The Use of Breath Analysis in the Management of Lung Cancer: Is It Ready for Primetime?
Abstract
1. Introduction
2. Methods
3. History of Breath Analysis
4. Composition of Exhaled Breath
5. Breath Sample Collection
Breath Collection Devices
6. Methods of Breath Analysis
6.1. Spectrometry-Based Methods
| Analytical Method | Number of Participants | Results | Ref. |
|---|---|---|---|
| Cyranose 320 | 14 LC patients, 19 α-1-anti-trypsin deficiency, 6 chronic pulmonary berryliosis, 20 HC | Sensitivity 71.4% Specificity 91.9% VOC signature: Isobutene, benzene methanol, ethanol, acetone, pentane, isoprene, isopranolol, dimethylsulfide, carbon disulfide, toluene | [67] |
| Colorimetric | 49 NSCLC patients, 18 COPD, 15 IPF, 20 PAH, 21 HC | Sensitivity 73.3% Specificity 72.4% | [68] |
| Cyranose 320 | 10 LC subjects, 10 COPD (a), 10 HC (b) | Accuracy 85% Accuracy 90% | [69] |
| Nanosensor array with gold nanoparticles | 30 LC, 26 colon cancer, 22 breast cancer, 18 prostate cancer, 22 HC | [70] | |
| Quartz microbalance (LibraNose) | 28 LC, 36 HC, 28 other lung disease | Sensitivity LC versus HC: 85%, LC vs. LC 92.8% Specificity LC versus HC 92.8%, LC vs. LD 78.6% | [71] |
| Colorimetric | 92 NSCLC, 67 LC screening group, 70 indeterminate lung nodules | Sensitivity 70% Specificity 86% | [72] |
| Nanosensor array with single wall carbon nanotubes + gold nanoparticles | 53 malignant nodules, 19 benign nodules | Sensitivity 86% Specificity 96% | [21] |
| LibraNose | 42 LC, 18 HC | Accuracy 94% | [73] |
| SAW-based eNose | 42 LC, 8 LD, 18 HC | 11 VOCs predict LC (styrene, decane, isoprene, hexanal, propyl benzene, 1,2,4-trimethyl benzene, heptanal, methyl cyclopentane | [74] |
| MOS sensors-based eNose | 43 LC, 58 HC | Sensitivity 95.3% Specificity 90.5% Accuracy 92.6% | [75] |
| SAW-based eNose | 15 LC, 7 LD, 10 HC | 11 VOCs predict LC | [76] |
| ENS Mk3 (E-Nose Pty, Sydney) | 16 LC, 11 LD, 18 smokers, 11 ex-smokers, 33 non-smokers | p-values = 0.045, 0.025, 0.001 for discriminating based on different e-nose | [77] |
| Nanoscale NA-NOSE | 25 LC (a), 22 HNC (b), 40 HC | Sensitivity 100% (a, b, c) Specificity 91% (a, b), 100% (c) | [78] |
| Colorimetric sensor assay | 92 LC, 137 HC | Accuracy 81.1% | [72] |
| NA-NOSE with GC-MS | 53 LC, 19 HC (a), adenocarcinoma and squamous (b), early and advanced disease (c) | Accuracy 88% (a, b, c) | [21] |
| MOS-SAW-based eNose | 47 LC, 42 HC | Sensitivity 93.62%, Specificity 83.37% | [79] |
| Nanomaterial-based eNose | 12 LC, 5 HC | Sensitivity 100% Specificity 80% | [80] |
| Cyranose 320 | 27 LC, 37 HC LC vs. Healthy smokers LC vs. never smokers | Sensitivity 63%, specificity 78%, accuracy 72% Sensitivity 96%, specificity 40%, accuracy 81% | [81] |
| QMB-based eNose | 20 LC, 10 LD | Accuracy 90% | [82] |
| Cyranose 320 | 38 LC, 39 COPD | Sensitivity 80%, Accuracy 48% | [83] |
| SpiroNose | 31 LC, 31 COPD (a), 37 asthma (b), 45 HC (c) | Accuracy: (a) 87% (b) 68% (c) 88% | [84] |
| Cyranose 320 | 25 LC, 166 current or former smokers without LC | Sensitivity 88%, Specificity 81.3% | [85] |
| BIONOTE | 23 LC, 77 HC | Sensitivity 86%, Specificity 95% | [86] |
| Cyranose 320 | 165 LC, 335 total (91 non-cancer, 79 HC) | Sensitivity 87.3%, Specificity 71.2% | [87] |
| Carbon nanotube sensor array | 56 LC, 188 HC | Sensitivity 75–100%, Specificity 86.2–96.6%, Accuracy 85.4–92.7% | [88] |
| Aeonose | 144 LC, 146 HC | Sensitivity 94.4% Specificity 32.9% | [89] |
| MOS sensor array | 6 LC, 10 HC | Sensitivity 85.7%, Specificity 100% | [42] |
| Cyranose 320 | 252 LC, 223 non-cancer controls (smokers (a), non-smokers (b)) | Sensitivity 95.8%, specificity 92.3% Sensitivity 96.2%, specificity 90.6% | [90] |
6.2. Electronic Nose (e-Nose) Technology
6.3. Canine Detection
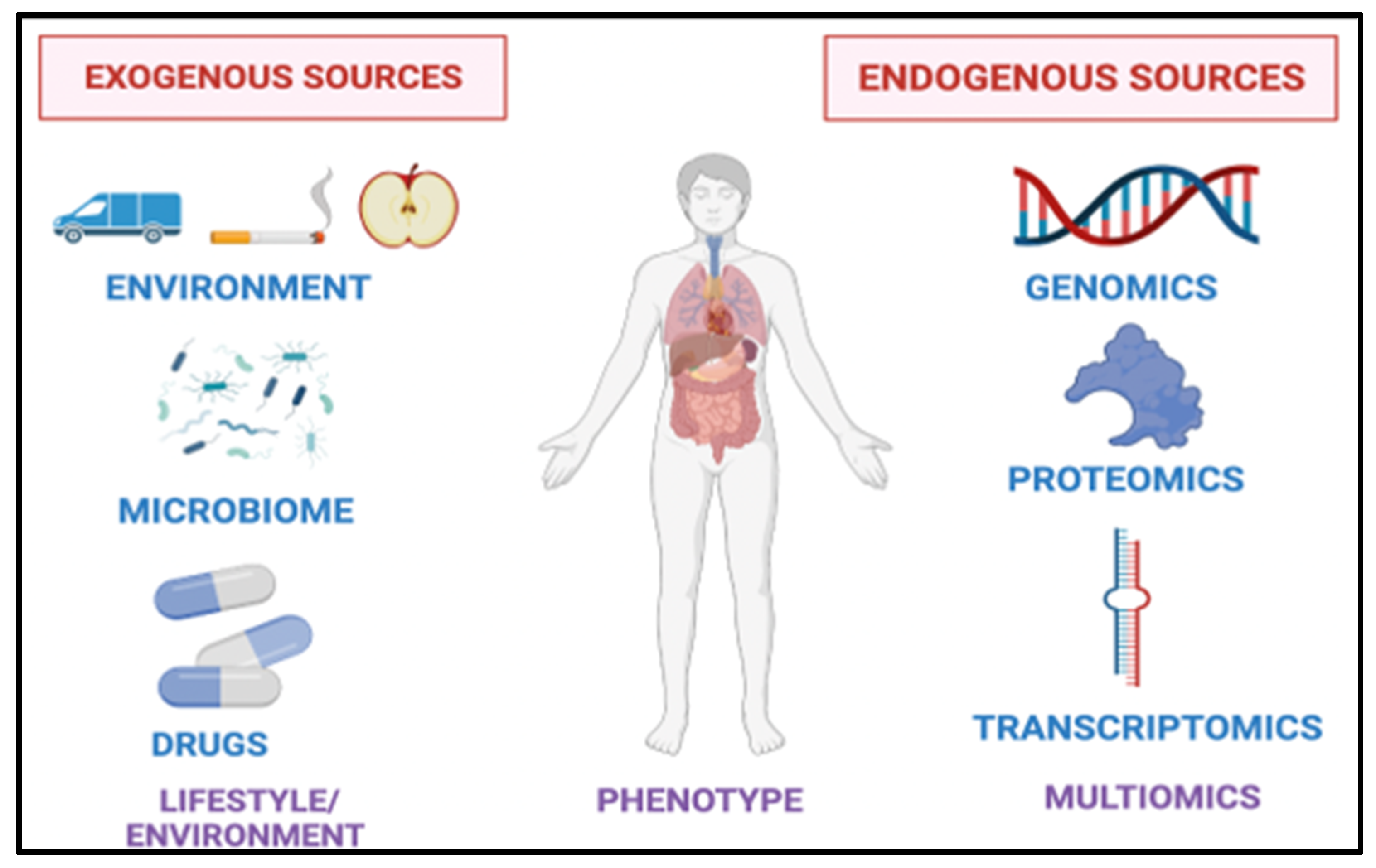
7. Factors Affecting Breath Analysis
7.1. Age/Sex
7.2. Smoking
7.3. Pollution
7.4. Food
7.5. Medications
7.6. The Microbiome
7.7. Hypoxia
7.8. Other Diagnoses
7.8.1. Lung Conditions
7.8.2. Non-Pulmonary Conditions
7.8.3. Extrapulmonary Malignancies
8. Applications of Breath Biomarkers in Clinical Practice
8.1. Early Detection and Diagnosis
8.2. Precision Medicine Applications
8.3. Monitoring for Treatment Response
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cancer.net. Lung Cancer—Non-Small Cell: Statistics. 2022. Available online: https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/statistics (accessed on 15 April 2022).
- Gay, C.M.; Stewart, C.A.; Park, E.M.; Diao, L.; Groves, S.M.; Heeke, S.; Nabet, B.Y.; Fujimoto, J.; Solis, L.M.; Lu, W.; et al. Patterns of transcription factor programs and immune pathway activation define four major subtypes of SCLC with distinct therapeutic vulnerabilities. Cancer Cell 2021, 39, 346–360.e7. [Google Scholar] [CrossRef]
- Rudin, C.M.; Poirier, J.T.; Byers, L.A.; Dive, C.; Dowlati, A.; George, J.; Heymach, J.V.; Johnson, J.E.; Lehman, J.M.; MacPherson, D.; et al. Molecular subtypes of small cell lung cancer: A synthesis of human and mouse model data. Nat. Rev. Cancer 2019, 19, 289–297. [Google Scholar] [CrossRef]
- Mok, T.; Wu, Y.L.; Lee, J.S.; Yu, C.J.; Sriuranpong, V.; Sandoval-Tan, J.; Ladrera, G.; Thongprasert, S.; Srimuninnimit, V.; Liao, M.; et al. Detection and Dynamic Changes of EGFR Mutations from Circulating Tumor DNA as a Predictor of Survival Outcomes in NSCLC Patients Treated with First-line Intercalated Erlotinib and Chemotherapy. Clin. Cancer Res. 2015, 21, 3196–3203. [Google Scholar] [CrossRef]
- Jee, J.; Lebow, E.S.; Murciano-Goroff, Y.R.; Jayakumaran, G.; Shen, R.; Brannon, A.R.; Benayed, R.; Namakydoust, A.; Offin, M.; Paik, P.K.; et al. Overall survival with circulating tumor DNA-guided therapy in advanced non-small cell lung cancer. J. Clin. Oncol. 2021, 39, 9009. [Google Scholar] [CrossRef]
- Giroux Leprieur, E.; Herbretau, G.; Dumenil, C.; Julie, C.; Giraud, V.; Labrune, S.; Dumoulin, J.; Tisserand, J.; Emile, J.-F.; Blons, H.; et al. Circulating tumor DNA evaluated by Next-Generation Sequencing is predictive of tumor response and prolonged clinical benefit with nivolumab in advanced non-small cell lung cancer. Oncoimmunology 2018, 7, e1424675. [Google Scholar] [CrossRef]
- Davidson, L.S. Mercaptan in the breath of patients with severe liver disease. Lancet 1949, 2, 197. [Google Scholar] [CrossRef]
- Pauling, L.; Robinson, A.B.; Teranishi, R.; Cary, P. Quantitative analysis of urine vapor and breath by gas-liquid partition chromatography. Proc. Natl. Acad. Sci. USA 1971, 68, 2374–2376. [Google Scholar] [CrossRef]
- Riely, C.A.; Cohen, G.; Lieberman, M. Ethane evolution: A new index of lipid peroxidation. Science 1974, 183, 208–210. [Google Scholar] [CrossRef]
- Phillips, M.; Hensley, P.; Baiter, R.A.; Cohan, S.L. An Improved Method for Collecting Breath for the Assay of Acetaldehyde. Alcohol. Clin. Exp. Res. 1984, 8, 293–296. [Google Scholar] [CrossRef]
- Phillips, M.; Gleeson, K.; Hughes, J.M.; Greenberg, J.; Cataneo, R.N.; Baker, L.; McVay, W.P. Volatile organic compounds in breath as markers of lung cancer: A cross-sectional study. Lancet 1999, 353, 1930–1933. [Google Scholar] [CrossRef]
- Gordon, S.M.; Szidon, J.P.; Krotoszynski, B.K.; Gibbons, R.D.; O’Neill, H.J. Volatile organic compounds in exhaled air from patients with lung cancer. Clin. Chem. 1985, 31, 1278–1282. [Google Scholar] [CrossRef]
- Fenske, J.D.; Paulson, S.E. Human breath emissions of VOCs. J. Air Waste Manag. Assoc. 1999, 49, 594–598. [Google Scholar] [CrossRef]
- Phillips, M.; Cataneo, R.N.; Cummin, A.R.; Gagliardi, A.J.; Gleeson, K.; Greenberg, J.; Maxfield, R.A.; Rom, W.N. Detection of lung cancer with volatile markers in the breath. Chest 2003, 123, 2115–2123. [Google Scholar] [CrossRef] [PubMed]
- Poli, D.; Goldoni, M.; Corradi, M.; Acampa, O.; Carbognani, P.; Internullo, E.; Casalini, A.; Mutti, A. Determination of aldehydes in exhaled breath of patients with lung cancer by means of on-fiber-derivatisation SPME-GC/MS. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2010, 878, 2643–2651. [Google Scholar] [CrossRef]
- Phillips, M.; Altorki, N.; Austin, J.H.; Cameron, R.B.; Cataneo, R.N.; Greenberg, J.; Kloss, R.; Maxfield, R.A.; Munawar, M.I.; Pass, H.I.; et al. Prediction of lung cancer using volatile biomarkers in breath. Cancer Biomark. 2007, 3, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Xu, F.; Wang, Y.; Pan, Y.; Lu, D.; Wang, P.; Ying, K.; Chen, E.; Zhang, W. A study of the volatile organic compounds exhaled by lung cancer cells in vitro for breath diagnosis. Cancer 2007, 110, 835–844. [Google Scholar] [CrossRef]
- Bajtarevic, A.; Ager, C.; Pienz, M.; Klieber, M.; Schwarz, K.; Ligor, M.; Ligor, T.; Filipiak, W.; Denz, H.; Fiegl, M.; et al. Noninvasive detection of lung cancer by analysis of exhaled breath. BMC Cancer 2009, 9, 348. [Google Scholar] [CrossRef]
- Fuchs, P.; Loeseken, C.; Schubert, J.K.; Miekisch, W. Breath gas aldehydes as biomarkers of lung cancer. Int. J. Cancer 2010, 126, 2663–2670. [Google Scholar] [CrossRef]
- Wang, Y.; Hu, Y.; Wang, D.; Yu, K.; Wang, L.; Zou, Y.; Zhao, C.; Zhang, X.; Wang, P.; Ying, K. The analysis of volatile organic compounds biomarkers for lung cancer in exhaled breath, tissues and cell lines. Cancer Biomark. 2012, 11, 129–137. [Google Scholar] [CrossRef]
- Peled, N.; Hakim, M.; Bunn, P.A., Jr.; Miller, Y.E.; Kennedy, T.C.; Mattei, J.; Mitchell, J.D.; Hirsch, F.R.; Haick, H. Non-invasive breath analysis of pulmonary nodules. J. Thorac. Oncol. 2012, 7, 1528–1533. [Google Scholar] [CrossRef]
- Zou, Y.; Hu, Y.; Jiang, Z.; Chen, Y.; Zhou, Y.; Wang, Z.; Wang, Y.; Jiang, G.; Tan, Z.; Hu, F. Exhaled metabolic markers and relevant dysregulated pathways of lung cancer: A pilot study. Ann. Med. 2022, 54, 790–802. [Google Scholar] [CrossRef] [PubMed]
- Tsou, P.-H.; Lin, Z.-L.; Pan, Y.-C.; Yang, H.-C.; Chang, C.-J.; Liang, S.-K.; Wen, Y.-F.; Chang, C.-H.; Chang, L.-Y.; Yu, K.-L.; et al. Exploring Volatile Organic Compounds in Breath for High-Accuracy Prediction of Lung Cancer. Cancers 2021, 13, 1431. [Google Scholar] [CrossRef]
- Wang, P.; Huang, Q.; Meng, S.; Mu, T.; Liu, Z.; He, M.; Li, Q.; Zhao, S.; Wang, S.; Qiu, M. Identification of lung cancer breath biomarkers based on perioperative breathomics testing: A prospective observational study. eClinicalMedicine 2022, 47, 101384. [Google Scholar] [CrossRef]
- Politi, L.; Monasta, L.; Rigressi, M.N.; Princivalle, A.; Gonfiotti, A.; Camiciottoli, G.; Perbellini, L. Discriminant Profiles of Volatile Compounds in the Alveolar Air of Patients with Squamous Cell Lung Cancer, Lung Adenocarcinoma or Colon Cancer. Molecules 2021, 26, 550. [Google Scholar] [CrossRef] [PubMed]
- Koureas, M.; Kirgou, P.; Amoutzias, G.; Hadjichristodoulou, C.; Gourgoulianis, K.; Tsakalof, A. Target Analysis of Volatile Organic Compounds in Exhaled Breath for Lung Cancer Discrimination from Other Pulmonary Diseases and Healthy Persons. Metabolites 2020, 10, 317. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, J.; Kowalkowski, T.; Buszewski, B. Searching for selected VOCs in human breath samples as potential markers of lung cancer. Lung Cancer 2019, 135, 123–129. [Google Scholar] [CrossRef]
- Jareno Esteban, J.; Munoz Lucas, M.A.; Carrillo Aranda, B.; Maldonado Sanz, J.A.; Civera Tejuca, C.; Aguilar Ros, A.; Rodriguez Trigo, G.; Gutierrez Ortega, C.; Alvarez Sala, J.L.; Callol Sanchez, L. Volatile organic compounds (VOC) in exhaled breath in patients with lung cancer, using the analytical technique thermal desorber- gase chromatography-spectrometer mases. Eur. Respir. J. 2012, 40 (Suppl. 56), P4204. [Google Scholar]
- Schumer, E.M.; Trivedi, J.R.; van Berkel, V.; Black, M.C.; Li, M.; Fu, X.-A.; Bousamra, M. High sensitivity for lung cancer detection using analysis of exhaled carbonyl compounds. J. Thorac. Cardiovasc. Surg. 2015, 150, 1517–1524. [Google Scholar] [CrossRef] [PubMed]
- Peralbo-Molina, A.; Calderón-Santiago, M.; Jurado-Gámez, B.; Luque de Castro, M.D.; Priego-Capote, F. Exhaled breath condensate to discriminate individuals with different smoking habits by GC–TOF/MS. Sci. Rep. 2017, 7, 1421. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Yang, D.; Brock, G.; Knipp, R.J.; Bousamra, M.; Nantz, M.H.; Fu, X.-A. Breath carbonyl compounds as biomarkers of lung cancer. Lung Cancer 2015, 90, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Corradi, M.; Poli, D.; Banda, I.; Bonini, S.; Mozzoni, P.; Pinelli, S.; Alinovi, R.; Andreoli, R.; Ampollini, L.; Casalini, A.; et al. Exhaled breath analysis in suspected cases of non-small-cell lung cancer: A cross-sectional study. J. Breath Res. 2015, 9, 027101. [Google Scholar] [CrossRef]
- Fu, X.A.; Li, M.; Knipp, R.J.; Nantz, M.H.; Bousamra, M. Noninvasive detection of lung cancer using exhaled breath. Cancer Med. 2014, 3, 174–181. [Google Scholar] [CrossRef]
- Bousamra, M., 2nd; Schumer, E.; Li, M.; Knipp, R.J.; Nantz, M.H.; van Berkel, V.; Fu, X.A. Quantitative analysis of exhaled carbonyl compounds distinguishes benign from malignant pulmonary disease. J. Thorac. Cardiovasc. Surg. 2014, 148, 1074–1080; discussion 1080–1081. [Google Scholar] [CrossRef]
- Schumer, E.M.; Black, M.C.; Bousamra, M., 2nd; Trivedi, J.R.; Li, M.; Fu, X.A.; van Berkel, V. Normalization of Exhaled Carbonyl Compounds After Lung Cancer Resection. Ann. Thorac. Surg. 2016, 102, 1095–1100. [Google Scholar] [CrossRef]
- Ligor, M.; Ligor, T.; Bajtarevic, A.; Ager, C.; Pienz, M.; Klieber, M.; Denz, H.; Fiegl, M.; Hilbe, W.; Weiss, W.; et al. Determination of volatile organic compounds in exhaled breath of patients with lung cancer using solid phase microextraction and gas chromatography mass spectrometry. Clin. Chem. Lab. Med. 2009, 47, 550–560. [Google Scholar] [CrossRef]
- Nardi-Agmon, I.; Abud-Hawa, M.; Liran, O.; Gai-Mor, N.; Ilouze, M.; Onn, A.; Bar, J.; Shlomi, D.; Haick, H.; Peled, N. Exhaled Breath Analysis for Monitoring Response to Treatment in Advanced Lung Cancer. J. Thorac. Oncol. 2016, 11, 827–837. [Google Scholar] [CrossRef]
- Phillips, M.; Bauer, T.L.; Pass, H.I. A volatile biomarker in breath predicts lung cancer and pulmonary nodules. J. Breath Res. 2019, 13, 036013. [Google Scholar] [CrossRef]
- Dent, A.G.; Sutedja, T.G.; Zimmerman, P.V. Exhaled breath analysis for lung cancer. J. Thorac. Dis. 2013, 5 (Suppl. 5), S540–S550. [Google Scholar] [CrossRef]
- Finamore, P.; Scarlata, S.; Incalzi, R.A. Breath analysis in respiratory diseases: State-of-the-art and future perspectives. Expert Rev. Mol. Diagn. 2019, 19, 47–61. [Google Scholar] [CrossRef]
- Jia, Z.; Patra, A.; Kutty, V.K.; Venkatesan, T. Critical Review of Volatile Organic Compound Analysis in Breath and In Vitro Cell Culture for Detection of Lung Cancer. Metabolites 2019, 9, 52. [Google Scholar] [CrossRef]
- Marzorati, D.; Mainardi, L.T.; Sedda, G.; Gasparri, R.; Spaggiari, L.; Cerveri, P. A Metal Oxide Gas Sensors Array for Lung Cancer Diagnosis through Exhaled Breath Analysis. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 1584–1587. [Google Scholar]
- Kneepkens, C.M.; Lepage, G.; Roy, C.C. The potential of the hydrocarbon breath test as a measure of lipid peroxidation. Free Radic. Biol. Med. 1994, 17, 127–160. [Google Scholar] [CrossRef]
- Shirasu, M.; Touhara, K. The scent of disease: Volatile organic compounds of the human body related to disease and disorder. J. Biochem. 2011, 150, 257–266. [Google Scholar] [CrossRef]
- Stavropoulos, G.; van Munster, K.; Ferrandino, G.; Sauca, M.; Ponsioen, C.; van Schooten, F.J.; Smolinska, A. Liver Impairment-The Potential Application of Volatile Organic Compounds in Hepatology. Metabolites 2021, 11, 618. [Google Scholar] [CrossRef]
- Janssens, E.; van Meerbeeck, J.P.; Lamote, K. Volatile organic compounds in human matrices as lung cancer biomarkers: A systematic review. Crit. Rev. Oncol./Hematol. 2020, 153, 103037. [Google Scholar] [CrossRef]
- Janfaza, S.; Khorsand, B.; Nikkhah, M.; Zahiri, J. Digging deeper into volatile organic compounds associated with cancer. Biol. Methods Protoc. 2019, 4, bpz014. [Google Scholar] [CrossRef]
- Antoniou, S.X.; Gaude, E.; Ruparel, M.; van der Schee, M.P.; Janes, S.M.; Rintoul, R.C. The potential of breath analysis to improve outcome for patients with lung cancer. J. Breath Res. 2019, 13, 034002. [Google Scholar] [CrossRef]
- Rahimpour, E.; Khoubnasabjafari, M.; Jouyban-Gharamaleki, V.; Jouyban, A. Non-volatile compounds in exhaled breath condensate: Review of methodological aspects. Anal. Bioanal. Chem. 2018, 410, 6411–6440. [Google Scholar] [CrossRef]
- Zhang, X.; Zou, Y.; An, C.; Ying, K.; Chen, X.; Wang, P. Sensitive detection of carcinoembryonic antigen in exhaled breath condensate using surface acoustic wave immunosensor. Sens. Actuators B Chem. 2015, 217, 100–106. [Google Scholar] [CrossRef]
- Effros, R.M.; Hoagland, K.W.; Bosbous, M.; Castillo, D.; Foss, B.; Dunning, M.; Gare, M.; Lin, W.; Sun, F. Dilution of respiratory solutes in exhaled condensates. Am. J. Respir. Crit. Care Med. 2002, 165, 663–669. [Google Scholar] [CrossRef]
- Effros, R.M.; Dunning, M.B., 3rd; Biller, J.; Shaker, R. The promise and perils of exhaled breath condensates. Am. J. Physiol. Lung Cell Mol. Physiol. 2004, 287, L1073–L1080. [Google Scholar] [CrossRef]
- Horváth, I.; Hunt, J.; Barnes, P.J.; Alving, K.; Antczak, A.; Baraldi, E.; Becher, G.; van Beurden, W.J.; Corradi, M.; Dekhuijzen, R.; et al. Exhaled breath condensate: Methodological recommendations and unresolved questions. Eur. Respir. J. 2005, 26, 523–548. [Google Scholar] [CrossRef]
- Steeghs, M.M.L.; Cristescu, S.M.; Harren, F.J.M. The suitability of Tedlar bags for breath sampling in medical diagnostic research. Physiol. Meas. 2006, 28, 73–84. [Google Scholar] [CrossRef]
- Soyer, O.U.; Dizdar, E.A.; Keskin, O.; Lilly, C.; Kalayci, O. Comparison of two methods for exhaled breath condensate collection. Allergy 2006, 61, 1016–1018. [Google Scholar] [CrossRef]
- van den Velde, S.; Quirynen, M.; van Hee, P.; van Steenberghe, D. Differences between Alveolar Air and Mouth Air. Anal. Chem. 2007, 79, 3425–3429. [Google Scholar] [CrossRef]
- Poli, D.; Carbognani, P.; Corradi, M.; Goldoni, M.; Acampa, O.; Balbi, B.; Bianchi, L.; Rusca, M.; Mutti, A. Exhaled volatile organic compounds in patients with non-small cell lung cancer: Cross sectional and nested short-term follow-up study. Respir. Res. 2005, 6, 71. [Google Scholar] [CrossRef]
- Kusano, M.; Mendez, E.; Furton, K.G. Development of headspace SPME method for analysis of volatile organic compounds present in human biological specimens. Anal. Bioanal. Chem. 2011, 400, 1817–1826. [Google Scholar] [CrossRef]
- Scheepers, P.T.; Konings, J.; Demirel, G.; Gaga, E.O.; Anzion, R.; Peer, P.G.; Dogeroglu, T.; Ornektekin, S.; van Doorn, W. Determination of exposure to benzene, toluene and xylenes in Turkish primary school children by analysis of breath and by environmental passive sampling. Sci. Total Environ. 2010, 408, 4863–4870. [Google Scholar] [CrossRef]
- Phillips, C.O.; Syed, Y.; Parthaláin, N.M.; Zwiggelaar, R.; Claypole, T.C.; Lewis, K.E. Machine learning methods on exhaled volatile organic compounds for distinguishing COPD patients from healthy controls. J. Breath Res. 2012, 6, 036003. [Google Scholar] [CrossRef]
- Henderson, K.A.; Matthews, I.P. Biological monitoring of midwives’ exposure to N2O using the Bio-VOC breath sampler. J. Expo. Anal. Environ. Epidemiol. 2002, 12, 309–312. [Google Scholar] [CrossRef]
- Hryniuk, A.; Ross, B.M. Detection of acetone and isoprene in human breath using a combination of thermal desorption and selected ion flow tube mass spectrometry. Int. J. Mass Spectrom. 2009, 285, 26–30. [Google Scholar] [CrossRef]
- Mistral. Mistral: Diagnosis in a Breath. Health in a Puff. 2022. Available online: https://www.mistral-breath.it/en/mistral/ (accessed on 1 July 2022).
- Medical, O. ReCIVA® Breath Sampler. Available online: https://www.owlstonemedical.com/products/reciva/ (accessed on 1 June 2022).
- MasaTECH. Ion Mobility Spectrometry—How Does It Work. 2022. Available online: https://www.masatech.eu/technology (accessed on 14 June 2022).
- Westhoff, M.; Litterst, P.; Freitag, L.; Urfer, W.; Bader, S.; Baumbach, J.I. Ion mobility spectrometry for the detection of volatile organic compounds in exhaled breath of patients with lung cancer: Results of a pilot study. Thorax 2009, 64, 744–748. [Google Scholar] [CrossRef] [PubMed]
- Machado, R.F.; Laskowski, D.; Deffenderfer, O.; Burch, T.; Zheng, S.; Mazzone, P.J.; Mekhail, T.; Jennings, C.; Stoller, J.K.; Pyle, J.; et al. Detection of lung cancer by sensor array analyses of exhaled breath. Am. J. Respir. Crit. Care Med. 2005, 171, 1286–1291. [Google Scholar] [CrossRef] [PubMed]
- Mazzone, P.J.; Hammel, J.; Dweik, R.; Na, J.; Czich, C.; Laskowski, D.; Mekhail, T. Diagnosis of lung cancer by the analysis of exhaled breath with a colorimetric sensor array. Thorax 2007, 62, 565–568. [Google Scholar] [CrossRef] [PubMed]
- Dragonieri, S.; Schot, R.; Mertens, B.J.; Le Cessie, S.; Gauw, S.A.; Spanevello, A.; Resta, O.; Willard, N.P.; Vink, T.J.; Rabe, K.F.; et al. An electronic nose in the discrimination of patients with asthma and controls. J. Allergy Clin. Immunol. 2007, 120, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Peng, G.; Hakim, M.; Broza, Y.Y.; Billan, S.; Abdah-Bortnyak, R.; Kuten, A.; Tisch, U.; Haick, H. Detection of lung, breast, colorectal, and prostate cancers from exhaled breath using a single array of nanosensors. Br. J. Cancer 2010, 103, 542–551. [Google Scholar] [CrossRef]
- D’Amico, A.; Pennazza, G.; Santonico, M.; Martinelli, E.; Roscioni, C.; Galluccio, G.; Paolesse, R.; Di Natale, C. An investigation on electronic nose diagnosis of lung cancer. Lung Cancer 2010, 68, 170–176. [Google Scholar] [CrossRef]
- Mazzone, P.J.; Wang, X.-F.; Xu, Y.; Mekhail, T.; Beukemann, M.C.; Na, J.; Kemling, J.W.; Suslick, K.S.; Sasidhar, M. Exhaled Breath Analysis with a Colorimetric Sensor Array for the Identification and Characterization of Lung Cancer. J. Thorac. Oncol. 2012, 7, 137–142. [Google Scholar] [CrossRef]
- Di Natale, C.; Macagnano, A.; Martinelli, E.; Paolesse, R.; D’Arcangelo, G.; Roscioni, C.; Finazzi-Agrò, A.; D’Amico, A. Lung cancer identification by the analysis of breath by means of an array of non-selective gas sensors. Biosens. Bioelectron. 2003, 18, 1209–1218. [Google Scholar] [CrossRef]
- Chen, X.; Cao, M.; Li, Y.; Hu, W.; Wang, P.; Ying, K.; Pan, H. A study of an electronic nose for detection of lung cancer based on a virtual SAW gas sensors array and imaging recognition method. Meas. Sci. Technol. 2005, 16, 1535–1546. [Google Scholar] [CrossRef]
- Blatt, R.; Bonarini, A.; Calabro, E.; Della Torre, M.; Matteucci, M.; Pastorino, U. Lung Cancer Identification by an Electronic Nose Based on an Array of MOS Sensors. In Proceedings of the 2007 International Joint Conference on Neural Networks, Orlando, FL, USA, 12–17 August 2007; pp. 1423–1428. [Google Scholar] [CrossRef]
- Wang, P.; Chen, X.; Xu, F.; Lu, D.; Cai, W.; Ying, K.; Wang, Y.; Hu, Y. Development of electronic nose for diagnosis of lung cancer at early atage. In Proceedings of the 2008 International Conference on Information Technology and Applications in Biomedicine, Shenzhen, China, 30–31 May 2008; pp. 588–591. [Google Scholar]
- Tran, V.; Chan, H.P.; Thurston, M.; Jackson, P.; Lewis, C.; Yates, D.; Bell, G.; Thomas, P. Breath Analysis of Lung Cancer Patients Using an Electronic Nose Detection System. Sens. J. IEEE 2010, 10, 1514–1518. [Google Scholar] [CrossRef]
- Hakim, M.; Billan, S.; Tisch, U.; Peng, G.; Dvrokind, I.; Marom, O.; Abdah-Bortnyak, R.; Kuten, A.; Haick, H. Diagnosis of head-and-neck cancer from exhaled breath. Br. J. Cancer 2011, 104, 1649–1655. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.I.; Yu, K.A.I.; Wang, Y.; Hu, Y.; Zhao, C.; Wang, L.I.N.; Ying, K.; Wang, P. A hybrid electronic noses’ system based on mos-saw detection units intended for lung cancer diagnosis. J. Innov. Opt. Health Sci. 2012, 5, 1150006. [Google Scholar] [CrossRef]
- Broza, Y.; Haick, H. Nanomaterial-based sensors for detection of disease by volatile organic compounds. Nanomedicine 2013, 8, 785–806. [Google Scholar] [CrossRef] [PubMed]
- Bikov, A.; Hernadi, M.; Korosi, B.Z.; Kunos, L.; Zsamboki, G.; Sutto, Z.; Tarnoki, A.D.; Tarnoki, D.L.; Losonczy, G.; Horvath, I. Expiratory flow rate, breath hold and anatomic dead space influence electronic nose ability to detect lung cancer. BMC Pulm. Med. 2014, 14, 202. [Google Scholar] [CrossRef] [PubMed]
- Capuano, R.; Santonico, M.; Pennazza, G.; Ghezzi, S.; Martinelli, E.; Roscioni, C.; Lucantoni, G.; Galluccio, G.; Paolesse, R.; Di Natale, C.; et al. The lung cancer breath signature: A comparative analysis of exhaled breath and air sampled from inside the lungs. Sci. Rep. 2015, 5, 16491. [Google Scholar] [CrossRef]
- Hubers, A.J.; Brinkman, P.; Boksem, R.J.; Rhodius, R.J.; Witte, B.I.; Zwinderman, A.H.; Heideman, D.A.; Duin, S.; Koning, R.; Steenbergen, R.D.; et al. Combined sputum hypermethylation and eNose analysis for lung cancer diagnosis. J. Clin. Pathol. 2014, 67, 707–711. [Google Scholar] [CrossRef] [PubMed]
- de Vries, R.; Brinkman, P.; van der Schee, M.P.; Fens, N.; Dijkers, E.; Bootsma, S.K.; de Jongh, F.H.; Sterk, P.J. Integration of electronic nose technology with spirometry: Validation of a new approach for exhaled breath analysis. J. Breath Res. 2015, 9, 046001. [Google Scholar] [CrossRef] [PubMed]
- McWilliams, A.; Beigi, P.; Srinidhi, A.; Lam, S.; MacAulay, C.E. Sex and Smoking Status Effects on the Early Detection of Early Lung Cancer in High-Risk Smokers Using an Electronic Nose. IEEE Trans. Biomed. Eng. 2015, 62, 2044–2054. [Google Scholar] [CrossRef]
- Rocco, R.; Incalzi, R.A.; Pennazza, G.; Santonico, M.; Pedone, C.; Bartoli, I.R.; Vernile, C.; Mangiameli, G.; La Rocca, A.; De Luca, G.; et al. BIONOTE e-nose technology may reduce false positives in lung cancer screening programmes. Eur. J. Cardiothorac. Surg. 2016, 49, 1112–1117; discussion 1117. [Google Scholar] [CrossRef]
- Tirzīte, M.; Bukovskis, M.; Strazda, G.; Jurka, N.; Taivans, I. Detection of lung cancer in exhaled breath with an electronic nose using support vector machine analysis. J. Breath Res. 2017, 11, 036009. [Google Scholar] [CrossRef]
- Huang, C.-H.; Zeng, C.; Wang, Y.-C.; Peng, H.-Y.; Lin, C.-S.; Chang, C.-J.; Yang, H.-Y. A Study of Diagnostic Accuracy Using a Chemical Sensor Array and a Machine Learning Technique to Detect Lung Cancer. Sensors 2018, 18, 2845. [Google Scholar] [CrossRef] [PubMed]
- Kort, S.; Tiggeloven, M.M.; Brusse-Keizer, M.; Gerritsen, J.W.; Schouwink, J.H.; Citgez, E.; de Jongh, F.H.C.; Samii, S.; van der Maten, J.; van den Bogart, M.; et al. Multi-centre prospective study on diagnosing subtypes of lung cancer by exhaled-breath analysis. Lung Cancer 2018, 125, 223–229. [Google Scholar] [CrossRef]
- Tirzite, M.; Bukovskis, M.; Strazda, G.; Jurka, N.; Taivans, I. Detection of lung cancer with electronic nose and logistic regression analysis. J. Breath Res. 2018, 13, 016006. [Google Scholar] [CrossRef]
- Williams, H.; Pembroke, A. Sniffer dogs in the melanoma clinic? Lancet 1989, 333, 734. [Google Scholar] [CrossRef]
- Willis, C.M.; Church, S.M.; Guest, C.M.; Cook, W.A.; McCarthy, N.; Bransbury, A.J.; Church, M.R.T.; Church, J.C.T. Olfactory detection of human bladder cancer by dogs: Proof of principle study. BMJ 2004, 329, 712. [Google Scholar] [CrossRef]
- Horvath, G.; Järverud, G.a.K.; Järverud, S.; Horváth, I. Human Ovarian Carcinomas Detected by Specific Odor. Integr. Cancer Ther. 2008, 7, 76–80. [Google Scholar] [CrossRef]
- McCulloch, M.; Jezierski, T.; Broffman, M.; Hubbard, A.; Turner, K.; Janecki, T. Diagnostic Accuracy of Canine Scent Detection in Early- and Late-Stage Lung and Breast Cancers. Integr. Cancer Ther. 2006, 5, 30–39. [Google Scholar] [CrossRef]
- Phillips, M.; Cataneo, R.N.; Greenberg, J.; Gunawardena, R.; Naidu, A.; Rahbari-Oskoui, F. Effect of age on the breath methylated alkane contour, a display of apparent new markers of oxidative stress. J. Lab. Clin. Med. 2000, 136, 243–249. [Google Scholar] [CrossRef]
- Wehinger, A.; Schmid, A.; Mechtcheriakov, S.; Ledochowski, M.; Grabmer, C.; Gastl, G.A.; Amann, A. Lung cancer detection by proton transfer reaction mass-spectrometric analysis of human breath gas. Int. J. Mass Spectrom. 2007, 265, 49–59. [Google Scholar] [CrossRef]
- Kischkel, S.; Miekisch, W.; Sawacki, A.; Straker, E.M.; Trefz, P.; Amann, A.; Schubert, J.K. Breath biomarkers for lung cancer detection and assessment of smoking related effects--confounding variables, influence of normalization and statistical algorithms. Clin. Chim. Acta 2010, 411, 1637–1644. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.M.; Wallace, L.A.; Brinkman, M.C.; Callahan, P.J.; Kenny, D.V. Volatile organic compounds as breath biomarkers for active and passive smoking. Environ. Health Perspect. 2002, 110, 689–698. [Google Scholar] [CrossRef]
- Phillips, M.; Altorki, N.; Austin, J.H.; Cameron, R.B.; Cataneo, R.N.; Kloss, R.; Maxfield, R.A.; Munawar, M.I.; Pass, H.I.; Rashid, A.; et al. Detection of lung cancer using weighted digital analysis of breath biomarkers. Clin. Chim. Acta 2008, 393, 76–84. [Google Scholar] [CrossRef]
- Fens, N.; Zwinderman, A.H.; van der Schee, M.P.; de Nijs, S.B.; Dijkers, E.; Roldaan, A.C.; Cheung, D.; Bel, E.H.; Sterk, P.J. Exhaled breath profiling enables discrimination of chronic obstructive pulmonary disease and asthma. Am. J. Respir. Crit. Care Med. 2009, 180, 1076–1082. [Google Scholar] [CrossRef]
- Euler, D.E.; Davé, S.J.; Guo, H. Effect of cigarette smoking on pentane excretion in alveolar breath. Clin. Chem. 1996, 42, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Hansel, A.; Holzinger, R.; Lindinger, W. Acetonitrile and benzene in the breath of smokers and non-smokers investigated by proton transfer reaction mass spectrometry (PTR-MS). Int. J. Mass Spectrom. Ion Process. 1995, 148, L1–L3. [Google Scholar] [CrossRef]
- Lammers, A.; Neerincx, A.H.; Vijverberg, S.J.H.; Longo, C.; Janssen, N.A.H.; Boere, A.J.F.; Brinkman, P.; Cassee, F.R.; van der Zee, A.H.M. The Impact of Short-Term Exposure to Air Pollution on the Exhaled Breath of Healthy Adults. Sensors 2021, 21, 2518. [Google Scholar] [CrossRef]
- Eckel, S.P.; Cockburn, M.; Shu, Y.H.; Deng, H.; Lurmann, F.W.; Liu, L.; Gilliland, F.D. Air pollution affects lung cancer survival. Thorax 2016, 71, 891–898. [Google Scholar] [CrossRef]
- Liu, X.; Mubarik, S.; Wang, F.; Yu, Y.; Wang, Y.; Shi, F.; Wen, H.; Yu, C. Lung Cancer Death Attributable to Long-Term Ambient Particulate Matter (PM2.5) Exposure in East Asian Countries during 1990–2019. Front. Med. 2021, 8, 742076. [Google Scholar] [CrossRef] [PubMed]
- Swanton, C.; Hill, W.; Lim, E.; Lee, C.; Weeden, C.E.; Augustine, M.; Chen, K.; Kuan, F.C.; Marongiu, F.; Rodrigues, F.; et al. LBA1 Mechanism of action and an actionable inflammatory axis for air pollution induced non-small cell lung cancer: Towards molecular cancer prevention. Ann. Oncol. 2022, 33, S1413. [Google Scholar] [CrossRef]
- Smith, D.; Spanel, P.; Davies, S. Trace gases in breath of healthy volunteers when fasting and after a protein-calorie meal: A preliminary study. J. Appl. Physiol. 1999, 87, 1584–1588. [Google Scholar] [CrossRef]
- Bruderer, T.; Gaisl, T.; Gaugg, M.T.; Nowak, N.; Streckenbach, B.; Müller, S.; Moeller, A.; Kohler, M.; Zenobi, R. On-Line Analysis of Exhaled Breath. Chem. Rev. 2019, 119, 10803–10828. [Google Scholar] [CrossRef]
- Borras, E.; Cheng, A.; Wun, T.; Reese, K.L.; Frank, M.; Schivo, M.; Davis, C.E. Detecting opioid metabolites in exhaled breath condensate (EBC). J. Breath Res. 2019, 13, 046014. [Google Scholar] [CrossRef]
- Parente, F.; Sainaghi, M.; Sangaletti, O.; Imbesi, V.; Maconi, G.; Anderloni, A.; Bianchi Porro, G. Different effects of short-term omeprazole, lansoprazole or pantoprazole on the accuracy of the (13)C-urea breath test. Aliment. Pharmacol. Ther. 2002, 16, 553–557. [Google Scholar] [CrossRef]
- Ates, H.C.; Mohsenin, H.; Wenzel, C.; Glatz, R.T.; Wagner, H.J.; Bruch, R.; Hoefflin, N.; Spassov, S.; Streicher, L.; Lozano-Zahonero, S.; et al. Biosensor-Enabled Multiplexed On-Site Therapeutic Drug Monitoring of Antibiotics. Adv. Mater. 2022, 34, 2104555. [Google Scholar] [CrossRef]
- Leeming, E.R.; Johnson, A.J.; Spector, T.D.; Le Roy, C.I. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients 2019, 11, 2862. [Google Scholar] [CrossRef]
- Liu, J.; Tan, Y.; Cheng, H.; Zhang, D.; Feng, W.; Peng, C. Functions of gut microbiota metabolites, current status and future perspectives. Aging Dis. 2022, 13, 1106–1126. [Google Scholar] [CrossRef]
- Gopalakrishnan, V.; Spencer, C.N.; Nezi, L.; Reuben, A.; Andrews, M.C.; Karpinets, T.V.; Prieto, P.A.; Vicente, D.; Hoffman, K.; Wei, S.C.; et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 2018, 359, 97–103. [Google Scholar] [CrossRef]
- Neyrinck, A.M.; Rodriguez, J.; Zhang, Z.; Nazare, J.A.; Bindels, L.B.; Cani, P.D.; Maquet, V.; Laville, M.; Bischoff, S.C.; Walter, J.; et al. Breath volatile metabolome reveals the impact of dietary fibres on the gut microbiota: Proof of concept in healthy volunteers. EBioMedicine 2022, 80, 104051. [Google Scholar] [CrossRef]
- Harshman, S.W.; Geier, B.A.; Fan, M.; Rinehardt, S.; Watts, B.S.; Drummond, L.A.; Preti, G.; Phillips, J.B.; Ott, D.K.; Grigsby, C.C. The identification of hypoxia biomarkers from exhaled breath under normobaric conditions. J. Breath Res. 2015, 9, 047103. [Google Scholar] [CrossRef] [PubMed]
- Orhan, H.; van Holland, B.; Krab, B.; Moeken, J.; Vermeulen, N.P.E.; Hollander, P.; Meerman, J.H.N. Evaluation of a Multi-parameter Biomarker Set for Oxidative Damage in Man: Increased Urinary Excretion of Lipid, Protein and DNA Oxidation Products after One Hour of Exercise. Free. Radic. Res. 2004, 38, 1269–1279. [Google Scholar] [CrossRef]
- Ullah, A.; Leong, S.W.; Wang, J.; Wu, Q.; Ghauri, M.A.; Sarwar, A.; Su, Q.; Zhang, Y. Cephalomannine inhibits hypoxia-induced cellular function via the suppression of APEX1/HIF-1α interaction in lung cancer. Cell Death Dis. 2021, 12, 490. [Google Scholar] [CrossRef] [PubMed]
- Barker, M.; Hengst, M.; Schmid, J.; Buers, H.J.; Mittermaier, B.; Klemp, D.; Koppmann, R. Volatile organic compounds in the exhaled breath of young patients with cystic fibrosis. Eur. Respir. J. 2006, 27, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Nowak, D.; Kasielski, M.; Antczak, A.; Pietras, T.; Bialasiewicz, P. Increased content of thiobarbituric acid-reactive substances and hydrogen peroxide in the expired breath condensate of patients with stable chronic obstructive pulmonary disease: No significant effect of cigarette smoking. Respir. Med. 1999, 93, 389–396. [Google Scholar] [CrossRef]
- Kostikas, K.; Papatheodorou, G.; Psathakis, K.; Panagou, P.; Loukides, S. Oxidative stress in expired breath condensate of patients with COPD. Chest 2003, 124, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Morozov, V.N.; Nikolaev, A.A.; Shlyapnikov, Y.M.; Mikheev, A.Y.; Shlyapnikova, E.A.; Bagdasaryan, T.R.; Burmistrova, I.A.; Smirnova, T.G.; Andrievskaya, I.Y.; Larionova, E.E.; et al. Non-invasive approach to diagnosis of pulmonary tuberculosis using microdroplets collected from exhaled air. J. Breath Res. 2018, 12, 036010. [Google Scholar] [CrossRef] [PubMed]
- FDA. InspectIR COVID-19 Breathalyzer—Letter of Authorization. 2022. Available online: https://www.fda.gov/media/157720/download (accessed on 20 June 2022).
- Hancock, G.; Sharma, S.; Galpin, M.; Lunn, D.; Megson, C.; Peverall, R.; Richmond, G.; Ritchie, G.A.D.; Owen, K.R. The correlation between breath acetone and blood betahydroxybutyrate in individuals with type 1 diabetes. J. Breath Res. 2020, 15, 017101. [Google Scholar] [CrossRef]
- Ferrandino, G.; Orf, I.; Smith, R.; Calcagno, M.; Thind, A.K.; Debiram-Beecham, I.; Williams, M.; Gandelman, O.; de Saedeleer, A.; Kibble, G.; et al. Breath Biopsy Assessment of Liver Disease Using an Exogenous Volatile Organic Compound-Toward Improved Detection of Liver Impairment. Clin. Transl. Gastroenterol. 2020, 11, e00239. [Google Scholar] [CrossRef]
- Altomare, D.F.; Di Lena, M.; Porcelli, F.; Trizio, L.; Travaglio, E.; Tutino, M.; Dragonieri, S.; Memeo, V.; de Gennaro, G. Exhaled volatile organic compounds identify patients with colorectal cancer. Br. J. Surg. 2013, 100, 144–150.e27. [Google Scholar] [CrossRef]
- Adam, M.E.; Fehervari, M.; Boshier, P.R.; Chin, S.T.; Lin, G.P.; Romano, A.; Kumar, S.; Hanna, G.B. Mass-Spectrometry Analysis of Mixed-Breath, Isolated-Bronchial-Breath, and Gastric-Endoluminal-Air Volatile Fatty Acids in Esophagogastric Cancer. Anal. Chem. 2019, 91, 3740–3746. [Google Scholar] [CrossRef]
- Clinicaltrials.gov. PAN-study: Pan-Cancer Early Detection Study (PAN). 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT03756597 (accessed on 15 August 2022).
- Kauczor, H.U.; Bonomo, L.; Gaga, M.; Nackaerts, K.; Peled, N.; Prokop, M.; Remy-Jardin, M.; von Stackelberg, O.; Sculier, J.P. ESR/ERS white paper on lung cancer screening. Eur. Radiol. 2015, 25, 2519–2531. [Google Scholar] [CrossRef]
- Aberle, D.R.; Adams, A.M.; Berg, C.D.; Black, W.C.; Clapp, J.D.; Fagerstrom, R.M.; Gareen, I.F.; Gatsonis, C.; Marcus, P.M.; Sicks, J.D. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef]
- Lung Cancer Indicator Detection (LuCID). 2015. Available online: https://clinicaltrials.gov/ct2/show/NCT02612532 (accessed on 1 June 2022).
- Handa, H.; Usuba, A.; Maddula, S.; Baumbach, J.I.; Mineshita, M.; Miyazawa, T. Exhaled breath analysis for lung cancer detection using ion mobility spectrometry. PLoS ONE 2014, 9, e114555. [Google Scholar] [CrossRef] [PubMed]
- Smyth, R.J.; Toomey, S.M.; Sartori, A.; O’Hanrahan, E.; Cuffe, S.D.; Breathnach, O.S.; Morgan, R.K.; Hennessy, B.T. Brief Report on the Detection of the EGFR T790M Mutation in Exhaled Breath Condensate from Lung Cancer Patients. J. Thorac. Oncol. 2018, 13, 1213–1216. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.J.; Toomey, S.; Smyth, R.; Madden, S.F.; Workman, J.; Cummins, R.; Sheehan, K.; Fay, J.; Naidoo, J.; Breathnach, O.S.; et al. Exhaled Breath Condensate (EBC) analysis of circulating tumour DNA (ctDNA) using a lung cancer specific UltraSEEK oncogene panel. Lung Cancer 2022, 168, 67–73. [Google Scholar] [CrossRef] [PubMed]
- St John, E.R.; Balog, J.; McKenzie, J.S.; Rossi, M.; Covington, A.; Muirhead, L.; Bodai, Z.; Rosini, F.; Speller, A.V.M.; Shousha, S.; et al. Rapid evaporative ionisation mass spectrometry of electrosurgical vapours for the identification of breast pathology: Towards an intelligent knife for breast cancer surgery. Breast Cancer Res. 2017, 19, 59. [Google Scholar] [CrossRef] [PubMed]
- Tzafetas, M.; Mitra, A.; Paraskevaidi, M.; Bodai, Z.; Kalliala, I.; Bowden, S.; Lathouras, K.; Rosini, F.; Szasz, M.; Savage, A.; et al. The intelligent knife (iKnife) and its intraoperative diagnostic advantage for the treatment of cervical disease. Proc. Natl. Acad. Sci. USA 2020, 117, 7338–7346. [Google Scholar] [CrossRef]
- Koundouros, N.; Karali, E.; Tripp, A.; Valle, A.; Inglese, P.; Perry, N.J.S.; Magee, D.J.; Anjomani Virmouni, S.; Elder, G.A.; Tyson, A.L.; et al. Metabolic Fingerprinting Links Oncogenic PIK3CA with Enhanced Arachidonic Acid-Derived Eicosanoids. Cell 2020, 181, 1596–1611. [Google Scholar] [CrossRef]
- Pérez-Sánchez, C.; Barbarroja, N.; Pantaleão, L.C.; López-Sánchez, L.M.; Ozanne, S.E.; Jurado-Gámez, B.; Aranda, E.; Lopez-Pedrera, C.; Rodríguez-Ariza, A. Clinical Utility of microRNAs in Exhaled Breath Condensate as Biomarkers for Lung Cancer. J. Pers. Med. 2021, 11, 111. [Google Scholar] [CrossRef]
- Xie, H.; Chen, J.; Lv, X.; Zhang, L.; Wu, J.; Ge, X.; Yang, Q.; Zhang, D.; Chen, J. Clinical Value of Serum and Exhaled Breath Condensate miR-186 and IL-1β Levels in Non-Small Cell Lung Cancer. Technol. Cancer Res. Treat. 2020, 19, 1533033820947490. [Google Scholar] [CrossRef]
- Ibrahim, F.K.; Ali-Labib, R.; Galal, I.H.; Mahmoud, H.M. MicroRNA-155 expression in exhaled breath condensate of patients with lung cancer. Egypt. J. Chest Dis. Tuberc. 2017, 66, 687–691. [Google Scholar] [CrossRef]
- de Vries, R.; Muller, M.; van der Noort, V.; Theelen, W.S.M.E.; Schouten, R.D.; Hummelink, K.; Muller, S.H.; Wolf-Lansdorf, M.; Dagelet, J.W.F.; Monkhorst, K.; et al. Prediction of response to anti-PD-1 therapy in patients with non-small-cell lung cancer by electronic nose analysis of exhaled breath. Ann. Oncol. 2019, 30, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Buma, A.I.G.; Muller, M.; de Vries, R.; Sterk, P.J.; van der Noort, V.; Wolf-Lansdorf, M.; Farzan, N.; Baas, P.; van den Heuvel, M.M. eNose analysis for early immunotherapy response monitoring in non-small cell lung cancer. Lung Cancer 2021, 160, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Di Giacomo, A.M.; Danielli, R.; Guidoboni, M.; Calabrò, L.; Carlucci, D.; Miracco, C.; Volterrani, L.; Mazzei, M.A.; Biagioli, M.; Altomonte, M.; et al. Therapeutic efficacy of ipilimumab, an anti-CTLA-4 monoclonal antibody, in patients with metastatic melanoma unresponsive to prior systemic treatments: Clinical and immunological evidence from three patient cases. Cancer Immunol. Immunother. 2009, 58, 1297–1306. [Google Scholar] [CrossRef] [PubMed]
- Jia, W.; Gao, Q.; Han, A.; Zhu, H.; Yu, J. The potential mechanism, recognition and clinical significance of tumor pseudoprogression after immunotherapy. Cancer Biol. Med. 2019, 16, 655–670. [Google Scholar] [CrossRef]

| Analytical Method | No. of Subjects | Results | Ref. |
|---|---|---|---|
| GC-MS | 12 LC subject, 17 controls | Increased levels of acetone, methyl ethyl ketone, n-propanol in LC patients compared to HC | [12] |
| GC-MS | 87 patients with LC (67 patients had PLC, 15 patients had MLC), 91 patients had no evidence of LC, 41 HC | Sensitivity 90% (60/67), specificity 83% (34/41), cross-validation: sensitivity 85% (57/67), specificity 81% (33/41), smokers/ex-smokers had no effect on sensitivity, histology, TNM staging had no effect on specificity VOCs identified: butane, pentane, 5-methyl decane, 3-methyl tridecane, 7-methyl trodecane, 4-methyl octane, 2-methyl hexane | [14] |
| aGC-MS | NSCLC (pre- and post-surgery) = 36 and 24, respectively, 35 healthy smoker, 50 HC | Increased levels of isoprene, 2-methyl pentane in NSCLC vs. COPD cohort Reduced levels of toluene, heptane, benzene in NSCLC cohort vs. control smokers cohort Only isoprene decreased post-surgery | [15] |
| GC-MS | 193 LC (128 prediction set, 65 test set); 211 HC (141 prediction set, 70 test set); 80 post-surgeries | Prediction of LC: Sensitivity 85%, specificity 80%, no difference between stage | [16] |
| SPME, GC on cell culture and breath analysis | 29 LC, 13 HC, 7 chronic bronchitis | Prediction of LC: Sensitivity 86%, control specificity 69%, chronic bronchitis specifically 71%, PPV 80.6%, NPV 78% | [17] |
| PTR-MS + SPME GC-MS | 220 LC (68 smokers,129 ex-smokers, 23 never smokers); 441 HC (84 smokers, 86 ex-smokers, 221 never smokers) | Decreased levels of isoprene, acetone, methanol in LC patients compared to controls (PTR-MS): 100% specificity For sensitivity: A:50% when add 2-butanone, benzaldehyde, 2,3-butanedione, 1-propranolol. B: 71% when add 3-hydroxy-2-butanone, 3-butyn-2-ol, 2-methyl-butane, 2-methyl-2-butene, acetophenone, 1-cyclopentene, methyl propyl sulphide, tetramethyl urea, n-pentanal, 1-methyl-1,33-cyclopentadiene, 2,3-dimethyl-2butanol. C sensitivity: 80% when add 1,2,3,4-tetrahydro-isoquinoline, 3,7-dimethyl-undecane, cyclobutyl-benzene, butyl acetate, ethylenimine, n-undecane | [18] |
| SPME + GC-MS | 12 LC, 12 Healthy smokers, 12 Healthy never smokers | Higher levels of pentanal, hexanal, octanal, nonanal in LC patients vs. controls No significant difference between SCLC and NSCLC Pentanal: sensitivity 75%, specificity 95.8% | [19] |
| SPME, GC on cell culture and exhaled breath | 85 LC, 70, benign lung disease, 88 HC | Significant difference in AUC > 0.6 and p < 0.01 in levels of 8-hexylpentadecane, 2-pentadecanone, 5-(1-methyl-)propylnonane, 3,7-dimethylpentadecanone between adenocarcinoma and squamous Correct classification of LC in 96.5% of cases, 34.3% of HC classified as benign and 33.3% of advanced LC incorrectly classified as early-stage LC | [20] |
| SPME + GC-MS | 72 subjects with pulmonary nodules- 19 benign and 53 LC | Significant difference in 1-octene levels between benign and LC patients (p = 0.0486). No significant difference between stages and histologies. | [21] |
| TD-GC-MS | 60 LC, 176 HC | Accuracy: 85 ± 4% Sensitivity: 83 ± 8% Specificity: 85 ± 7% AUC: 0.89 ± 0.06 | [22] |
| SIFT-MS | 148 LC, 168 HC | Accuracy: 0.92, Sensitivity: 0.96, Specificity: 0.88, AUC: 0.98 | [23] |
| HPPI-TOFMS | 157 LC, 368 HC | Accuracy 89.1%, Sensitivity 89.2%, Specificity 89.1%, AUC 0.952 VOCs: Acetaldehyde, 2-hydroxyacetaldehyde, isoprene, pentanal, butyric acid, toluene, 2,5-dimethylfuran, cyclohexanone, hexanal, heptanal, acetophenone, propylcyclohexane, octanal, nonanal, decanal, 2,3-dimethyldecane | [24] |
| Ion molecule reaction mass spectrometry | 36 LC adenocarcinoma patients 25 squamous cell LC patients 52 colon cancer 45 HCC | Adenocarcinoma: Sensitivity: 86%, Specificity: 84% Squamous: Sensitivity 88%, Specificity 84% Colon: Sensitivity 96%, Specificity 73% | [25] |
| SPME and GC-MS | 51 confirmed LC 38 with pathological findings suggestive of LC but not confirmed | CA+ versus HC: Accuracy 89%, AUC 0.94 CA- vs. HC: Accuracy 82%, AUC 0.906 | [26] |
| GC-MS | 108 LC patients 121 HC | Sensitivity: 80% Specificity 91.23% | [27] |
| TD-GC-MS | 210 subjects in total (control group n = 89, COPD group n = 40, LC group n = 81) | Nanoic acid as biomarker for LC: Sensitivity: 32% Specificity: 88% PPV: 62% NPV: 67% | [28] |
| Silicon microchip Mass spectrometry | 34 LC, 187 HC | Decrease in ECC after lung resection | [29] |
| GC-TOF-MS | 48 LC, 130 Risk factor subjects (active smokers and ex-smokers), 61 HC (non-smokers without respiratory disease) | UA panel: LC versus RF: Sensitivity 58.1%, specificity 63.7% Control vs. LC Sensitivity 83.7%, Specificity 83.3% Control versus RF: Sensitivity 63.7%, Specificity 69.4% DA panel: LC versus RF: Sensitivity 75.5%, specificity 70.5% Control vs. LC: Sensitivity 77.5%, Specificity 89.8% Control versus RF: Sensitivity 79.5%, Specificity 71.4% | [30] |
| FT-ICR-MS | 85 patients untreated LC, 34 BPN, 85 HC | Six carbonyl compounds (C4H8O, C5H10O, C2H4O2, C4H8O2, C6H10O2, C9H16O2) had significantly elevated concentrations in lung cancer patients vs. controls. LC versus benign nodules: Sensitivity 100%, Specificity 64% LC versus smokers: Sensitivity 100%, Specificity 86% LC versus non-smokers: Sensitivity 96%, Specificity 100% | [31] |
| SPME/GC-MS | 138 subjects suspected of LC inc. 71 subsequently confirmed to have LC | AUC = 0.80, sensitivity 72.5% and specificity 75.8% at the flex point. | [32] |
| FT-ICR-MS | 97 LC, 88 HC, 32 BPN | VOCs elevated in LC: 2-butanone, 2-hydroxyacetaldehyde, 3-hydroxy-2-butanone, 4-hydroxyhexanal Sensitivity 89.8% Specificity 81.3% | [33] |
| FT-ICR-MS | 88 HC, 107 LC, 40 BPD, 7 solitary lung metastases | Four ECC elevated: 2-butanone, 3-hydroxy-2-butanone, 4-hydroxyhexanal, 2-hydroxyacetaldehyde Sensitivity 83% Specificity 74% | [34] |
| FT-ICR-MS | 31 LC patients pre- and post-resection, 187 HC | Decrease in four ECCs post-surgery: 2-butanone, 3-hydroxy-2-butanone, 2-hydroxyacetaldehyde, 4-hydroxyhexanal | [35] |
| SPME-GC/MS | 123 LC patients 361 HC | Sensitivity 63.5% Specificity 72.4% AUC 0.65 | [36] |
| SPME-GC | 13 HC, 29 LC patients, and 7 patients with chronic bronchitis | Sensitivity 86.2% Specificity 70% PPV 80.6% NPV 77.8% VOCs: Styrene, decane, isoprene, benzene, undecane, 1-hexene, hexanol, propyl benzene, 1,2,4-trimethyl benzene, heptanal, methyl cyclopentane | [17] |
| GC/MS, Na nose Sensor array | 39 LC patients | VOCs: Styrene, α-Phellandrene (5-isopropyl-2-methyl-1,3-cyclohexadiene), dodecane,4-methyl PPV 86% Sensitivity 93% Specificity 85% | [37] |
| GC-MS | Discovery phase: 301 subjects screened for LC Validation phase: 161 subjects | MAGIIC biomarker (C4/C5 derivatives) LC Sensitivity 75.4% LC Specificity 85% LC Accuracy 84% | [38] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keogh, R.J.; Riches, J.C. The Use of Breath Analysis in the Management of Lung Cancer: Is It Ready for Primetime? Curr. Oncol. 2022, 29, 7355-7378. https://doi.org/10.3390/curroncol29100578
Keogh RJ, Riches JC. The Use of Breath Analysis in the Management of Lung Cancer: Is It Ready for Primetime? Current Oncology. 2022; 29(10):7355-7378. https://doi.org/10.3390/curroncol29100578
Chicago/Turabian StyleKeogh, Rachel J., and John C. Riches. 2022. "The Use of Breath Analysis in the Management of Lung Cancer: Is It Ready for Primetime?" Current Oncology 29, no. 10: 7355-7378. https://doi.org/10.3390/curroncol29100578
APA StyleKeogh, R. J., & Riches, J. C. (2022). The Use of Breath Analysis in the Management of Lung Cancer: Is It Ready for Primetime? Current Oncology, 29(10), 7355-7378. https://doi.org/10.3390/curroncol29100578





