The Implementation of a Primary HPV Self-Testing Cervical Screening Program in Malaysia through Program ROSE—Lessons Learnt and Moving Forward
Abstract
1. Tailoring the Global Roadmap towards Cervical Cancer Elimination to the Real-World Setting
2. The Malaysian Landscape
3. Overcoming Barriers to Implementing the WHO Cervical Cancer Elimination Targets
3.1. Political Commitment and Costs Justification
3.2. Infrastructure and Healthcare Providers for Cervical Screening
3.3. Knowledge and Acceptance of Cervical Screening
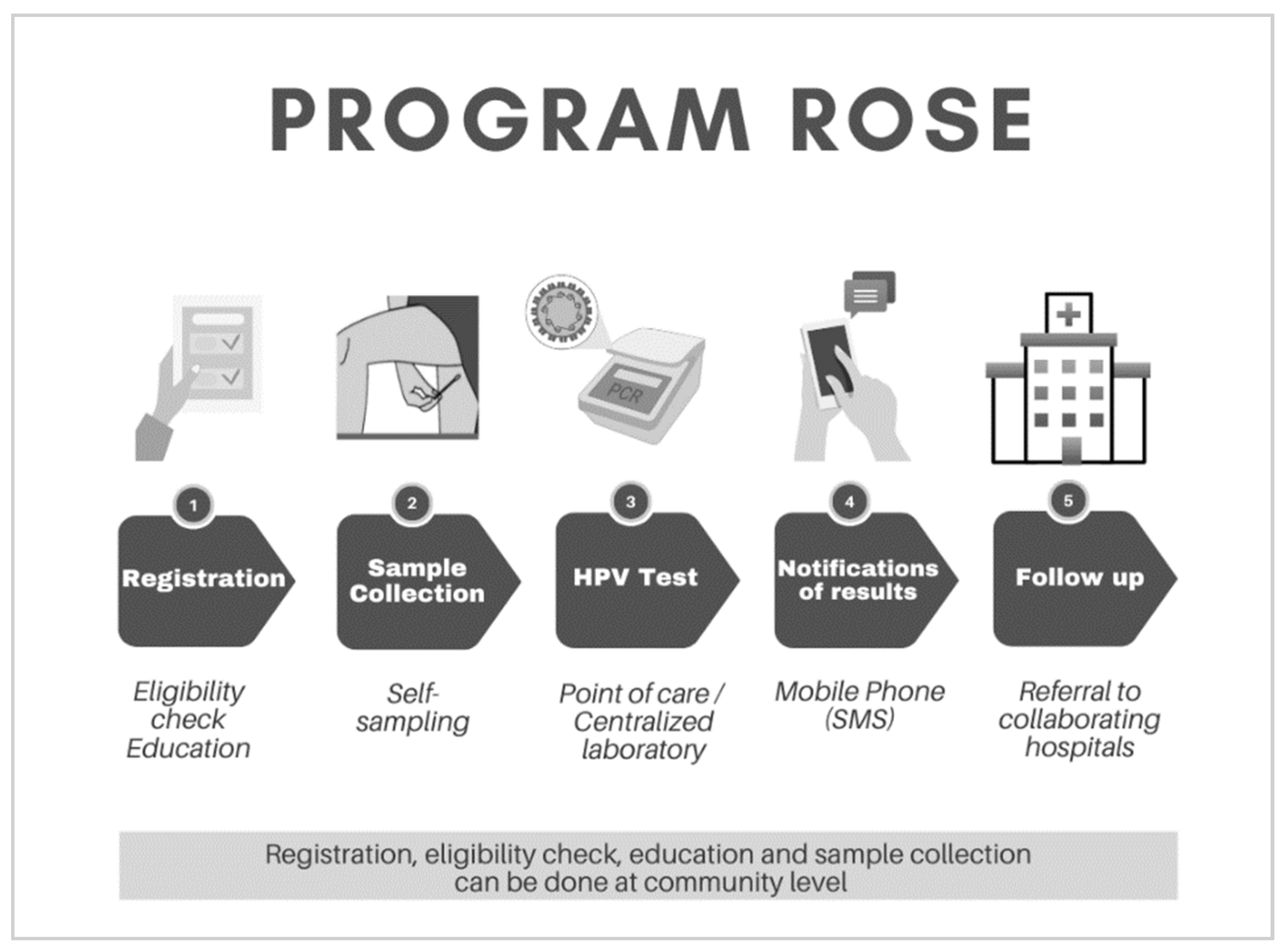
4. The Evolution of Program ROSE (Removing Obstacles to Cervical Screening)
4.1. Accelerating Innovation through Collaboration
4.2. Acceptability of Self-Testing for HPV Testing in Malaysia
4.3. Success Measured by Linkage to Care
5. Looking Forward and Concluding Remarks
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- World Health Organization. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Canfell, K. Towards the global elimination of cervical cancer. Papillomavirus Res. 2019, 8, 100170. [Google Scholar] [CrossRef] [PubMed]
- Dorji, T.; Nopsopon, T.; Tamang, S.T.; Pongpirul, K. Human papillomavirus vaccination uptake in low-and middle-income countries: A meta-analysis. eClinicalMedicine 2021, 34, 100863. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health Emergencies List; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- UNHCR. Global Trends Forced Displacement in 2021; The UN Refugee Agency: Copenhagen, Denmark, 2022. [Google Scholar]
- World Health Organization. WHO Launches Appeal to Respond to Urgent Health Needs in the Greater Horn of Africa. Available online: https://www.who.int/news/item/02-08-2022-who-launches-appeal-to-respond-to-urgent-health-needs-in-the-greater-horn-of-africa (accessed on 23 August 2022).
- WFP; FAO. Hunger Hotspots. FAO-WFP Early Warnings on Acute Food Insecurity: June to September 2022 Outlook; WFP: Rome, Italy, 2022. [Google Scholar]
- Zhao, S.; Huang, L.; Basu, P.; Domingo, E.J.; Supakarapongkul, W.; Ling, W.Y.; Ocviyanti, D.; Rezhake, R.; Qiao, Y.; Tay, E.H.; et al. Cervical cancer burden, status of implementation and challenges of cervical cancer screening in Association of Southeast Asian Nations (ASEAN) countries. Cancer Lett. 2022, 525, 22–32. [Google Scholar] [CrossRef]
- Quek, D. The Malaysian Health Care System: A Review. In Proceedings of the Intensive Workshop on Health Systems in Transition, Kuala Lumpur, Malaysia, 29–30 April 2009. [Google Scholar]
- Ministry of Health Malaysia. National Strategic Plan for Cancer Control Programme 2021–2025; Ministry of Health Malaysia: Putrajaya, Malaysia, 2021. [Google Scholar]
- Ministry of Health Malaysia. National Cancer Control Blueprint (NCCB) 2008–2015; Ministry of Health Malaysia: Putrajaya, Malaysia, 2008. [Google Scholar]
- Ministry of Health Malaysia. Family Health Development Division MOH. Annual Report 2019; Ministry of Health Malaysia: Putrajaya, Malaysia, 2019. [Google Scholar]
- UNESCO Institute of Statistics. Malaysia|UNESCO UIS. Education and Literacy. 2022. Available online: http://uis.unesco.org/en/country/my (accessed on 23 August 2022).
- Rao, S.R.; Kampan, N.; Chew, K.T.; Shafiee, M.N. The impact of the COVID-19 pandemic on the national HPV immunization program in Malaysia. Front. Public Health 2022, 10, 907720. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia. Annual Report 2020; Ministry of Health Malaysia: Putrajaya, Malaysia, 2020. [Google Scholar]
- Mohd, Z.S. HPV Vaccination and Screening in APEC during the COVID-19 Pandemic: Status Update, Lessons Learned, Next Steps. APEC Policy Dialogue Cerv. Cancer 2020, 2020. [Google Scholar]
- Ministry of Health Malaysia. Guidelines for Primary HPV Testting in Cervical Cancer Screening in Malaysia; Ministry of Health Malaysia: Putrajaya, Malaysia, 2019. [Google Scholar]
- Family Health Development Division. Guidebook for Cervical Cancer Screening; Ministry of Health Malaysia: Putrajaya, Malaysia, 2019. [Google Scholar]
- Othman, N.H.; Rebolj, M. Challenges to Cervical Screening in a Developing Country: The Case of Malaysia. Asian Pac. J. Cancer Prev. 2009, 10, 747–752. [Google Scholar]
- Ministry of Health Malaysia. Malaysia’s Health 2004; Ministry of Health Malaysia: Putrajaya, Malaysia, 2004. [Google Scholar]
- Ministry of Health Malaysia. Family Health Development Division. Annual Report 2017; Ministry of Health Malaysia: Putrajaya, Malaysia, 2017. [Google Scholar]
- Ministry of Health Malaysia. Health Facts 2021; Ministry of Health Malaysia: Putrajaya, Malaysia, 2021. [Google Scholar]
- Parliament of Malaysia: House of Representatives. In Proceedings of the Parliamentary Business of the 3rd Session of Fourteenth Parliament 2020, 2nd Meeting, Kuala Lumpur, Malaysia, 13 July–27 August 2020.
- Ministry of Health Malaysia. Progress in the Implementation of the Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem and Its Associated Goals and Targets for the Period 2020–2030; Union for International Cancer Contro (UICC): Geneva, Switzerland, 2022. [Google Scholar]
- Ronco, G.; Dillner, J.; Elfstrom, K.M.; Tunesi, S.; Snijders, P.J.; Arbyn, M.; Kitchener, H.; Segnan, N.; Gilham, C.; Giorgi-Rossi, P.; et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: Follow-up of four European randomised controlled trials. Lancet 2014, 383, 524–532. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guideline for Screening and Treatment of Cervical Pre-Cancer Lesions for Cervical Cancer Prevention, 2nd ed.; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Casas, C.P.R.; Albuquerque, R.C.R.; Loureiro, R.B.; Gollner, A.M.; Freitas, M.G.; Duque, G.; Viscondi, J.Y.K. Cervical cancer screening in low- and middle-income countries: A systematic review of economic evaluation studies. Clinics 2022, 77, 100080. [Google Scholar] [CrossRef]
- Brisson, M.; Kim, J.J.; Canfell, K.; Drolet, M.; Gingras, G.; Burger, A.E.; Martin, D.; Simms, K.T.; Bénard, É; Boily, M.-C.; et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: A comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet 2020, 395, 575–590. [Google Scholar] [CrossRef]
- Canfell, K.; Kim, J.J.; Brisson, M.; Keane, A.; Simms, K.T.; Caruana, M.; Burger, A.E.; Martin, D.; Nguyen, D.T.N.; Bénard, É; et al. Mortality impact of achieving WHO cervical cancer elimination targets: A comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet 2020, 395, 591–603. [Google Scholar] [CrossRef]
- Khoo, S.P.; Lim, W.T.; Rajasuriar, R.; Nasir, N.H.; Gravitt, P.; Woo, Y.L. The Acceptability and Preference of Vaginal Self-sampling for Human Papillomavirus (HPV) Testing among a Multi-ethnic Asian Female Population. Cancer Prev. Res. 2020, 14, 105–112. [Google Scholar] [CrossRef]
- Commonwealth Secretariat. Conquering Cervical Cancer in the Commonwealth: Addressing Myths and Misconceptions; UICC: Geneva, Switzerland, 2022. [Google Scholar]
- Ogilvie, G.S.; van Niekerk, D.; Krajden, M.; Smith, L.W.; Cook, D.; Gondara, L.; Ceballos, K.; Quinlan, D.; Lee, M.; Martin, R.E.; et al. Effect of Screening With Primary Cervical HPV Testing vs Cytology Testing on High-grade Cervical Intraepithelial Neoplasia at 48 Months: The HPV FOCAL Randomized Clinical Trial. JAMA 2018, 320, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Yong, C.; Hong, L.; Lee, K.; Krishnasamy, I.; Nasir, N.B.; Gravitt, P.; Lee, Y.; Woo, Y. Healthcare Providers’ Views on Cervical Screening: A Qualitative Study of Barriers to Cervical Screening in Malaysia. J. Glob. Oncol. 2018, 4, 214s. [Google Scholar] [CrossRef]
- Ma’Som, M.; Bhoo-Pathy, N.; Nasir, N.H.; Bellinson, J.; Subramaniam, S.; Ma, Y.; Yap, S.-H.; Goh, P.-P.; Gravitt, P.; Woo, Y.L. Attitudes and factors affecting acceptability of self-administered cervicovaginal sampling for human papillomavirus (HPV) genotyping as an alternative to Pap testing among multiethnic Malaysian women. BMJ Open 2016, 6, e011022. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Raifu, A.O.; Weiderpass, E.; Bray, F.; Anttila, A. Trends of cervical cancer mortality in the member states of the European Union. Eur. J. Cancer 2009, 45, 2640–2648. [Google Scholar] [CrossRef]
- Smith, M.; Canfell, K. Impact of the Australian National Cervical Screening Program in women of different ages. Med. J. Aust. 2016, 205, 359–364. [Google Scholar] [CrossRef]
- Alfaro, K.; Maza, M.; Cremer, M.; Masch, R.; Soler, M. Removing global barriers to cervical cancer prevention and moving towards elimination. Nat. Rev. Cancer 2021, 21, 607–608. [Google Scholar] [CrossRef]
- Burd, E.M. Human papillomavirus and cervical cancer. Clin. Microbiol. Rev. 2003, 16, 1–17. [Google Scholar] [CrossRef]
- Stanczuk, G.; Baxter, G.; Currie, H.; Lawrence, J.; Cuschieri, K.; Wilson, A.; Arbyn, M. Clinical validation of hrHPV testing on vaginal and urine self-samples in primary cervical screening (cross-sectional results from the Papillomavirus Dumfries and Galloway—PaVDaG study). BMJ Open 2016, 6, e010660. [Google Scholar] [CrossRef]
- Arbyn, M.; Smith, S.B.; Temin, S.; Sultana, F.; Castle, P. Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: Updated meta-analyses. BMJ 2018, 363, k4823. [Google Scholar] [CrossRef] [PubMed]
- Meijer, C.J.; Berkhof, J.; Castle, P.E.; Hesselink, A.T.; Franco, E.L.; Ronco, G.; Arbyn, M.; Bosch, F.X.; Cuzick, J.; Dillner, J.; et al. Guidelines for human papillomavirus DNA test requirements for primary cervical cancer screening in women 30 years and older. Int. J. Cancer 2009, 124, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Depuydt, C.; Benoy, I.; Bogers, J.; Cuschieri, K.; Schmitt, M.; Pawlita, M.; Geraets, D.; Heard, I.; Gheit, T.; et al. VALGENT: A protocol for clinical validation of human papillomavirus assays. J. Clin. Virol. 2016, 76 (Suppl. 1), S14–S21. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Simon, M.; Peeters, E.; Xu, L.; Meijer, C.J.; Berkhof, J.; Cuschieri, K.; Bonde, J.; Vanlencak, A.O.; Zhao, F.-H.; et al. 2020 list of human papillomavirus assays suitable for primary cervical cancer screening. Clin. Microbiol. Infect. 2021, 27, 1083–1095. [Google Scholar] [CrossRef]
- Mandelblatt, J.S.; Lawrence, W.F.; Womack, S.M.; Jacobson, D.; Yi, B.; Hwang, Y.-T.; Gold, K.; Barter, J.; Shah, K. Benefits and Costs of Using HPV Testing to Screen for Cervical Cancer. JAMA 2002, 287, 2372–2381. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woo, Y.L.; Khoo, S.P.; Gravitt, P.; Hawkes, D.; Rajasuriar, R.; Saville, M. The Implementation of a Primary HPV Self-Testing Cervical Screening Program in Malaysia through Program ROSE—Lessons Learnt and Moving Forward. Curr. Oncol. 2022, 29, 7379-7387. https://doi.org/10.3390/curroncol29100579
Woo YL, Khoo SP, Gravitt P, Hawkes D, Rajasuriar R, Saville M. The Implementation of a Primary HPV Self-Testing Cervical Screening Program in Malaysia through Program ROSE—Lessons Learnt and Moving Forward. Current Oncology. 2022; 29(10):7379-7387. https://doi.org/10.3390/curroncol29100579
Chicago/Turabian StyleWoo, Yin Ling, Su Pei Khoo, Patti Gravitt, David Hawkes, Reena Rajasuriar, and Marion Saville. 2022. "The Implementation of a Primary HPV Self-Testing Cervical Screening Program in Malaysia through Program ROSE—Lessons Learnt and Moving Forward" Current Oncology 29, no. 10: 7379-7387. https://doi.org/10.3390/curroncol29100579
APA StyleWoo, Y. L., Khoo, S. P., Gravitt, P., Hawkes, D., Rajasuriar, R., & Saville, M. (2022). The Implementation of a Primary HPV Self-Testing Cervical Screening Program in Malaysia through Program ROSE—Lessons Learnt and Moving Forward. Current Oncology, 29(10), 7379-7387. https://doi.org/10.3390/curroncol29100579




