Cancer Care Team Functioning during COVID-19: A Narrative Literature Review and Synthesis
Abstract
1. Introduction
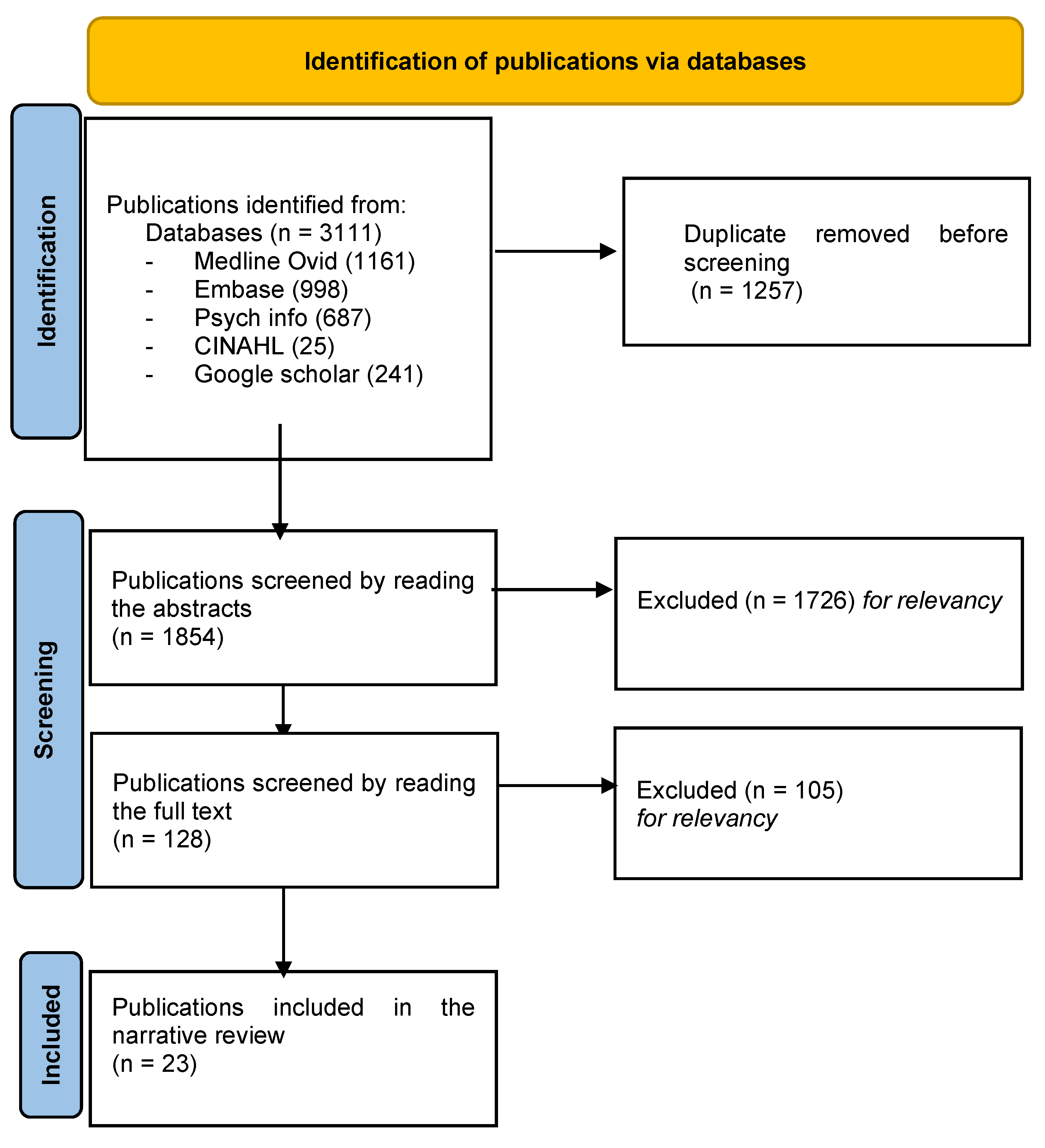
2. Methods
2.1. Sources of Information
2.2. Search Terms and Years
2.3. Publication Selection Criteria
2.4. Data Synthesis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shao, J.; Rodrigues, M.; Corter, A.L.; Baxter, N.N. Multidisciplinary care of breast cancer patients: A scoping review of multidisciplinary styles, processes, and outcomes. Curr. Oncol. 2019, 26, e385–e397. [Google Scholar] [CrossRef] [PubMed]
- Pickard, T.; Williams, S.; Tetzlaff, E.; Petraitis, C.; Hylton, H. Team-Based Care in Oncology: The Impact of the Advanced Practice Provider. Am. Soc. Clin. Oncol. Educ. Book 2023, 43, e390572. [Google Scholar] [CrossRef] [PubMed]
- Takvorian, S.U.; Balogh, E.; Nass, S.; Valentin, V.L.; Hoffman-Hogg, L.; Oyer, R.A.; Carlson, R.W.; Meropol, N.J.; Sheldon, L.K.; Shulman, L.N. Developing and sustaining an effective and resilient oncology careforce: Opportunities for action. J. Natl. Cancer Inst. 2019, 112, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Riera, R.; Bagattini, Â.M.; Pacheco, R.L.; Pachito, D.V.; Roitberg, F.; Ilbawi, A. Delays and disruptions in cancer health care due to COVID-19 pandemic: Systematic review. JCO Glob. Oncol. 2021, 7, 311–323. [Google Scholar] [CrossRef] [PubMed]
- Doshi, P. The elusive definition of pandemic influenza. Bull. World Health Organ. 2011, 89, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Hlubocky, F.J.; Symington, B.E.; McFarland, D.C.; Gallagher, C.M.; Dragnev, K.H.; Burke, J.M.; Lee, R.T.; El-Jawahri, A.; Popp, B.; Rosenberg, A.R.; et al. Impact of the COVID-19 Pandemic on Oncologist Burnout, Emotional Well-Being, and Moral Distress: Considerations for the Cancer Organization’s Response for Readiness, Mitigation, and Resilience. JCO Oncol. Pract. 2021, 17, 365–374. [Google Scholar] [CrossRef]
- Tannenbaum, S.I.; Traylor, A.M.; Thomas, E.J.; Salas, E. Managing teamwork in the face of pandemic: Evidence-based tips. BMJ Qual Saf. 2021, 30, 59–63. [Google Scholar] [CrossRef]
- Salas, E.; Frush, K. Improving Patient Safety through Teamwork and Team Training; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Salas, E.; Shuffler, M.L.; Thayer, A.L.; Bedwell, W.L.; Lazzara, E.H. Understanding and improving teamwork in organizations: A scientifically based practical guide. Hum. Resour. Manag. 2015, 54, 599–622. [Google Scholar] [CrossRef]
- McGuier, E.A.; Kolko, D.J.; Klem, M.L.; Feldman, J.; Kinkler, G.; Diabes, M.A.; Weingart, L.R.; Wolk, C.B. Team functioning and implementation of innovations in healthcare and human service settings: A systematic review protocol. Syst. Rev. 2021, 10, 189. [Google Scholar] [CrossRef]
- Kilpatrick, K.; Paquette, L.; Bird, M.; Jabbour, M.; Carter, N.; Tchouaket, É. Team functioning and beliefs about team effectiveness in inter-professional teams: Questionnaire development and validation. J. Multidiscip. Healthc. 2019, 12, 827–839. [Google Scholar] [CrossRef]
- Gittell, J.H. Relational coordination: Coordinating work through relationships of shared goals, shared knowledge and mutual respect. In Relational Perspectives in Organizational Studies: A Research Companion; Edward Elgar Publishing: Camberley, UK, 2006; pp. 74–94. [Google Scholar]
- Gittell, J.H.; Fairfield, K.M.; Bierbaum, B.; Head, W.; Jackson, R.; Kelly, M.; Laskin, R.; Lipson, S.; Siliski, J.; Thornhill, T.; et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: A nine-hospital study of surgical patients. Med. Care 2000, 38, 807–819. [Google Scholar] [CrossRef] [PubMed]
- Taplin, S.H.; Weaver, S.; Salas, E.; Chollette, V.; Edwards, H.M.; Bruinooge, S.S.; Kosty, M.P. Reviewing cancer care team effectiveness. J. Oncol. Pract. 2015, 11, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Azar, J.M.; Johnson, C.S.; Frame, A.M.; Perkins, S.M.; Cottingham, A.H.; Litzelman, D.K. Evaluation of interprofessional relational coordination and patients’ perception of care in outpatient oncology teams. J. Interprof. Care 2017, 31, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Sataloff, R.T.; Bush, M.L.; Chandra, R.; Chepeha, D.; Rotenberg, B.; Fisher, E.W.; Goldenberg, D.; Hanna, E.Y.; Kerschner, J.E.; Kraus, D.H. Systematic and other reviews: Criteria and complexities. Ann. Otol. Rhinol. Laryngol. 2021, 130, 649–652. [Google Scholar] [CrossRef] [PubMed]
- Green, B.N.; Johnson, C.D.; Adams, A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J. Chiropr. Med. 2006, 5, 101–117. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Banerjee, S.; Lim, K.H.J.; Murali, K.; Kamposioras, K.; Punie, K.; Oing, C.; O’Connor, M.; Thorne, E.; Devnani, B.; Lambertini, M.; et al. The impact of COVID-19 on oncology professionals: Results of the ESMO Resilience Task Force survey collaboration. Esmo Open 2021, 6, 100058. [Google Scholar] [CrossRef]
- Mohamedbhai, H.; Fernando, S.; Ubhi, H.; Chana, S.; Visavadia, B. Advent of the virtual multidisciplinary team meeting: Do remote meetings work? Br. J. Oral Maxillofac. Surg. 2021, 59, 1248–1252. [Google Scholar] [CrossRef]
- Turner, K.; Bobonis Babilonia, M.; Naso, C.; Nguyen, O.; Gonzalez, B.D.; Oswald, L.B.; Robinson, E.; Elston Lafata, J.; Ferguson, R.J.; Alishahi Tabriz, A. Health care providers’ and professionals’ experiences with telehealth oncology implementation during the COVID-19 pandemic: A qualitative study. J. Med. Internet Res. 2022, 24, e29635. [Google Scholar] [CrossRef]
- Marshall, V.K.; Mason, T.M.; Chavez, M.; Martinez-Tyson, D.; Bugajski, A. Impact of COVID-19 on Oncology Healthcare Providers: The Resilience of a Profession. Cancer Nurs. 2022, 45, E407–E416. [Google Scholar] [CrossRef]
- Perlmutter, B.; Said, S.A.; Hossain, M.S.; Simon, R.; Joyce, D.; Walsh, R.M.; Augustin, T. Lessons learned and keys to success: Provider experiences during the implementation of virtual oncology tumor boards in the era of COVID-19. J. Surg. Oncol. 2022, 125, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Standiford, T.C.; Davuluri, K.; Trupiano, N.; Portney, D.; Gruppen, L.; Vinson, A.H. Physician leadership during the COVID-19 pandemic: An emphasis on the team, well-being and leadership reasoning. BMJ Leader 2021, 5, 20–25. [Google Scholar] [CrossRef]
- Paterson, C.; Bacon, R.; Dwyer, R.; Morrison, K.S.; Toohey, K.; O’Dea, A.; Slade, J.; Mortazavi, R.; Roberts, C.; Pranavan, G. The role of telehealth during the COVID-19 pandemic across the interdisciplinary cancer team: Implications for practice. Semin Oncol Nurs. 2020, 36, 151090. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, D.; Touati, N.; Kilpatrick, K.; Durand, M.J.; Turcotte, A.; Prady, C.; Poder, T.G.; Richard, P.O.; Soldera, S.; Berbiche, D.; et al. Building resilience in oncology teams: Protocol for a realist evaluation of multiple cases. PLoS ONE 2022, 17, e0268393. [Google Scholar] [CrossRef] [PubMed]
- Chênevert, D.; Brown, T.L.; Pomey, M.-P.; Benomar, N.; Colombat, P.; Fouquereau, E.; Loiselle, C.G. Investigating a Participatory Intervention in Multidisciplinary Cancer Care Teams Using an Integrative Organizational Model: A Study Protocol. Front. Psychol. 2022, 13, 798863. [Google Scholar] [CrossRef] [PubMed]
- Boparai, S.; Carrigg, J.; Holland, C.; Kennedy, C.; Nguyen, F.; Pham, T.; Sozer, B. Oncology social workers’ responses to and reflections on COVID-19. Aust. Social Work 2021, 74, 127–128. [Google Scholar] [CrossRef]
- Anderson, N.; Thompson, K.; Andrews, J.; Chesson, B.; Cray, A.; Phillips, D.; Ryan, M.; Soteriou, S.; Trainor, G.; Touma, N. Planning for a pandemic: Mitigating risk to radiation therapy service delivery in the COVID-19 era. J. Med. Radiat. Sci. 2020, 67, 243–248. [Google Scholar] [CrossRef]
- Besson, J.; McNamara, C.; Brown, E. Pivots and pirouettes: Adapting a robust departmental CPD and training program to the COVID-19 crisis. J. Med. Radiat. Sci. 2020, 67, 356–359. [Google Scholar] [CrossRef]
- Farah, E.; El Bizri, M.; Day, R.; Matai, L.; Horne, F.; Hanna, T.P.; Armstrong, D.; Marlin, S.; Jerome, O.; Brenner, D.R.; et al. Report from the Ready for the Next Round Thought-Leadership Roundtables on Building Resilience in Cancer Care and Control in Canada-Colorectal Cancer Canada; 2021. Curr. Oncol. 2022, 29, 1723–1743. [Google Scholar] [CrossRef]
- Shah, M.A.; Emlen, M.F.; Shore, T.; Mayer, S.; Leonard, J.P.; Rossi, A.; Martin, P.; Ritchie, E.; Niesvizky, R.; Pastore, R.; et al. Hematology and oncology clinical care during the coronavirus disease 2019 pandemic. CA Cancer J. Clin. 2020, 70, 349–354. [Google Scholar] [CrossRef]
- Davies, C.; Campbell, S.; Hutton, J.; Morgan, A.; Cherry, M.G. A summary of the rapid services changes made in response to staff psychological needs and maintaining care to those with cancer in light of COVID-19. Psycho-Oncology 2020, 29, 1393. [Google Scholar] [CrossRef] [PubMed]
- Soukup, T.; Sevdalis, N.; Green, J.S.; Lamb, B.W. Quality improvement for cancer multidisciplinary teams: Lessons learned from the Anglian Germ Cell Cancer Collaborative Group. Br. J. Cancer 2021, 124, 313–314. [Google Scholar] [CrossRef] [PubMed]
- Ngoi, N.; Lim, J.; Ow, S.; Jen, W.Y.; Lee, M.; Teo, W.; Ho, J.; Sundar, R.; Tung, M.; Lee, Y.; et al. A segregated-team model to maintain cancer care during the COVID-19 outbreak at an academic center in Singapore. Ann. Oncol. 2020, 31, 840–843. [Google Scholar]
- Ueda, M.; Martins, R.; Hendrie, P.C.; McDonnell, T.; Crews, J.R.; Wong, T.L.; McCreery, B.; Jagels, B.; Crane, A.; Byrd, D.R.; et al. Managing Cancer Care during the COVID-19 Pandemic: Agility and Collaboration Toward a Common Goal. J. Natl. Compr. Canc. Netw. 2020, 18, 366–369. [Google Scholar] [CrossRef] [PubMed]
- Le Tallec, P.; Gesbert, C.; Mercier, C.; Crenn, E. Ethical competence of the radiation therapist in the management of a crisis. Cancer Radiother. 2022, 26, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Jazieh, A.R.; Chan, S.L.; Curigliano, G.; Dickson, N.; Eaton, V.; Garcia-Foncillas, J.; Gilmore, T.; Horn, L.; Kerr, D.J.; Lee, J.; et al. Delivering Cancer Care During the COVID-19 Pandemic: Recommendations and Lessons Learned From ASCO Global Webinars. JCO Glob. Oncol. 2020, 6, 1461–1471. [Google Scholar] [CrossRef] [PubMed]
- Rosa, W.E.; Roberts, K.E.; Schlak, A.E.; Applebaum, A.J.; Breitbart, W.S.; Kantoff, E.H.; Pessin, H.; Lichtenthal, W.G. The Critical Need for a Meaning-Centered Team-Level Intervention to Address Healthcare Provider Distress Now. Int. J. Environ. Res. Public Health 2022, 19, 7801. [Google Scholar] [CrossRef]
- Reynolds, K.L.; Klempner, S.J.; Parikh, A.; Hochberg, E.P.; Michaelson, M.D.; Mooradian, M.J.; Lee, R.J.; Soumerai, T.E.; Hobbs, G.; Piotrowska, Z.; et al. The Art of Oncology: COVID-19 Era. Oncologist 2020, 25, 997–1000g. [Google Scholar] [CrossRef]
- Bansal, G.J.; Chopra, S. Symptomatic breast services in the post-COVID-19 era. Br. J. Hosp. Med. 2021, 82, 1–3. [Google Scholar] [CrossRef]
- Baker, A. Crossing the quality chasm: A new health system for the 21st century. BMJ 2001, 323, 1192. [Google Scholar] [CrossRef]
- Knebel, E.; Greiner, A.C. Health Professions Education: A Bridge to Quality; National Academies Press: Washington, DC, USA, 2003. [Google Scholar]
- Baker, D.P.; Gustafson, S.; Beaubien, J.M. Medical Team Training Programs. Adv. Patient Saf. Res. Implement. 2005, 4, 253. [Google Scholar]
- Busari, J.O.; Moll, F.M.; Duits, A.J. Understanding the impact of interprofessional collaboration on the quality of care: A case report from a small-scale resource limited health care environment. J. Multidiscip. Healthc. 2017, 10, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Nazir, A. Healthcare leadership lessons from COVID-19. J. Am. Geriatr. Soc. 2021, 69, 2793–2794. [Google Scholar] [CrossRef] [PubMed]
- Marlow, S.L.; Lacerenza, C.N.; Salas, E. Communication in virtual teams: A conceptual framework and research agenda. Hum. Resour. Manag. Rev. 2017, 27, 575–589. [Google Scholar] [CrossRef]
- Rajasekaran, R.B.; Whitwell, D.; Cosker, T.D.; Gibbons, C.L.; Carr, A. Will virtual multidisciplinary team meetings become the norm for musculoskeletal oncology care following the COVID-19 pandemic?-experience from a tertiary sarcoma centre. BMC Musculoskelet. Disord. 2021, 22, 18. [Google Scholar] [CrossRef]
- Paul, R.; Drake, J.R.; Liang, H. Global virtual team performance: The effect of coordination effectiveness, trust, and team cohesion. IEEE Trans. Prof. Commun. 2016, 59, 186–202. [Google Scholar] [CrossRef]
- Blandford, A.; Wesson, J.; Amalberti, R.; AlHazme, R.; Allwihan, R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob. Health 2020, 8, e1364–e1365. [Google Scholar] [CrossRef]
- Kanavos, P.; Vogelsang, M.; Haig, M.; Kolovou, V. Challenges for health systems seeking to embrace virtual health care for population health. Eur. J. Health Econ. 2022, 23, 1079–1083. [Google Scholar] [CrossRef]
- Alliger, G.M.; Cerasoli, C.P.; Tannenbaum, S.I.; Vessey, W.B. Team resilience: How teams flourish under pressure. Organ. Dyn. 2015, 44, 176–184. [Google Scholar] [CrossRef]
- Hendrikx, I.E.; Vermeulen, S.C.; Wientjens, V.L.; Mannak, R.S. Is Team Resilience More Than the Sum of Its Parts? A Quantitative Study on Emergency Healthcare Teams during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2022, 19, 6968. [Google Scholar] [CrossRef]
- Hartwig, A.; Clarke, S.; Johnson, S.; Willis, S. Workplace team resilience: A systematic review and conceptual development. Organ. Psychol. Rev. 2020, 10, 169–200. [Google Scholar] [CrossRef]
- Mills, J.; Ramachenderan, J.; Chapman, M.; Greenland, R.; Agar, M. Prioritising workforce wellbeing and resilience: What COVID-19 is reminding us about self-care and staff support. Palliat. Med. 2020, 34, 1137–1139. [Google Scholar] [CrossRef] [PubMed]
- Burki, T.K. Burnout among cancer professionals during COVID-19. Lancet Oncol. 2020, 21, 1402. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef] [PubMed]
- McEwen, K.; Boyd, C.M. A measure of team resilience: Developing the resilience at work team scale. J. Occup. Environ. Med. 2018, 60, 258–272. [Google Scholar] [CrossRef]
- Rieckert, A.; Schuit, E.; Bleijenberg, N.; Ten Cate, D.; de Lange, W.; de Man-van Ginkel, J.M.; Mathijssen, E.; Smit, L.C.; Stalpers, D.; Schoonhoven, L. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open 2021, 11, e043718. [Google Scholar] [CrossRef]
- Gasper, H.; Ahern, E.; Roberts, N.; Chan, B.; Lwin, Z.; Collective, M.C.C.C.Q.R. COVID-19 and the cancer care workforce: From doctors to ancillary staff. Semin. Oncol. 2020, 47, 309–311. [Google Scholar] [CrossRef]
- Hlubocky, F.J. Attending to oncology team well-being. JCO Oncol. Pract. 2022, 18, 541–542. [Google Scholar] [CrossRef]
| Author/Year | Type | Objective(s) | Participants |
|---|---|---|---|
| Banerjee et al., 2021 [19] | Original | To investigate wellbeing, burnout, and job performance in oncology over time since COVID-19 | N = 1520 oncology professionals |
| Mohamedbhai et al., 2021 [20] | Original | To evaluate the effects of virtual head-and-neck multidisciplinary team meetings on the functioning of the team | N = 97 head-and-neck cancer team members (i.e., oncologists, nurses, pathologists, radiologists, dieticians, speech and language therapists) |
| Turner et al., 2022 [21] | Original | To explore oncology healthcare professionals’ experiences with the implementation of telehealth during the COVID-19 pandemic | N = 40 healthcare professionals in oncology (physicians, advanced practice providers, social workers, psychologists, dieticians, pharmacists) |
| Marshall et al., 2022 [22] | Original | To explore the impact of COVID-19 on oncology healthcare professionals | N = 30 (registered and advanced practice nurses, oncologists, pharmacists, mental health counselors, genetic counselors) |
| Perlmutter et al., 2022 [23] | Original | To identify key contributors to success and common pitfalls associated with virtual multidisciplinary meetings | N = 253 (surgeons, nurses, advanced practice providers, residents, fellows) |
| Hlubocky et al., 2021 [6] | Original | To describe the occupational and personal consequences of the COVID-19 pandemic on oncologists’ wellbeing and patient care | N = 25 oncologists |
| Standiford, 2020 [24] | Original | To explore the attributes and techniques that are important to effectively lead teams during a crisis | N= 16 physicians |
| Paterson et al., 2020 [25] | Literature review | To explore the role of telehealth during the COVID-19 pandemic across the interdisciplinary cancer care team | N/A |
| Tremblay et al., 2022 [26] | Protocol | To better understand how a multicomponent intervention builds resilience in oncology teams | |
| Chenevert et al., 2022 [27] | Protocol | To evaluate a participatory interventional approach that fosters team resilience and determine whether enhanced resilience improves teams’ mental health status and organizational outcomes | |
| Boparai et al., 2021 [28] | Special/knowledge exchange article | To discuss how oncology social workers in Australia adapted to the challenges of providing support to patients with cancer during the COVID-19 pandemic | Social workers |
| Anderson et al., 2020 [29] | Special/commentary | To describe the experiences of a cancer center with radiation therapy services during initial stages of the COVID-19 pandemic | N/A |
| Besson et al., 2020 [30] | Special/commentary | To examine the rationale for and methods of adapting a robust continuing professional development program and training for radiation therapists | N/A |
| Farah et al., 2021 [31] | Special/report | To identify stakeholders’ views on strategies to build healthcare resilience for future health threats | Patients, oncologists, researchers, and healthcare system representatives |
| Shah et al., 2020 [32] | Special/report | To highlight the transformation undertaken in a busy oncology care department to prepare for the COVID-19 crisis | N/A |
| Davies et al., 2020 [33] | Special/clinical correspondence | To discuss measures in place to support oncology staff throughout the COVID-19 pandemic | Oncology team members |
| Soukup et al., 2021 [34] | Special/editorial piece | To present lessons learned from a collaborative cancer group during COVID-19 | N/A |
| Ngoi et al., 2020 [35] | Special/editorial piece | To present a segregated team model to maintain cancer care during COVID-19 | N/A |
| Ueda et al., 2020 [36] | Special/special feature | To highlight the importance of organizational structure, preparation, agility, and a shared vision amidst the global pandemic | N/A |
| Tallec et al., 2022 [37] | Special/brief communication | To highlight teams’ and radiation therapists’ needs in the event of crisis | N/A |
| Jazieh et al., 2020 [38] | Special article | To present recommendations that may improve our understanding of COVID-19′s effects on cancer care and increase readiness to manage future outbreaks effectively | N/A |
| Rosa et al., 2022 [39] | Special/essay | To describe principles underlying a meaning-centered team-level intervention to reduce burnout among health care professionals during a health crisis | N/A |
| Reynolds et al., 2020 [40] | Special/perspectives | To describe teamwork and resilience in a hematology/oncology department treating patients with COVID-19 | Oncology team members |
| Author/Year | Theme 1: Swiftly Adopting Virtual Technology for Communication and Interprofessional Collaboration |
|---|---|
| Mohamedbhai et al., 2021 [20] |
|
| Turner et al., 2022 [21] |
|
| Perlmutter et al., 2022 [23] |
|
| Standiford, 2020 [41] |
|
| Paterson et al., 2020 [25] |
|
| Boparai et al., 2021 [28] |
|
| Anderson et al., 2020 [29] |
|
| Farah et al., 2021 [31] |
|
| Shah et al., 2020 [32] |
|
| Soukup et al., 2021 [34] |
|
| Ngoi et al., 2020 [35] |
|
| Ueda et al., 2020 [36] |
|
| Jazieh et al., 2020 [38] |
|
| Reynolds et al., 2020 [40] |
|
| Author/Year | Theme 2: Promoting Team Resilience |
|---|---|
| Banerjee et al., 2021 [19] |
|
| Marshall et al., 2022 [22] |
|
| Tremblay et al., 2022 [26] |
|
| Chenevert et al., 2022 [27] |
|
| Besson et al., 2020 [30] |
|
| Farah et al., 2021 [31] |
|
| Le Tallec et al., 2022 [37] |
|
| Hlubocky et al., 2021 [6] |
|
| Author/Year | Theme 3: Encouraging Self-Care and Optimizing Team Support |
|---|---|
| Banerjee et al., 2021 [19] |
|
| Marshall et al., 2022 [22] |
|
| Boparai et al., 2021 [28] |
|
| Anderson et al., 2020 [29] |
|
| Farah et al., 2021 [31] |
|
| Davies et al., 2020 [33] |
|
| Ngoi et al., 2020 [35] |
|
| Ueda et al., 2020 [36] |
|
| Rosa et al., 2022 [39] |
|
| Hlubocky et al., 2021 [6] |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Attieh, S.; Loiselle, C.G. Cancer Care Team Functioning during COVID-19: A Narrative Literature Review and Synthesis. Curr. Oncol. 2024, 31, 335-349. https://doi.org/10.3390/curroncol31010022
Attieh S, Loiselle CG. Cancer Care Team Functioning during COVID-19: A Narrative Literature Review and Synthesis. Current Oncology. 2024; 31(1):335-349. https://doi.org/10.3390/curroncol31010022
Chicago/Turabian StyleAttieh, Samar, and Carmen G. Loiselle. 2024. "Cancer Care Team Functioning during COVID-19: A Narrative Literature Review and Synthesis" Current Oncology 31, no. 1: 335-349. https://doi.org/10.3390/curroncol31010022
APA StyleAttieh, S., & Loiselle, C. G. (2024). Cancer Care Team Functioning during COVID-19: A Narrative Literature Review and Synthesis. Current Oncology, 31(1), 335-349. https://doi.org/10.3390/curroncol31010022






