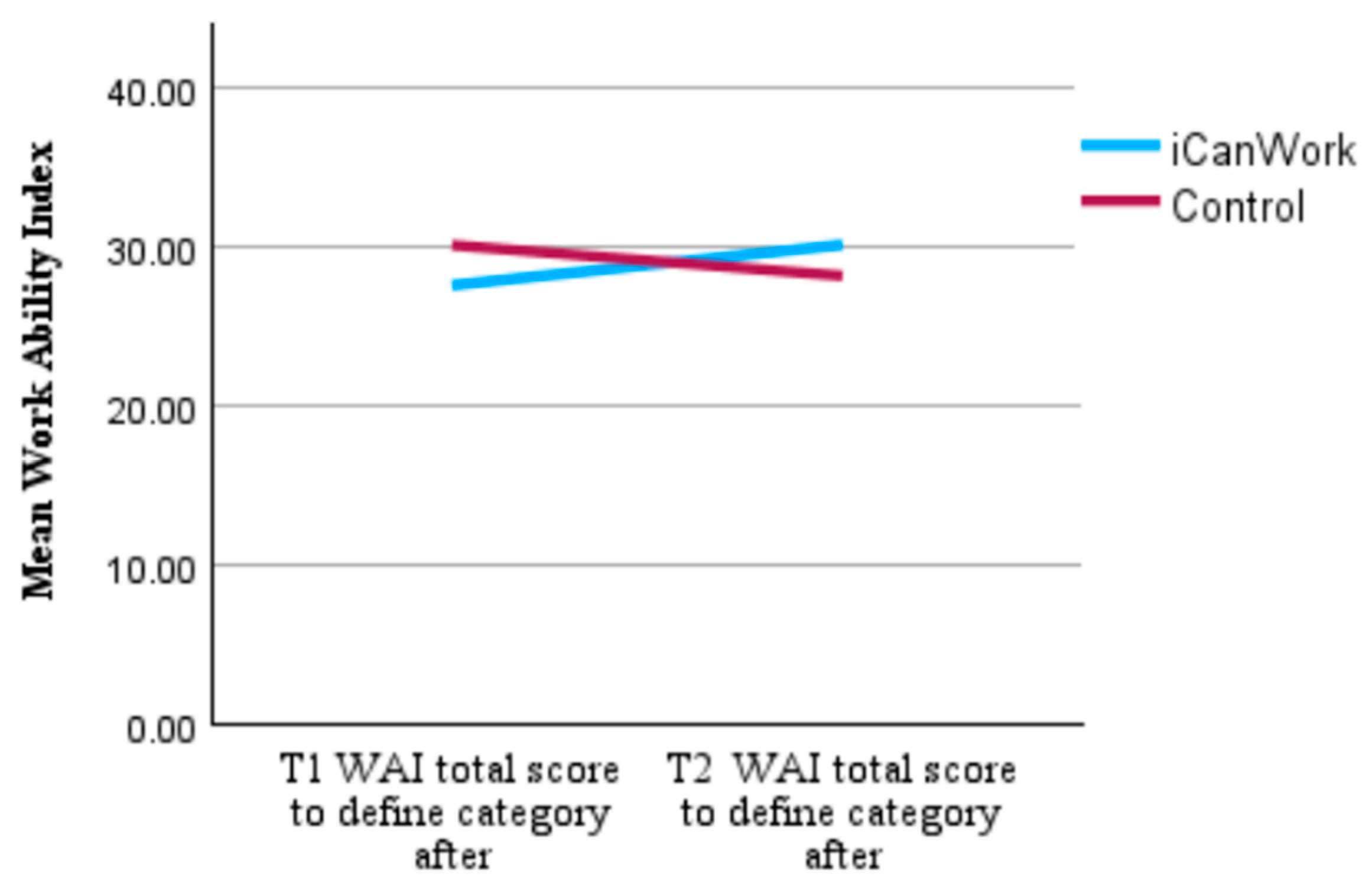
3.5. Work Ability Index (WAI)
3.6. PROPr QoL Domains
3.7. Specific Support Services Utilized Post-Consultation
4. Discussion
4.1. Comparison of iCanWork with Existing RTW Support Interventions
4.2. Areas for Enhancement for iCanWork Based on Specific Components of Other RTW Interventions
4.3. Limitations
4.4. Implications for Future Research and Policy
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| ANOVA | Analysis of Variance |
| CAWSE | Cancer and Work Scale |
| CFIR | Consolidated Framework for Implementation Research |
| CONSORT | Consolidated Standards of Reporting Trials |
| ILWC | Individuals Living with Cancer |
| ITBC | Individuals Touched by Cancer |
| NOC | National Occupational Classification |
| NPT | Normalization Process Theory |
| OT | Occupational Therapy |
| PROM | Patient-Reported Outcome Measure |
| QoL | Quality of Life |
| RCT | Randomized Controlled Trial |
| RTW | Return to Work |
| STTS-R | Satisfaction with Therapy and Therapist Scale-Revised |
| TIDieR | Template for Intervention Description and Replication |
| VR | Vocational Rehabilitation |
| WAI | Work Ability Index |
References
- Maheu, C.; Singh, M.; Tock, W.L.; Robert, J.; Vodermaier, A.; Parkinson, M.; Dolgoy, N. The cancer and work scale (CAWSE): Assessing return to work likelihood and employment sustainability after cancer. Curr. Oncol. 2025, 32, 166. [Google Scholar] [CrossRef]
- Maheu, C.; Parkinson, M.; Wong, C.; Yashmin, F.; Longpré, C. Self-Employed Canadians’ Experiences with Cancer and Work: A Qualitative Study. Curr. Oncol. 2023, 30, 4586–4602. [Google Scholar] [CrossRef] [PubMed]
- Sabariego, M.; Rosas, M.; Piludu, M.A.; Acquas, E.; Giorgi, O.; Corda, M.G. Active avoidance learning differentially activates ERK phosphorylation in the primary auditory and visual cortices of Roman high- and low-avoidance rats. Physiol. Behav. 2019, 201, 31–41. [Google Scholar] [CrossRef]
- Skivington, K.; Lifshen, M.; Mustard, C. Implementing a collaborative return-to-work program: Lessons from a qualitative study in a large Canadian healthcare organization. Work 2016, 55, 613–624. [Google Scholar] [CrossRef] [PubMed]
- Fitch, M.I.; Nicoll, I. Returning to work after cancer: Survivors’, caregivers’, and employers’ perspectives. Psychooncology 2019, 28, 792–798. [Google Scholar] [CrossRef] [PubMed]
- de Boer, A.G.; Torp, S.; Popa, A.; Horsboel, T.; Zadnik, V.; Rottenberg, Y.; Bardi, E.; Bultmann, U.; Sharp, L. Long-term work retention after treatment for cancer: A systematic review and meta-analysis. J. Cancer Surviv. 2020, 14, 135–150. [Google Scholar] [CrossRef]
- de Boer, A.G.E.M.; Frings-Dresen, M.H.W. Employment and the common cancers: Return to work of cancer survivors. Occup. Med. 2009, 59, 378–380. [Google Scholar] [CrossRef]
- Short, P.F.; Vasey, J.J.; Tunceli, K. Employment pathways in a large cohort of adult cancer survivors. Cancer 2005, 103, 1292–1301. [Google Scholar] [CrossRef]
- Sumari, M.; Kassim, N.M.; Razak, N.S.A.A. A conceptualisation of resilience among cancer surviving employed women in malaysia. TQR 2022, 27, 1552. [Google Scholar] [CrossRef]
- Molinero, R.G.; González, P.R.; Zayas, A.; Guil, R. Resilience and workability among breast cancer survivors. J. Dev. Educ. Psychol. Rev. INFAD Psicol. 2019, 4, 37–44. [Google Scholar]
- de Rijk, A.; Amir, Z.; Cohen, M.; Furlan, T.; Godderis, L.; Knezevic, B.; Miglioretti, M.; Munir, F.; Popa, A.E.; Sedlakova, M.; et al. The challenge of return to work in workers with cancer: Employer priorities despite variation in social policies related to work and health. J. Cancer Surviv. 2020, 14, 188–199. [Google Scholar] [CrossRef]
- Greidanus, M.A.; Tamminga, S.J.; de Rijk, A.E.; Frings-Dresen, M.H.W.; de Boer, A.G.E.M. What Employer Actions Are Considered Most Important for the Return to Work of Employees with Cancer? A Delphi Study Among Employees and Employers. J. Occup. Rehabil. 2019, 29, 406–422. [Google Scholar] [CrossRef] [PubMed]
- Awang, H.; Tan, L.Y.; Mansor, N.; Tongkumchum, P.; Eso, M. Factors related to successful return to work following multidisciplinary rehabilitation. J. Rehabil. Med. 2017, 49, 520. [Google Scholar] [CrossRef] [PubMed]
- Iragorri, N.; de Oliveira, C.; Fitzgerald, N.; Essue, B. The indirect cost burden of cancer care in canada: A systematic literature review. Appl. Health Econ. Health Policy 2021, 19, 325–341. [Google Scholar] [CrossRef]
- de Boer, A.G.E.M.; Taskila, T.K.; Tamminga, S.J.; Feuerstein, M.; Frings-Dresen, M.H.W.; Verbeek, J.H. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst. Rev. 2015, 2015, CD007569. [Google Scholar] [CrossRef] [PubMed]
- de Boer, A.G.; Tamminga, S.J.; Boschman, J.S.; Hoving, J.L. Non-medical interventions to enhance return to work for people with cancer. Cochrane Database Syst. Rev. 2024, 3, CD007569. [Google Scholar]
- Lamore, K.; Dubois, T.; Rothe, U.; Leonardi, M.; Girard, I.; Manuwald, U.; Nazarov, S.; Silvaggi, F.; Guastafierro, E.; Scaratti, C.; et al. Return to work interventions for cancer survivors: A systematic review and a methodological critique. Int. J. Environ. Res. Public Health 2019, 16, 1343. [Google Scholar] [CrossRef]
- Cocchiara, R.A.; Sciarra, I.; D’Egidio, V.; Sestili, C.; Mancino, M.; Backhaus, I.; Mannocci, A.; De Luca, A.; Frusone, F.; Di Bella, O.; et al. Returning to work after breast cancer: A systematic review of reviews. Work 2018, 61, 463–476. [Google Scholar] [CrossRef]
- Paltrinieri, S.; Fugazzaro, S.; Bertozzi, L.; Bassi, M.C.; Pellegrini, M.; Vicentini, M.; Mazzini, E.; Costi, S. Return to work in European Cancer survivors: A systematic review. Support. Care Cancer 2018, 26, 2983–2994. [Google Scholar] [CrossRef]
- Canadian Cancer Society. Canadian Cancer Statistics Advisory Committee in collaboration with the Canadian Cancer Society, Statistics Canada and the Public Health Agency of Canada. In Canadian Cancer Statistics: A 2024 Special Report on the Economic Impact of Cancer in Canada; Canadian Cancer Society: Toronto, ON, Canada, 2024. [Google Scholar]
- de Boer, A.G.E.M.; Taskila, T.; Ojajärvi, A.; van Dijk, F.J.H.; Verbeek, J.H.A.M. Cancer survivors and unemployment: A meta-analysis and meta-regression. JAMA 2009, 301, 753–762. [Google Scholar] [CrossRef]
- Parkinson, M.; Maheu, C. Cancer and Work. Can. Oncol. Nurs. J. Rev. Can. Soins Infirm. Oncol. 2019, 29, 258–266. [Google Scholar]
- Maheu, C.; Parkinson, M.; Oldfield, M.; Kita-Stergiou, M.; Bernstein, L.; Esplen, M.J.; Hernandez, C.; Zanchetta, M.; Singh, M.; on behalf of the Cancer and Work Core Team Members. Cancer and Work. 2016. Available online: https://www.cancerandwork.ca/ (accessed on 4 August 2021).
- Parkinson, M.; Maheu, C. Supporting Patients Surviving Cancer with Return to Work. www.fpon.ca. 2022, 4–5, 13. Available online: http://www.bccancer.bc.ca/family-oncology-network-site/Documents/2022%20Spring%20FPONjournal%20WebMay5.pdf (accessed on 29 April 2025).
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A.; PAFS consensus group. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016, 2, 64. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [PubMed]
- Ilmarinen, J. The Work Ability Index (WAI). Occup. Med. 2006, 57, 160. [Google Scholar] [CrossRef]
- Tengland, P.-A. The concept of work ability. J. Occup. Rehabil. 2011, 21, 275–285. [Google Scholar] [CrossRef]
- Gagné, M.; Forest, J.; Vansteenkiste, M.; Crevier-Braud, L.; van den Broeck, A.; Aspeli, A.K.; Bellerose, J.; Benabou, C.; Chemolli, E.; Güntert, S.T.; et al. The Multidimensional Work Motivation Scale: Validation evidence in seven languages and nine countries. Eur. J. Work Organ. Psychol. 2015, 24, 178–196. [Google Scholar] [CrossRef]
- Li, V.W.; Sahota, J.; Dev, D.K.; Gill, D.D.; Evans, V.C.; Axler, A.; Chakrabarty, T.; Do, A.; Keramatian, K.; Nunez, J.-J.; et al. A Randomized Evaluation of MoodFX, a Patient-Centred e-Health Tool to Support Outcome Measurement for Depression: Une évaluation randomisée de MoodFX, un outil de santé en ligne centré sur le patient pour soutenir la mesure du résultat dans la dépression. Can. J. Psychiatry 2024, 69, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Teimour, A.; Narmin, H.R.; Yahya, K.; Farid, Z. Development and evaluation of a new questionnaire for rating of cognitive failures at work. Int. J. Occup. Hyg. 2011, 3, 6–11. [Google Scholar]
- Maheu, C.; Parkinson, M.; Oldfield, M.; Kita-Stergiou, M.; Bernstein, L.; Esplen, M.J.; Hernandez, C.; Zanchetta, M.; Singh, M.; on behalf of the Cancer and Work Core Team Members. Checklist Adapted for the Cancer and Work Website. Cancer and Work Cognitive Symptoms at Work Checklist. Cancer and Work. 2016. Available online: https://www.cancerandwork.ca/tools/cognitive/ (accessed on 4 February 2025).
- Clement, S.; Brohan, E.; Jeffery, D.; Henderson, C.; Hatch, S.L.; Thornicroft, G. Development and psychometric properties the Barriers to Access to Care Evaluation scale (BACE) related to people with mental ill health. BMC Psychiatry 2012, 12, 36. [Google Scholar] [CrossRef]
- Rhoades, L.; Eisenberger, R. Perceived organizational support: A review of the literature. J. Appl. Psychol. 2002, 87, 698–714. [Google Scholar] [CrossRef]
- Demirtaş-Zorbaz, S.; Ulaş Kılıç, Ö.; Akın Arıkan, Ç. Career Adapt-Abilities Scale: Reliability Generalization Meta-Analysis. Psychol. Rep. 2024, 332941241278327. [Google Scholar] [CrossRef]
- Nitkin, P.; Parkinson, M.; Schultz, I.Z. Cancer and Work—A Canadian Perspective; Canadian Association of Psychological Oncology: Toronto, ON, Canada, 2011. [Google Scholar]
- Maheu, C.; Kocum, L.; Parkinson, M.; Robinson, L.; Bernstein, L.J.; Zanchetta, M.S.; Singh, M.; Hernandez, C.; Yashmin, F.; Esplen, M.J. Evaluation of usability and satisfaction of two online tools to guide return to work for cancer survivors on the cancer and work website. J. Occup. Rehabil. 2021, 32, 452–463. [Google Scholar] [CrossRef] [PubMed]
- Parkinson, M.; Maheu, C. Navigating return to work cancer survivor: Supportive strategies and insights. Plans Trusts 2024, 42, 16–22. [Google Scholar]
- Tamminga, S.J.; de Boer, A.G.E.M.; Verbeek, J.H.A.M.; Frings-Dresen, M.H.W. Return-to-work interventions integrated into cancer care: A systematic review. Occup. Environ. Med. 2010, 67, 639–648. [Google Scholar] [CrossRef] [PubMed]
- de Boer, A.G.E.M.; Greidanus, M.A.; Dewa, C.S.; Duijts, S.F.A.; Tamminga, S.J. Introduction to special section on: Current topics in cancer survivorship and work. J. Cancer Surviv. 2020, 14, 101–105. [Google Scholar] [CrossRef]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and analysis of pilot studies: Recommendations for good practice. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef]
- Sim, J.; Lewis, M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J. Clin. Epidemiol. 2012, 65, 301–308. [Google Scholar] [CrossRef]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Teare, M.D.; Dimairo, M.; Shephard, N.; Hayman, A.; Whitehead, A.; Walters, S.J. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: A simulation study. Trials 2014, 15, 264. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.-J.; Tang, J.; Li, J.-M.; Zhu, L.-L.; Xu, J.-S. Exploration of interventions to enhance return-to-work for cancer patients: A scoping review. Clin. Rehabil. 2021, 35, 1674–1693. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. CONSORT-EHEALTH: Implementation of a checklist for authors and editors to improve reporting of web-based and mobile randomized controlled trials. Stud. Health Technol. Inform. 2013, 192, 657–661. [Google Scholar]
- Eysenbach, G.; CONSORT-EHEALTH Group. CONSORT-EHEALTH: Improving and standardizing evaluation reports of Web-based and mobile health interventions. J. Med. Internet Res. 2011, 13, e126. [Google Scholar] [CrossRef]
- Sheill, G.; Guinan, E.; Brady, L.; Hevey, D.; Hussey, J. Exercise interventions for patients with advanced cancer: A systematic review of recruitment, attrition, and exercise adherence rates. Palliat. Support. Care 2019, 17, 686–696. [Google Scholar] [CrossRef]
- Oei, T.P.; Shuttlewood, G.J. Development of a satisfaction with therapy and therapist Scale. Aust. N. Z. J. Psychiatry 1999, 33, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Oei, T.P.; Green, A.L. The satisfaction with therapy and therapist scale-Revised (STTS-R) for group psychotherapy: Psychometric properties and confirmatory factor analysis. Prof. Psychol. Res. Pract. 2008, 39, 435–442. [Google Scholar] [CrossRef]
- Sidani, S.; Epstein, D.R.; Fox, M. Psychometric evaluation of a multi-dimensional measure of satisfaction with behavioral interventions. Res. Nurs. Health 2017, 40, 459–469. [Google Scholar] [CrossRef]
- Eze, A.; Anyebe, M.O.; Nnamani, R.G.; Nwaogaidu, J.C.; Mmegwa, P.U.; Akubo, E.A.; Bako, V.N.; Ishaya, S.N.; Eze, M.I.; Ekwueme, F.O.; et al. Online cognitive-behavioral intervention for stress among English as a second language teachers: Implications for school health policy. Front. Psychiatry 2023, 14, 1140300. [Google Scholar] [CrossRef]
- de Boer, A.G.E.M.; Verbeek, J.H.A.M.; Spelten, E.R.; Uitterhoeve, A.L.J.; Ansink, A.C.; de Reijke, T.M.; Kammeijer, M.; Sprangers, M.A.G.; van Dijk, F.J.H. Work ability and return-to-work in cancer patients. Br. J. Cancer 2008, 98, 1342–1347. [Google Scholar] [CrossRef]
- Stapelfeldt, C.M.; Momsen, A.-M.H.; Jensen, A.B.; Andersen, N.T.; Nielsen, C.V. Municipal return to work management in cancer survivors: A controlled intervention study. Acta Oncol. 2021, 60, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Tamminga, S.J.; Verbeek, J.H.A.M.; Bos, M.M.E.M.; Fons, G.; Kitzen, J.J.E.M.; Plaisier, P.W.; Frings-Dresen, M.H.W.; de Boer, A.G.E.M. Two-Year Follow-Up of a Multi-centre Randomized Controlled Trial to Study Effectiveness of a Hospital-Based Work Support Intervention for Cancer Patients. J. Occup. Rehabil. 2019, 29, 701–710. [Google Scholar] [CrossRef]
- Magnavita, N.; Meraglia, I.; Viti, G.; Borghese, L. The Work Ability Index (WAI) in the Healthcare Sector: A Cross-Sectional/Retrospective Assessment of the Questionnaire. Int. J. Environ. Res. Public Health 2024, 21, 349. [Google Scholar] [CrossRef]
- Radkiewicz, P.; Widerszal-Bazyl, M. Psychometric properties of Work Ability Index in the light of comparative survey study. Int. Congr. Ser. 2005, 1280, 304–309. [Google Scholar] [CrossRef]
- Ilmarinen, J.; Tuomi, K. Past, Present and Future of Work Ability. People Work Res. Rep. 2004, 65, 1–25. [Google Scholar]
- Hays, R.D.; Spritzer, K.L.; Schalet, B.D.; Cella, D. PROMIS®-29 v2.0 profile physical and mental health summary scores. Qual. Life Res. 2018, 27, 1885–1891. [Google Scholar] [CrossRef]
- Kang, D.; Kim, Y.; Lim, J.; Yoon, J.; Kim, S.; Kang, E.; Nam, H.; Shim, S.; Lee, M.; Bok, H.; et al. Validation of the Korean Version of the Patient-Reported Outcomes Measurement Information System 29 Profile V2.1 among Cancer Survivors. Cancer Res. Treat. 2022, 54, 10–19. [Google Scholar] [CrossRef]
- Nekhlyudov, L.; Campbell, G.B.; Schmitz, K.H.; Brooks, G.A.; Kumar, A.J.; Ganz, P.A.; Von Ah, D. Cancer-related impairments and functional limitations among long-term cancer survivors: Gaps and opportunities for clinical practice. Cancer 2022, 128, 222–229. [Google Scholar] [CrossRef]
- Munir, F.; Yarker, J.; McDermott, H. Employment and the common cancers: Correlates of work ability during or following cancer treatment. Occup. Med. 2009, 59, 381–389. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Hartmann, C.; Fischer, F.; Klapproth, C.P.; Röhle, R.; Rose, M.; Karsten, M.M. PROMIS-29 and EORTC QLQ-C30: An empirical investigation towards a common conception of health. Qual. Life Res. 2023, 32, 749–758. [Google Scholar] [CrossRef] [PubMed]
- Tamminga, S.J.; Verbeek, J.H.A.M.; Bos, M.M.E.M.; Fons, G.; Kitzen, J.J.E.M.; Plaisier, P.W.; Frings-Dresen, M.H.W.; de Boer, A.G.E.M. Effectiveness of a hospital-based work support intervention for female cancer patients—A multi-centre randomised controlled trial. PLoS ONE 2013, 8, e63271. [Google Scholar] [CrossRef]
- de Boer, A.G.E.M.; de Wind, A.; Coenen, P.; van Ommen, F.; Greidanus, M.A.; Zegers, A.D.; Duijts, S.F.A.; Tamminga, S.J. Cancer survivors and adverse work outcomes: Associated factors and supportive interventions. Br. Med. Bull. 2023, 145, 60–71. [Google Scholar] [CrossRef]
- Government of Canada, N.O.C. National Occupational Classification—Canada.ca. 2021. Available online: https://noc.esdc.gc.ca/ (accessed on 1 July 2022).
- Leensen, M.C.J.; Groeneveld, I.F.; van der Heide, I.; Rejda, T.; van Veldhoven, P.L.J.; van Berkel, S.; Snoek, A.; van Harten, W.; Frings-Dresen, M.H.W.; de Boer, A.G.E.M. Return to work of cancer patients after a multidisciplinary intervention including occupational counselling and physical exercise in cancer patients: A prospective study in the Netherlands. BMJ Open 2017, 7, e014746. [Google Scholar] [CrossRef]
- Maheu, C.; Parkinson, M. Supporting cancer survivors’ return to work: E-course for primary care providers. J. Fam. Pract. Oncol. 2021, 36, 2–3. Available online: http://www.bccancer.bc.ca/family-oncology-network-site/Documents/2021SpringFPONjournal_Apr29web.pdf (accessed on 21 July 2022).
- Leensen, M.C.J.; Groeneveld, I.F.; Rejda, T.; Groenenboom, P.; van Berkel, S.; Brandon, T.; de Boer, A.G.E.M.; Frings-Dresen, M.H.W. Feasibility of a multidisciplinary intervention to help cancer patients return to work. Eur. J. Cancer Care 2018, 27, e12690. [Google Scholar] [CrossRef]
- Sheppard, D.M.; Frost, D.; Jefford, M.; O’Connor, M.; Halkett, G. “Beyond Cancer”: A study protocol of a multimodal occupational rehabilitation programme to support breast cancer survivors to return work. BMJ Open 2019, 9, e032505. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, D.M.; Frost, D.; Jefford, M.; O’Connor, M.; Halkett, G. Building a novel occupational rehabilitation program to support cancer survivors to return to health, wellness, and work in Australia. J. Cancer Surviv. 2020, 14, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Greidanus, M.A.; de Boer, A.G.E.M.; de Rijk, A.E.; Frings-Dresen, M.H.W.; Tamminga, S.J. The MiLES intervention targeting employers to promote successful return to work of employees with cancer: Design of a pilot randomised controlled trial. Trials 2020, 21, 363. [Google Scholar] [CrossRef]
- Hunter, E.G.; Gibson, R.W.; Arbesman, M.; D’Amico, M. Systematic Review of Occupational Therapy and Adult Cancer Rehabilitation: Part 2. Impact of Multidisciplinary Rehabilitation and Psychosocial, Sexuality, and Return-to-Work Interventions. Am. J. Occup. Ther. 2017, 71, 7102100040p1–7102100040p8. [Google Scholar] [CrossRef]
- Kovacevic, N.; Žagar, T.; Homar, V.; Pelhan, B.; Sremec, M.; Rozman, T.; Besic, N. Benefits of early integrated and vocational rehabilitation in breast cancer on work ability, sick leave duration, and disability rates. Healthcare 2024, 12, 2433. [Google Scholar] [CrossRef] [PubMed]
- Zaman, A.C.G.N.M.; Tytgat, K.M.A.J.; Klinkenbijl, J.H.G.; den Boer, F.C.; Brink, M.A.; Brinkhuis, J.C.; Bruinvels, D.J.; Dol, L.C.M.; van Duijvendijk, P.; Hemmer, P.H.J.; et al. Effectiveness of a Tailored Work-Related Support Intervention for Patients Diagnosed with Gastrointestinal Cancer: A Multicenter Randomized Controlled Trial. J. Occup. Rehabil. 2021, 31, 323–338. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.N.; Nambiema, A.; Porro, B.; Descatha, A.; Aublet-Cuvelier, A.; Evanoff, B.; Roquelaure, Y. Effectiveness of Physical Activity Interventions on Return to Work After a Cancer Diagnosis: A Systematic Review and Meta-analysis. J. Occup. Rehabil. 2023, 33, 4–19. [Google Scholar] [CrossRef]
- Silver, J.K. Cancer prehabilitation and its role in improving health outcomes and reducing health care costs. Semin. Oncol. Nurs. 2015, 31, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Black, O.; Keegel, T.; Sim, M.R.; Collie, A.; Smith, P. The Effect of Self-Efficacy on Return-to-Work Outcomes for Workers with Psychological or Upper-Body Musculoskeletal Injuries: A Review of the Literature. J. Occup. Rehabil. 2018, 28, 16–27. [Google Scholar] [CrossRef]
- Rick, O.; Kalusche, E.-M.; Dauelsberg, T.; König, V.; Korsukéwitz, C.; Seifart, U. Reintegrating cancer patients into the workplace. Dtsch. Arztebl. Int. 2012, 109, 702–708. [Google Scholar] [CrossRef]
- Lieb, M.; Wünsch, A.; Schieber, K.; Bergelt, C.; Faller, H.; Geiser, F.; Goerling, U.; Hönig, K.; Hornemann, B.; Maatouk, I.; et al. Return to work after cancer: Improved mental health in working cancer survivors. Psychooncology 2022, 31, 893–901. [Google Scholar] [CrossRef]
- Bijker, R.; Duijts, S.F.A.; Smith, S.N.; de Wildt-Liesveld, R.; Anema, J.R.; Regeer, B.J. Functional Impairments and Work-Related Outcomes in Breast Cancer Survivors: A Systematic Review. J. Occup. Rehabil. 2018, 28, 429–451. [Google Scholar] [CrossRef]
- Zomkowski, K.; Cruz de Souza, B.; Pinheiro da Silva, F.; Moreira, G.M.; de Souza Cunha, N.; Sperandio, F.F. Physical symptoms and working performance in female breast cancer survivors: A systematic review. Disabil. Rehabil. 2018, 40, 1485–1493. [Google Scholar] [CrossRef]
- Lorig, K.R.; Sobel, D.S.; Ritter, P.L.; Laurent, D.; Hobbs, M. Effect of a self-management program on patients with chronic disease. Eff. Clin. Pract. 2001, 4, 256–262. [Google Scholar]
- Ritter, P.L.; Lorig, K. The English and Spanish Self-Efficacy to Manage Chronic Disease Scale measures were validated using multiple studies. J. Clin. Epidemiol. 2014, 67, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Fassier, J.-B.; Lamort-Bouché, M.; Broc, G.; Guittard, L.; Péron, J.; Rouat, S.; Carretier, J.; Fervers, B.; Letrilliart, L.; Sarnin, P. Developing a Return to Work Intervention for Breast Cancer Survivors with the Intervention Mapping Protocol: Challenges and Opportunities of the Needs Assessment. Front. Public Health 2018, 6, 35. [Google Scholar] [CrossRef] [PubMed]
- Fassier, J.-B.; Guittard, L.; Fervers, B.; Rouat, S.; Sarnin, P.; Carretier, J.; Broc, G.; Letrilliart, L.; Péron, J.; Lamort-Bouché, M. Using intervention mapping to facilitate and sustain return-to work after breast cancer: Protocol for the FASTRACS multicentre randomized controlled trial. BMC Cancer 2024, 24, 1107. [Google Scholar] [CrossRef]
- Kausto, J.; Miranda, H.; Martimo, K.-P.; Viikari-Juntura, E. Partial sick leave--review of its use, effects and feasibility in the Nordic countries. Scand. J. Work Environ. Health 2008, 34, 239–249. [Google Scholar] [CrossRef] [PubMed]
| Variable | iCanWork (n = 12) | Control (n = 11) | Total (n = 23) |
|---|---|---|---|
| Age (years) | Mean (SD): 43.08 ± 9.22 | Mean (SD): 48.27 ± 8.34 | Mean (SD): 45.57 ± 9.01 |
| Months to RTW | Mean (SD): 9.75 ± 5.34 | Mean (SD): 12.55 ± 6.56 | Mean (SD): 11.09 ± 5.99 |
| Gender | |||
| Women | 12 (100.0%) | 10 (90.9%) | 22 (95.7%) |
| Men | 0 (0.0%) | 1 (9.1%) | 1 (4.3%) |
| Marital Status | |||
| Married/Common law | 10 (62.5%) | 6 (37.5%) | 16 (69.6%) |
| Never Married | 2 (50.0%) | 2 (50.0%) | 4 (17.4%) |
| Separated | 0 (0.0%) | 2 (100.0%) | 2 (8.7%) |
| Other | 0 (0.0%) | 1 (100.0%) | 1 (4.3%) |
| Education | |||
| Less than High School | 0 (0.0%) | 1 (100.0%) | 1 (4.3%) |
| High School Graduate | 1 (100.0%) | 0 (0.0%) | 1 (4.3%) |
| Some College | 1 (33.3%) | 2 (66.7%) | 3 (13.0%) |
| University/College Graduate | 6 (46.2%) | 7 (53.8%) | 13 (56.5%) |
| Postgraduate | 4 (80.0%) | 1 (20.0%) | 5 (21.7%) |
| Diagnosis | |||
| Breast Cancer | 11 (91.7%) | 8 (72.7%) | 19 (82.6%) |
| Non-Hodgkin Lymphoma | 1 (8.3%) | 2 (18.2%) | 3 (13.0%) |
| Oral Cancer | 0 (0.0%) | 1 (9.1%) | 1 (4.3%) |
| Treatment | |||
| Chemotherapy (Yes) | 9 (75.0%) | 9 (81.8%) | 18 (78.3%) |
| Radiation (Yes) | 5 (41.7%) | 5 (45.5%) | 10 (43.5%) |
| ID | Before RTW | After RTW | Reasons |
|---|---|---|---|
| P1 | 1 VR | 2 VR | Met the benchmark for before and after RTW |
| P2 | 2 VR, 1 OT | 1 VR | Met the benchmark for before and after RTW |
| P3 | 2 VR, 1 OT | 0 | Met before RTW; unmet after RTW due to scheduling issues |
| P4 | 1 VR, 1 OT | 1 VR | Met the benchmark for before and after RTW |
| P5 | 1 VR, 1 OT | 1 VR | Met the benchmark for before and after RTW |
| P6 | 2 VR, 1 OT | 0 | Met before RTW; unmet after RTW due to scheduling issues |
| P7 | 2 VR, 0 OT | 0 | Met before RTW; OT not delivered despite attempts; RTW not attempted |
| P8 | 2 VR, 1 OT | 0 | Met before RTW; RTW not attempted during study time frame |
| P9 | 1 VR, 1 OT | 1 VR | Met the benchmark for before and after RTW |
| P10 | 2 VR, 1 OT | 0 | Met before RTW; RTW not attempted during study time frame |
| P11 | 1 VR | 0 | Met before RTW; study ended before additional VR could occur |
| P12 | 1 VR | 0 | Met before RTW; study ended before additional VR could occur |
| Domain | Item | Intervention Count Agree (%) (n = 12) | Control Count Agree (%) (n = 5) |
|---|---|---|---|
| Satisfaction with Intervention | I am satisfied with the quality of the intervention I received (Item 1). | 9 (75.0%) | 2 (40.0%) |
| The interventionist listened to what I was trying to say (Item 2). | 12 (100.0%) | 2 (40.0%) | |
| My needs were met by the program (Item 3). | 8 (66.7%) | 2 (40.0%) | |
| The interventionist provided an adequate explanation (Item 4). | 12 (100.0%) | 2 (40.0%) | |
| I would recommend the program to a friend (Item 5). | 9 (75.0%) | 2 (40.0%) | |
| The interventionist was not negative or critical towards me (Item 6). | 9 (75.0%) | 2 (40.0%) | |
| I would return to the program if I needed help (Item 7). | 9 (75.0%) | 2 (40.0%) | |
| Satisfaction with Therapist | The interventionist was friendly and warm towards me (Item 8). | 12 (100.0%) | 2 (40.0%) |
| I am now able to deal more effectively with my problems (Item 9). | 5 (41.7%) | 2 (40.0%) | |
| I felt free to express myself (Item 10). | 12 (100.0%) | 2 (40.0%) | |
| I was able to focus on what was of real concern to me (Item 11). | 10 (83.3%) | 2 (40.0%) | |
| The interventionist seemed to understand what I was thinking and feeling (Item 12). | 9 (75.0%) | 2 (40.0%) | |
| Perceived Changes in Condition | How much did this intervention help with the specific problems that led you to the program? (Item 13) | 10 (83.3%) | 4 (80.0%) |
| RTW Status | iCanWork (n = 12) | Control (n = 11) | Total (n = 23) |
|---|---|---|---|
| Returned Full-Time | 6 (50.0%) | 4 (36.4%) | 10 (43.5%) |
| Returned Part-Time | 4 (33.3%) | 6 (54.5%) | 10 (43.5%) |
| Did Not Return to Work | 2 (16.7%) | 1 (9.1%) | 3 (13.0%) |
| Median Time to RTW (months) | 8.0 | 11.00 | 11.0 |
| Mean Time to RTW (months) | 10.4 | 13.5 | 12.1 |
| Time | WAI Category | iCanWork (n, %) | Control (n, %) | Total (n) | Mann–Whitney U | Exact p-Value |
|---|---|---|---|---|---|---|
| T1 | Poor (7–27 points) | 4 (44.4%) | 5 (55.6%) | 9 | ||
| Moderate (28–36 points) | 7 (58.3%) | 5 (41.7%) | 12 | |||
| Good (37–43 points) | 1 (50.0%) | 1 (50.0%) | 2 | 69.50 | 0.33 | |
| T2 | Poor (7–27 points) | 5 (71.4%) | 2 (28.6%) | 7 | ||
| Moderate (28–36 points) | 5 (55.6%) | 4 (44.4%) | 9 | |||
| Good (37–43 points) | 2 (66.7%) | 1 (33.3%) | 3 | 36.50 | 0.650 |
| Domain | Groups n = 12 iCanWork n = 7 Control | Baseline Mean (SD) (T1) | Three Months After Baseline (T2) Mean (SD) | p-Value (Within Group) | p-Value (Between Groups) |
|---|---|---|---|---|---|
| Physical function | iCanWork | 50.93 ± 7.845 | 50.89 ± 7.103 | 0.799 | |
| Control | 42.95 ± 6.783 | 44.31 ± 5.818 | 0.116 | 0.995 | |
| Anxiety | iCanWork | 58.75 ± 7.30 | 57.25 ± 6.70 | 0.423 | |
| Control | 59.21 ± 8.78 | 60.71 ± 9.78 | 0.753 | 0.574 | |
| Depression | iCanWork | 51.70 ± 8.05 | 53.44 ± 6.95 | 0.423 | |
| Control | 54.75 ± 9.58 | 59.11 ± 9.91 | 0.753 | 0.280 | |
| Fatigue | iCanWork | 52.23 ± 10.55 | 49.82 ± 5.57 | 0.350 | |
| Control | 58.57 ± 8.42 | 58.44 ± 8.10 | 0.753 | 0.040 * | |
| Sleep disturbance | iCanWork | 51.05 ± 10.90 | 47.92 ± 10.61 | 0.173 | |
| Control | 58.66 ± 9.64 | 55.67 ± 8.38 | 0.225 | 0.131 | |
| Social roles and activities | iCanWork | 51.61 ± 1.39 | 51.61 ± 1.39 | 0.262 | |
| Control | 44.54 ± 6.67 | 43.63 ± 6.14 | 0.917 | 0.017 * | |
| Pain interference | iCanWork | 48.78 ± 8.098 | 49.39 ± 8.249 | 0.735 | |
| Control | 58.14 ± 10.237 | 61.47 ± 6.265 | 0.893 | 0.006 * | |
| Pain intensity | iCanWork | 2.70 (3.03) | 1.83 (2.41) | 0.262 | |
| Control | 3.80 (2.52) | 5.43 (2.15) | 0.202 | 0.063 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maheu, C.; Parkinson, M.; Johnson, K.; Tock, W.L.; Dolgoy, N.; Dupuis, S.-P.; Singh, M. Pilot Randomized Controlled Trial of iCanWork: Theory-Guided Return-to-Work Intervention for Individuals Touched by Cancer. Curr. Oncol. 2025, 32, 266. https://doi.org/10.3390/curroncol32050266
Maheu C, Parkinson M, Johnson K, Tock WL, Dolgoy N, Dupuis S-P, Singh M. Pilot Randomized Controlled Trial of iCanWork: Theory-Guided Return-to-Work Intervention for Individuals Touched by Cancer. Current Oncology. 2025; 32(5):266. https://doi.org/10.3390/curroncol32050266
Chicago/Turabian StyleMaheu, Christine, Maureen Parkinson, Kyla Johnson, Wing Lam Tock, Naomi Dolgoy, Simon-Pierre Dupuis, and Mina Singh. 2025. "Pilot Randomized Controlled Trial of iCanWork: Theory-Guided Return-to-Work Intervention for Individuals Touched by Cancer" Current Oncology 32, no. 5: 266. https://doi.org/10.3390/curroncol32050266
APA StyleMaheu, C., Parkinson, M., Johnson, K., Tock, W. L., Dolgoy, N., Dupuis, S.-P., & Singh, M. (2025). Pilot Randomized Controlled Trial of iCanWork: Theory-Guided Return-to-Work Intervention for Individuals Touched by Cancer. Current Oncology, 32(5), 266. https://doi.org/10.3390/curroncol32050266







