Purely Off-Clamp Laparoscopic Partial Nephrectomy Stands the Test of Time: 15 Years Functional and Oncologic Outcomes from a Single Center Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Dataset
- Age, gender, race, body mass index (BMI), relevant comorbidities (hypertension and diabetes), ASA score;
- Tumor side and clinical size;
- Clamping technique, hemoglobin drop, perioperative complications and length of hospital stay (LOS);
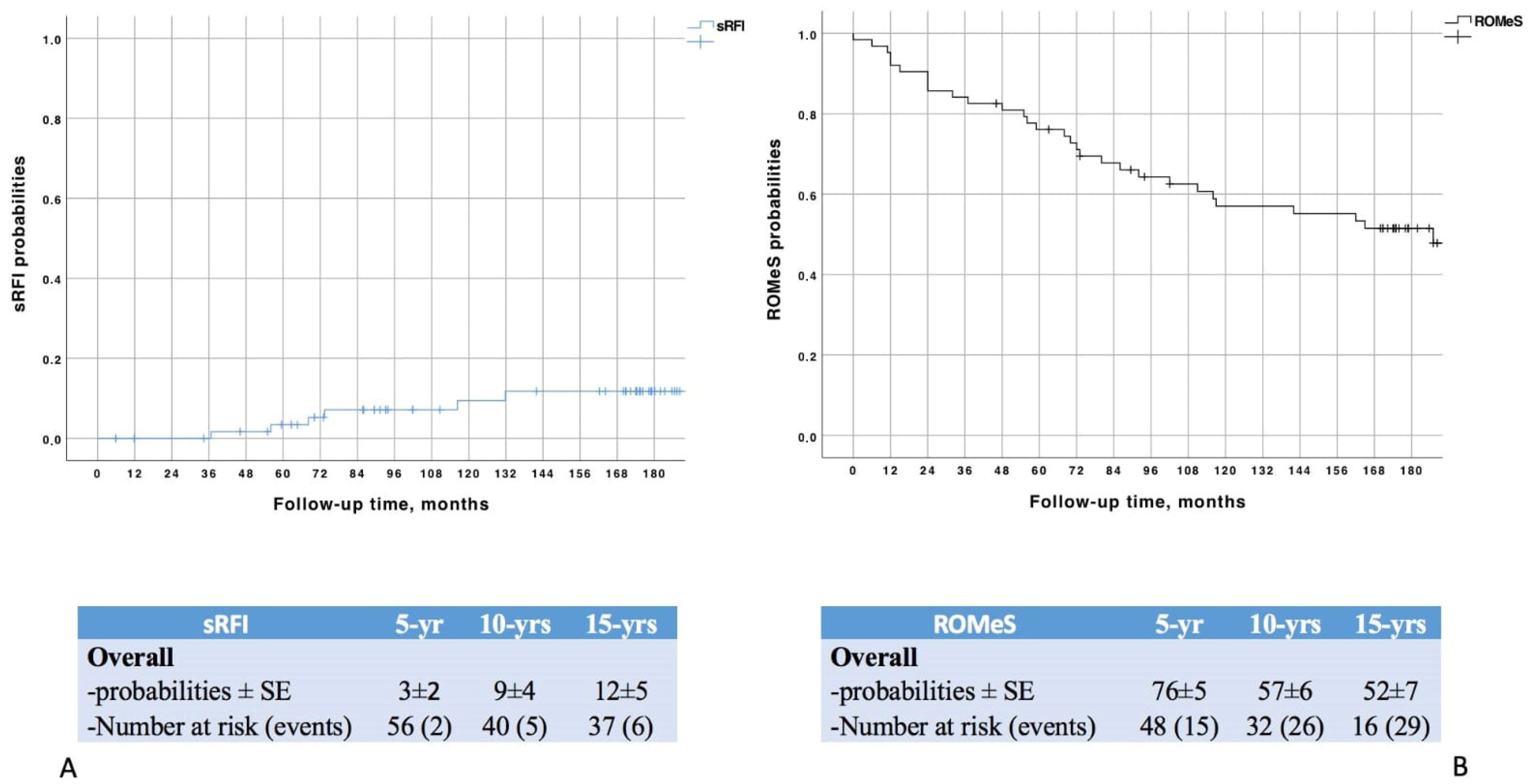
- Serum creatinine levels before surgery and at follow-up. At each assessment, estimated glomerular filtration rates [eGFR] was calculated by means of the Chronic Kidney Disease Epidemiology Collaboration formula [5] and stratified according to the National Kidney Foundation and the Kidney Disease Outcomes Quality Initiative [6]. Any new onset of Chronic Kidney Disease (CKD) stage ≥ IIIa (or ≥ IV, in patients with a baseline already <60 mL/min/1.73 m2) was defined as “significant renal function impairment” (sRFI);
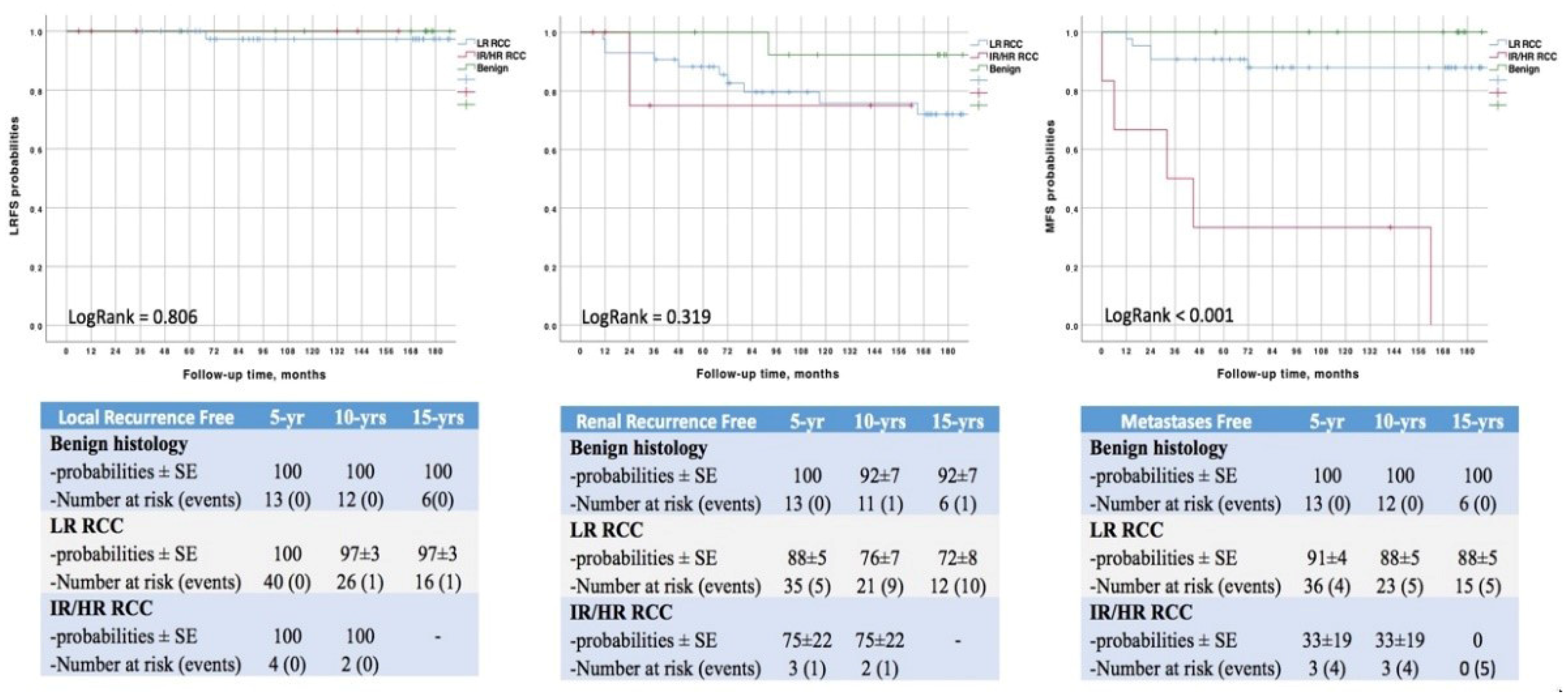
- Final histology and staging [7]. Patients with clear cell (ccRCC) and non-clear cell renal cell carcinomas (non-ccRCC) were stratified into risk groups according to the Mayo Clinic Risk Stratification System (MCRSS) [8] and the University of California Integrated Staging System (UCISS) [9], respectively;
- Tumor recurrence time and site. Disease-free (DFS), cancer-specific (CSS) and overall survival (OS).
2.2. Postoperative Care and Surgical Technique
2.3. Study Objective
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Ljungberg, B.; Albiges, L.; Abu-Ghanem, Y.; Bedke, J.; Capitanio, U.; Dabestani, S.; Fernández-Pello, S.; Giles, R.H.; Hofmann, F.; Hora, M.; et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update. Eur. Urol. 2022, 82, 399–410. [Google Scholar] [CrossRef]
- Gallucci, M.; Guaglianone, S.; Carpanese, L.; Papalia, R.; Simone, G.; Forestiere, E.; Leonardo, C. Superselective Embolization as First Step of Laparoscopic Partial Nephrectomy. Urology 2007, 69, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Winfield, H.N.; Donovan, J.F.; Lund, G.O.; Kreder, K.J.; Stanley, K.E.; Brown, B.P.; Loening, S.A.; Clayman, R.V. Laparoscopic Partial Nephrectomy: Initial Experience and Comparison to the Open Surgical Approach. J. Urol. 1995, 153, 1409–1414. [Google Scholar] [CrossRef]
- Inker, L.A.; Schmid, C.H.; Tighiouart, H.; Eckfeldt, J.H.; Feldman, H.I.; Greene, T.; Kusek, J.W.; Manzi, J.; Van Lente, F.; Zhang, Y.L.; et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 2012, 367, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Coresh, J.; Astor, B.C.; Greene, T.; Eknoyan, G.; Levey, A.S. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third national health and nutrition examination survey. Am. J. Kidney Dis. 2003, 41, 1–12. [Google Scholar] [CrossRef]
- Novara, G.; Ficarra, V.; Antonelli, A.; Artibani, W.; Bertini, R.; Carini, M.; Cunico, S.C.; Imbimbo, C.; Longo, N.; Martignoni, G.; et al. Validation of the 2009 TNM version in a large multi-institutional cohort of patients treated for renal cell carcinoma: Are further improvements needed? Eur Urol. 2010, 58, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Leibovich, B.C.; Blute, M.L.; Cheville, J.C.; Lohse, C.M.; Frank, I.; Kwon, E.D.; Weaver, A.L.; Parker, A.S.; Zincke, H. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: A stratification tool for prospective clinical trials. Cancer 2003, 97, 1663–1671. [Google Scholar] [CrossRef]
- Zisman, A.; Pantuck, A.J.; Dorey, F.; Said, J.W.; Shvarts, O.; Quintana, D.; Gitlitz, B.J.; Dekernion, J.B.; Figlin, R.A.; Belldegrun, A.S. Improved Prognostication of Renal Cell Carcinoma Using an Integrated Staging System. J. Clin. Oncol. 2001, 19, 1649–1657. [Google Scholar] [CrossRef]
- Brassetti, A.; Anceschi, U.; Bertolo, R.; Ferriero, M.; Tuderti, G.; Costantini, M.; Capitanio, U.; Larcher, A.; Antonelli, A.; Mottrie, A.; et al. Comprehensive long-term assessment of outcomes following robot-assisted partial nephrectomy for renal cell carcinoma: The ROMe’s achievement and its predicting nomogram. Minerva Urol. Nephrol. 2020, 72, 482–489. [Google Scholar] [CrossRef]
- Simone, G.; Misuraca, L.; Tuderti, G.; Minisola, F.; Ferriero, M.; Romeo, G.; Costantini, M.; Al-Rawashdah, S.F.; Guaglianone, S.; Gallucci, M. Purely off-clamp robotic partial nephrectomy: Preliminary 3-year oncological and functional outcomes. Int. J. Urol. 2018, 25, 606–614. [Google Scholar] [CrossRef]
- Gill, I.S.; Eisenberg, M.S.; Aron, M.; Berger, A.; Ukimura, O.; Patil, M.B.; Campese, V.; Thangathurai, D.; Desai, M.M. “Zero ischemia” partial nephrectomy: Novel laparoscopic and robotic technique. Eur Urol. 2011, 59, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Simone, G.; Papalia, R.; Guaglianone, S.; Forestiere, E.; Gallucci, M. Preoperative Superselective Transarterial Embolization in Laparoscopic Partial Nephrectomy: Technique, Oncologic, and Functional Outcomes. J. Endourol. 2009, 23, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- Pandolfo, S.D.; Loizzo, D.; Beksac, A.T.; Derweesh, I.; Celia, A.; Bianchi, L.; Elbich, J.; Costa, G.; Carbonara, U.; Lucarelli, G.; et al. Percutaneous thermal ablation for cT1 renal mass in solitary kidney: A multicenter trifecta comparative analysis versus robot-assisted partial nephrectomy. Eur. J. Surg. Oncol. (EJSO) 2022. [Google Scholar] [CrossRef]
- Pandolfo, S.D.; Beksac, A.T.; Derweesh, I.H.; Celia, A.; Schiavina, R.; Bianchi, L.; Costa, G.; Carbonara, U.; Loizzo, D.; Lucarelli, G.; et al. Percutaneous Ablation Vs Robot-Assisted Partial Nephrectomy for Completely Endophytic Renal Masses: A Multicenter Trifecta Analysis with a Minimum 3-Year Follow-Up. J. Endourol. 2022. [Google Scholar] [CrossRef]
- Brassetti, A.; Cacciamani, G.E.; Mari, A.; Garisto, J.D.; Bertolo, R.; Sundaram, C.P.; Derweesh, I.; Bindayi, A.; Dasgupta, P.; Porter, J.; et al. On-Clamp vs. Off-Clamp Robot-Assisted Partial Nephrectomy for cT2 Renal Tumors: Retrospective Propensity-Score-Matched Multicenter Outcome Analysis. Cancers 2022, 14, 4431. [Google Scholar] [CrossRef]
- Zini, L.; Perrotte, P.; Capitanio, U.; Jeldres, C.; Shariat, S.F.; Antebi, E.; Saad, F.; Patard, J.J.; Montorsi, F.; Karakiewicz, P.I. Radical versus partial nephrectomy: Effect on overall and noncancer mortality. Cancer 2009, 115, 1465–1471. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.; Mullins, J.K.; Pierorazio, P.M.; Jayram, G.; Cohen, J.E.; Matlaga, B.R.; Allaf, M.E. Trends in Renal Surgery: Robotic Technology is Associated with Increased Use of Partial Nephrectomy. J. Urol. 2013, 189, 1229–1235. [Google Scholar] [CrossRef]
- Hughes, D.; Camp, C.; O’Hara, J.; Adshead, J. Health resource use after robot-assisted surgery vs open and conventional laparoscopic techniques in oncology: Analysis of English secondary care data for radical prostatectomy and partial nephrectomy. BJU Int. 2016, 117, 940–947. [Google Scholar] [CrossRef]
- Pierorazio, P.M.; Patel, H.D.; Feng, T.; Yohannan, J.; Hyams, E.S.; Allaf, M.E. Robotic-assisted Versus Traditional Laparoscopic Partial Nephrectomy: Comparison of Outcomes and Evaluation of Learning Curve. Urology 2011, 78, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Hevelone, N.D.; Lipsitz, S.R.; Kowalczyk, K.J.; Hu, J.C. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J. Urol. 2012, 187, 1392–1398. [Google Scholar] [CrossRef] [PubMed]
- Lane, B.R.; Campbell, S.C.; Gill, I.S. 10-Year Oncologic Outcomes After Laparoscopic and Open Partial Nephrectomy. J. Urol. 2013, 190, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Porpiglia, F.; Fiori, C.; Terrone, C.; Bollito, E.; Fontana, D.; Scarpa, R.M. Assessment of surgical margins in renal cell carcinoma after nephron sparing: A comparative study: Laparoscopy vs open surgery. J Urol. 2005, 173, 1098–1101. [Google Scholar] [CrossRef] [PubMed]
- Simone, G.; De Nunzio, C.; Ferriero, M.; Cindolo, L.; Brookman-May, S.; Papalia, R.; Sperduti, I.; Collura, D.; Leonardo, C.; Anceschi, U.; et al. Trends in the use of partial nephrectomy for cT1 renal tumors: Analysis of a 10-yr European multicenter dataset. Eur. J. Surg. Oncol. (EJSO) 2016, 42, 1729–1735. [Google Scholar] [CrossRef]
- Thompson, R.H.; Lane, B.R.; Lohse, C.M.; Leibovich, B.C.; Fergany, A.; Frank, I.; Gill, I.S.; Blute, M.L.; Campbell, S.C. Every Minute Counts When the Renal Hilum Is Clamped During Partial Nephrectomy. Eur. Urol. 2010, 58, 340–345. [Google Scholar] [CrossRef]
- Antonelli, A.; Cindolo, L.; Sandri, M.; Veccia, A.; Annino, F.; Bertagna, F.; Carini, M.; Celia, A.; D’Orta, C.; De Concilio, B.; et al. Is off-clamp robot-assisted partial nephrectomy beneficial for renal function? Data from the CLOCK trial. BJU Int. 2021, 129, 217–224. [Google Scholar] [CrossRef]
- Bertolo, R.; Bove, P.; Sandri, M.; Celia, A.; Cindolo, L.; Cipriani, C.; Falsaperla, M.; Leonardo, C.; Mari, A.; Parma, P.; et al. Randomized Clinical Trial Comparing On-clamp Versus Off-clamp Laparoscopic Partial Nephrectomy for Small Renal Masses (CLOCK II Laparoscopic Study): A Intention-to-treat Analysis of Perioperative Outcomes. Eur. Urol. Open Sci. 2022, 46, 75–81. [Google Scholar] [CrossRef]
- Pandolfo, S.D.; Beksac, A.T.; Derweesh, I.; Celia, A.; Schiavina, R.; Bianchi, L.; Costa, G.; Carbonara, U.; Loizzo, D.; Lucarelli, G.; et al. On-clamp versus purely off-clamp robot-assisted partial nephrectomy in solitary kidneys: Comparison of perioperative outcomes and chronic kidney disease progression at two high-volume centers. Minerva Urol Nephrol. 2021, 73, 739–745. [Google Scholar]
- Lane, B.R.; Novick, A.C.; Babineau, D.; Fergany, A.F.; Kaouk, J.H.; Gill, I.S. Comparison of Laparoscopic and Open Partial Nephrectomy for Tumor in a Solitary Kidney. J. Urol. 2008, 179, 847–852. [Google Scholar] [CrossRef]
- Thompson, R.H.; Frank, I.; Lohse, C.M.; Saad, I.R.; Fergany, A.; Zincke, H.; Leibovich, B.C.; Blute, M.L.; Novick, A.C. The Impact of Ischemia Time During Open Nephron Sparing Surgery on Solitary Kidneys: A Multi-Institutional Study. J. Urol. 2007, 177, 471–476. [Google Scholar] [CrossRef]
- Ng, A.M.; Shah, P.H.; Kavoussi, L.R. Laparoscopic Partial Nephrectomy: A Narrative Review and Comparison with Open and Robotic Partial Nephrectomy. J. Endourol. 2017, 31, 976–984. [Google Scholar] [CrossRef]
- Simone, G.; Gill, I.S.; Mottrie, A.; Kutikov, A.; Patard, J.-J.; Alcaraz, A.; Rogers, C.G. Indications, Techniques, Outcomes, and Limitations for Minimally Ischemic and Off-clamp Partial Nephrectomy: A Systematic Review of the Literature. Eur. Urol. 2015, 68, 632–640. [Google Scholar] [CrossRef]
- Wszolek, M.F.; Kenney, P.A.; Lee, Y.; Libertino, J.A. Comparison of hilar clamping and non-hilar clamping partial nephrectomy for tumours involving a solitary kidney. BJU Int. 2010, 107, 1886–1892. [Google Scholar] [CrossRef] [PubMed]
- Simone, G.; Capitanio, U.; Tuderti, G.; Presicce, F.; Leonardo, C.; Ferriero, M.; Misuraca, L.; Costantini, M.; Larcher, A.; Minisola, F.; et al. On-clamp versus off-clamp partial nephrectomy: Propensity score-matched comparison of long-term functional outcomes. Int. J. Urol. 2019, 26, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.D.; Abdel Raheem, A.; Kim, K.H.; Oh, C.K.; Park, S.Y.; Kim, Y.S.; Ham, W.S.; Han, W.K.; Choi, Y.D.; Chung, B.H.; et al. Functional and oncological outcomes of open, laparoscopic and robot-assisted partial nephrectomy: A multicentre comparative matched-pair analyses with a median of 5 years’ follow-up. BJU Int. 2018, 122, 618–626. [Google Scholar] [CrossRef]
- Mukkamala, A.; He, C.; Weizer, A.Z.; Hafez, K.S.; Miller, D.C.; Montgomery, J.S.; Wolf, J.S. Long-Term Oncologic Outcomes of Minimally Invasive Partial Nephrectomy for Renal-Cell Carcinoma. J. Endourol. 2014, 28, 649–654. [Google Scholar] [CrossRef]
- Stewart, S.B.; Thompson, R.H.; Psutka, S.P.; Cheville, J.C.; Lohse, C.M.; Boorjian, S.A.; Leibovich, B.C. Evaluation of the National Comprehensive Cancer Network and American Urological Association Renal Cell Carcinoma Surveillance Guidelines. J. Clin. Oncol. 2014, 32, 4059–4065. [Google Scholar] [CrossRef] [PubMed]

| LPN | Overall n = 63 | No ROMeS n = 30 (48%) | ROMeS n = 33 (52%) | p |
|---|---|---|---|---|
| Age, yrs | 64(54–71) | 71(62–75) | 57(50–66) | 0.001 |
| Male gender, n(%) | 39(60%) | 23(77%) | 16(48%) | 0.021 |
| BMI | 24.5(21.8–27.8) | 24(21.7–27.6) | 24.5(21.8–28.1) | 0.445 |
| Solitary kidney, n(%) | 3(4%) | 2(7%) | 1(3%) | 0.498 |
| Diabetes, n(%) | 14(22%) | 6(20%) | 8(24%) | 0.473 |
| Hypertension, n(%) | 33(52%) | 16(53%) | 17(52%) | 0.491 |
| ASA score ≧ 3, n(%) | 9(14%) | 4(13%) | 5(15%) | 0.434 |
| Clinical Tumor Size, cm | 3(2–4) | 3(2–4) | 3(2–4) | 0.464 |
| LPN | Overall n = 63 | No ROMeS n = 30 (48%) | ROMeS n = 33 (52%) | p |
|---|---|---|---|---|
| LOS, days | 5 (3–6) | 5 (4–6) | 5 (3–6) | 0.873 |
| Hb drop, g/dL | 2.5 (2.1–2.7) | 2.5 (2.1–3) | 2.1 (2.1–2.5) | 0.124 |
| PSM, n (%) | 3 (5%) | 3 (10%) | 0 (0%) | 0.063 |
| Histology, n (%) | 0.026 | |||
| -Benign | 14 (22%) | 3 (10%) | 11 (33%) | |
| -ccRCC | 40 (63%) | 23 (77%) | 17 (51%) | |
| -non-ccRCC | 9 (15%) | 4 (13%) | 5 (15%) | |
| pT †, n (%) | 0.997 | |||
| -1a | 47 (75%) | 22 (74%) | 25 (76%) | |
| -1b | 12 (19%) | 6 (20%) | 6 (18%) | |
| -2a | 2 (3%) | 1 (3%) | 1 (3%) | |
| -3a | 2 (3%) | 1 (3%) | 1 (3%) | |
| MCRSS ‡, n (%) | 0.022 | |||
| -Low Risk | 35 (56%) | 18 (60%) | 17 (52%) | |
| -Intermediate/High Risk | 5 (8%) | 5 (17%) | 0 (0%) | |
| UCISS ¥, n (%) | 0.077 | |||
| -Low Risk | 8 (13%) | 3 (10%) | 5 (15%) | |
| -Intermediate/High Risk | 1 (1%) | 1 (3%) | 0 (0%) | |
| eGFR, mL/min/1.73 m2 | ||||
| -at baseline | 80.1 (64.7–89.9) | 80 (64.5–87.9) | 80.5 (66.4–92.4) | 0.573 |
| -at last follow-up | 75.1 (62.9–84.9) | 55.3 (62.9–75) | 79.3 (74.2–95.3) | <0.001 |
| sRFI, n (%) | 9 (14%) | 9 (30%) | 0 (0%) | <0.001 |
| Univariable Analysis | Multivariable Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |||
| Lower | Higher | Lower | Higher | |||||
| Age | 1.06 | 1.02 | 1.10 | 0.002 | 1.05 | 1.004 | 1.09 | 0.03 |
| Male Gender | 2.80 | 1.19 | 6.59 | 0.02 | 1.61 | 0.68 | 3.82 | 0.28 |
| BMI | 0.96 | 0.87 | 1.06 | 0.43 | - | - | - | - |
| Solitary Kidney | 2.45 | 0.58 | 10.34 | 0.22 | - | - | - | - |
| Diabetes Mellitus | 0.96 | 0.77 | 1.17 | 0.82 | - | - | - | - |
| Hypertension | 1.10 | 0.89 | 1.23 | 0.78 | - | - | - | - |
| ASA score ≧ 3 | 0.81 | 0.88 | 1.09 | 0.61 | - | - | - | - |
| Clinical tumor size | 1.08 | 0.87 | 1.35 | 0.48 | - | - | - | - |
| Preoperative eGFR | 0.99 | 0.97 | 1.02 | 0.79 | - | - | - | - |
| LR RCC vs. Benign IR/HR RCC vs. Benign | 3.06 11.32 | 1.01 2.79 | 10.26 45.85 | 0.047 0.001 | 3.24 5.72 | 1.01 1.27 | 10.88 25.77 | 0.048 0.023 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brassetti, A.; Anceschi, U.; Bove, A.M.; Prata, F.; Costantini, M.; Ferriero, M.; Mastroianni, R.; Misuraca, L.; Tuderti, G.; Torregiani, G.; et al. Purely Off-Clamp Laparoscopic Partial Nephrectomy Stands the Test of Time: 15 Years Functional and Oncologic Outcomes from a Single Center Experience. Curr. Oncol. 2023, 30, 1196-1205. https://doi.org/10.3390/curroncol30010092
Brassetti A, Anceschi U, Bove AM, Prata F, Costantini M, Ferriero M, Mastroianni R, Misuraca L, Tuderti G, Torregiani G, et al. Purely Off-Clamp Laparoscopic Partial Nephrectomy Stands the Test of Time: 15 Years Functional and Oncologic Outcomes from a Single Center Experience. Current Oncology. 2023; 30(1):1196-1205. https://doi.org/10.3390/curroncol30010092
Chicago/Turabian StyleBrassetti, Aldo, Umberto Anceschi, Alfredo Maria Bove, Francesco Prata, Manuela Costantini, Mariaconsiglia Ferriero, Riccardo Mastroianni, Leonardo Misuraca, Gabriele Tuderti, Giulia Torregiani, and et al. 2023. "Purely Off-Clamp Laparoscopic Partial Nephrectomy Stands the Test of Time: 15 Years Functional and Oncologic Outcomes from a Single Center Experience" Current Oncology 30, no. 1: 1196-1205. https://doi.org/10.3390/curroncol30010092
APA StyleBrassetti, A., Anceschi, U., Bove, A. M., Prata, F., Costantini, M., Ferriero, M., Mastroianni, R., Misuraca, L., Tuderti, G., Torregiani, G., Covotta, M., Gallucci, M., & Simone, G. (2023). Purely Off-Clamp Laparoscopic Partial Nephrectomy Stands the Test of Time: 15 Years Functional and Oncologic Outcomes from a Single Center Experience. Current Oncology, 30(1), 1196-1205. https://doi.org/10.3390/curroncol30010092







