Wait Times and Survival in Lung Cancer Patients across the Province of Quebec, Canada
Abstract
:1. Introduction
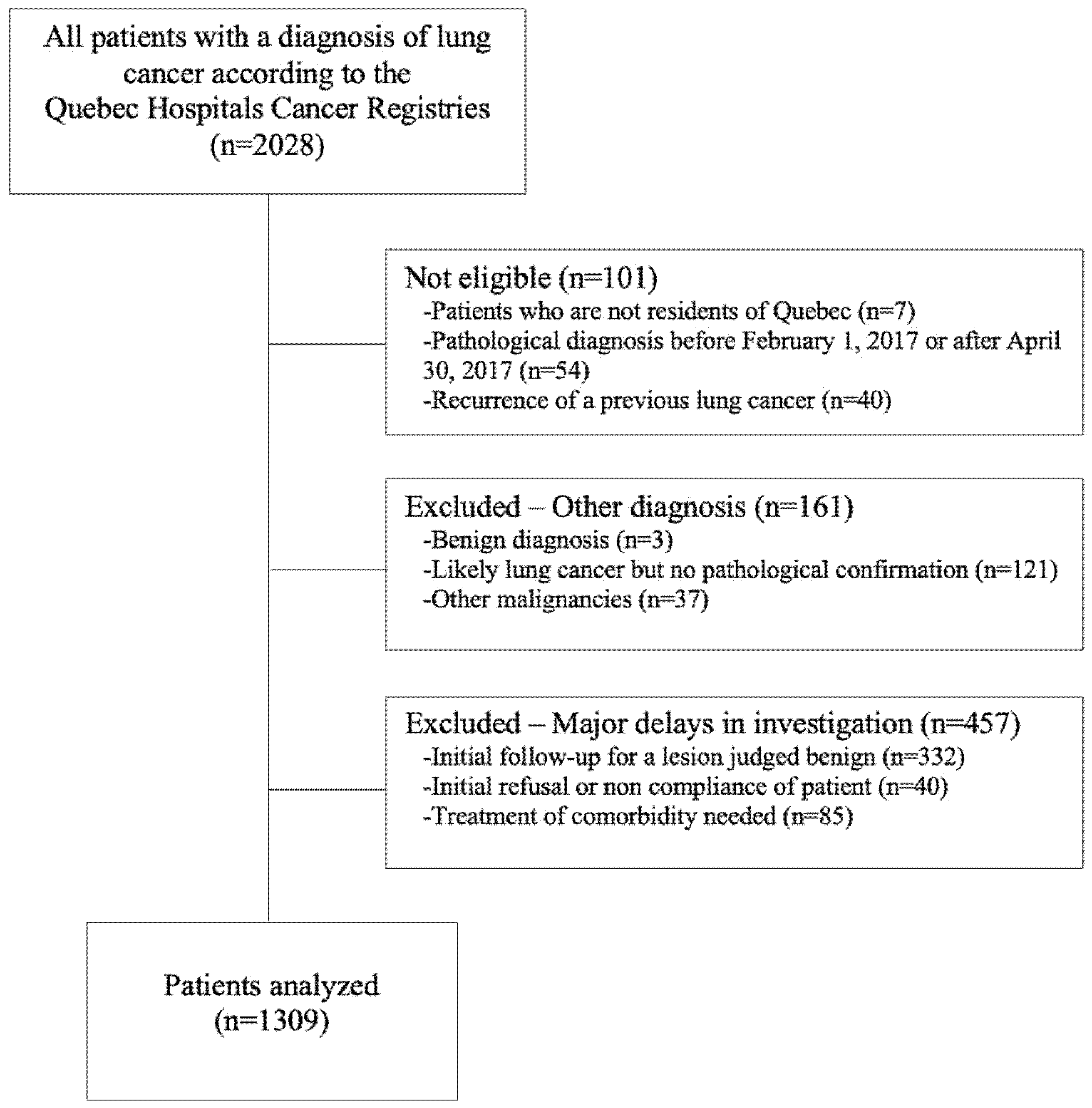
2. Materials and Methods
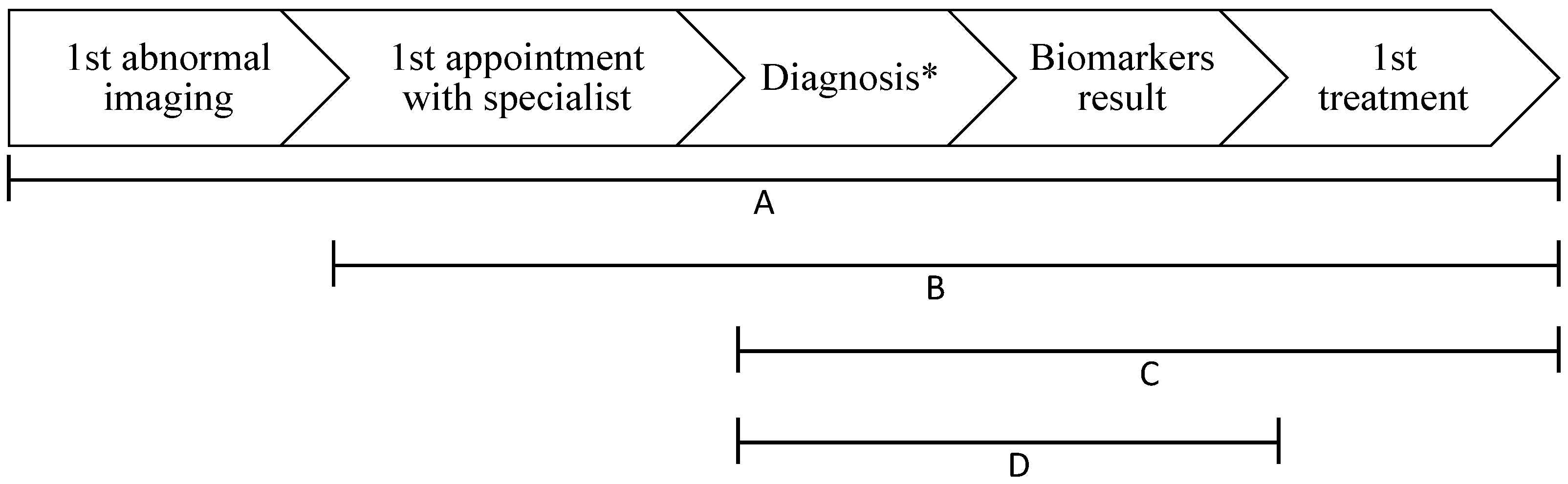
- First abnormal imaging to first treatment;
- First appointment with a specialist to first treatment;
- First appointment with a specialist to surgery;
- Diagnosis to first treatment;
- ○
- Diagnosis to surgery;
- ○
- Diagnosis to definitive radiation;
- ○
- Diagnosis to definitive chemoradiation;
- ○
- Diagnosis to systemic treatment.
- Radiation referral to radiation;
- Diagnosis to biomarker result.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Intervals | NSCLC I–II | NSCLC III–IV | p-Value | ||
|---|---|---|---|---|---|
| n | Time, d | n | Time, d | ||
| 1st abnormal imaging to 1st treatment | 326 | 114 (13–384) | 413 | 66 (0–300) | <0.0001 |
| 1st appointment with specialist to 1st treatment | 319 | 79 (0–249) | 417 | 50 (0–205) | <0.0001 |
| Radiation referral to first radiation treatment | 60 | 36 (11–145) | 107 | 27 (0–211) | 0.5 |
| 1st appointment with specialist to surgery | 252 | 77 (6–285) | 49 | 75 (9–205) | 0.7 |
| Diagnosis * to 1st treatment | 208 | 48 (0–185) | 382 | 29 (0–147) | <0.0001 |
| Intervals | NSCLC | SCLC | p-Value | ||
|---|---|---|---|---|---|
| n | Time, d | n | Time, d | ||
| 1st abnormal imaging to 1st treatment | 739 | 86 (0–384) | 125 | 34 (2–259) | <0.0001 |
| 1st appointment with specialist to 1st treatment | 736 | 62 (0–249) | 125 | 25 (1–191) | <0.0001 |
| Radiation referral to first radiation treatment | 167 | 29 (0–211) | 21 | 35 (14–163) | 0.1 |
| Diagnosis * to 1st treatment | 590 | 35 (0–185) | 122 | 13 (0–68) | <0.0001 |
| Diagnosis * to definitive chemoradiation | 83 | 35 (8–118) | 24 | 21 (0–68) | 0.0006 |
| Wait Times | NSCLC I–II | NSCLC III–IV | ||||
|---|---|---|---|---|---|---|
| n | HR (95% CI) | p-Value | n | HR (95% CI) | p-Value | |
| 1st abnormal imaging to 1st treatment | 300 | 1.00 (1.00–1.01) | 1.0 | 368 | 0.99 (0.99–1.00) | <0.0001 |
| 1st appointment with specialist to 1st treatment | 292 | 1.00 (0.99–1.01) | 0.9 | 369 | 0.99 (0.99–1.00) | <0.0001 |
| Diagnosis * to 1st treatment | 194 | 1.00 (0.99–1.01) | 0.6 | 348 | 0.99 (0.99–1.00) | 0.02 |
| Wait Times | NSCLC | SCLC | ||||
|---|---|---|---|---|---|---|
| n | HR (95% CI) | p-Value | n | HR (95% CI) | p-Value | |
| 1st abnormal imaging to 1st treatment | 668 | 0.99 (0.99–0.99) | <0.0001 | 108 | 1.00 (0.99–1.00) | 0.3 |
| 1st appointment with specialist to 1st treatment | 661 | 0.99 (0.99–0.99) | <0.0001 | 106 | 1.00 (0.99–1.00) | 0.3 |
| Diagnosis * to 1st treatment | 542 | 0.99 (0.99–0.99) | <0.0001 | 103 | 0.99 (0.98–1.00) | 0.2 |
References
- Noone, A.M.; Howlader, N.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; et al. (Eds.) SEER Cancer Statistics Review 1975–2015; National Cancer Institute: Bethesda, MD, USA, 2018. Available online: https://seer.cancer.gov/csr/1975_2015/ (accessed on 21 March 2021).
- Ellison, L.F. Progress in net cancer survival in Canada over 20 years. Health Rep. 2018, 29, 10–18. [Google Scholar]
- Canadian Cancer Statistics Advisory Committee; Statistics Canada and the Public Health Agency of Canada (CCS). Canadian Cancer Statistics 2021; Canadian Cancer Statistics Advisory Committee. 2021. Available online: https://cdn.cancer.ca/-/media/files/research/cancer-statistics/2021-statistics/2021-pdf-en-final.pdf (accessed on 7 November 2021).
- Stanley, K.E. Prognostic factors for survival in patients with inoperable lung cancer. J. Natl. Cancer Inst. 1980, 65, 25–32. [Google Scholar] [PubMed]
- Blackstock, A.W.; Herndon, J.E.; Paskett, E.D.; Perry, M.C.; Graziano, S.L.; Muscato, J.J.; Kosty, M.P.; Akerley, W.L.; Holland, J.; Fleishman, S. Outcomes among African-American/non-African-American patients with advanced non-small-cell lung carcinoma: Report from the Cancer and Leukemia Group B. J. Natl. Cancer Inst. 2002, 94, 284–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Society, C.C. Prognosis and Survival for Lung Cancer. Available online: https://www.cancer.ca/en/cancer-information/cancer-type/lung/prognosis-and-survival/?region=on (accessed on 26 July 2021).
- Kawaguchi, T.; Takada, M.; Kubo, A.; Matsumura, A.; Fukai, S.; Tamura, A.; Saito, R.; Maruyama, Y.; Kawahara, M.; Ou, S.H. Performance status and smoking status are independent favorable prognostic factors for survival in non-small cell lung cancer: A comprehensive analysis of 26,957 patients with NSCLC. J. Thorac. Oncol. 2010, 5, 620–630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sculier, J.P.; Chansky, K.; Crowley, J.J.; Van Meerbeeck, J.; Goldstraw, P. The impact of additional prognostic factors on survival and their relationship with the anatomical extent of disease expressed by the 6th Edition of the TNM Classification of Malignant Tumors and the proposals for the 7th Edition. J. Thorac. Oncol. 2008, 3, 457–466. [Google Scholar] [CrossRef]
- Schild, S.E.; Tan, A.D.; Wampfler, J.A.; Ross, H.J.; Yang, P.; Sloan, J.A. A new scoring system for predicting survival in patients with non-small cell lung cancer. Cancer Med. 2015, 4, 1334–1343. [Google Scholar] [CrossRef] [PubMed]
- Frelinghuysen, M.; Fest, J.; Van der Voort Van, N.C.; Van der Holt, B.; Hoogeman, M.; Nuyttens, J. Consequences of Referral Time and Volume Doubling Time in Inoperable Patients with Early Stage Lung Cancer. Clin. Lung Cancer 2017, 18, e403–e409. [Google Scholar] [CrossRef] [PubMed]
- Mathews, M.; Ryan, D.; Bulman, D. What does satisfaction with wait times mean to cancer patients? BMC Cancer 2015, 15, 1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- BTS recommendations to respiratory physicians for organising the care of patients with lung cancer. The Lung Cancer Working Party of the British Thoracic Society Standards of Care Committee. Thorax 1998, 53 (Suppl. 1), S1–S8. [CrossRef] [PubMed] [Green Version]
- Jean Latreille, M.C.; Bélanger, C. Mécanisme Central de Gestion d’Accès à la Chirurgie Oncologique: Cadre de Référence; Direction Québécoise de Cancérologie, Ed.; La Direction des communications du Ministère de la Santé et des Services Sociaux: Québec, QC, Canada, 2012.
- Loutfi, A.; Laflamme, B.; Corriveau, M. Mécanisme Central de Gestion de l’Accès aux Services de Radio-Oncologie: Cadre de Référence; Direction Québécoise de Cancérologie, Ed.; La Direction des Communications du Ministère de la Santé et des Services Sociaux: Québec, QC, Canada, 2010.
- Malin, J.L.; Asch, S.M.; Kerr, E.A.; McGlynn, E.A. Evaluating the quality of cancer care: Development of cancer quality indicators for a global quality assessment tool. Cancer 2000, 88, 701–707. [Google Scholar] [CrossRef]
- Liberman, M.; Liberman, D.; Sampalis, J.S.; Mulder, D.S. Delays to surgery in non-small-cell lung cancer. Can. J. Surg. 2006, 49, 31–36. [Google Scholar] [PubMed]
- Jensen, A.R.; Mainz, J.; Overgaard, J. Impact of delay on diagnosis and treatment of primary lung cancer. Acta Oncol. 2002, 41, 147–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olsson, J.K.; Schultz, E.M.; Gould, M.K. Timeliness of care in patients with lung cancer: A systematic review. Thorax 2009, 64, 749–756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasymjanova, G.; Small, D.; Cohen, V.; Jagoem, R.T.; Batist, G.; Sateren, W.; Ernst, P.; Pepe, C.; Sakr, L.; Agulnik, J. Lung cancer care trajectory at a Canadian centre: An evaluation of how wait times affect clinical outcomes. Curr. Oncol. 2017, 24, 302–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Largey, G.; Ristevski, E.; Chambers, H.; Davis, H.; Briggs, P. Lung cancer interval times from point of referral to the acute health sector to the start of first treatment. Aust. Health Rev. 2016, 40, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Forrest, L.F.; Adams, J.; White, M.; Rubin, G. Factors associated with timeliness of post-primary care referral, diagnosis and treatment for lung cancer: Population-based, data-linkage study. Br. J. Cancer 2014, 111, 1843–1851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Virally, J.; Choudat, L.; Chebbo, M.; Sartene, R.; Jagot, J.L.; Elhadad, A.; Brassier, D.; Habib, E.; Chalmin, B.; Boiron, C. Epidemiology and delays in the management of 355 patients with lung cancer. Rev. Mal. Respir. 2006, 23, 43–48. [Google Scholar] [CrossRef]

| Alliance Estrie-Montérégie (n = 214, 16%) | CHUM (n = 441, 34%) | CUSM (n = 200, 15%) | IUCPQ (n = 454, 35%) | p-Value | |
|---|---|---|---|---|---|
| Age, y | 68.8 ± 8.4 | 68.0 ± 9.2 | 69.1 ± 9.4 | 68.1 ± 9.7 | 0.5 |
| Sex | 0.3 | ||||
| Male | 114 (53%) | 209 (47%) | 90 (45%) | 213 (47%) | |
| Female | 100 (47%) | 232 (53%) | 110 (55%) | 241 (53%) | |
| Smoking status | 0.04 | ||||
| Ever-smoker | 200 (94%) | 409 (93%) | 172 (86%) | 416 (92%) | |
| Never-smoker | 5 (2%) | 21 (5%) | 18 (9%) | 22 (5%) | |
| Unknown | 9 (4%) | 11 (3%) | 10 (5%) | 16 (4%) | |
| ECOG performance status | <0.0001 | ||||
| 0 | 56 (26%) | 173 (39%) | 53 (27%) | 160 (35%) | |
| 1 | 57 (27%) | 117 (27%) | 53 (27%) | 159 (35%) | |
| 2 | 54 (25%) | 74 (17%) | 49 (25%) | 82 (18%) | |
| 3 | 34 (16%) | 61 (14%) | 26 (13%) | 35 (8%) | |
| 4 | 1 (1%) | 2 (1%) | 2 (1%) | 0 | |
| Unknown | 12 (6%) | 14 (3%) | 17 (9%) | 18 (4%) | |
| Histopathology | 0.1 | ||||
| NSCLC | |||||
| Adenocarcinoma | 120 (56%) | 240 (54%) | 105 (53%) | 222 (49%) | |
| Squamous cell | 42 (20%) | 96 (22%) | 46 (23%) | 112 (25%) | |
| Other § | 12 (6%) | 51 (12%) | 20 (10%) | 55 (12%) | |
| SCLC | 40 (19%) | 54 (12%) | 29 (15%) | 65 (14%) | |
| Stage | 0.7 | ||||
| NSCLC | |||||
| I | 44 (21%) | 99 (23%) | 42 (21%) | 92 (20%) | |
| II | 15 (7%) | 32 (7%) | 13 (7%) | 40 (9%) | |
| III | 32 (15%) | 89 (20%) | 40 (20%) | 77 (17%) | |
| IV | 83 (39%) | 167 (38%) | 76 (38%) | 180 (40%) | |
| SCLC | |||||
| Limited | 10 (5%) | 15 (3%) | 4 (2%) | 16 (4%) | |
| Extensive | 30 (14%) | 39 (9%) | 25 (13%) | 49 (11%) | |
| Biomarkers | |||||
| EGFR mutation | |||||
| Positive | 8 (4%) | 13 (3%) | 4 (2%) | 5 (1%) | 0.02 |
| Negative | 66 (31%) | 150 (34%) | 62 (31%) | 115 (25%) | |
| Unknown | 140 (65%) | 278 (63%) | 134 (67%) | 334 (74%) | |
| ALK translocation | |||||
| Positive | 1 (1%) | 3 (1%) | 1 (1%) | 1 (0%) | 0.02 |
| Negative | 71 (33%) | 165 (37%) | 54 (27%) | 121 (27%) | |
| Unknown | 142 (66%) | 273 (62%) | 145 (73%) | 332 (73%) | |
| PD-L1 expression | |||||
| <1% | 10 (5%) | 32 (7%) | 25 (13%) | 18 (4%) | 0.0003 |
| 1%–49% | 22 (10%) | 59 (13%) | 33 (17%) | 44 (10%) | |
| ≥50% | 24 (11%) | 57 (13%) | 24 (12%) | 51 (11%) | |
| Unknown | 158 (74%) | 293 (66%) | 118 (59%) | 341 (75%) | |
| Primary treatment | 0.02 | ||||
| Surgery | 42 (20%) | 127 (29%) | 49 (25%) | 106 (23%) | |
| Definitive radiation * | 21 (10%) | 26 (6%) | 11 (6%) | 40 (9%) | |
| Definitive chemoradiation | 14 (7%) | 34 (8%) | 24 (12%) | 40 (9%) | |
| Systemic | 59 (28%) | 135 (31%) | 61 (31%) | 110 (24%) | |
| Symptoms-directed ** | 68 (32%) | 101 (23%) | 42 (21%) | 134 (30%) | |
| Unknown | 10 (5%) | 18 (4%) | 13 (7%) | 24 (5%) | |
| Number of investigations per patient † | 7.0 ± 2.1 | 7.3 ± 1.9 | 6.6 ± 1.6 | 6.7 ± 1.8 | <0.0001 |
| Procedure leading to diagnosis | 0.01 | ||||
| Flexible bronchoscopy | 55 (26%) | 124 (28%) | 124 (28%) | 134 (30%) | |
| EBUS/EUS | 30 (14%) | 84 (19%) | 84 (19%) | 84 (19%) | |
| Transthoracic needle biopsy | 66 (301%) | 97 (22%) | 97 (22%) | 114 (25%) | |
| Thoracoscopy | 16 (8%) | 67 (15%) | 67 (15%) | 44 (10%) | |
| Biopsy of a metastasis | 27 (13%) | 46 (10%) | 46 (10%) | 55 (12%) | |
| Thoracentesis | 16 (8%) | 20 (5%) | 20 (5%) | 19 (4%) | |
| Other ¶ | 0 | 2 (1%) | 2 (1%) | 2 (0%) | |
| Unknown | 4 (2%) | 1 (0%) | 1 (0%) | 2 (0%) | |
| Tumor board review | 37 (17%) | 59 (13%) | 30 (15%) | 68 (15%) | 0.6 |
| Intervals | Time, d |
|---|---|
| 1st abnormal imaging to 1st treatment (n = 864) | 80 (0–384) |
| 1st appointment with specialist to 1st treatment (n = 861) | 57 (0–249) |
| Radiation referral to first radiation treatment (n = 188) | 29 (0–211) |
| 1st appointment with specialist to surgery (n = 304) | 76 (6–285) |
| Diagnosis * to 1st treatment (n = 712) | 31 (0–185) |
| Diagnosis to surgery (n = 180) | 45 (0–185) |
| Diagnosis to definitive radiation (n = 92) | 40 (3–168) |
| Diagnosis to definitive chemoradiation (n = 107) | 30 (0–118) |
| Diagnosis to systemic treatment (n = 333) | 21 (0–138) |
| Pathology result to biomarkers result (n = 378) | 14 (0–231) |
| Wait Times | n | Follow-Up | Unadjusted HR (95% CI) | p-Value | Adjusted HR (95% CI) † | p-Value |
|---|---|---|---|---|---|---|
| 1st abnormal imaging to 1st treatment | 776 | ≤60 days >60 days | 0.97 (0.96–0.98) 0.99 (0.99–0.99) | <0.0001 <0.0001 | 0.98 (0.97–0.99) 1.00 (1.00–1.00) | 0.002 0.8 |
| 1st appointment with specialist to 1st treatment | 767 | ≤60 days >60 days | 0.96 (0.95–0.98) 0.99 (0.99–0.99) | <0.0001 <0.0001 | 0.98 (0.96–0.99) 1.00 (1.00–1.00) | 0.001 0.2 |
| Diagnosis * to 1st treatment | 645 | ≤60 days >60 days | 0.92 (0.88–0.95) 0.99 (0.98–0.99) | <0.0001 <0.0001 | 0.93 (0.89–0.97) 1.00 (1.00–1.00) | 0.0002 0.9 |
| Pathology result to biomarkers result | 339 | ≤60 days >60 days | 0.95 (0.90–1.01) 1.00 (0.99–1.00) | 0.07 0.4 | 0.95 (0.90–1.01) 1.00 (1.00–1.01) | 0.1 0.7 |
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age | 1.01 (1.00–1.02) | 0.09 | 1.01 (1.00–1.03) | 0.03 |
| Female sex (vs. male) | 0.76 (0.63–0.91) | 0.003 | 0.66 (0.58–0.88) | 0.002 |
| Ever-smoker (vs. never) | 1.15 (0.77–1.71) | 0.5 | ||
| ECOG performance status (vs. 0) | ||||
| 1 | 2.76 (2.19–3.48) | <0.0001 | 1.38 (1.07–1.78) | 0.01 |
| 2 | 4.30 (3.29–5.63) | <0.0001 | 1.77 (1.31–2.38) | 0.0002 |
| 3 | 8.40 (5.61–12.6) | <0.0001 | 2.63 (1.63–4.24) | <0.0001 |
| Healthcare network (vs. IUCPQ) | ||||
| CHUM | 1.00 (0.81–1.25) | 1.0 | ||
| CUSM | 1.04 (0.78–1.37) | 0.5 | ||
| Alliance Estrie-Montérégie | 1.03 (0.78–1.37) | 1.0 | ||
| Histology and stage (vs. NSCLC stage I) | ||||
| NSCLC stage II | 2.03 (1.24–3.34) | 0.005 | 2.11 (1.22–3.66) | 0.008 |
| NSCLC stage III | 5.73 (3.97–8.27) | <0.0001 | 3.92 (2.40–6.41) | <0.0001 |
| NSCLC stage IV | 9.20 (6.50–13.02) | <0.0001 | 3.61 (1.96–6.65) | <0.0001 |
| LS-SCLC | 8.04 (4.89–13.23) | <0.0001 | 4.44 (2.31–8.54) | <0.0001 |
| ES-SCLC | 13.78 (9.32–20.38) | <0.0001 | 4.46 (2.35–8.47) | <0.0001 |
| Treatment (vs. surgery) | ||||
| Definitive radiation * | 2.71 (1.81–4.07) | <0.0001 | 1.67 (1.05–2.66) | 0.03 |
| Definitive chemoradiation | 4.40 (3.07–6.31) | <0.0001 | 1.61 (0.99–2.62) | 0.06 |
| Palliative systemic treatment | 8.49 (6.37–11.31) | <0.0001 | 2.92 (1.70–4.99) | <0.0001 |
| Wait times ** | ||||
| 1st abnormal imaging to 1st treatment | ||||
| ≤60 days | 0.97 (0.96–0.98) | <0.0001 | ||
| >60 days | 0.99 (0.99–0.99) | <0.0001 | ||
| 1st appointment with specialist to 1st treatment | ||||
| ≤60 days | 0.96 (0.95–0.98) | <0.0001 | ||
| >60 days | 0.99 (0.99–0.99) | <0.0001 | ||
| Diagnosis † to 1st treatment | ||||
| ≤60 days | 0.92 (0.88–0.95) | <0.0001 | 0.93 (0.89–0.97) | 0.0002 |
| >60 days | 0.99 (0.98–0.99) | <0.0001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denault, M.-H.; Labbé, C.; St-Pierre, C.; Fournier, B.; Gagné, A.; Morillon, C.; Joubert, P.; Simard, S.; Martel, S. Wait Times and Survival in Lung Cancer Patients across the Province of Quebec, Canada. Curr. Oncol. 2022, 29, 3187-3199. https://doi.org/10.3390/curroncol29050259
Denault M-H, Labbé C, St-Pierre C, Fournier B, Gagné A, Morillon C, Joubert P, Simard S, Martel S. Wait Times and Survival in Lung Cancer Patients across the Province of Quebec, Canada. Current Oncology. 2022; 29(5):3187-3199. https://doi.org/10.3390/curroncol29050259
Chicago/Turabian StyleDenault, Marie-Hélène, Catherine Labbé, Carolle St-Pierre, Brigitte Fournier, Andréanne Gagné, Claudia Morillon, Philippe Joubert, Serge Simard, and Simon Martel. 2022. "Wait Times and Survival in Lung Cancer Patients across the Province of Quebec, Canada" Current Oncology 29, no. 5: 3187-3199. https://doi.org/10.3390/curroncol29050259
APA StyleDenault, M.-H., Labbé, C., St-Pierre, C., Fournier, B., Gagné, A., Morillon, C., Joubert, P., Simard, S., & Martel, S. (2022). Wait Times and Survival in Lung Cancer Patients across the Province of Quebec, Canada. Current Oncology, 29(5), 3187-3199. https://doi.org/10.3390/curroncol29050259








