Simplifying Serious Illness Communication: Preparing or Deciding
Abstract
1. Case
2. The Problem
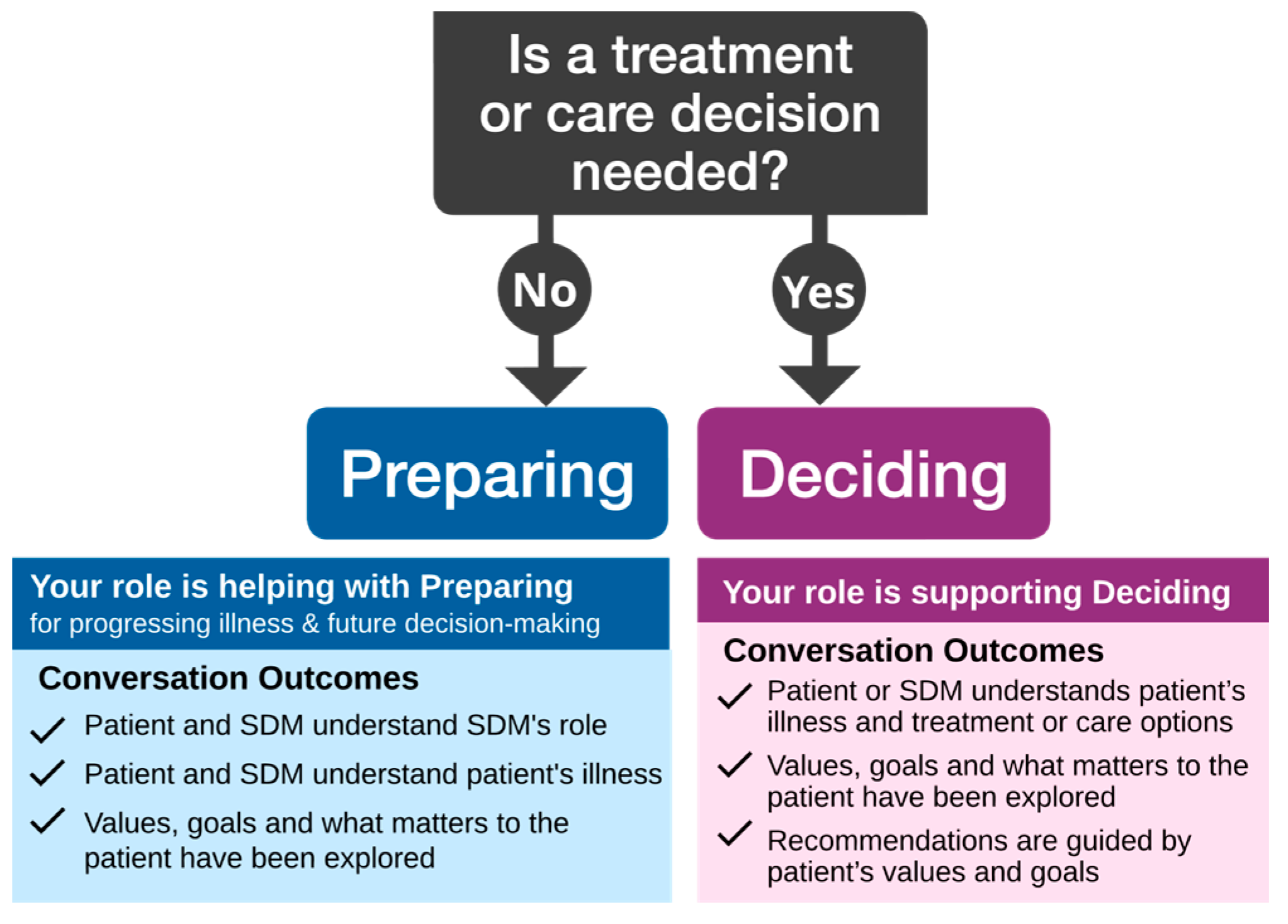
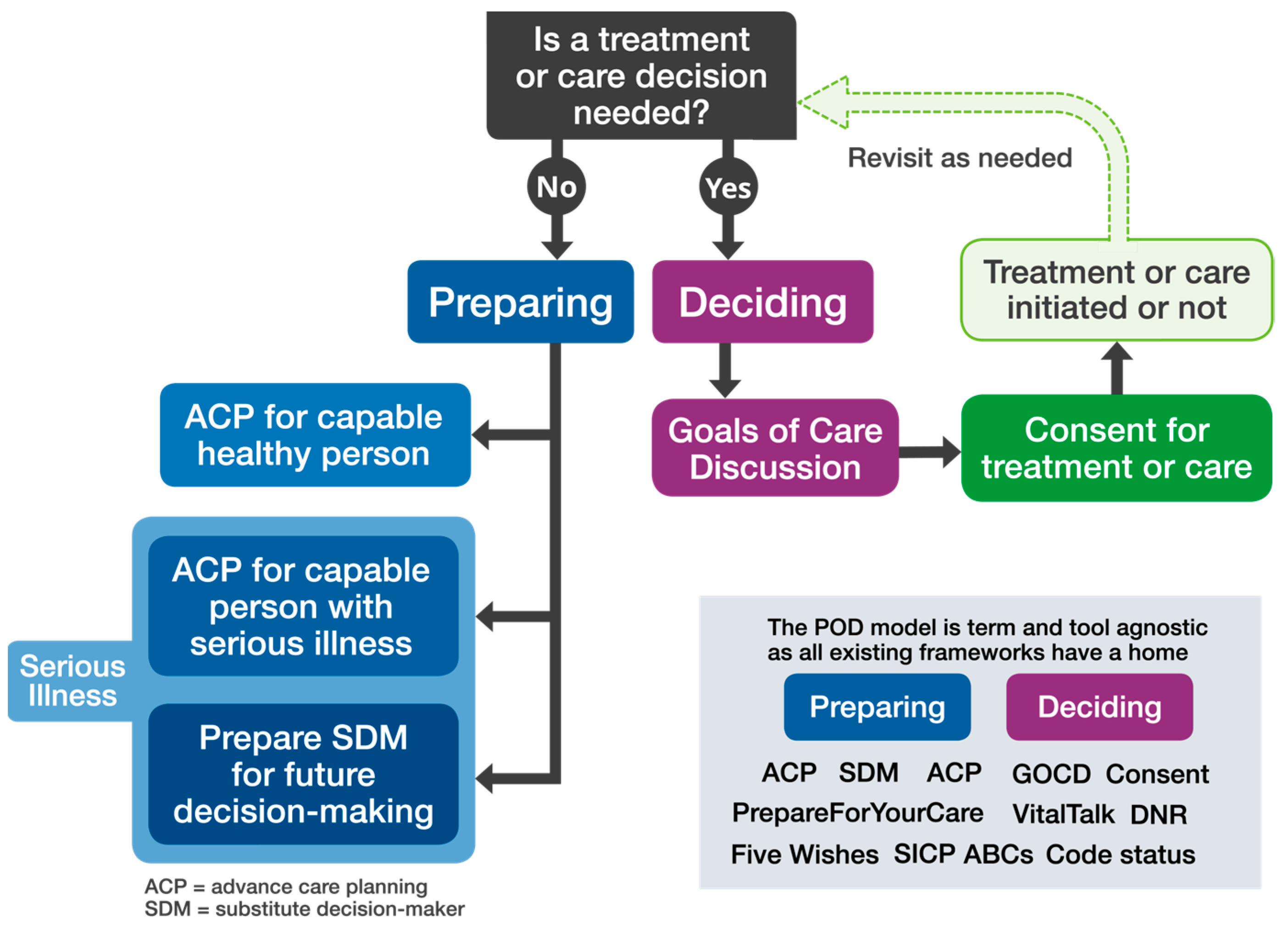
3. A Solution—The Preparing or Deciding (POD) Model
4. What Is Involved with Preparing?
5. What Is Involved with Deciding?
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Detering, K.M.; Hancock, A.D.; Reade, M.C.; Silvester, W. The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ 2010, 340, c1345. [Google Scholar] [CrossRef] [PubMed]
- Bernacki, R.; Paladino, J.; Neville, B.A.; Hutchings, M.; Kavanagh, J.; Geerse, O.P.; Lakin, J.; Sanders, J.J.; Miller, K.; Lipsitz, S.; et al. Effect of the Serious Illness Care Program in Outpatient Oncology: A Cluster Randomized Clinical Trial. JAMA Intern. Med. 2019, 179, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.; Kim, G.L.; Bytautas, J.; Webster, F. Differing conceptualizations of the goals of care discussion: A critical discourse analysis. J. Pain Symptom Manag. 2022, 63, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Morrison, R.S.; Meier, D.E.; Arnold, R.M. What’s Wrong with Advance Care Planning? JAMA 2021, 326, 1575–1576. [Google Scholar] [CrossRef] [PubMed]
- Periyakoil, V.S.; von Gunten, C.F.; Arnold, R.; Hickman, S.; Morrison, R.S.; Sudore, R. Caught in a loop with advance care planning and advance directives: How to move forward? J. Palliat. Med. 2022, 25, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Sudore, R.L.; Lum, H.D.; You, J.J.; Hanson, L.C.; Meier, D.E.; Pantilat, S.Z.; Matlock, D.D.; Rietjens, J.; Korfage, I.J.; Ritchie, C.S.; et al. Defining Advance Care Planning for Adults: A Consensus Definition from a Multidisciplinary Delphi Panel. J. Pain Symptom Manag. 2017, 53, 821–832. [Google Scholar] [CrossRef] [PubMed]
- You, J.J.; Fowler, R.A.; Heyland, D.K. Just ask: Discussing goals of care with patients in hospital with serious illness. CMAJ 2014, 186, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.J.; Paladino, J.; Reaves, E.; Luetke-Stahlman, H.; Price, R.A.; Lorenz, K.; Hanson, L.C.; Curtis, J.R.; Meier, D.E.; Fromme, E.K.; et al. Quality Measurement of Serious Illness Communication: Recommendations for Health Systems Based on Findings from a Symposium of National Experts. J Palliat. Med. 2020, 23, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Weiner, L.; Zadeh, S.; Battles, H.; Baird, K.; Ballard, E.; Osherow, J.; Pao, M. Allowing adolescents and young adults to plan their end-of-life care. Pediatrics 2012, 130, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Freytag, J.; Street, R.L.; Barnes, D.E.; Shi, Y.; Volow, A.M.; Shim, J.K.; Alexander, S.C.; Sudore, R.L. Empowering Older Adults to Discuss Advance Care Planning During Clinical Visits: The PREPARE Randomized Trial. J. Am. Geriatr. Soc. 2020, 68, 1210–1217. [Google Scholar] [CrossRef] [PubMed]
- Back, A.L.; Arnold, R.; Baile, W.; Fryer-Edwards, K.; Alexander, S.; Barley, G.; Gooley, T.; Tulsky, J. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch. Intern. Med. 2007, 167, 453–460. [Google Scholar] [CrossRef]
- Jimenez, G.; Tan, W.S.; Virk, A.K.; Low, C.K.; Car, J.; Ho, A.H. Overview of Systematic Reviews of Advance Care Planning: Summary of Evidence and Global Lessons. J. Pain Symptom Manag. 2018, 56, 436–459. [Google Scholar] [CrossRef] [PubMed]
- Weeks, J.C.; Catalano, P.J.; Cronin, A.; Finkelman, M.D.; Mack, J.W.; Keating, N.L.; Schrag, D. Patients’ Expectations about Effects of Chemotherapy for Advanced Cancer. NEJM 2012, 367, 1616–1625. [Google Scholar] [CrossRef] [PubMed]
- O’Hare, A.M.; Kurella Tamura, M.; Lavallee, D.C.; Vig, E.K.; Taylor, J.S.; Hall, Y.N.; Katz, R.; Curtis, R.C. Assessment of Self-reported Prognostic Expectations of People Undergoing Dialysis: United States Renal Data System Study of Treatment Preferences (USTATE). JAMA Intern. Med. 2019, 179, 1325–1333. [Google Scholar] [CrossRef]
- Ozdemir, S.; Lee, J.J.; Malhotra, C.; Teo, I.; Yeo, K.K.; Than, A.; Sim, K.L.; Finkelstein, E. Associations between prognostic awareness, acceptance of illness, and psychological and spiritual well-being among patients with heart failure. J. Card. Fail. 2022, 28, 736–743. [Google Scholar] [CrossRef] [PubMed]
- Paladino, J.; Lakin, J.R.; Sanders, J.J. Communication Strategies for Sharing Prognostic Information with Patients: Beyond Survival Statistics. JAMA 2019, 322, 1345–1346. [Google Scholar] [CrossRef] [PubMed]
- Norton, S.A.; Metzger, M.; Deluca, J.; Alexander, S.C.; Quill, T.E.; Gramling, R. Palliative care communication: Linking patients’ prognoses, values, and goals of care. Res. Nurs. Health 2013, 36, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Scheunemann, L.P.; Ernecoff, N.C.; Buddadhumaruk, P.; Carson, S.S.; Hough, C.L.; Curtis, J.R.; Anderson, W.G.; Steingrub, J.; Lo, B.; Matthay, M.; et al. Clinician-Family Communication about Patients’ Values and Preferences in Intensive Care Units. JAMA Intern. Med. 2019, 179, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Barry, M.J.; Edgman-Levitan, S. Shared Decision Making-The Pinnacle of Patient-Centered Care Nothing about me without me. NEJM 2012, 366, 780–781. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.A.; Tark, A.; Estrada, L.V.; Dhingra, L.; Stone, P.W. Timing of goals of care discussions in nursing homes: A systematic review. JAMDA 2023, 24, 1820–1830. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myers, J.; Steinberg, L.; Incardona, N.; Simon, J.; Sanders, J.; Seow, H. Simplifying Serious Illness Communication: Preparing or Deciding. Curr. Oncol. 2024, 31, 5832-5837. https://doi.org/10.3390/curroncol31100433
Myers J, Steinberg L, Incardona N, Simon J, Sanders J, Seow H. Simplifying Serious Illness Communication: Preparing or Deciding. Current Oncology. 2024; 31(10):5832-5837. https://doi.org/10.3390/curroncol31100433
Chicago/Turabian StyleMyers, Jeff, Leah Steinberg, Nadia Incardona, Jessica Simon, Justin Sanders, and Hsien Seow. 2024. "Simplifying Serious Illness Communication: Preparing or Deciding" Current Oncology 31, no. 10: 5832-5837. https://doi.org/10.3390/curroncol31100433
APA StyleMyers, J., Steinberg, L., Incardona, N., Simon, J., Sanders, J., & Seow, H. (2024). Simplifying Serious Illness Communication: Preparing or Deciding. Current Oncology, 31(10), 5832-5837. https://doi.org/10.3390/curroncol31100433




