Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Outcome, Inclusion Criteria, and Exclusion Criteria
2.2. Search Strategy
2.3. Study Selection and Data Extraction
2.4. Methodological Quality and the Risk of Bias Assessment
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Included Studies
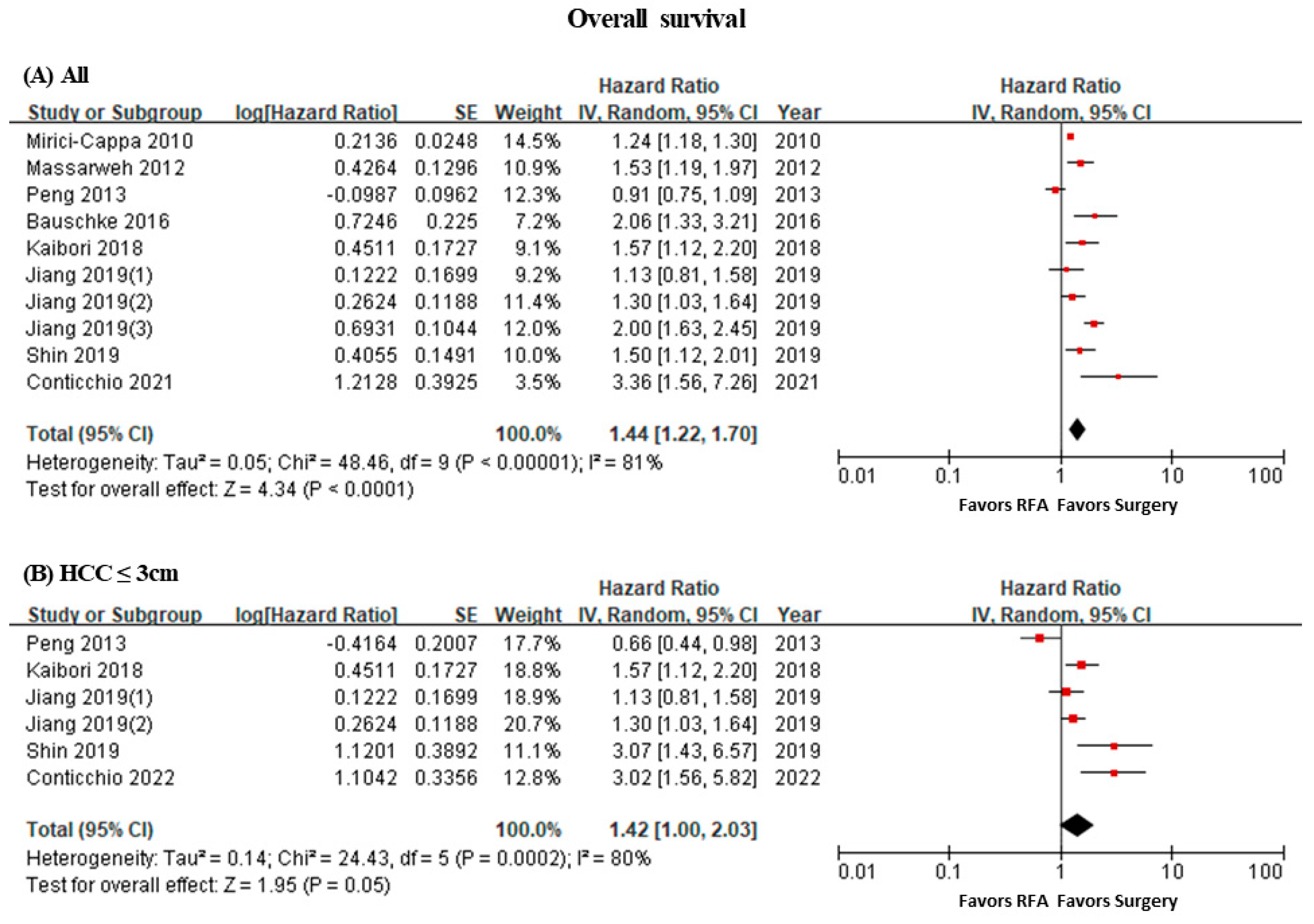
3.2. Overall Survival
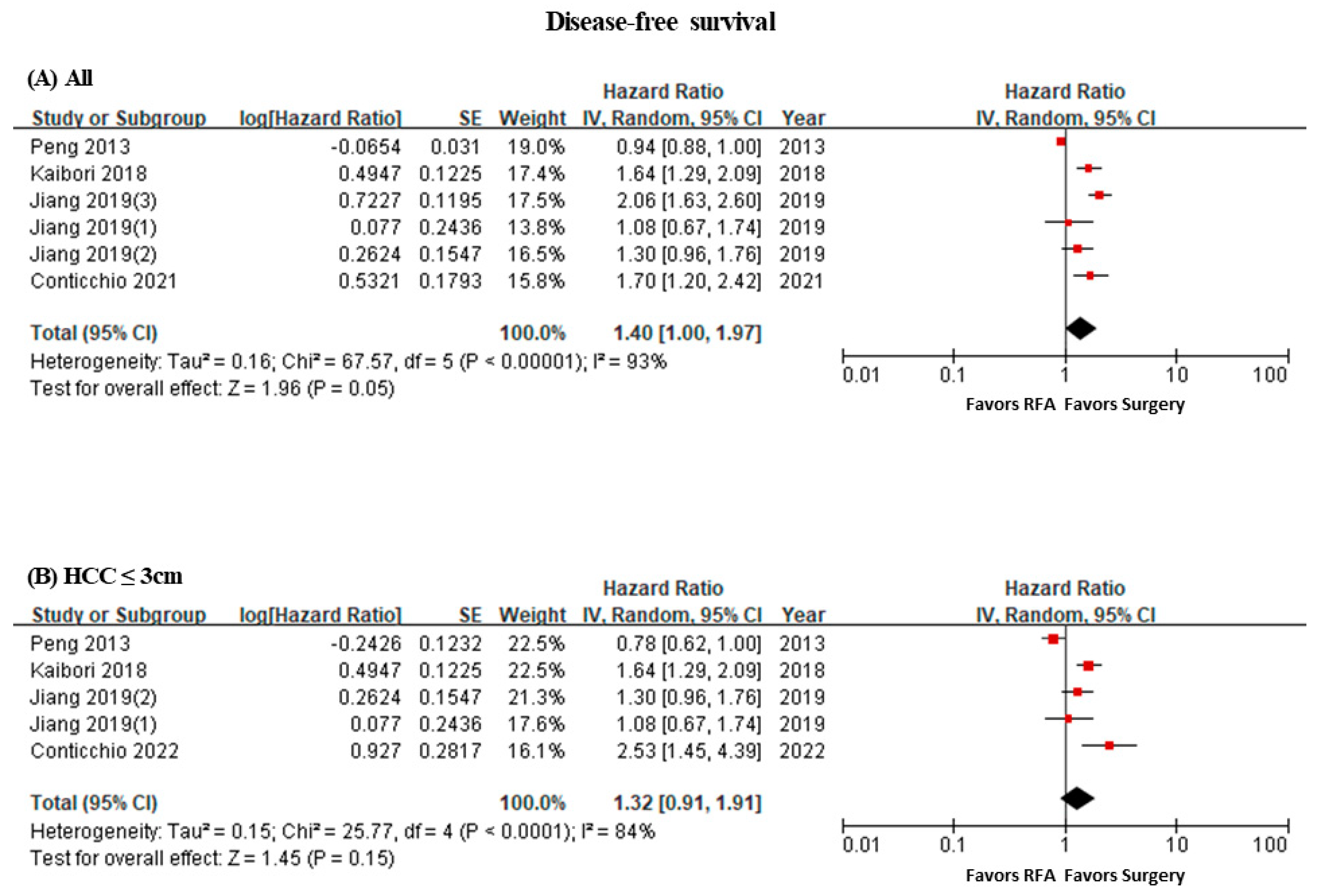
3.3. Disease-Free Survival
3.4. Recurrence
3.5. Short-Term Mortality
3.6. Adverse Events
3.7. Length of Hospital Stay
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rumgay, H.; Arnold, M.; Ferlay, J.; Lesi, O.; Cabasag, C.J.; Vignat, J.; Laversanne, M.; McGlynn, K.A.; Soerjomataram, I. Global burden of primary liver cancer in 2020 and predictions to 2040. J. Hepatol. 2022, 77, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- Chon, Y.E.; Park, S.Y.; Hong, H.P.; Son, D.; Lee, J.; Yoon, E.; Kim, S.S.; Ahn, S.B.; Jeong, S.W.; Jun, D.W. Hepatocellular carcinoma incidence is decreasing in Korea but increasing in the very elderly. Clin. Mol. Hepatol. 2023, 29, 120–134. [Google Scholar] [CrossRef] [PubMed]
- Korean Liver Cancer Association. 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma. J. Liver Cancer 2023, 23, 1126. [Google Scholar] [CrossRef]
- Baquero, G.A.; Rich, M.W. Perioperative care in older adults. J. Geriatr. Cardiol. 2015, 12, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Partridge, J.S.; Harari, D.; Dhesi, J.K. Frailty in the older surgical patient: A review. Age Ageing 2012, 41, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Lee, J.M.; Lee, J.Y.; Kim, S.H.; Yoon, J.H.; Kim, Y.J.; Han, J.K.; Choi, B.I. Radiofrequency ablation of hepatocellular carcinoma as first-line treatment: Long-term results and prognostic factors in 162 patients with cirrhosis. Radiology 2014, 270, 900–909. [Google Scholar] [CrossRef]
- Xu, Q.; Kobayashi, S.; Ye, X.; Meng, X. Comparison of hepatic resection and radiofrequency ablation for small hepatocellular carcinoma: A meta-analysis of 16,103 patients. Sci. Rep. 2014, 4, 7252. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.L.; Liu, X.D.; Liang, M.; Luo, B.M. Radiofrequency Ablation versus Hepatic Resection for Small Hepatocellular Carcinoma: Systematic Review of Randomized Controlled Trials with Meta-Analysis and Trial Sequential Analysis. Radiology 2018, 287, 461–472. [Google Scholar] [CrossRef]
- Federico, P.; Giunta, E.F.; Pappalardo, A.; Tufo, A.; Marte, G.; Attademo, L.; Fabbrocini, A.; Petrillo, A.; Daniele, B. How to Treat Hepatocellular Carcinoma in Elderly Patients. Pharmaceuticals 2021, 14, 233. [Google Scholar] [CrossRef]
- Kim, S.Y.; Park, J.E.; Lee, Y.J.; Seo, H.J.; Sheen, S.S.; Hahn, S.; Jang, B.H.; Son, H.J. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J. Clin. Epidemiol. 2013, 66, 408–414. [Google Scholar] [CrossRef]
- Conticchio, M.; Delvecchio, A.; Ratti, F.; Gelli, M.; Anelli, F.M.; Laurent, A.; Vitali, G.C.; Magistri, P.; Assirati, G.; Felli, E.; et al. Laparoscopic surgery versus radiofrequency ablation for the treatment of single hepatocellular carcinoma </=3 cm in the elderly: A propensity score matching analysis. HPB 2022, 24, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Conticchio, M.; Inchingolo, R.; Delvecchio, A.; Laera, L.; Ratti, F.; Gelli, M.; Anelli, F.; Laurent, A.; Vitali, G.; Magistri, P.; et al. Radiofrequency ablation vs. surgical resection in elderly patients with hepatocellular carcinoma in Milan criteria. World J. Gastroenterol. 2021, 27, 2205–2218. [Google Scholar] [CrossRef] [PubMed]
- Delvecchio, A.; Inchingolo, R.; Laforgia, R.; Ratti, F.; Gelli, M.; Anelli, M.F.; Laurent, A.; Vitali, G.; Magistri, P.; Assirati, G.; et al. Liver resection vs. radiofrequency ablation in single hepatocellular carcinoma of posterosuperior segments in elderly patients. World J. Gastrointest. Surg. 2021, 13, 1696–1707. [Google Scholar] [CrossRef]
- Shin, J.; Yu, J.H.; Jin, Y.J.; Suh, Y.J.; Kim, D.H.; Byun, S.; Lee, J.W. Effective therapeutic options for elderly patients with hepatocellular carcinoma: A nationwide cohort study. Medicine 2019, 98, e16150. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.Q.; Wang, Z.X.; Deng, Y.N.; Yang, Y.; Wang, G.Y.; Chen, G.H. Efficacy of Hepatic Resection vs. Radiofrequency Ablation for Patients With Very-Early-Stage or Early-Stage Hepatocellular Carcinoma: A Population-Based Study With Stratification by Age and Tumor Size. Front. Oncol. 2019, 9, 113. [Google Scholar] [CrossRef]
- Kaibori, M.; Yoshii, K.; Hasegawa, K.; Ogawa, A.; Kubo, S.; Tateishi, R.; Izumi, N.; Kadoya, M.; Kudo, M.; Kumada, T.; et al. Treatment Optimization for Hepatocellular Carcinoma in Elderly Patients in a Japanese Nationwide Cohort. Ann. Surg. 2019, 270, 121–130. [Google Scholar] [CrossRef]
- Harada, N.; Maeda, T.; Yoshizumi, T.; Ikeda, T.; Kayashima, H.; Ikegami, T.; Harimoto, N.; Takaki, S.; Maehara, Y. Laparoscopic Liver Resection Is a Feasible Treatment for Patients with Hepatocellular Carcinoma and Portal Hypertension. Anticancer Res. 2016, 36, 3489–3497. [Google Scholar]
- Bauschke, A.; Altendorf-Hofmann, A.; Mothes, H.; Rauchfuss, F.; Settmacher, U. Partial liver resection results in a significantly better long-term survival than locally ablative procedures even in elderly patients. J. Cancer Res. Clin. Oncol. 2016, 142, 1099–1108. [Google Scholar] [CrossRef]
- Ito, T.; Tanaka, S.; Iwai, S.; Takemura, S.; Hagihara, A.; Uchida-Kobayashi, S.; Shinkawa, H.; Nishioka, T.; Kawada, N.; Kubo, S. Outcomes of laparoscopic hepatic resection versus percutaneous radiofrequency ablation for hepatocellular carcinoma located at the liver surface: A case-control study with propensity score matching. Hepatol. Res. 2016, 46, 565–574. [Google Scholar] [CrossRef]
- Liu, P.H.; Hsu, C.Y.; Lee, Y.H.; Hsia, C.Y.; Huang, Y.H.; Su, C.W.; Chiou, Y.Y.; Lin, H.C.; Huo, T.I. Uncompromised treatment efficacy in elderly patients with hepatocellular carcinoma: A propensity score analysis. Medicine 2014, 93, e264. [Google Scholar] [CrossRef]
- Peng, Z.W.; Liu, F.R.; Ye, S.; Xu, L.; Zhang, Y.J.; Liang, H.H.; Lin, X.J.; Lau, W.Y.; Chen, M.S. Radiofrequency ablation versus open hepatic resection for elderly patients (>65 years) with very early or early hepatocellular carcinoma. Cancer 2013, 119, 3812–3820. [Google Scholar] [CrossRef] [PubMed]
- Massarweh, N.N.; Park, J.O.; Yeung, R.S.; Flum, D.R. Comparative assessment of the safety and effectiveness of radiofrequency ablation among elderly medicare beneficiaries with hepatocellular carcinoma. Ann. Surg. Oncol. 2012, 19, 1058–1065. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mirici-Cappa, F.; Gramenzi, A.; Santi, V.; Zambruni, A.; Di Micoli, A.; Frigerio, M.; Maraldi, F.; Di Nolfo, M.A.; Del Poggio, P.; Benvegnu, L.; et al. Treatments for hepatocellular carcinoma in elderly patients are as effective as in younger patients: A 20-year multicentre experience. Gut 2010, 59, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Feng, K.; Yan, J.; Li, X.; Xia, F.; Ma, K.; Wang, S.; Bie, P.; Dong, J. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J. Hepatol. 2012, 57, 794–802. [Google Scholar] [CrossRef] [PubMed]
- Takayama, T.; Hasegawa, K.; Izumi, N.; Kudo, M.; Shimada, M.; Yamanaka, N.; Inomata, M.; Kaneko, S.; Nakayama, H.; Kawaguchi, Y.; et al. Surgery versus Radiofrequency Ablation for Small Hepatocellular Carcinoma: A Randomized Controlled Trial (SURF Trial). Liver Cancer 2022, 11, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Kim, B.H.; Park, J.W. The emerging age-pattern changes of patients with hepatocellular carcinoma in Korea. Clin. Mol. Hepatol. 2023, 29, 99–101. [Google Scholar] [CrossRef]
- Renne, S.L.; Di Tommaso, L. A clinical and pathological update on hepatocellular carcinoma. J. Liver Cancer 2022, 22, 14–22. [Google Scholar] [CrossRef]
- Lim, M.; Kim, J.M.; Kwon, J.E.; Jeong, E.S.; Yang, J.; Lee, O.; Kim, K.D.; Kim, S.J.; Rhu, J.; Choi, G.S.; et al. Hepatocellular Carcinoma Arising from Hepatocellular Adenoma in an Elderly Male Patient. J. Liver Cancer 2021, 21, 87–91. [Google Scholar] [CrossRef]
- Honda, T.; Miyaaki, H.; Ichikawa, T.; Taura, N.; Miuma, S.; Shibata, H.; Isomoto, H.; Takeshima, F.; Nakao, K. Clinical characteristics of hepatocellular carcinoma in elderly patients. Oncol. Lett. 2011, 2, 851–854. [Google Scholar] [CrossRef]
- Shimada, S.; Kamiyama, T.; Orimo, T.; Nagatsu, A.; Asahi, Y.; Sakamoto, Y.; Kamachi, H.; Taketomi, A. Prognoses, outcomes, and clinicopathological characteristics of very elderly patients with hepatocellular carcinoma who underwent hepatectomy. World J. Surg. Oncol. 2020, 18, 122. [Google Scholar] [CrossRef]
- Kim, Y.S.; Rhim, H.; Lim, H.K.; Choi, D.; Lee, W.J.; Jeon, T.Y.; Joh, J.W.; Kim, S.J. Intraoperative radiofrequency ablation for hepatocellular carcinoma: Long-term results in a large series. Ann. Surg. Oncol. 2008, 15, 1862–1870. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Lokken, R.P.; Mehta, N. Optimal treatment for small HCC (<3 cm): Resection, liver transplantation, or locoregional therapy? JHEP Rep. 2023, 5, 100781. [Google Scholar] [CrossRef]
- Lee, J.; Jin, Y.J.; Shin, S.K.; Kwon, J.H.; Kim, S.G.; Suh, Y.J.; Jeong, Y.; Yu, J.H.; Lee, J.W.; Kwon, O.S.; et al. Surgery versus radiofrequency ablation in patients with Child- Pugh class-A/single small (</=3 cm) hepatocellular carcinoma. Clin. Mol. Hepatol. 2022, 28, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; He, Y.; Xu, L.; Zhao, F.; Zhou, Y.; Zhang, L.; Peng, Q.; Zhang, H.; Zhang, Q.; Cao, T.; et al. Higher Risk of Dyslipidemia With Coformulated Elvitegravir, Cobicistat, Emtricitabine, and Tenofovir Alafenamide than Efavirenz, Lamivudine, and Tenofovir Disoproxil Fumarate Among Antiretroviral-Naive People Living With HIV in China. J. Acquir. Immune Defic. Syndr. 2022, 91, S8–S15. [Google Scholar] [CrossRef] [PubMed]
- van Amerongen, M.J.; Jenniskens, S.F.M.; van den Boezem, P.B.; Futterer, J.J.; de Wilt, J.H.W. Radiofrequency ablation compared to surgical resection for curative treatment of patients with colorectal liver metastases—A meta-analysis. HPB 2017, 19, 749–756. [Google Scholar] [CrossRef]
- Tympa, A.; Theodoraki, K.; Tsaroucha, A.; Arkadopoulos, N.; Vassiliou, I.; Smyrniotis, V. Anesthetic Considerations in Hepatectomies under Hepatic Vascular Control. HPB Surg. 2012, 2012, 720754. [Google Scholar] [CrossRef][Green Version]
- Iwasaka, H.; Kitano, T.; Mizutani, A.; Taniguchi, K.; Honda, N.; Kim, Y.I.; Kobayashi, M. Hemodynamic and oxygen delivery-consumption changes during partial liver resection. J. Anesth. 1993, 7, 145–150. [Google Scholar] [CrossRef]
- Jang, J.Y.; Jung, J.; Lee, D.; Shim, J.H.; Kim, K.M.; Lim, Y.S.; Lee, H.C.; Park, J.H.; Yoon, S.M. Stereotactic body radiation therapy for elderly patients with small hepatocellular carcinoma: A retrospective observational study. J. Liver Cancer 2022, 22, 136–145. [Google Scholar] [CrossRef]
- De Cock, A.M.; Strens, D.; Van Osta, P.; Standaert, B. Infections and hospital bed-days among aging adults: A five-year retrospective study in a Belgian general hospital. Front. Med. Technol. 2022, 4, 912469. [Google Scholar] [CrossRef]
- Cosqueric, G.; Sebag, A.; Ducolombier, C.; Thomas, C.; Piette, F.; Weill-Engerer, S. Sarcopenia is predictive of nosocomial infection in care of the elderly. Br. J. Nutr. 2006, 96, 895–901. [Google Scholar] [CrossRef]
- Jo, S.J.; Rhu, J.; Kim, J.M.; Choi, G.S.; Joh, J.W. Indications for open hepatectomy in the era of laparoscopic liver resection: A high volume single institutional study. J. Liver Cancer 2022, 22, 146–157. [Google Scholar] [CrossRef] [PubMed]
| Study | Country | Study Design | PSM | Participating Institution | Recruitment Period | Inclusion Criteria | Elderly Definition | Number | Intervention Group | Control Group | Follow-Up (Months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Conticchio 2022 [11] | Europe | Retrospective cohort | Yes | Multicenter | 2009–2019 | single ≤ 3 cm HCC | 70 | 116 (58/58) | RFA | LLR | 36 |
| Conticchio 2021 [12] | Europe | Retrospective cohort | Yes | Multicenter | 2009–2019 | HCC with Child A-B disease, in BCLC 0/A stage, with tumor within Milan criteria | 70 | 272 (136/136) | RFA | LR | 60 |
| Delvecchio 2021 [13] | Europe | Retrospective cohort | Yes | Multicenter | 2009–2019 | single HCC ≤ 3 cm located in posterosuperior segments (4a, 7, 8) | 70 | 52 (26/26) | RFA | LR | 60 |
| Shin 2019 [14] | Korea | Retrospective cohort | Yes | Multicenter | 2008–2014 | BCLC 0-A staged HCC patients | 70 | 270 (139/131) | RFA | LR | 108 |
| Jiang 2019 [15] | USA | Retrospective cohort | Yes | SEER DB | 2004–2015 | very early- or early-stage HCC | 65 | 1912 (956/956) | RFA | LR | 60 |
| Kaibori 2018 [16] | Japan | Retrospective cohort | Yes | Multicenter | 2000–2007 | early-stage HCC (≤3 cm) | 75 | 922 (461/461) | RFA | LR | 60 |
| Harada 2016 [17] | Japan | Retrospective cohort | No | Multicenter | 2008–2015 | primary HCC with BCLC stage 0 and A disease and portal hypertension | NR | 88 (40/48) | RFA | LLR, OLR | 84 |
| Bauschke 2016 [18] | Germany | Retrospective cohort | No | Single | 1995–2014 | HCC patients | 70 | 127 (64/63) | RFA | partial LR | 120 |
| Ito 2016 [19] | Japan | Retrospective cohort | Yes | Single | 2011–2013 | surface HCC (≤3 cm, 1–3 nodules) | NR | 54 (27–27) | RFA | LR | 36 |
| Liu 2014 [20] | Taiwan | Retrospective cohort | Yes | Single | 2002–2013 | newly diagnosed HCC | 75 | 257 (139/118) | RFA | LR | 120 |
| Peng 2013 [21] | China | Retrospective cohort | No | Single | 2003–2007 | very early or early HCC (single HCC ≤ 5 cm or up to 3 nodules < 3 cm) | 65 | 180 (89/91) | RFA | OLR | 80 |
| Massarweh 2012 [22] | USA | Retrospective cohort | No | Medicare DB | 2002–2005 | HCC patients | 66 | 415 (206/209) | RFA | LR | 60 |
| Mirici-Cappa 2010 [23] | Italy | Retrospective cohort | Yes | Multicenter | 1987–2004 | HCC patients | 70 | 238 (119/32) | RFA | LR | 120 |
| Outcomes | No of Studies | No. of Patients, RFA/Surgery | Pooled OR | 95% CI | I2 | p of Chi2 |
|---|---|---|---|---|---|---|
| All | ||||||
| In-hospital mortality | 3 | 167/217 | 0.61 | 0.06–5.93 | 0% | 0.61 |
| 30-day mortality | 1 | 206/209 | 0.51 | 0.24–1.08 | NA | NA |
| 90-day mortality | 2 | 342/345 | 0.69 | 0.42–1.14 | 0% | 0.92 |
| Liver failure-related mortality | 2 | 109/159 | 0.09 | 0.00–1.61 | NA | NA |
| Sensitivity analysis: HCC size ≤ 3 cm | ||||||
| In-hospital mortality | 1 | 58/58 | NA | NA | NA | NA |
| 30-day mortality | 0 | - | - | - | - | - |
| 90-day mortality | 1 | 58/58 | 1 | 0.14–7.35 | NA | NA |
| Liver failure-related mortality | 0 | - | - | - | - | - |
| Outcomes | No of Studies | No. of Patients, RFA/Surgery | Pooled OR | 95% CI | I2 | p of Chi2 |
|---|---|---|---|---|---|---|
| Overall complications | 3 | 183/231 | 0.22 | 0.14–0.36 | 0% | 0.67 |
| Major complications | 3 | 245/295 | 0.33 | 0.13–0.84 | 40% | 0.19 |
| Minor complications | 3 | 183/231 | 1.02 | 0.11–9.81 | 80% | 0.006 |
| Postoperative liver failure | 3 | 245/295 | 0.09 | 0.02–0.41 | 0% | 0.49 |
| Postoperative heart failure | 2 | 115/117 | 0.25 | 0.03–2.28 | 0% | 0.79 |
| Postoperative respiratory failure | 1 | 136/136 | 0.37 | 0.14–0.99 | NA | NA |
| Postoperative renal failure | 1 | 136/136 | 0.16 | 0.02–1.35 | NA | NA |
| Bile leakage | 2 | 156/204 | 0.29 | 0.03–2.49 | 0% | 0.48 |
| Ascites | 2 | 225/227 | 0.12 | 0.03–0.42 | 8% | 0.3 |
| Hemorrhage | 1 | 136/136 | 0.26 | 0.07–0.94 | NA | NA |
| Wound infection | 1 | 136/136 | 0.28 | 0.06–1.35 | NA | NA |
| Intra-abdominal abscess | 1 | 136/136 | 0.06 | 0.00–0.97 | NA | NA |
| Portal vein thrombosis | 1 | 136/136 | 0.5 | 0.04–5.54 | NA | NA |
| Systemic infection | 1 | 136/136 | 0.26 | 0.08–0.82 | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, J.-J.; Koo, S.; Choi, G.H.; Lee, M.W.; Ryoo, S.; Park, J.; Park, D.A. Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Curr. Oncol. 2024, 31, 324-334. https://doi.org/10.3390/curroncol31010021
Yoo J-J, Koo S, Choi GH, Lee MW, Ryoo S, Park J, Park DA. Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Current Oncology. 2024; 31(1):324-334. https://doi.org/10.3390/curroncol31010021
Chicago/Turabian StyleYoo, Jeong-Ju, Sujin Koo, Gi Hong Choi, Min Woo Lee, Seungeun Ryoo, Jungeun Park, and Dong Ah Park. 2024. "Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis" Current Oncology 31, no. 1: 324-334. https://doi.org/10.3390/curroncol31010021
APA StyleYoo, J.-J., Koo, S., Choi, G. H., Lee, M. W., Ryoo, S., Park, J., & Park, D. A. (2024). Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Current Oncology, 31(1), 324-334. https://doi.org/10.3390/curroncol31010021





