The Use of Virtual Care in Patients with Hematologic Malignancies: A Scoping Review
Abstract
:1. Introduction
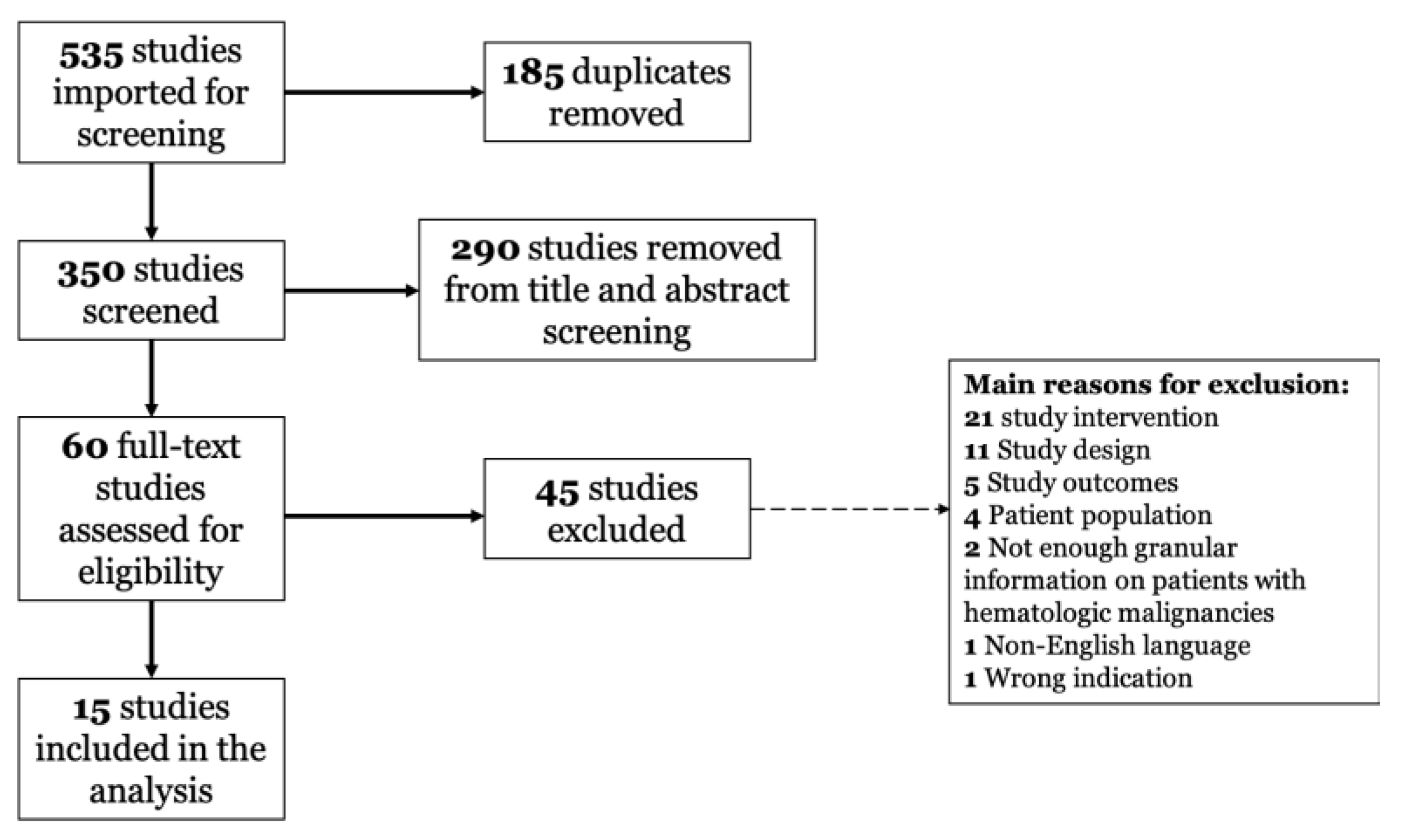
2. Materials and Methods
2.1. Methodology of Scoping Review
2.2. Data Sources and Search Terms
2.3. Article Selection and Data Abstraction
3. Results
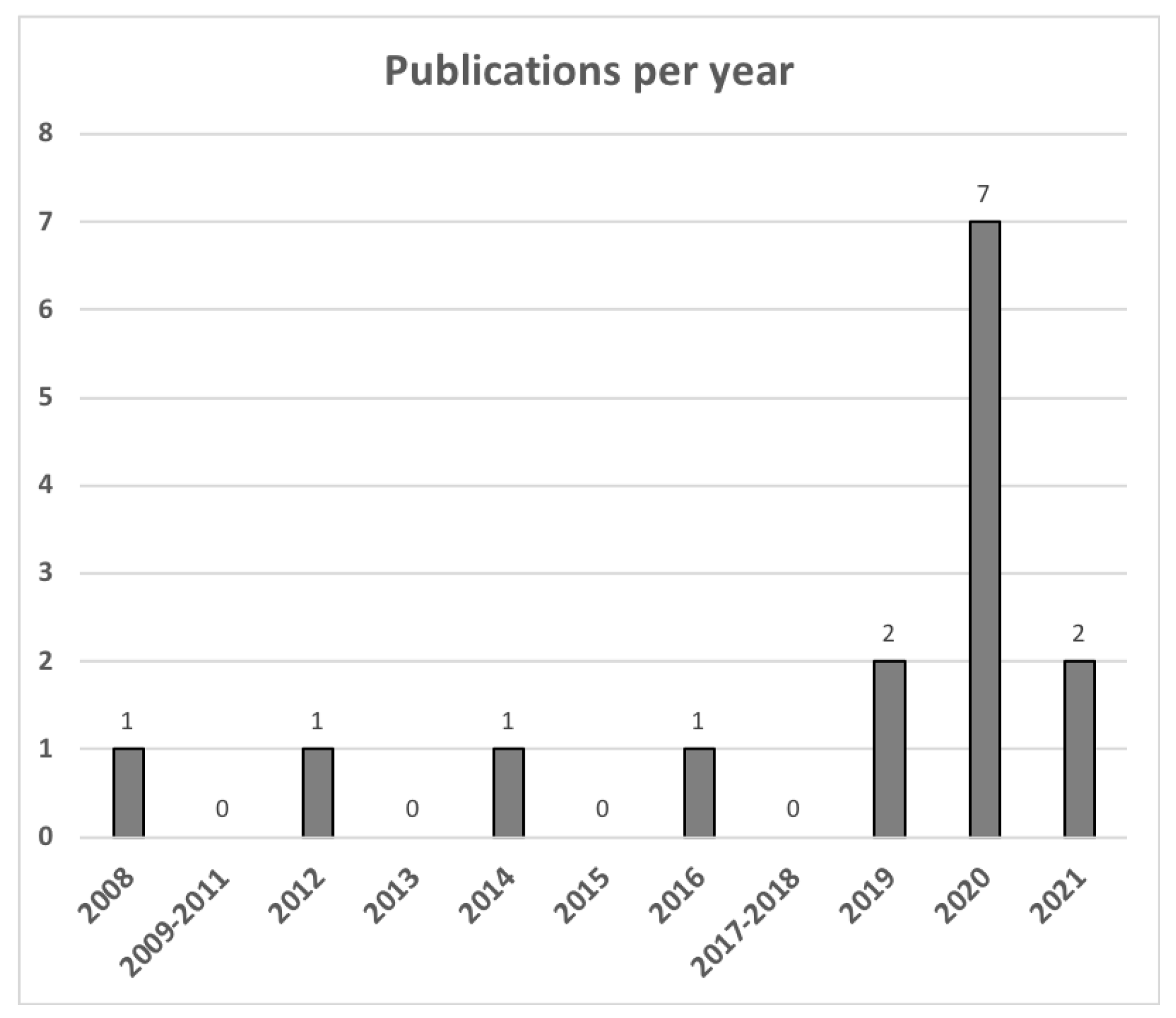
3.1. Publication Demographics
3.2. Use of App-Based Interventions
3.3. Use of Phone Call Interventions
3.4. Use of Video Interventions
3.5. Use of Mixed Interventions
3.6. Virtual Care during the COVID-19 Pandemic
3.7. Satisfaction with Virtual Care
3.7.1. Patient Satisfaction
3.7.2. Provider Satisfaction
3.8. Clinical Outcomes with Virtual Care
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Woolliscroft, J.O. Innovation in Response to the COVID-19 Pandemic Crisis. Acad. Med. J.-Sociation Am. Med. Coll. 2020, 95, 1140–1142. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Informatics Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Bokolo, A., Jr. Use of Telemedicine and Virtual Care for Remote Treatment in Response to COVID-19 Pandemic. J. Med. Syst. 2020, 44, 132. [Google Scholar] [CrossRef] [PubMed]
- Vijenthira, A.; Gong, I.Y.; Fox, T.A.; Booth, S.; Cook, G.; Fattizzo, B.; Martín-Moro, F.; Razanamahery, J.; Riches, J.C.; Zwicker, J.; et al. Outcomes of patients with hematologic malignancies and COVID-19: A systematic review and meta-analysis of 3377 patients. Blood 2020, 136, 2881–2892. [Google Scholar] [CrossRef]
- Wang, Q.; Berger, N.A.; Xu, R. When hematologic malignancies meet COVID-19 in the United States: Infections, death and dis-parities. Blood Rev. 2021, 47, 100775. [Google Scholar] [CrossRef]
- Chen, L.; Payne, J.B.; Dance, K.V.; Imbody, C.B.; Ho, C.D.; Ayers, A.A.; Flowers, C.R. Priorities for Rural Lymphoma Survivors: A Qualitative Study. Clin. Lymphoma Myeloma Leuk. 2020, 20, 47–52.e3. [Google Scholar] [CrossRef] [Green Version]
- Levine, O.H.; McGillion, M.; Levine, M. Virtual Cancer Care During the COVID-19 Pandemic and Beyond: A Call for Evaluation. JMIR Cancer 2020, 6, e24222. [Google Scholar] [CrossRef]
- Abdel-Rahman, O. Patient-related barriers to some virtual healthcare services among cancer patients in the USA: A popula-tion-based study. J. Comp. Eff. Res. 2021, 10, 119–126. [Google Scholar] [CrossRef]
- Lesley, G.C.; Tahmasebi, H.; Meti, N.; Wright, F.C.; Thawer, A.; Cheung, M.; Singh, S. Cancer Treatment During COVID-19: A Qualitative Analysis of Patient-Perceived Risks and Experiences with Virtual Care. J. Patient Exp. 2021, 8, 23743735211039328. [Google Scholar] [CrossRef]
- Berlin, A.; Lovas, M.; Truong, T.; Melwani, S.; Liu, J.; Liu, Z.A.; Badzynski, A.; Carpenter, M.B.; Virtanen, C.; Morley, L.; et al. Implementation and Outcomes of Virtual Care Across a Tertiary Cancer Center During COVID-19. JAMA Oncol. 2021, 7, 597–602. [Google Scholar] [CrossRef]
- Zhang, H.; Cha, E.E.; Lynch, K.; Cahlon, O.; Gomez, D.R.; Shaverdian, N.; Gillespie, E.F. Radiation Oncologist Perceptions of Telemedicine from Consultation to Treatment Planning: A Mixed-Methods Study. Int. J. Radiat. Oncol. 2020, 108, 421–429. [Google Scholar] [CrossRef]
- Ambrosini, F.; Stasio, A.D.; Mantica, G.; Cavalone, B.; Serao, A. COVID-19 pandemic and uro-oncology follow-up: A “virtual” multidisciplinary team strategy and patients’ satisfaction assessment. Arch. Ital. Urol. Androl. 2020, 92. [Google Scholar] [CrossRef]
- Shaverdian, N.; Gillespie, E.F.; Cha, E.; Kim, S.Y.; Benvengo, S.; Chino, F.; Kang, J.J.; Li, Y.; Atkinson, T.M.; Lee, N.; et al. Impact of Telemedicine on Patient Satisfaction and Perceptions of Care Quality in Radiation Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hsiehchen, D.; Muquith, M.; Haque, W.; Espinoza, M.; Yopp, A.; Beg, M.S. Clinical Efficiency and Safety Outcomes of Virtual Care for Oncology Patients During the COVID-19 Pandemic. JCO Oncol. Pr. 2021, 17, e1327–e1332. [Google Scholar] [CrossRef] [PubMed]
- Royce, T.J.; Sanoff, H.K.; Rewari, A. Telemedicine for Cancer Care in the Time of COVID-19. JAMA Oncol. 2020, 6, 1698. [Google Scholar] [CrossRef]
- Rodin, D.; Lovas, M.; Berlin, A. The reality of virtual care: Implications for cancer care beyond the pandemic. Healthcare 2020, 8, 100480. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Applebaum, A.J.; Duhamel, K.N.; Winkel, G.; Rini, C.; Greene, P.B.; Mosher, C.E.; Redd, W.H. Therapeutic alliance in telephone-administered cognitive-behavioral therapy for hematopoietic stem cell transplant survivors. J. Consult. Clin. Psychol. 2012, 80, 811–816. [Google Scholar] [CrossRef] [Green Version]
- Nawas, M.T.; Landau, H.J.; Sauter, C.S.; Featherstone, C.A.; Kenny, S.A.; Rodriguez, E.S.; Johnson, L.G.; Giralt, S.A.; Scordo, M. Pilot Study of Telehealth Evaluations in Patients Undergoing Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2020, 26, e135–e137. [Google Scholar] [CrossRef]
- Ector, G.I.; Westerweel, P.E.; Hermens, R.P.; Braspenning, K.A.; Heeren, B.C.; Vinck, O.M.; de Jong, J.J.; Janssen, J.J.; Blijlevens, N.M. The Development of a Web-Based, Patient-Centered Intervention for Patients with Chronic Myeloid Leukemia (CMyLife): Design Thinking Development Approach. J. Med. Internet Res. 2020, 22, e15895. [Google Scholar] [CrossRef]
- Poudyal, B.S.; Gyawali, B.; Rondelli, D. Rapidly established telehealth care for blood cancer patients in Nepal during the COVID-19 pandemic using the free app Viber. Ecancermedicalscience 2020, 14, ed104. [Google Scholar] [PubMed]
- Zhang, T.; Song, Y.; Ying, Z.T.; Ping, L.; Zhang, C.; Xie, Y.; Liu, W.; Lin, N.; Tu, M.; Deng, L.; et al. Feasibility of mo-bile-deployed care management based on standardized ePRO and computer-interpretable-guideline engine for lymphoma patients. J. Clin. Oncol. 2019, 37. [Google Scholar] [CrossRef]
- Rueter, M.; Jeanneau, P.; Nogaro, J.C.; Lapeyre-Mestre, M.; Borel, C.; Bauvin, E.; Compaci, G.; Laurent, G.; Despas, F. The impact of ambulatory medical assistance during chemotherapy and follow-up for patients with diffuse large B-cell lymphoma (DLBCL) on the overall survival: PM1-113. Fundam. Clin. Pharmacol. 2014, 28 (Suppl. 1), 54. [Google Scholar]
- Condom, M.; Mussetti, A.; Maluquer, C.; Parody, R.; González-Barca, E.; Arnan, M.; Albasanz-Puig, A.; Pomares, H.; Salas, M.Q.; Carro, I.; et al. The direct and indirect effects of COVID-19 pandemic in a real-life hematological setting. Cancer Rep. 2021, 4, e1358. [Google Scholar] [CrossRef]
- Lupo-Stanghellini, M.T.; Messina, C.; Marktel, S.; Carrabba, M.G.; Peccatori, J.; Corti, C.; Ciceri, F. Following-up allogeneic transplantation recipients during the COVID-19 pandemic. Lancet Haematol. 2020, 7, e564–e565. [Google Scholar] [CrossRef]
- Dyer, G.; Gilroy, N.; Brown, L.; Hogg, M.; Brice, L.; Kabir, M.; Greenwood, M.; Larsen, S.R.; Moore, J.; Hertzberg, M.; et al. What They Want: Inclusion of Blood and Marrow Transplanation Survivor Preference in the Development of Models of Care for Long-Term Health in Sydney, Australia. Biol. Blood Marrow Transplant. 2016, 22, 731–743. [Google Scholar] [CrossRef] [Green Version]
- Koffman, B.; Pagel, J.M.; Kaempf, A.; Park, B.; Avruch, L.; Lee, C.; Movassaghi, B.; Byrd, J.C.; Skarbnik, A.; Davids, M.S.; et al. An Innovative Telemedicine Platform to Provide Expert Access to Patients with Chronic Lymphocytic Leukemia (CLL). Blood 2019, 134, 4716. [Google Scholar] [CrossRef]
- Koffman, B.; Pagel, J.M.; Bailey, N.; Kaempf, A.; Park, B.; Avruch, L.; Lee, C.X.; Movassaghi, B.; Byrd, J.C.; Skarbnik, A.P.; et al. Impact of CLL society’s (CLLS) free expert access program (EAP) for chronic lymphocytic leukemia (CLL) patients (pts). HemaSphere 2020, 4 (Suppl. 1), 871–872. [Google Scholar]
- Overend, A.; Khoo, K.; Delorme, M.; Krause, V.; Avanessian, A.; Saltman, D. Evaluation of a nurse-led telephone follow-up clinic for patients with indolent and chronic hematological malignancies: A pilot study. Can. Oncol. Nurs. J. 2008, 18, 64–68. [Google Scholar] [CrossRef] [Green Version]
- Narayanan, S.; Lopez, G.; Powers-James, C.; Fellman, B.M.; Chunduru, A.; Li, Y.; Bruera, E.; Cohen, L. Integrative Oncology Consultations Delivered via Telehealth in 2020 and In-Person in 2019: Paradigm Shift During the COVID-19 World Pandemic. Integr. Cancer Ther. 2021, 20. [Google Scholar] [CrossRef]
- Fattizzo, B.; Giannotta, J.A.; Barcellini, W.; Barbanti, M.C.; Bucelli, C.; Cassin, R.; Cattaneo, D.; Cavallaro, F.; Ferla, V.; Fracchiolla, N.S.; et al. Ensuring continuity of care of hematologic patients during COVID-19 pandemic in a tertiary hospital in Lombardy (Italy). Blood Adv. 2020, 4, 2996–2999. [Google Scholar] [CrossRef] [PubMed]
- Runge, J.S.; Brown, A.B.; Phillips, T.J.; Kaminski, M.S.; Carty, S.A.; Wilcox, R.A. The Feasibility of Virtual Toxicity Assessments in Lymphoma Patients Receiving Im-munochemotherapy. Blood 2020, 136, 1–2. [Google Scholar] [CrossRef]
- Isidori, A.; De Leval, L.; Gergis, U.; Musto, P.; Porcu, P. Management of Patients with Hematologic Malignancies During the COVID-19 Pandemic: Practical Considerations and Lessons to Be Learned. Front. Oncol. 2020, 10, 1439. [Google Scholar] [CrossRef] [PubMed]
- Severe, J.; Tang, R.; Horbatch, F.; Onishchenko, R.; Naini, V.; Blazek, M.C. Factors Influencing Patients’ Initial Decisions Regarding Telepsychiatry Participation During the COVID-19 Pandemic: Telephone-Based Survey. JMIR Form. Res. 2020, 4, e25469. [Google Scholar] [CrossRef] [PubMed]
- Loree, J.M.; Dau, H.; Rebić, N.; Howren, A.; Gastonguay, L.; McTaggart-Cowan, H.; Gill, S.; Raghav, K.; De Vera, M.A. Virtual Oncology Appointments during the Initial Wave of the COVID-19 Pandemic: An International Survey of Patient Perspectives. Curr. Oncol. 2021, 28, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Kenney, L.B.; Vrooman, L.M.; Lind, E.D.; Brace-O’Neill, J.; Mulder, J.E.; Nekhlyudov, L.; Recklitis, C.J. Virtual visits as long-term follow-up care for childhood cancer survivors: Patient and provider satisfaction during the COVID-19 pandemic. Pediatr. Blood Cancer 2021, 68, e28927. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Waller, M.; Pandya, A.; Portnoy, J. A Review of Patient and Provider Satisfaction with Telemedicine. Curr. Allergy Asthma Rep. 2020, 20, 72. [Google Scholar] [CrossRef]
- Chi, M. The Hidden Cost of Cancer: Helping Clients Cope with Financial Toxicity. Clin. Soc. Work J. 2019, 47, 249–257. [Google Scholar] [CrossRef]
- Knight, T.G.; Deal, A.M.; Dusetzina, S.B.; Muss, H.B.; Choi, S.K.; Bensen, J.T.; Williams, G. Financial Toxicity in Adults With Cancer: Adverse Outcomes and Noncompliance. J. Oncol. Pr. 2018, 14, e665–e673. [Google Scholar] [CrossRef]
- Lentz, R.; Benson, A.B., III.; Kircher, S. Financial toxicity in cancer care: Prevalence, causes, consequences, and reduction strategies. J. Surg. Oncol. 2019, 120, 85–92. [Google Scholar] [CrossRef]
- Alam Siddiquee, N.K.; Poudyal, A.; Pandey, A.; Shrestha, N.; Karki, S.; Subedi, R.; Sah, A.K.; Dirghayu, K.C. Telemedicine in Resource-Limited Setting: Narrative Synthesis of Evidence in Nepalese Context. Smart Homecare Technol. TeleHealth 2020, 6, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Lovell, T.; Albritton, J.; Dalto, J.; Ledward, C.; Daines, W. Virtual vs traditional care settings for low-acuity urgent conditions: An economic analysis of cost and utilization using claims data. J. Telemed. Telecare 2021, 27, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Baker, A. Crossing the Quality Chasm: A New Health System for the 21st Century. BMJ 2001, 323, 1192. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suleman, A.; Vijenthira, A.; Berlin, A.; Prica, A.; Rodin, D. The Use of Virtual Care in Patients with Hematologic Malignancies: A Scoping Review. Curr. Oncol. 2022, 29, 892-900. https://doi.org/10.3390/curroncol29020076
Suleman A, Vijenthira A, Berlin A, Prica A, Rodin D. The Use of Virtual Care in Patients with Hematologic Malignancies: A Scoping Review. Current Oncology. 2022; 29(2):892-900. https://doi.org/10.3390/curroncol29020076
Chicago/Turabian StyleSuleman, Adam, Abi Vijenthira, Alejandro Berlin, Anca Prica, and Danielle Rodin. 2022. "The Use of Virtual Care in Patients with Hematologic Malignancies: A Scoping Review" Current Oncology 29, no. 2: 892-900. https://doi.org/10.3390/curroncol29020076
APA StyleSuleman, A., Vijenthira, A., Berlin, A., Prica, A., & Rodin, D. (2022). The Use of Virtual Care in Patients with Hematologic Malignancies: A Scoping Review. Current Oncology, 29(2), 892-900. https://doi.org/10.3390/curroncol29020076




