A Survey Detailing Early Onset Colorectal Cancer Patient and Caregiver Experiences in Canada
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Design and Questionnaire
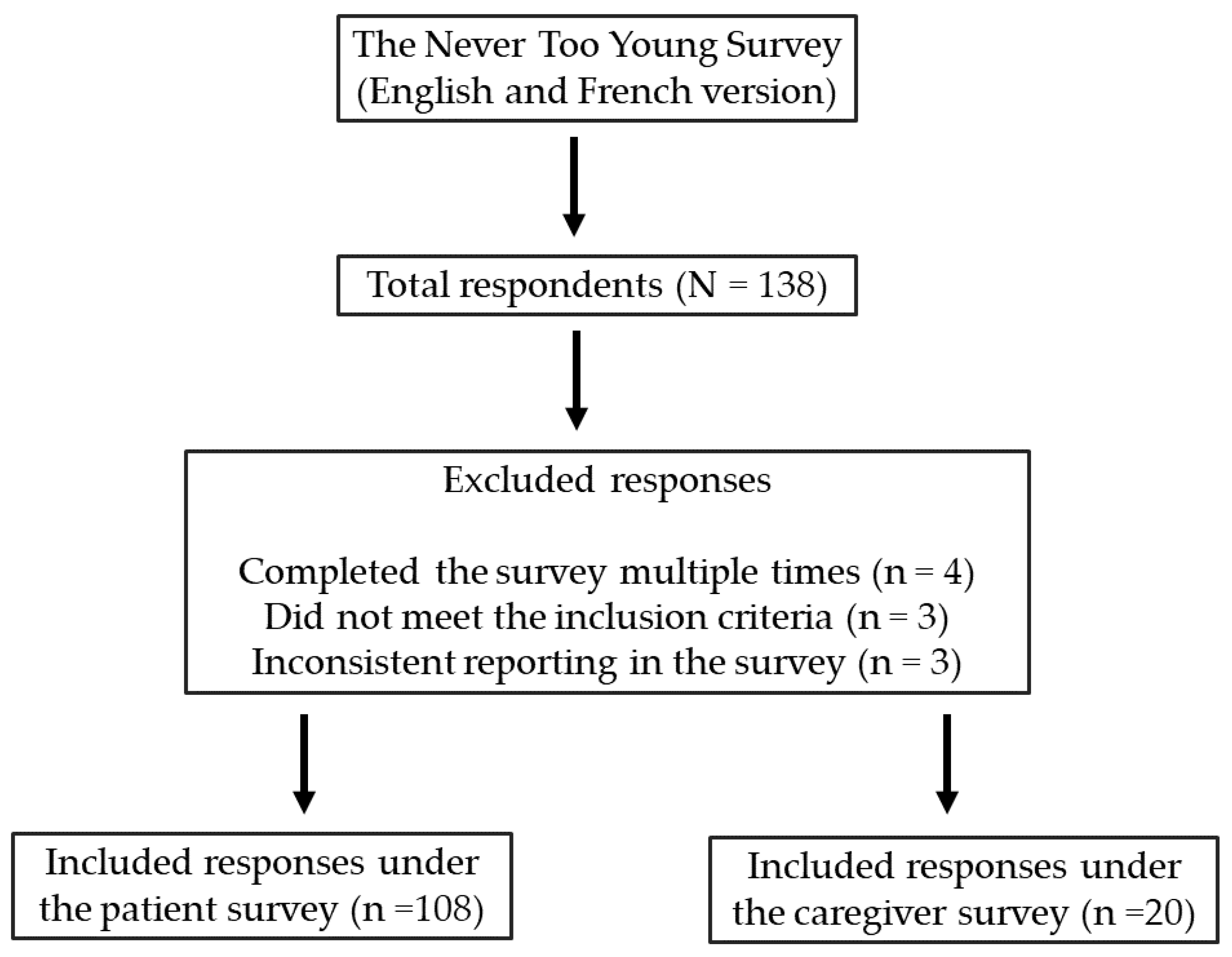
2.2. Study Population and Participant Recruitment
2.3. Data Collection
2.4. Data Analysis
2.5. Ethics Approval
3. Results
3.1. Respondent Demographics
3.2. EOCRC Awareness
3.3. Diagnosis and Patient Experiences towards Receiving a Diagnosis
3.4. Health History and Behavioral Risk Factors for Colorectal Cancer
3.5. Treatment Experiences of Early Age Onset Colorectal Cancer Patients
3.6. Sexuality and Fertility Experiences of Early Age Onset Colorectal Cancer Patients
3.7. Patient Mental Health Experiences
3.8. Caregiver Mental Health Experiences
3.9. Financial Health
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Brenner, D.R.; Gillis, J.; Demers, A.A.; Ellison, L.F.; Billette, J.-M.; Zhang, S.X.; Liu, J.L.; Woods, R.R.; Finley, C.; Fitzgerald, N.; et al. Projected estimates of cancer in Canada in 2024. CMAJ 2024, 196, E615–E623. [Google Scholar] [CrossRef] [PubMed]
- Canadian Cancer Statistics Advisory Committee. Canadian Cancer Statistics 2023. Available online: https://cancer.ca/en/research/cancer-statistics (accessed on 7 November 2023).
- Brenner, D.R.; Ruan, Y.; Shaw, E.; De, P.; Heitman, S.J.; Hilsden, R.J. Increasing Colorectal Cancer Incidence Trends among Younger Adults in Canada. Prev. Med. 2017, 105, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D.R.; Heer, E.; Sutherland, R.L.; Ruan, Y.; Tinmouth, J.; Heitman, S.J.; Hilsden, R.J. National Trends in Colorectal Cancer Incidence Among Older and Younger Adults in Canada. JAMA Netw. Open 2019, 2, e198090. [Google Scholar] [CrossRef] [PubMed]
- AlZaabi, A.; AlHarrasi, A.; AlMusalami, A.; AlMahyijari, N.; Al Hinai, K.; AlAdawi, H.; Al-Shamsi, H.O. Early Onset Colorectal Cancer: Challenges across the Cancer Care Continuum. Ann. Med. Surg. 2022, 82, 104453. [Google Scholar] [CrossRef] [PubMed]
- Colorectal Cancer Canada. Never Too Young for Colorectal Cancer. Patient & Caregiver Survey Report. Available online: https://www.colorectalcancercanada.com/app/uploads/2021/04/FINAL-ENG-N2Y-Survey-Report-Apr2021.pdf (accessed on 7 November 2023).
- Wolf, A.M.D.; Fontham, E.T.H.; Church, T.R.; Flowers, C.R.; Guerra, C.E.; LaMonte, S.J.; Etzioni, R.; McKenna, M.T.; Oeffinger, K.C.; Shih, Y.-C.T.; et al. Colorectal Cancer Screening for Average-Risk Adults: 2018 Guideline Update from the American Cancer Society. CA Cancer J. Clin. 2018, 68, 250–281. [Google Scholar] [CrossRef] [PubMed]
- Recommendations on Screening for Colorectal Cancer in Primary Care. CMAJ 2016, 188, 340–348. [CrossRef] [PubMed]
- Never Too Young Survey and Report 2020. Colorectal Cancer Alliance. Findings from an Online Survey of Young-Onset Colorectal Cancer Patients and Survivors. Available online: https://www.ccalliance.org/about/never-too-young/survey (accessed on 7 November 2023).
- Survival Statistics for Colorectal Cancer. Available online: https://cancer.ca/en/cancer-information/cancer-types/colorectal/prognosis-and-survival/survival-statistics (accessed on 7 November 2023).
- Colorectal Cancer Canada. Never Too Young For Colorectal Cancer Program Update. 2022. Available online: https://www.colorectalcancercanada.com/app/uploads/2022/05/N2Y-MAY-2022-Program-Brief-All-updated.pdf (accessed on 7 November 2023).
- Inflammatory Bowel Disease (IBD) (2021) Canada.Ca. Available online: https://www.canada.ca/en/public-health/services/chronic-diseases/inflammatory-bowel-disease.html (accessed on 7 November 2023).
- Mounsey, A.L.; Halladay, J.; Sadiq, T.S. Hemorrhoids. Am. Fam. Physician 2011, 84, 204–210. [Google Scholar] [PubMed]
- Bowel Cancer, UK. Never Too Young Report. Available online: https://www.bowelcanceruk.org.uk/campaigning/never-too-young/ (accessed on 7 November 2023).
- Vuik, F.E.; Nieuwenburg, S.A.; Bardou, M.; Lansdorp-Vogelaar, I.; Dinis-Ribeiro, M.; Bento, M.J.; Zadnik, V.; Pellisé, M.; Esteban, L.; Kaminski, M.F.; et al. Increasing Incidence of Colorectal Cancer in Young Adults in Europe over the Last 25 Years. Gut 2019, 68, 1820–1826. [Google Scholar] [CrossRef] [PubMed]
- Goldvaser, H.; Purim, O.; Kundel, Y.; Shepshelovich, D.; Shochat, T.; Shemesh-Bar, L.; Sulkes, A.; Brenner, B. Colorectal Cancer in Young Patients: Is It a Distinct Clinical Entity? Int. J. Clin. Oncol. 2016, 21, 684–695. [Google Scholar] [CrossRef]
- Fu, J.; Yang, J.; Tan, Y.; Jiang, M.; Wen, F.; Huang, Y.; Chen, H.; Yi, C.; Zheng, S.; Yuan, Y. Young Patients (≤35 Years Old) with Colorectal Cancer Have Worse Outcomes Due to More Advanced Disease: A 30-Year Retrospective Review. Medicine 2014, 93, e135. [Google Scholar] [CrossRef]
- Siegel, R.L.; Torre, L.A.; Soerjomataram, I.; Hayes, R.B.; Bray, F.; Weber, T.K.; Jemal, A. Global Patterns and Trends in Colorectal Cancer Incidence in Young Adults. Gut 2019, 68, 2179–2185. [Google Scholar] [CrossRef] [PubMed]
- Aminisani, N.; Nikbakht, H.; Jafarabadi, M.A.; Shamshirgaran, S.M. Depression, Anxiety, and Health Related Quality of Life among Colorectal Cancer Survivors. J. Gastrointest. Oncol. 2017, 8, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.; Oveisi, N.; McTaggart-Cowan, H.; Loree, J.M.; Murphy, R.A.; De Vera, M.A. Colorectal Cancer and Onset of Anxiety and Depression: A Systematic Review and Meta-Analysis. Curr. Oncol. 2022, 29, 8751–8766. [Google Scholar] [CrossRef] [PubMed]
- Sanford, S.D.; Zhao, F.; Salsman, J.M.; Chang, V.T.; Wagner, L.I.; Fisch, M.J. Symptom Burden among Young Adults with Breast or Colorectal Cancer. Cancer 2014, 120, 2255–2263. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.E.; Cao, H.S.T.; Hu, C.-Y.; Chang, G.J.; Feig, B.W.; Rodriguez-Bigas, M.A.; Nguyen, S.T.; Skibber, J.M.; You, Y.N. Functional Deficits and Symptoms of Long-Term Survivors of Colorectal Cancer Treated by Multimodality Therapy Differ by Age at Diagnosis. J. Gastrointest. Surg. 2015, 19, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Perl, G.; Nordheimer, S.; Lando, S.; Benedict, C.; Brenner, B.; Perry, S.; Shmoisman, G.; Purim, O.; Amit, L.; Stemmer, S.M.; et al. Young Patients and Gastrointestinal (GI) Tract Malignancies—Are We Addressing the Unmet Needs? BMC Cancer 2016, 16, 630. [Google Scholar] [CrossRef] [PubMed]
- Salz, T.; Baxi, S.S.; Blinder, V.S.; Elkin, E.B.; Kemeny, M.M.; McCabe, M.S.; Moskowitz, C.S.; Onstad, E.E.; Saltz, L.B.; Temple, L.K.F.; et al. Colorectal Cancer Survivors’ Needs and Preferences for Survivorship Information. J. Oncol. Pract. 2014, 10, e277–e282. [Google Scholar] [CrossRef] [PubMed]
- Heyne, S.; Esser, P.; Geue, K.; Friedrich, M.; Mehnert-Theuerkauf, A. Frequency of Sexual Problems and Related Psychosocial Characteristics in Cancer Patients-Findings From an Epidemiological Multicenter Study in Germany. Front. Psychol. 2021, 12, 679870. [Google Scholar] [CrossRef]
- Ussher, J.M.; Perz, J.; Gilbert, E.; The Australian Cancer and Sexuality Study Team. Perceived Causes and Consequences of Sexual Changes after Cancer for Women and Men: A Mixed Method Study. BMC Cancer 2015, 15, 268. [Google Scholar] [CrossRef]
- Reese, J.B.; Handorf, E.; Haythornthwaite, J.A. Sexual Quality of Life, Body Image Distress, and Psychosocial Outcomes in Colorectal Cancer: A Longitudinal Study. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2018, 26, 3431–3440. [Google Scholar] [CrossRef]
- Blum-Barnett, E.; Madrid, S.; Burnett-Hartman, A.; Mueller, S.R.; McMullen, C.K.; Dwyer, A.; Feigelson, H.S. Financial Burden and Quality of Life among Early-Onset Colorectal Cancer Survivors: A Qualitative Analysis. Health Expect. 2019, 22, 1050–1057. [Google Scholar] [CrossRef] [PubMed]
- Mo, M.; Jia, P.; Zhu, K.; Huang, W.; Han, L.; Liu, C.; Huang, X. Financial Toxicity Following Surgical Treatment for Colorectal Cancer: A Cross-Sectional Study. Support. Care Cancer 2023, 31, 110. [Google Scholar] [CrossRef] [PubMed]

| Variable. | Total N | % |
|---|---|---|
| Doctor seen at symptom onset | ||
| Primary care provider | 93 | 56.2 |
| Pediatrician | 1 | 0.6 |
| Gastroenterologist | 16 | 9.9 |
| Emergency room doctor | 28 | 17.3 |
| OBGYN | 3 | 1.9 |
| Urologist | 1 | 0.6 |
| Urgent care | 9 | 5.6 |
| Surgeon | 6 | 3.7 |
| Other | 7 | 4.3 |
| Time between symptoms onset and seeking medical attention | ||
| <1 month | 22 | 21.8 |
| 1–3 months | 30 | 29.7 |
| 3–6 months | 15 | 14.9 |
| 6+ months | 34 | 33.7 |
| Received a rectal exam prior to diagnosis | ||
| Yes | 45 | 43.3 |
| No | 55 | 52.9 |
| N/A | 4 | 3.8 |
| Doctor that led to colonoscopy | ||
| Family/primary care provider | 54 | 45.0 |
| Gastroenterologist | 21 | 17.5 |
| Emergency room doctor | 16 | 13.3 |
| OBGYN | 1 | 0.8 |
| Urgent care with ER | 1 | 0.8 |
| Pediatrician | 1 | 0.8 |
| Surgeon | 21 | 17.5 |
| Other (please specify) | 5 | 4.2 |
| Level of concern by doctors following description of symptoms | ||
| They did not seem concerned | 47 | 45.2 |
| They seemed slightly concerned | 22 | 21.2 |
| They seemed moderately concerned | 23 | 22.1 |
| They seemed very concerned | 12 | 11.5 |
| Felt that doctors dismissed the signs and symptoms of colorectal cancer due to patient age | ||
| Yes | 63 | 51.2 |
| No | 52 | 42.3 |
| I do not know | 7 | 5.7 |
| Yes, but for a reason other than age | 1 | 0.8 |
| Mistaken diagnosis | ||
| None of the below | 56 | 32.6 |
| Hemorrhoids | 38 | 22.1 |
| Symptoms of childbirth | 8 | 4.7 |
| Appendicitis | 3 | 1.7 |
| Gynecological issues | 7 | 4.1 |
| IBS | 10 | 5.8 |
| IBD | 3 | 1.7 |
| Mental health issues | 7 | 4.1 |
| Crohn’s/Colitis | 11 | 6.4 |
| Other | 29 | 16.9 |
| Variable | Colon Cancer | Rectal Cancer | ||
|---|---|---|---|---|
| Total N | % | Total N | % | |
| Did any of your providers discuss sexual side effects due to radiation and surgery before treatment? | ||||
| Painful sex | 1 | 1% | >10 | 15% |
| Decrease in sex drive | 3–10 | 7% | >10 | 17% |
| Loss of sexual function | 3–10 | 9% | >10 | 19% |
| Infertility | >10 | 16% | >10 | 28% |
| I do not remember | >10 | 16% | 1 | 1% |
| Providers did not discuss any of the above | >10 | 49% | >10 | 20% |
| Did you experience any of the following after treatment? | ||||
| Painful sex | 3–10 | 13% | >10 | 22% |
| Decrease in sex drive | >10 | 49% | >10 | 33% |
| Loss of sexual function | 3–10 | 13% | >10 | 20% |
| Infertility | 2 | 3% | >10 | 17% |
| I do not remember | 3–10 | 16% | 3 | 3% |
| Prefer not to answer | 3–10 | 6% | 3–10 | 4% |
| Sexual function issues after treatment and surgery | ||||
| No loss of sexual function | 32 | 56% | 16 | 35% |
| Partial loss of sexual function | 15 | 26% | 16 | 35% |
| Total loss of sexual function | 0 | 0% | 6 | 13% |
| Prefer not to answer | 3 | 5% | 4 | 9% |
| Even with guidance from medical staff, I am still afraid to have sex | ||||
| Always | 0 | 0% | 4 | 10% |
| Often | 3 | 7% | 8 | 21% |
| Sometimes | 4 | 9% | 9 | 23% |
| Never | 33 | 73% | 15 | 38% |
| Prefer not to say | 5 | 11% | 3 | 8% |
| Sexual dysfunction puts a strain on relationships | ||||
| Always | 2 | 5% | 4 | 10% |
| Often | 2 | 5% | 7 | 18% |
| Sometimes | 11 | 28% | 11 | 28% |
| Never | 23 | 58% | 16 | 41% |
| Prefer not to say | 2 | 5% | 1 | 3% |
| Sexual dysfunction affects ability to become intimate with others | ||||
| Always | 1 | 2% | 6 | 16% |
| Often | 3 | 7% | 9 | 24% |
| Sometimes | 12 | 29% | 11 | 30% |
| Never | 22 | 54% | 10 | 27% |
| Prefer not to say | 3 | 7% | 1 | 3% |
| Feel awkward to receive guidance for sexual life | ||||
| Always | 2 | 5% | 4 | 12% |
| Often | 3 | 7% | 2 | 6% |
| Sometimes | 12 | 28% | 11 | 33% |
| Never | 22 | 51% | 15 | 45% |
| Prefer not to say | 4 | 9% | 1 | 3% |
| I believe that I am not a complete person due to sexual dysfunction | ||||
| Always | 1 | 3% | 7 | 18% |
| Often | 3 | 8% | 4 | 11% |
| Sometimes | 4 | 10% | 11 | 29% |
| Never | 29 | 73% | 15 | 39% |
| Prefer not to say | 3 | 8% | 1 | 3% |
| I worry that I am not enough for a significant other due to sexual dysfunction | ||||
| Always | 2 | 5% | 7 | 18% |
| Often | 2 | 5% | 10 | 26% |
| Sometimes | 10 | 25% | 8 | 21% |
| Never | 21 | 53% | 12 | 32% |
| Prefer not to say | 5 | 13% | 1 | 3% |
| Medical professional discussed fertility preservation during diagnosis or treatment | ||||
| No | 27 | 43% | 22 | 47% |
| Reproductive health issues prior to treatment | ||||
| No | 39 | 62% | 33 | 69% |
| Treatment resulted in sterility or infertility | ||||
| No | 16 | 26% | 7 | 15% |
| Gaps | Recommendations |
|---|---|
| Delayed diagnosis |
|
| Misdiagnosis and Dismissal |
|
| Lack of Mental Health Support |
|
| Financial Toxicity |
|
| Inadequate Communication |
|
| Caregiver Support |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Auer, R.; Meszaros, C.; Fossouo, L.; Vandermeer, L.; Stein, B.D. A Survey Detailing Early Onset Colorectal Cancer Patient and Caregiver Experiences in Canada. Curr. Oncol. 2024, 31, 3149-3160. https://doi.org/10.3390/curroncol31060238
Auer R, Meszaros C, Fossouo L, Vandermeer L, Stein BD. A Survey Detailing Early Onset Colorectal Cancer Patient and Caregiver Experiences in Canada. Current Oncology. 2024; 31(6):3149-3160. https://doi.org/10.3390/curroncol31060238
Chicago/Turabian StyleAuer, Rebecca, Claudia Meszaros, Lucresse Fossouo, Lisa Vandermeer, and Barry D. Stein. 2024. "A Survey Detailing Early Onset Colorectal Cancer Patient and Caregiver Experiences in Canada" Current Oncology 31, no. 6: 3149-3160. https://doi.org/10.3390/curroncol31060238
APA StyleAuer, R., Meszaros, C., Fossouo, L., Vandermeer, L., & Stein, B. D. (2024). A Survey Detailing Early Onset Colorectal Cancer Patient and Caregiver Experiences in Canada. Current Oncology, 31(6), 3149-3160. https://doi.org/10.3390/curroncol31060238





