An Evaluation of 90Y Bremsstrahlung SPECT Image Quality in the Presence of 99mTc: A Technical Perspective on Same-Day Radioembolization
Abstract
1. Introduction
2. Materials and Methods
2.1. Phantom Preparation
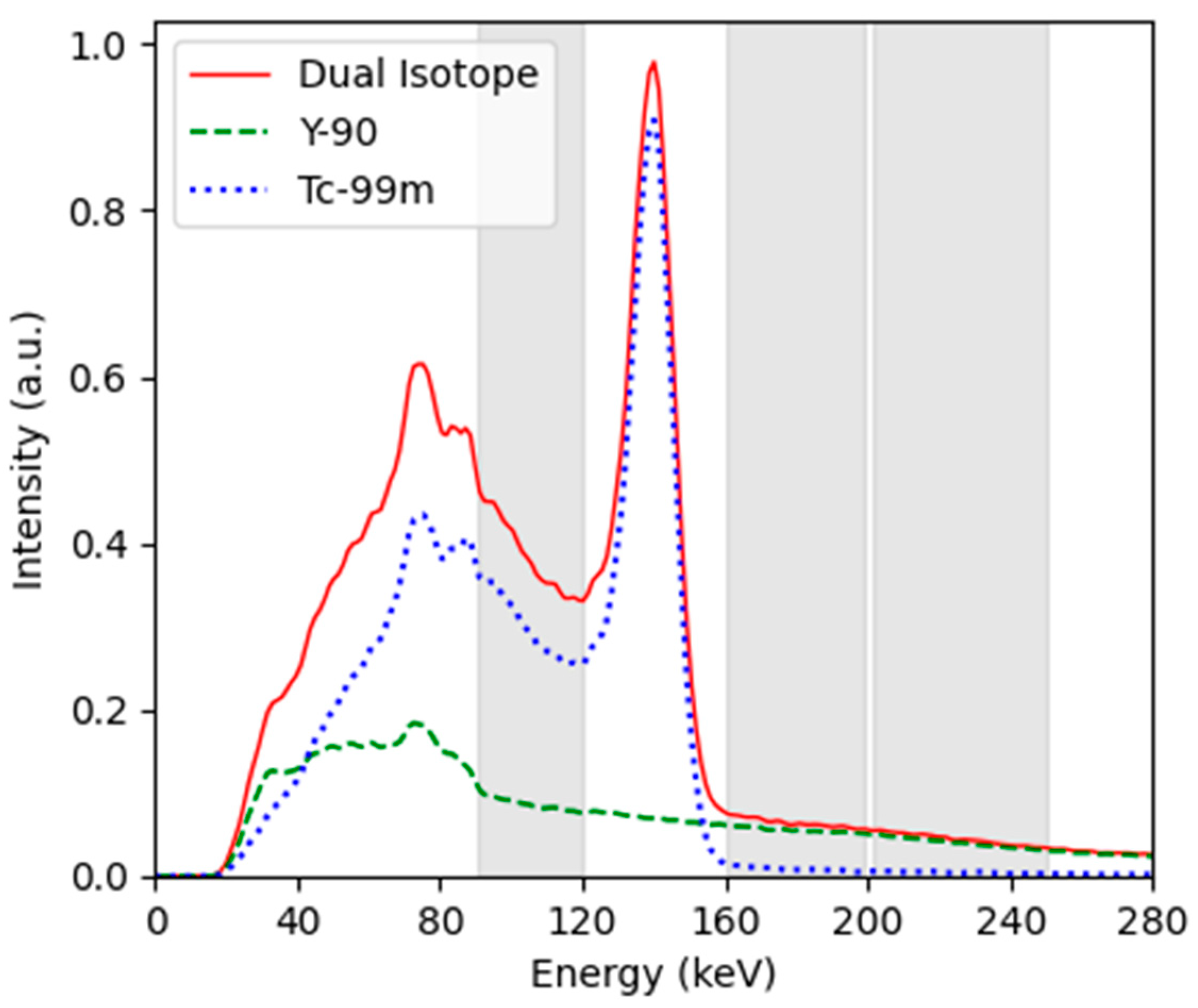
2.2. Imaging
2.3. Image Quality Analysis
3. Results
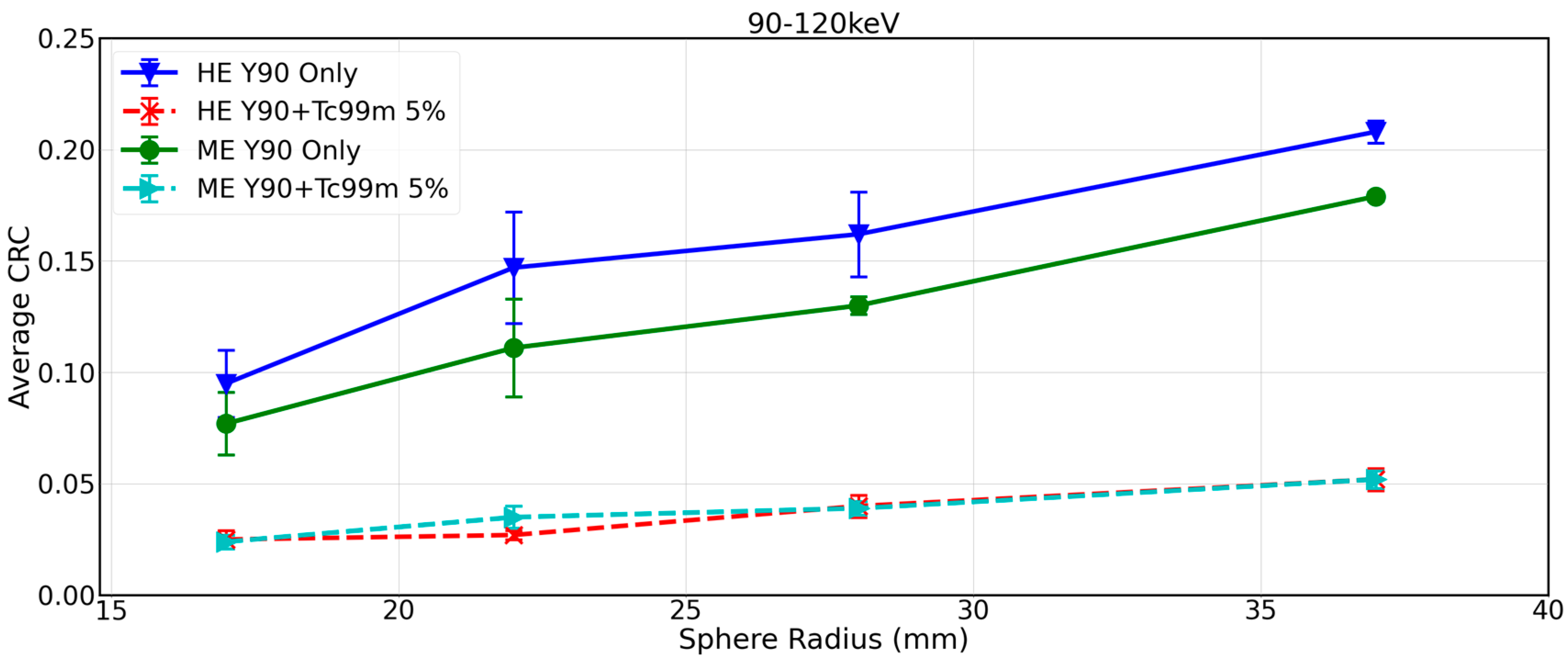
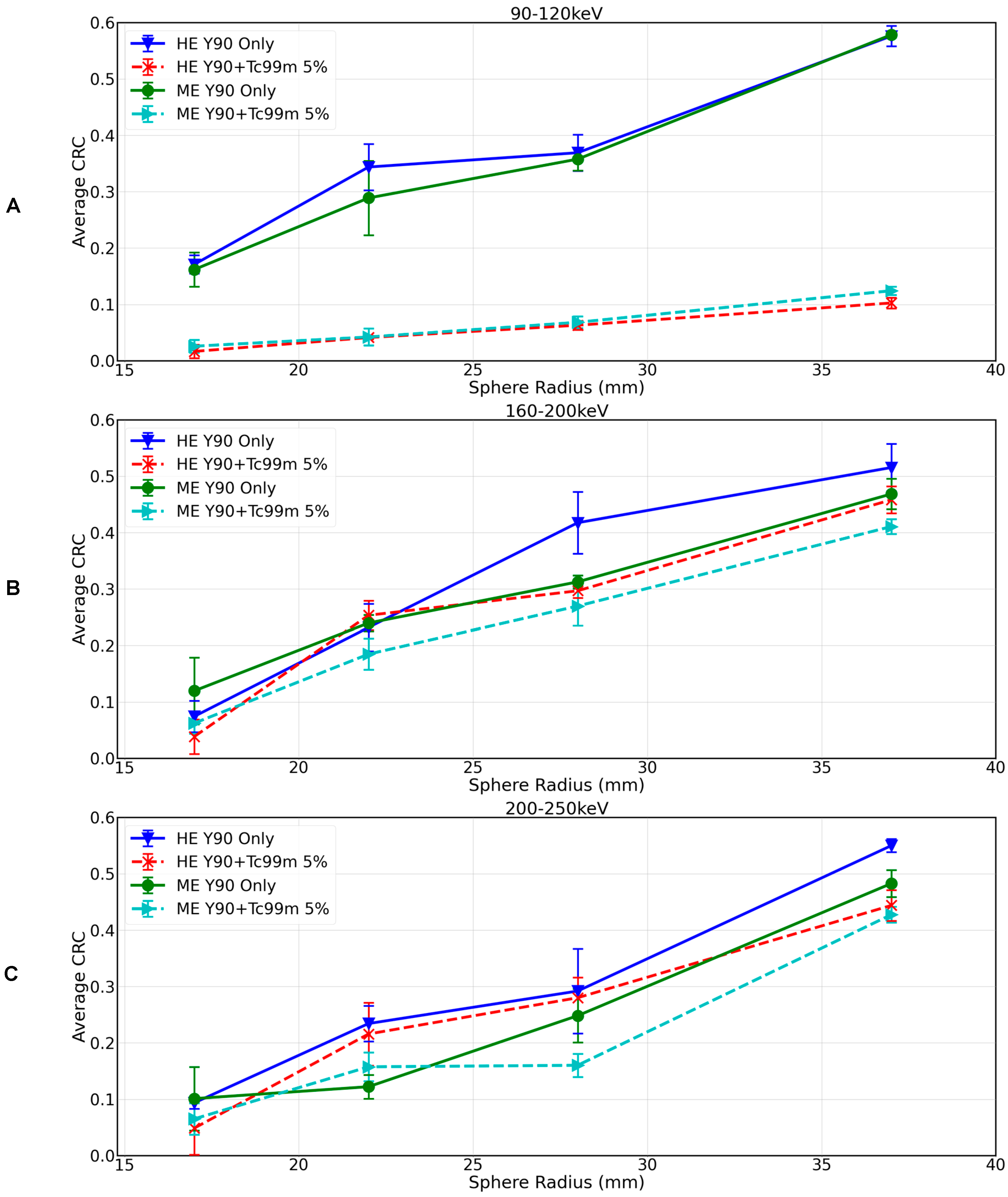
3.1. Impact of 99mTc on 90Y Bremsstrahlung SPECT/CT with Local Site Protocol
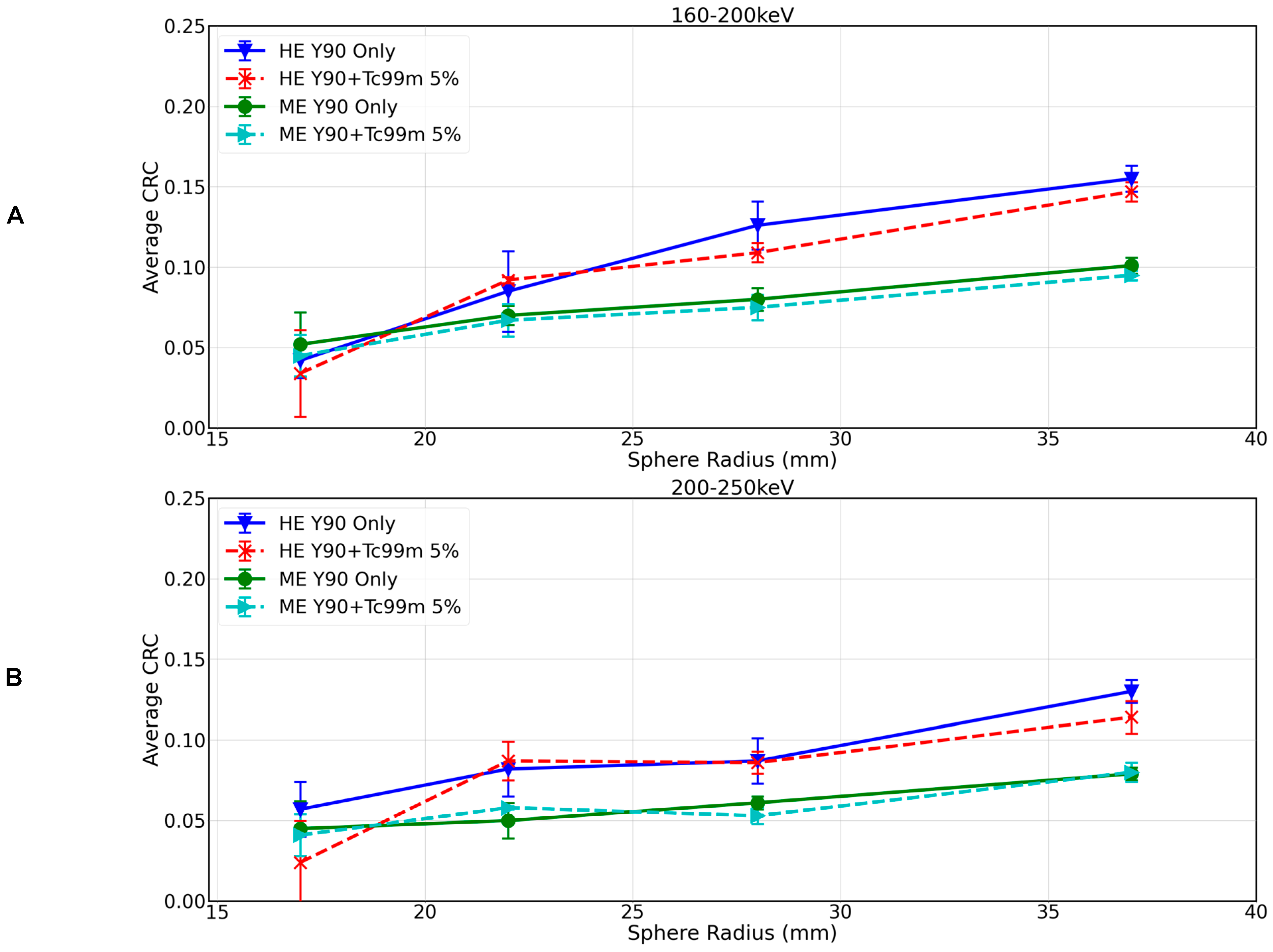
3.2. Impact of 99mTc on 90Y Bremsstrahlung SPECT/CT with Same-Day SIRT Protocols Applicable to Commercial Imaging Systems
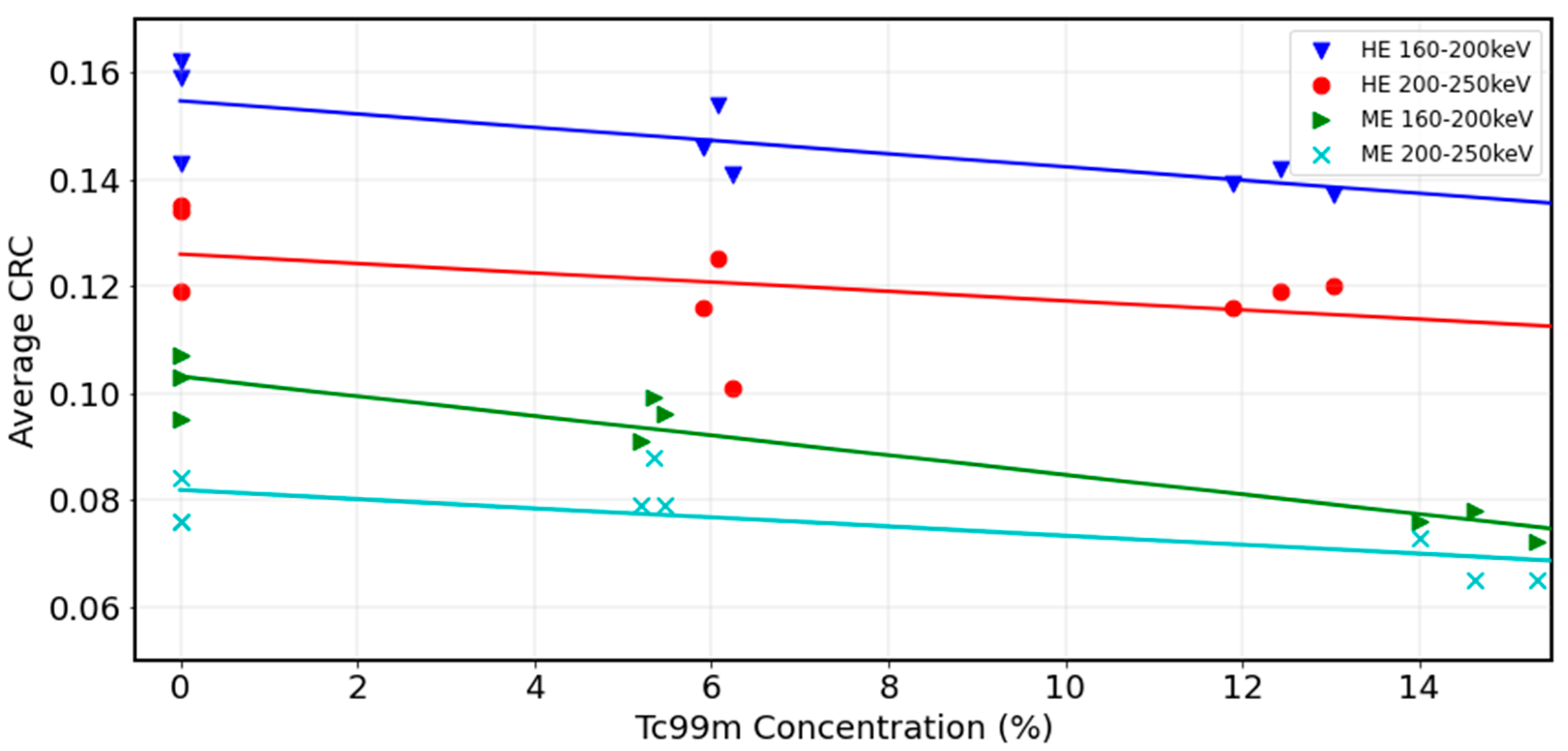
3.3. Impact of 99mTc on 90Y Bremsstrahlung SPECT/CT with Same-Day SIRT Protocols Including Advanced Reconstruction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Chiesa, C.; Sjogreen-Gleisner, K.; Walrand, S.; Strigari, L.; Flux, G.; Gear, J.; Stokke, C.; Gabina, P.M.; Bernhardt, P.; Konijnenberg, M. EANM dosimetry committee series on standard operational procedures: A unified methodology for 99mTc-MAA pre- and 90Y peri-therapy dosimetry in liver radioembolization with 90Y microspheres. EJNMMI Phys. 2021, 8, 77. [Google Scholar] [CrossRef] [PubMed]
- Gates, V.L.; Marshall, K.G.; Salzig, K.; Williams, M.; Lewandowski, R.J.; Salem, R. Outpatient single-session yttrium-90 glass microsphere radioembolization. J. Vasc. Interv. Radiol. 2014, 25, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Li, M.D.; Chu, K.F.; DePietro, A.; Wu, V.; Wehrenberg-Klee, E.; Zurkiya, O.; Liu, R.W.; Ganguli, S. Same-Day Yttrium-90 Radioembolization: Feasibility with Resin Microspheres. J. Vasc. Interv. Radiol. 2019, 30, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Gabr, A.; Kallini, J.R.; Gates, V.L.; Hickey, R.; Kulik, L.; Desai, K.; Thornburg, B.; Marshall, K.; Salzig, K.; Williams, M.; et al. Same-day 90Y radioembolization: Implementing a new treatment paradigm. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 2353–2359. [Google Scholar] [CrossRef]
- Levillain, H.; Bagni, O.; Deroose, C.M.D.; Dieudonné, A.; Gnesin, S.; Grosser, O.S.; Kappadath, S.C.; Kennedy, A.; Kokabi, N.; Liu, D.M.; et al. International recommendations for personalised selective internal radiation therapy of primary and metastatic liver diseases with yttrium-90 resin microspheres. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1570–1584. [Google Scholar] [CrossRef]
- Levillain, H.; Duran Derijckere, I.; Marin, G.; Guiot, T.; Vouche, M.; Reynaert, N.; Hendlisz, A.; Vanderlinden, B.; Flamen, P. 90Y-PET/CT-based dosimetry after selective internal radiation therapy predicts outcome in patients with liver metastases from colorectal cancer. EJNMMI Res. 2018, 8, 60. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.T.; Alessio, A.M.; Johnson, G.E.; Vaidya, S.; Kwan, S.W.; Monsky, W.; Wilson, A.E.; Lewis, D.H.; Padia, S.A. Prospective Trial Using Internal Pair-Production Positron Emission Tomography to Establish the Yttrium-90 Radioembolization Dose Required for Response of Hepatocellular Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2018, 101, 358–365. [Google Scholar] [CrossRef]
- Pasciak, A.S.; Bourgeois, A.C.; McKinney, J.M.; Chang, T.T.; Osborne, D.R.; Acuff, S.N.; Bradley, Y.C. Radioembolization and the Dynamic Role of (90)Y PET/CT. Front. Oncol. 2014, 4, 38. [Google Scholar] [CrossRef]
- Keane, G.; Lam, M.; Braat, A.; Bruijnen, R.; Kaufmann, N.; de Jong, H.; Smits, M. Transarterial Radioembolization (TARE) Global Practice Patterns: An International Survey by the Cardiovascular and Interventional Radiology Society of Europe (CIRSE). Cardiovasc. Intervent. Radiol. 2024, 47, 1224–1236. [Google Scholar] [CrossRef]
- Dewaraja, Y.K.; Chun, S.Y.; Srinivasa, R.N.; Kaza, R.K.; Cuneo, K.C.; Majdalany, B.S.; Novelli, P.M.; Ljungberg, M.; Fessler, J.A. Improved quantitative 90 Y bremsstrahlung SPECT/CT reconstruction with Monte Carlo scatter modeling. Med. Phys. 2017, 44, 6364–6376. [Google Scholar] [CrossRef] [PubMed]
- Siman, W.; Mikell, J.K.; Kappadath, S.C. Practical reconstruction protocol for quantitative 90Y bremsstrahlung SPECT/CT. Med. Phys. 2016, 43, 5093–5103. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Bhattacharya, M.; Frey, E.C. Simultaneous Tc-99m/I-123 dual-radionuclide myocardial perfusion/innervation imaging using Siemens IQ-SPECT with SMARTZOOM collimator. Phys. Med. Biol. 2014, 59, 2813–2828. [Google Scholar] [CrossRef] [PubMed]
- Kangasmaa, T.; Kuikka, J.; Sohlberg, A. Optimisation of simultaneous tl-201/tc-99m dual isotope reconstruction with monte-carlo-based scatter correction. Int. J. Mol. Imaging 2012, 2012, 695632. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fan, P.; Hutton, B.F.; Holstensson, M.; Ljungberg, M.; Pretorius, P.H.; Prasad, R.; Ma, T.; Liu, Y.; Wang, S.; Thorn, S.L.; et al. Scatter and crosstalk corrections for (99m)Tc/(123)I dual-radionuclide imaging using a CZT SPECT system with pinhole collimators. Med. Phys. 2015, 42, 6895–6911. [Google Scholar] [CrossRef]
- NEMA NU 2-2007; Performance Measurements of Positron Emission Tomographs. National Electrical Manufacturers Association: Rosslyn, VA, USA, 2007.
- Brunson, C.P.; McGregor, H.J.; Hennemeyer, C.T.; Patel, M.V.; Woodhead, G.J.; Young, S.J. Measurement of the Tumor-to-Normal Ratio for Radioembolization of Hepatocellular Carcinoma: A Prospective Study Comparing 2-Dimensional Perfusion Angiography, Technetium-99m Macroaggregated Albumin, and Yttrium-90 SPECT/CT. J. Vasc. Interv. Radiol. 2024, 35, 94–101. [Google Scholar] [CrossRef]
- Campbell, G.S.; Reed, D.K.; Desai, A.; TLirette, S. Liver Tumor Enhancement at Hybrid Angio-CT and Comparison with Tumor and Hepatic Parenchymal Distribution of Yttrium-90 Microspheres by Positron Emission Tomography. Cureus 2023, 15, e49861. [Google Scholar] [CrossRef]
- Attarwala, A.A.; Molina-Duran, F.; Büsing, K.A.; Schönberg, S.O.; Bailey, D.L.; Willowson, K.; Glatting, G. Quantitative and qualitative assessment of Yttrium-90 PET/CT imaging. PLoS ONE 2014, 9, e110401. [Google Scholar] [CrossRef]
- NEMA NU 1-2023; Performance Measurements of Gamma Cameras. National Electrical Manufacturers Association: Rosslyn, VA, USA, 2023.
- Elschot, M.; Lam, M.G.E.H.; van den Bosch, M.A.A.J.; Viergever, M.A.; de Jong, H.W.A.M. Quantitative Monte Carlo–Based 90Y SPECT Reconstruction. J. Nucl. Med. 2013, 54, 1557–1563. [Google Scholar] [CrossRef]
- van Nierop, B.J.; Prince, J.F.; van Rooij, R.; van den Bosch, M.A.A.J.; Lam, M.G.E.H.; de Jong, H.W.A.M. Accuracy of SPECT/CT-based lung dose calculation for Holmium-166 hepatic radioembolization before OSEM convergence. Med. Phys. 2018, 45, 3871–3879. [Google Scholar] [CrossRef]
- Elschot, M.; Smits, M.L.J.; Nijsen, J.F.W.; Lam, M.G.E.H.; Zonnenberg, B.A.; van den Bosch, M.A.A.J.; Viergever, M.A.; de Jong, H.W.A.M. Quantitative Monte Carlo-based holmium-166 SPECT reconstruction. Med. Phys. 2013, 40, 112502. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Staring, M.; Murphy, K.; Viergever, M.A.; Pluim, J.P. elastix: A toolbox for intensity-based medical image registration. IEEE Trans. Med. Imaging 2010, 29, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Shamonin, D.P.; Bron, E.E.; Lelieveldt, B.P.F.; Smits, M.; Klein, S.; Staring, M. Alzheimer’s Disease Neuroimaging Initiative. Fast parallel image registration on CPU and GPU for diagnostic classification of Alzheimer’s disease. Front. Neuroinform. 2014, 7, 50. [Google Scholar] [CrossRef]
- Labour, J.; Boissard, P.; Baudier, T.; Khayi, F.; Kryza, D.; Durebex, P.V.; Parisse-Di Martino, S.; Mognetti, T.; Sarrut, D.; Badel, J.N. Yttrium-90 quantitative phantom study using digital photon counting PET. EJNMMI Phys. 2021, 8, 56. [Google Scholar] [CrossRef]
- van Elmbt, L.; Vandenberghe, S.; Walrand, S.; Pauwels, S.; Jamar, F. Comparison of yttrium-90 quantitative imaging by TOF and non-TOF PET in a phantom of liver selective internal radiotherapy. Phys. Med. Biol. 2011, 56, 6759–6777. [Google Scholar] [CrossRef]

| Exp. | Scan Time (min) | Collimator | [Aeff] 90Y (GBq) | [Aeff] 99mTc (MBq) | % 99mTc |
|---|---|---|---|---|---|
| 1 90Y only | 20 (3 reps *) | HE | 3.2 | 0 | 0% |
| 2 90Y only | 20 (3 reps) | ME | 3.1 | 0 | 0% |
| 3 90Y+99mTc | 20 (3 reps) | ME | 3.1 | 450 | 15% |
| 4 90Y+99mTc | 20 (3 reps) | HE | 3.0 | 376 | 13% |
| 5 90Y+99mTc | 25 (3 reps) | HE | 3.1 | 189 | 6% |
| 6 90Y+99mTc | 25 (3 reps) | ME | 3.1 | 165 | 5% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keane, G.; van Rooij, R.; Lam, M.; Braat, A.; Smits, M.; de Jong, H. An Evaluation of 90Y Bremsstrahlung SPECT Image Quality in the Presence of 99mTc: A Technical Perspective on Same-Day Radioembolization. Curr. Oncol. 2024, 31, 7511-7522. https://doi.org/10.3390/curroncol31120554
Keane G, van Rooij R, Lam M, Braat A, Smits M, de Jong H. An Evaluation of 90Y Bremsstrahlung SPECT Image Quality in the Presence of 99mTc: A Technical Perspective on Same-Day Radioembolization. Current Oncology. 2024; 31(12):7511-7522. https://doi.org/10.3390/curroncol31120554
Chicago/Turabian StyleKeane, Grace, Rob van Rooij, Marnix Lam, Arthur Braat, Maarten Smits, and Hugo de Jong. 2024. "An Evaluation of 90Y Bremsstrahlung SPECT Image Quality in the Presence of 99mTc: A Technical Perspective on Same-Day Radioembolization" Current Oncology 31, no. 12: 7511-7522. https://doi.org/10.3390/curroncol31120554
APA StyleKeane, G., van Rooij, R., Lam, M., Braat, A., Smits, M., & de Jong, H. (2024). An Evaluation of 90Y Bremsstrahlung SPECT Image Quality in the Presence of 99mTc: A Technical Perspective on Same-Day Radioembolization. Current Oncology, 31(12), 7511-7522. https://doi.org/10.3390/curroncol31120554





