Psychological Problems among Head and Neck Cancer Patients in Relation to Utilization of Healthcare and Informal Care and Costs in the First Two Years after Diagnosis
Abstract
:1. Introduction
2. Materials & Methods
2.1. Patients and Procedure
2.2. Outcome Measures
2.3. Statistical Analysis
3. Results
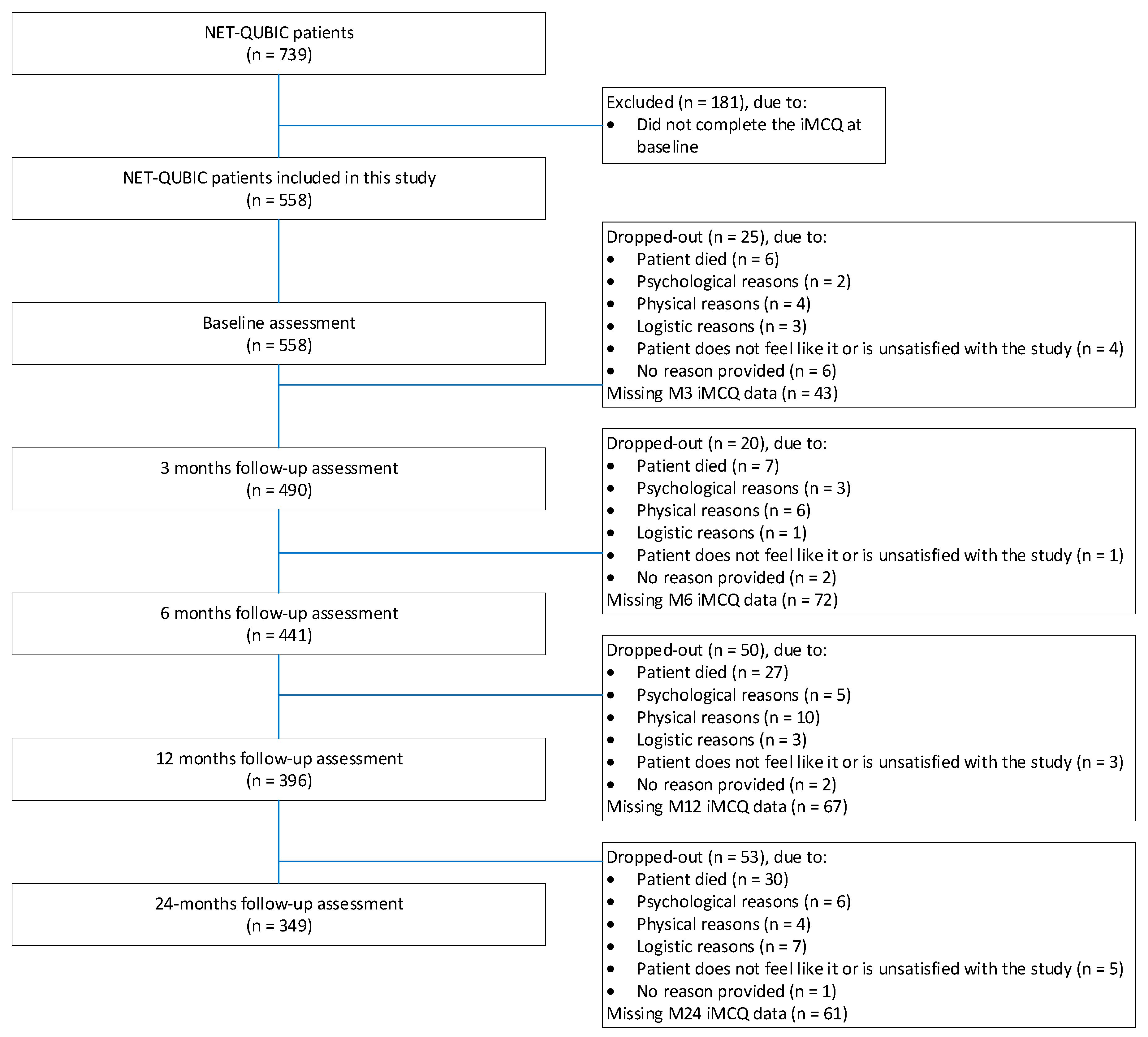
3.1. Study Population
3.2. Use of Healthcare and Informal Care
3.3. Psychological Problems in Relation to Use of Healthcare and Informal Care
3.4. Psychological Problems in Relation to Costs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Distress | Symptoms of Anxiety | Symptoms of Depression | Fear of Cancer Recurrence | Anxiety Disorder | Depression Disorder | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| % Patients Using Service | % Patients Using Service | % Patients Using Service | % Patients Using Service | % Patients Using Service | % Patients Using Service | |||||||
| Baseline (N = 558) | (N = 206) | (N = 408) | (N = 146) | (N = 408) | (N = 80) | (N = 476) | (N = 251) | (N = 307) | (N = 11) | (N = 439) | (N = 14) | (N = 435) |
| Mental healthcare | 5% | 2% | 5.5% | 3% | 6% | 3% | 4% | 3% | 9% | 3% | 21% | 3% |
| General practitioner | 93% | 91% | 96% | 90% | 92% | 92% | 94% | 90% | 91% | 92% | 100% | 92% |
| Other supportive care | 66% | 53% | 67% | 54% | 56% | 58% | 62% | 55% | 45% | 56% | 36% | 57% |
| Informal care | 17% | 10% | 16% | 12% | 21% | 11% | 14% | 11% | 18% | 12% | 0% | 12% |
| 3-month follow-up (N = 490) | (N = 173) | (N = 314) | (N = 124) | (N = 363) | (N = 65) | (N = 423) | (N = 220) | (N = 256) | (N = 8) | (N = 396) | (N = 10) | (N = 393) |
| Mental healthcare | 13% | 6% | 16% | 6% | 14% | 8% | 11% | 6% | 25% | 7% | 30% | 7% |
| General practitioner | 77% | 76% | 77% | 76% | 83% | 75% | 79% | 73% | 100% | 75% | 90% | 75% |
| Other supportive care | 81% | 79% | 87% | 76% | 74% | 81% | 86% | 75% | 100% | 79% | 80% | 80% |
| Informal care | 30% | 21% | 32% | 21% | 37% | 22% | 28% | 20% | 63% | 23% | 30% | 24% |
| 6-month follow-up (N = 441) | (N = 160) | (N = 278) | (N = 117) | (N = 321) | (N = 62) | (N = 377) | (N = 196) | (N = 233) | (N = 6) | (N = 355) | (N = 10) | (N = 351) |
| Mental healthcare | 11% | 5% | 14% | 5% | 15% | 6% | 11% | 5% | 33% | 7% | 40% | 6% |
| General practitioner | 71% | 63% | 74% | 63% | 68% | 66% | 69% | 64% | 100% | 66% | 70% | 66% |
| Other supportive care | 71% | 70% | 74% | 69% | 69% | 71% | 75% | 67% | 83% | 71% | 70% | 71% |
| Informal care | 23% | 13% | 23% | 15% | 36% | 14% | 20% | 14% | 33% | 16% | 100% | 16% |
| 12-month follow-up (N = 396) | (N = 136) | (N = 257) | (N = 97) | (N = 296) | (N = 54) | (N = 340) | (N = 173) | (N = 213) | (N = 6) | (N = 316) | (N = 8) | (N = 314) |
| Mental healthcare | 11% | 6% | 12% | 6% | 9% | 8% | 10% | 5% | 0% | 6% | 13% | 5% |
| General practitioner | 65% | 52% | 67% | 53% | 63% | 56% | 63% | 52% | 83% | 56% | 63% | 56% |
| Other supportive care | 61% | 60% | 61% | 60% | 56% | 61% | 61% | 59% | 83% | 59% | 50% | 60% |
| Informal care | 14% | 12% | 14% | 12% | 20% | 12% | 15% | 11% | 0% | 11% | 0% | 12% |
| 24-month follow-up (N = 349) | (N = 114) | (N = 232) | (N = 82) | (N = 264) | (N = 40) | (N = 307) | (N = 151) | (N = 191) | (N = 5) | (N = 283) | (N = 7) | (N = 281) |
| Mental healthcare | 6% | 3% | 7% | 3% | 5% | 4% | 5% | 3% | 20% | 4% | 0% | 4% |
| General practitioner | 63% | 57% | 66% | 57% | 55% | 60% | 58% | 60% | 100% | 60% | 57% | 61% |
| Other supportive care | 65% | 48% | 67% | 49% | 65% | 52% | 60% | 48% | 80% | 51% | 43% | 52% |
| Informal care | 12% | 8% | 15% | 8% | 10% | 9% | 10% | 8% | 0% | 8% | 0% | 8% |
Appendix B
| Distress | Symptoms of Anxiety | Symptoms of Depression | Fear of Cancer Recurrence | Depression Disorder | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| % Patients Using Service | % Patients Using Service | % Patients Using Service | % Patients Using Service | % Patients Using Service | ||||||
| 12-month follow-up (N = 396) | (N = 54) | (N = 263) | (N = 29) | (N = 289) | (N = 29) | (N = 292) | (N = 98) | (N = 244) | (N = 22) | (N = 301) |
| Mental healthcare | 20% | 4% | 31% | 5% | 17% | 6% | 11% | 5% | 18% | 6% |
| General practitioner | 65% | 53% | 76% | 53% | 69% | 54% | 59% | 55% | 59% | 56% |
| Other supportive care | 63% | 60% | 66% | 60% | 69% | 60% | 62% | 59% | 64% | 60% |
| Informal care | 22% | 10% | 17% | 11% | 24% | 11% | 14% | 12% | 14% | 10% |
| 24-month follow-up (N = 349) | (N = 40) | (N = 233) | (N = 22) | (N = 252) | (N = 19) | (N = 257) | (N = 81) | (N = 212) | (N = 16) | (N = 281) |
| Mental healthcare | 8% | 3% | 14% | 3% | 11% | 4% | 7% | 3% | 19% | 3% |
| General practitioner | 70% | 58% | 73% | 59% | 74% | 59% | 63% | 58% | 63% | 61% |
| Other supportive care | 58% | 51% | 64% | 51% | 58% | 52% | 64% | 49% | 56% | 51% |
| Informal care | 13% | 8% | 23% | 8% | 11% | 9% | 7% | 9% | 31% | 8% |
References
- Buchmann, L.; Ashby, S.; Cannon, R.B.; Hunt, J.P. Psychosocial distress in patients with thyroid cancer. Otolaryngol. -Head Neck Surg. 2015, 152, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.T.; Zhong, W.N.; Jiang, Y. Measurement of distress and its alteration during treatment in patients with nasopharyngeal carcinoma. Head Neck 2014, 36, 1077–1086. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.; Pandey, S.; Salins, N.; Deodhar, J.; Patil, V.; Gupta, T.; Laskar, S.G.; Budrukkar, A.; Murthy, V.; Joshi, A.; et al. Distress Screening in Head and Neck Cancer Patients Planned for Cancer-Directed Radiotherapy. Laryngoscope 2021, 131, 2023–2029. [Google Scholar] [CrossRef] [PubMed]
- Neilson, K.; Pollard, A.; Boonzaier, A.; Corry, J.; Castle, D.; Smith, D.; Trauer, T.; Couper, J. A longitudinal study of distress (depression and anxiety) up to 18 months after radiotherapy for head and neck cancer. Psycho-Oncology 2013, 22, 1843–1848. [Google Scholar] [CrossRef]
- Van Beek, F.; Jansen, F.; Mak, L.; Lissenberg-Witte, B.; Buter, J.; Vergeer, M.; Voortman, J.; Cuijpers, P.; Leemans, C.; Verdonck-de Leeuw, I. The course of symptoms of anxiety and depression from time of diagnosis up to 2 years follow-up in head and neck cancer patients treated with primary (chemo) radiation. Oral Oncol. 2020, 102, 104576. [Google Scholar] [CrossRef]
- Wu, Y.-S.; Lin, P.-Y.; Chien, C.-Y.; Fang, F.-M.; Chiu, N.-M.; Hung, C.-F.; Lee, Y.; Chong, M.-Y. Anxiety and depression in patients with head and neck cancer: 6-month follow-up study. Neuropsychiatr. Dis. Treat. 2016, 12, 1029. [Google Scholar] [CrossRef] [Green Version]
- Hammerlid, E.; Ahlner-Elmqvist, M.; Bjordal, K.; Biörklund, A.; Evensen, J.; Boysen, M.; Jannert, M.; Kaasa, S.; Sullivan, M.; Westin, T. A prospective multicentre study in Sweden and Norway of mental distress and psychiatric morbidity in head and neck cancer patients. Br. J. Cancer 1999, 80, 766–774. [Google Scholar] [CrossRef] [Green Version]
- Hammerlid, E.; Silander, E.; Hörnestam, L.; Sullivan, M. Health-related quality of life three years after diagnosis of head and neck cancer—a longitudinal study. Head Neck J. Sci. Spec. Head Neck 2001, 23, 113–125. [Google Scholar] [CrossRef]
- Lydiatt, W.M.; Moran, J.; Burke, W.J. A review of depression in the head and neck cancer patient. Clin. Adv. Hematol. Oncol. 2009, 7, 397–403. [Google Scholar]
- Mehnert, A.; Brähler, E.; Faller, H.; Härter, M.; Keller, M.; Schulz, H.; Wegscheider, K.; Weis, J.; Boehncke, A.; Hund, B. Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J. Clin. Oncol. 2014, 32, 3540–3546. [Google Scholar] [CrossRef]
- Mirosevic, S.; Thewes, B.; van Herpen, C.; Kaanders, J.; Merkx, T.; Humphris, G.; Baatenburg de Jong, R.J.; Langendijk, J.A.; Leemans, C.R.; Terhaard, C.H. Prevalence and clinical and psychological correlates of high fear of cancer recurrence in patients newly diagnosed with head and neck cancer. Head Neck 2019, 41, 3187–3200. [Google Scholar] [CrossRef] [PubMed]
- Dunne, S.; Mooney, O.; Coffey, L.; Sharp, L.; Desmond, D.; Timon, C.; O’Sullivan, E.; Gallagher, P. Psychological variables associated with quality of life following primary treatment for head and neck cancer: A systematic review of the literature from 2004 to 2015. Psycho-Oncology 2017, 26, 149–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlson, L.E.; Bultz, B.D. Efficacy and medical cost offset of psychosocial interventions in cancer care: Making the case for economic analyses. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2004, 13, 837–849. [Google Scholar] [CrossRef] [PubMed]
- Van Beek, F.E.; Wijnhoven, L.M.; Holtmaat, K.; Custers, J.A.; Prins, J.B.; Verdonck-de Leeuw, I.M.; Jansen, F. Psychological problems among cancer patients in relation to healthcare and societal costs: A systematic review. Psycho-Oncology 2021, 30, 1801–1835. [Google Scholar] [CrossRef]
- Williams, J.T.W.; Pearce, A. A systematic review of fear of cancer recurrence related healthcare use and intervention cost-effectiveness. Psycho-Oncology 2021, 30, 1185–1195. [Google Scholar] [CrossRef]
- Kuhnt, S.; Brähler, E.; Faller, H.; Härter, M.; Keller, M.; Schulz, H.; Wegscheider, K.; Weis, J.; Boehncke, A.; Hund, B. Twelve-month and lifetime prevalence of mental disorders in cancer patients. Psychother. Psychosom. 2016, 85, 289–296. [Google Scholar] [CrossRef]
- Jeffery, D.D.; Art Ambrosio, L.; Hopkins, L.; Burke, H.B. Mental health comorbidities and cost/utilization outcomes in head and neck cancer patients. J. Psychosoc. Oncol. 2019, 37, 301–318. [Google Scholar] [CrossRef]
- Laurence, B.; Mould-Millman, N.K.; Nero Jr, K.E.; Salter, R.O.; Sagoo, P.K. Depression and hospital admission in older patients with head and neck cancer: Analysis of a national healthcare database. Gerodontology 2017, 34, 284–287. [Google Scholar] [CrossRef]
- Verdonck-de Leeuw, I.; Jansen, F.; Brakenhoff, R.; Langendijk, J.; Takes, R.; Terhaard, C.; de Jong, R.B.; Smit, J.; Leemans, C. Advancing interdisciplinary research in head and neck cancer through a multicenter longitudinal prospective cohort study: The NETherlands QUality of life and BIomedical Cohort (NET-QUBIC) data warehouse and biobank. BMC Cancer 2019, 19, 765. [Google Scholar]
- Paleri, V.; Wight, R. Applicability of the adult comorbidity evaluation–27 and the Charlson indexes to assess comorbidity by notes extraction in a cohort of United Kingdom patients with head and neck cancer: A retrospective study. J. Laryngol. Otol. 2002, 116, 200–205. [Google Scholar] [CrossRef]
- Spinhoven, P.; Ormel, J.; Sloekers, P.; Kempen, G.; Speckens, A.E.; van Hemert, A.M. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol. Med. 1997, 27, 363–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Custers, J.A.; van den Berg, S.W.; van Laarhoven, H.W.; Bleiker, E.M.; Gielissen, M.F.; Prins, J.B. The cancer worry scale: Detecting fear of recurrence in breast cancer survivors. Cancer Nurs. 2014, 37, E44–E50. [Google Scholar] [CrossRef] [PubMed]
- Custers, J.A.; Gielissen, M.F.; Janssen, S.H.; de Wilt, J.H.; Prins, J.B. Fear of cancer recurrence in colorectal cancer survivors. Support. Care Cancer 2016, 24, 555–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van de Wal, M.; van Oort, I.; Schouten, J.; Thewes, B.; Gielissen, M.; Prins, J. Fear of cancer recurrence in prostate cancer survivors. Acta Oncol. 2016, 55, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Wittchen, H.-U. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. J. Psychiatr. Res. 1994, 28, 57–84. [Google Scholar] [CrossRef]
- Bouwmans, C.; Hakkaart-van Rooijen, L.; Koopmanschap, M.; Krol, M.; Severens, H.; Brouwer, W. Guideline iMTA Medical Consumption Questionnaire; iMTA, Erasmus Universiteit: Rotterdam, The Netherlands, 2013. [Google Scholar]
- Bouwmans, C.; Krol, M.; Severens, H.; Koopmanschap, M.; Brouwer, W.; Hakkaart-van Roijen, L. The iMTA productivity cost questionnaire: A standardized instrument for measuring and valuing health-related productivity losses. Value Health 2015, 18, 753–758. [Google Scholar] [CrossRef] [Green Version]
- Hakkaart-Van Rooijen, L.; Tan, S.; Bouwmans, C. Handleiding voor Kostenonderzoek, Methoden en Standaardprijzen voor Ecenomische Valuaties in de Gezondheidszorg; Erasmus Universiteit Rotterdam: Rotterdam, The Netherlands, 2010. [Google Scholar]
- Elliot, R.; Payne, K. Statistical handling of data in economic analysis. In Essentials of Economic Evaluation in Healthcare; Pharmaceutical Press: London, UK, 2005; pp. 185–202. [Google Scholar]
- Jansen, F.; Brakenhoff, R.H.; Baatenburg de Jong, R.J.; Langendijk, J.A.; Leemans, C.R.; Takes, R.P.; Terhaard, C.H.; Smit, J.H.; Verdonck-de Leeuw, I.M. Study retention and attrition in a longitudinal cohort study including patient-reported outcomes, fieldwork and biobank samples: Results of the Netherlands quality of life and Biomedical cohort study (NET-QUBIC) among 739 head and neck cancer patients and 262 informal caregivers. BMC Med. Res. Methodol. 2022, 22, 27. [Google Scholar]
- Pan, X.; Sambamoorthi, U. Health care expenditures associated with depression in adults with cancer. J. Community Support. Oncol. 2015, 13, 240. [Google Scholar] [CrossRef] [Green Version]
- Boele, F.W.; Meads, D.; Jansen, F.; Verdonck-de Leeuw, I.M.; Heimans, J.J.; Reijneveld, J.C.; Short, S.C.; Klein, M. Healthcare utilization and productivity loss in glioma patients and family caregivers: The impact of treatable psychological symptoms. J. Neuro.-Oncol. 2020, 147, 485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mausbach, B.T.; Decastro, G.; Schwab, R.B.; Tiamson-Kassab, M.; Irwin, S.A. Healthcare use and costs in adult cancer patients with anxiety and depression. Depress. Anxiety 2020, 37, 908–915. [Google Scholar] [CrossRef] [PubMed]
- de Leeuw, J.R.J.; de Graeff, A.; Ros, W.J.; Blijham, G.H.; Hordijk, G.J.; Winnubst, J.A. Prediction of depression 6 months to 3 years after treatment of head and neck cancer. Head Neck J. Sci. Spec. Head Neck 2001, 23, 892–898. [Google Scholar] [CrossRef] [PubMed]
- Brebach, R.; Sharpe, L.; Costa, D.S.; Rhodes, P.; Butow, P. Psychological intervention targeting distress for cancer patients: A meta-analytic study investigating uptake and adherence. Psycho-Oncology 2016, 25, 882–890. [Google Scholar] [CrossRef] [Green Version]
- Van Beek, F.; Wijnhoven, L.; Custers, J.; Holtmaat, K.; De Rooij, B.; Horevoorts, N.; Aukema, E.; Verheul, S.; Eerenstein, S.; Strobbe, L. Adjustment disorder in cancer patients after treatment: Prevalence and acceptance of psychological treatment. Support. Care Cancer 2021, 30, 1797–1806. [Google Scholar] [CrossRef]
- Kissane, D.W. Unrecognised and untreated depression in cancer care. Lancet. Psychiatry 2014, 1, 320–321. [Google Scholar] [CrossRef]
- Armstrong, R.A. When to use the Bonferroni correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef]
- Walker, E.R.; Cummings, J.R.; Hockenberry, J.M.; Druss, B.G. Insurance status, use of mental health services, and unmet need for mental health care in the United States. Psychiatr. Serv. 2015, 66, 578–584. [Google Scholar] [CrossRef]
| Excluded Patients (n = 181) | Included Patients 2 (n = 558) | p-Value | |
|---|---|---|---|
| Mean age (SD) | 62 (11) | 64 (9) | 0.07 |
| Women | 43 (24%) | 147 (26%) | 0.49 |
| Living alone | 57 (43%) | 106 (21%) | <0.01 |
| Education level 1 | |||
| Low | 64 (48%) | 215 (42%) | 0.13 |
| Middle | 37 (28%) | 134 (26%) | |
| High | 31 (24%) | 167 (32%) | |
| Tumor site | |||
| Oral cavity | 43 (24%) | 156 (28%) | 0.36 |
| Oropharynx | 63 (35%) | 199 (36%) | |
| HPV positive | 26 (41%) | 104 (52%) | |
| HPV negative | 30 (48%) | 69 (35%) | |
| HPV unknown | 7 (11%) | 26 (13%) | |
| Hypopharynx | 18 (10%) | 34 (6%) | |
| Larynx | 53 (29%) | 152 (27%) | |
| Unknown primary | 4 (2%) | 17 (3%) | |
| Clinical tumor stage 3 | |||
| 0/I/II | 57 (31%) | 238 (43%) | 0.01 |
| III/IV | 124 (69%) | 320 (57%) | |
| Treatment | |||
| Surgery | 36 (20%) | 116 (21%) | 0.37 |
| Radiotherapy | 56 (31%) | 185 (33%) | |
| Chemoradiotherapy | 62 (34%) | 153 (27%) | |
| Surgery and radiotherapy | 20 (11%) | 86 (15%) | |
| Surgery and chemoradiotherapy | 6 (3%) | 17 (3%) | |
| WHO performance status | |||
| 0 | 112 (62%) | 395 (71%) | 0.03 |
| 1 or more | 69 (38%) | 163 (29%) | |
| ACE-27 comorbidity | |||
| None/mild | 97 (58%) | 371 (70%) | <0.01 |
| Moderate/severe | 71 (42%) | 160 (30%) | |
| Psychological outcomes at baseline | |||
| High level of distress (HADS-T ≥ 11) | 206 (37%) | ||
| Symptoms of anxiety (HADS-A ≥ 8) | 146 (26%) | ||
| Symptoms of depression (HADS-D ≥ 8) | 80 (14%) | ||
| High level of fear of recurrence (CWS ≥ 14) | 251 (46%) | ||
| Anxiety disorder | 11 (2%) | ||
| Depression disorder | 14 (3%) |
| Baseline (N = 558) | 3-Month Follow-Up (N = 490) | 6-Month Follow-Up (N = 441) | 12-Month Follow-Up (N = 396) | 24-Month Follow-Up (N = 349) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % Patients Using Service | Mean Number (SD) of Contacts or Hours * | % Patients Using Service | Mean Number (SD) of Contacts or Hours * | % Patients Using Service | Mean Number (SD) of Contacts or Hours * | % Patients Using Service | Mean Number (SD) of Contacts or Hours * | % Patients Using Service | Mean Number (SD) of Contacts or Hours * | |
| Mental healthcare | 3% | 4.4 (6.4) | 8% | 2.9 (2.7) | 8% | 4.1 (3.5) | 8% | 3.0 (2.8) | 4% | 4.1 (3.8) |
| Primary care | 92% | 3.8 (3.3) | 76% | 4.2 (4.3) | 66% | 3.6 (4.5) | 57% | 3.3 (2.6) | 59% | 4.5 (20.7) |
| Supportive care | 58% | 4.3 (6.2) | 80% | 7.8 (9.2) | 71% | 9.0 (12.4) | 60% | 7.7 (11.5) | 54% | 7.06 (12.2) |
| Social work | 4% | 3.5 (4.7) | 4% | 6.8 (5.7) | 5% | 1.7 (1.6) | 4% | 3.4 (4.7) | 4% | 10.1 (12.1) |
| Physical therapy | 13% | 8.3 (8.0) | 22% | 8.1 (6.3) | 32% | 11.7 (10.9) | 26% | 10.4 (10.4) | 25% | 6.2 (13.0) |
| Support group | 1% | 12.3 (8.2) | 4% | 6.9 (5.8) | 5% | 19.4 (15.8) | 4% | 14.8 (11.4) | 2% | 10.75 (10.7) |
| Dietitian | 27% | 1.4 (1.3) | 56% | 3.0 (3.5) | 27% | 1.9 (1.6) | 12% | 2.0 (1.7) | 8% | 1.6 (0.9) |
| Speech therapy | 9% | 2.1 (2.1) | 18% | 2.8 (5.6) | 16% | 3.3 (3.8) | 11% | 4.9 (6.1) | 6% | 5.7 (6.7) |
| Oral care | 38% | 1.3 (0.7) | 52% | 3.5 (6.1) | 39% | 1.5 (1.2) | 34% | 1.3 (0.9) | 28% | 1.2 (1.0) |
| Informal care | 13% | 29.3 (39.4) | 24% | 61.0 (97.2) | 17% | 46.9 (90.4) | 13% | 49.2 (63.9) | 9% | 57.6 (74.7) |
| Baseline (N = 558) | 3-Month Follow-Up (N = 490) | 6-Month Follow-Up (N = 441) | 12-Month Follow-Up (N = 396) | 24-Month Follow-Up (N = 396) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | ||
| Measured at baseline | |||||||||||
| Distress | Mental healthcare | N/A | N/A | N/A | |||||||
| Primary care | 1.74 (1.13–2.67) | 0.01 | |||||||||
| Supportive care | 1.59 (1.09–2.32) | 0.02 | 1.78 (1.11–2.87) | 0.02 | |||||||
| Informal care | 1.48 (0.86–2.53) | 0.16 | 1.36 (0.85–2.18) | 0.20 | |||||||
| Symptoms of anxiety | Mental healthcare | N/A | N/A | ||||||||
| Primary care | 2.54 (1.05–6.11) | 0.04 | 1.61 (0.99–2.62) | 0.057 | 1.77 (1.10–2.87) | 0.02 | |||||
| Supportive care | 1.55 (1.02–2.36) | 0.04 | 1.98 (1.07–3.67) | 0.03 | 1.99 (1.17–3.36) | 0.01 | |||||
| Informal care | 1.57 (0.94–2.60) | 0.08 | 1.27 (0.70–2.31) | 0.440 | |||||||
| Symptoms of depression | Mental healthcare | N/A | |||||||||
| Primary care | 1.54 (0.75–3.16) | 0.24 | |||||||||
| Supportive care | |||||||||||
| Informal care | 1.68 (0.87–3.23) | 0.12 | 1.62 (0.89–2.95) | 0.12 | 2.58 (1.34–4.97) | 0.005 | |||||
| Fear of cancer recurrence | Mental healthcare | N/A | N/A | ||||||||
| Primary care | 1.60 (1.06–2.40) | 0.03 | |||||||||
| Supportive care | 1.64 (1.00–2.70) | 0.05 | 1.47 (0.94–2.29) | 0.09 | |||||||
| Informal care | 1.71 (1.06–2.76) | 0.03 | |||||||||
| Anxiety disorder | Mental healthcare | N/A | |||||||||
| Primary care | |||||||||||
| Supportive care | |||||||||||
| Informal care | 4.76 (1.04–21.81) | 0.045 | |||||||||
| Depression disorder | Mental healthcare | N/A | N/A | N/A | |||||||
| Primary care | |||||||||||
| Supportive care | |||||||||||
| Informal care | |||||||||||
| Measured at 12-months follow-up | |||||||||||
| Distress | Mental healthcare | N/A | |||||||||
| Primary care | |||||||||||
| Supportive care | |||||||||||
| Informal care | 2.08 (0.88–4.92) | 0.10 | |||||||||
| Symptoms of anxiety | Mental healthcare | N/A | N/A | ||||||||
| Primary care | 2.71 (1.11-6.62) | 0.03 | |||||||||
| Supportive care | |||||||||||
| Informal care | 2.90 (0.84-10.06) | 0.09 | |||||||||
| Symptoms of depression | Mental healthcare | ||||||||||
| Primary care | |||||||||||
| Supportive care | |||||||||||
| Informal care | |||||||||||
| Fear of cancer recurrence | Mental healthcare | ||||||||||
| Primary care | |||||||||||
| Supportive care | 1.74 (1.01-2.98) | 0.04 | |||||||||
| Informal care | |||||||||||
| Depression disorder | Mental healthcare | N/A | N/A | ||||||||
| Primary care | |||||||||||
| Supportive care | |||||||||||
| Informal care | 6.42 (1.64-9.81) | 0.01 | |||||||||
| Baseline | 3-Month Follow-Up | 6-Month Follow-Up | 12-Month Follow-Up | 24-Month Follow-Up | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (95% BCa CI) | % * | Mean (95% BCa CI) | % * | Mean (95% BCa CI) | % * | Mean (95% BCa CI) | % * | Mean (95% BCa CI) | % * | |
| Measured at baseline | ||||||||||
| Distress | €93 (18; 180) | 99.1% | €21 (−230; 214) | 58.7% | €−58 (−283; 90) | 28.2% | €−5 (−158; 141) | 48.7% | €100 (−105; 534) | 74.1% |
| Symptoms of anxiety | €125 (45; 231) | 99.7% | €−40 (−252; 203) | 34.5% | €−83 (−291; 81) | 19.1% | €−15 (−166; 149) | 42.6% | €−12 (−248; 182) | 45.3% |
| Symptoms of depression | €49 (−79; 215) | 76.1% | €24 (−203; 311) | 56.3% | €−85 (268; 145) | 20.3% | €−30 (−194; 196) | 36.1% | €−104 (−328; 168) | 19.9% |
| Fear of cancer recurrence | €80 (10; 162) | 98.3% | €−66 (−273; 98) | 24.5% | €−18 (−194; 127) | 42.6% | €94 (−58; 276) | 87.8% | €4 (−185; 141) | 52.4% |
| Anxiety disorder | €−68 (−277; 141) | 26.1% | €393 (−301; 2706) | 69.1% | €418 (−128; 1391) | 89.3% | €262 (−149; 1086) | 82.1% | €−167 (−847; 177) | 23.6% |
| Depression disorder | €89 (−156; 646) | 68.2% | €547 (−41; 2077) | 91.1% | €388 (−108; 1238) | 89.9% | €422 (−21; 1045) | 95.1% | €−284 (−705; 36) | 5.2% |
| Measured at 12-months follow-up | ||||||||||
| Distress | €166 (−58; 477) | 89.6% | €−33 (−247; 215) | 37.0% | ||||||
| Symptoms of anxiety | €42 (−161; 406) | 60.8% | €124 (−167; 570) | 75.1% | ||||||
| Symptoms of depression | €165 (−85; 660) | 82.7% | €20 (−196; 574) | 51.0% | ||||||
| Fear of cancer reoccurrence | €89 (−120; 498) | 72.0% | €67 (−118; 236) | 76.3% | ||||||
| Depression disorder | €−81 (−286; 258) | 26.1% | €391 (−188; 1061) | 89.6% | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Beek, F.E.; Jansen, F.; Baatenburg de Jong, R.J.; Langendijk, J.A.; Leemans, C.R.; Smit, J.H.; Takes, R.P.; Terhaard, C.H.J.; Custers, J.A.E.; Prins, J.B.; et al. Psychological Problems among Head and Neck Cancer Patients in Relation to Utilization of Healthcare and Informal Care and Costs in the First Two Years after Diagnosis. Curr. Oncol. 2022, 29, 3200-3214. https://doi.org/10.3390/curroncol29050260
van Beek FE, Jansen F, Baatenburg de Jong RJ, Langendijk JA, Leemans CR, Smit JH, Takes RP, Terhaard CHJ, Custers JAE, Prins JB, et al. Psychological Problems among Head and Neck Cancer Patients in Relation to Utilization of Healthcare and Informal Care and Costs in the First Two Years after Diagnosis. Current Oncology. 2022; 29(5):3200-3214. https://doi.org/10.3390/curroncol29050260
Chicago/Turabian Stylevan Beek, Florie E., Femke Jansen, Rob J. Baatenburg de Jong, Johannes A. Langendijk, C. René Leemans, Johannes H. Smit, Robert P. Takes, Chris H. J. Terhaard, José A. E. Custers, Judith B. Prins, and et al. 2022. "Psychological Problems among Head and Neck Cancer Patients in Relation to Utilization of Healthcare and Informal Care and Costs in the First Two Years after Diagnosis" Current Oncology 29, no. 5: 3200-3214. https://doi.org/10.3390/curroncol29050260
APA Stylevan Beek, F. E., Jansen, F., Baatenburg de Jong, R. J., Langendijk, J. A., Leemans, C. R., Smit, J. H., Takes, R. P., Terhaard, C. H. J., Custers, J. A. E., Prins, J. B., Lissenberg-Witte, B. I., & Verdonck-de Leeuw, I. M. (2022). Psychological Problems among Head and Neck Cancer Patients in Relation to Utilization of Healthcare and Informal Care and Costs in the First Two Years after Diagnosis. Current Oncology, 29(5), 3200-3214. https://doi.org/10.3390/curroncol29050260






