Interventional Cardiology in Switzerland 2006
Summary
Zusammenfassung
Introduction
Methods
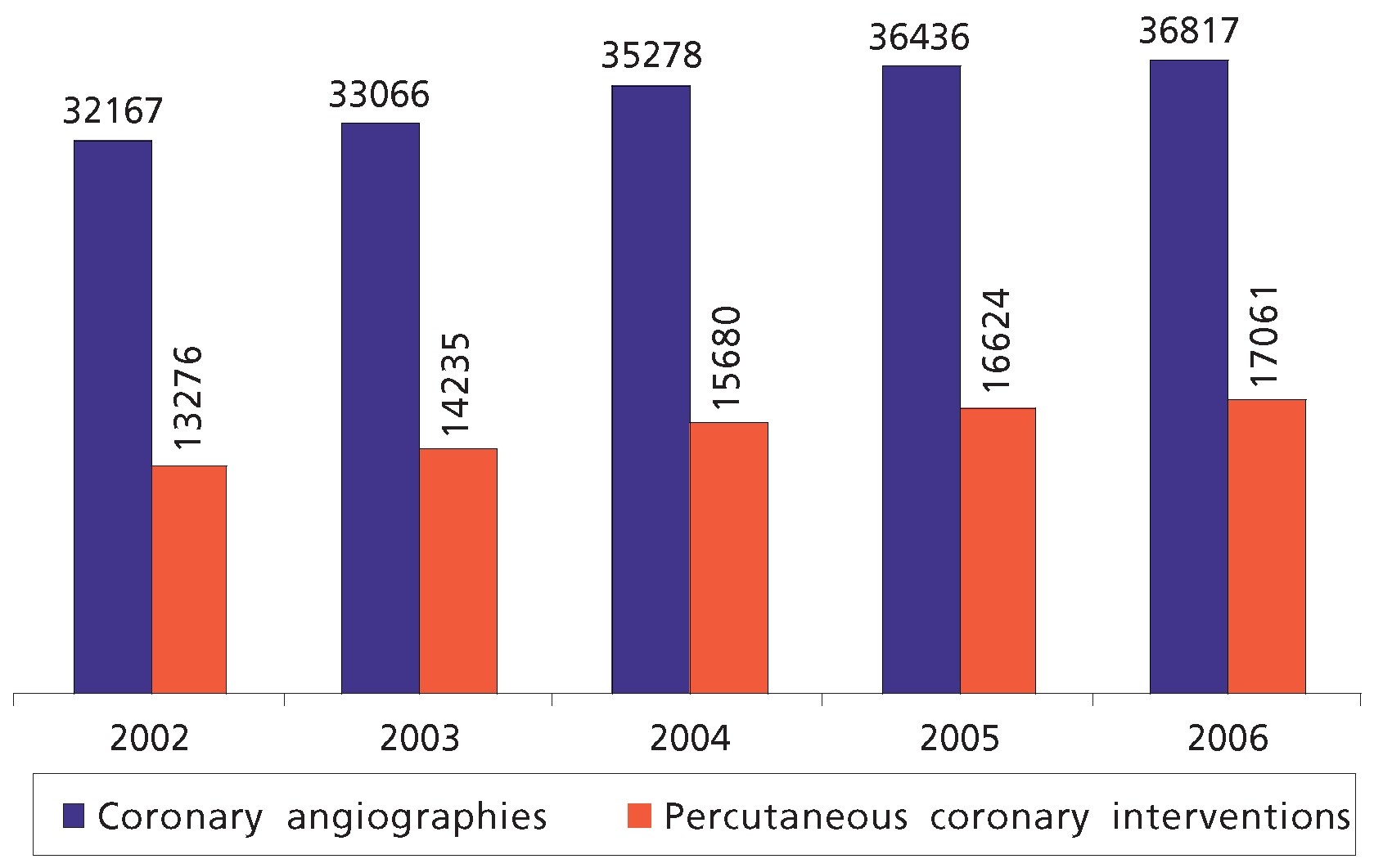
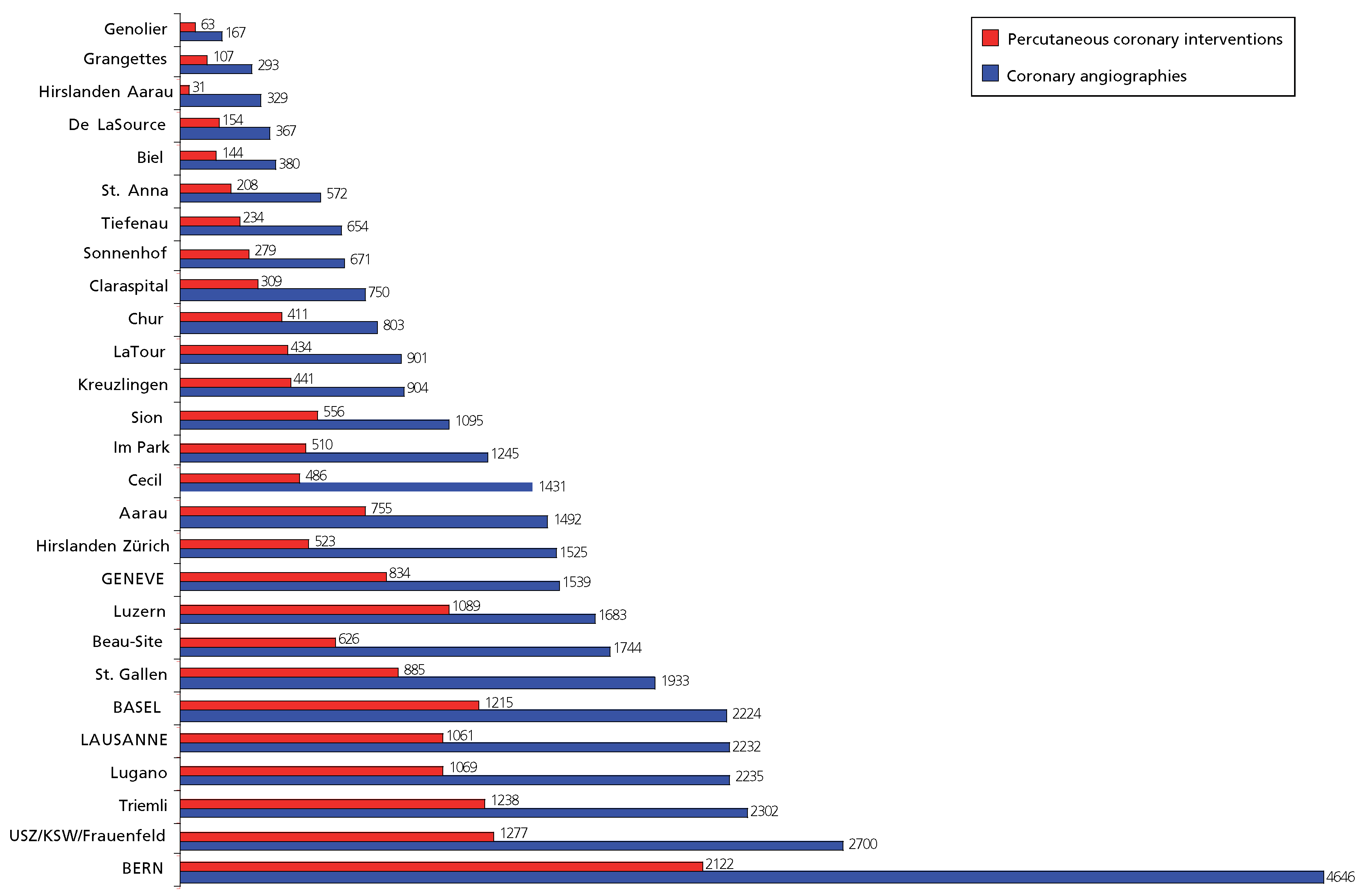
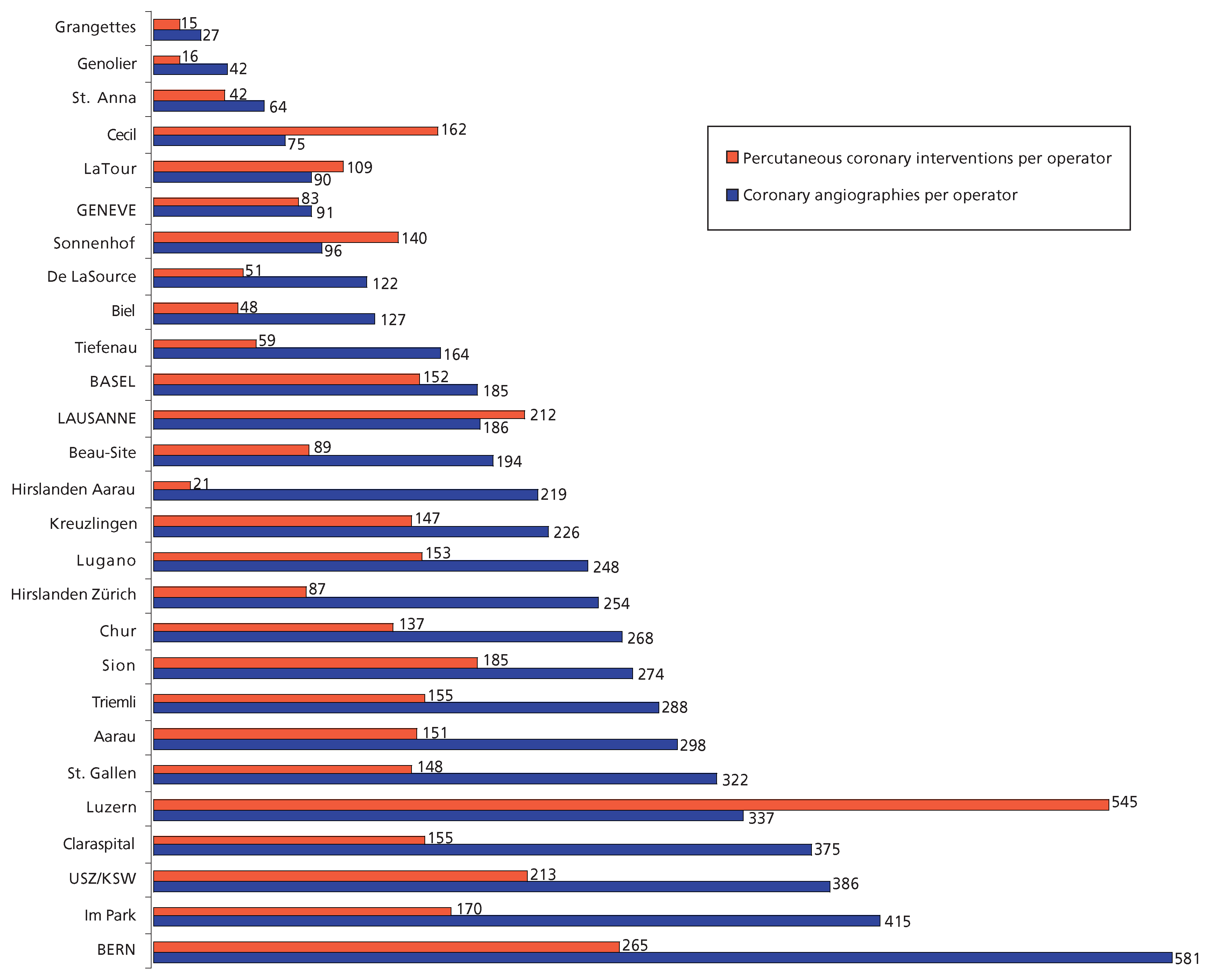
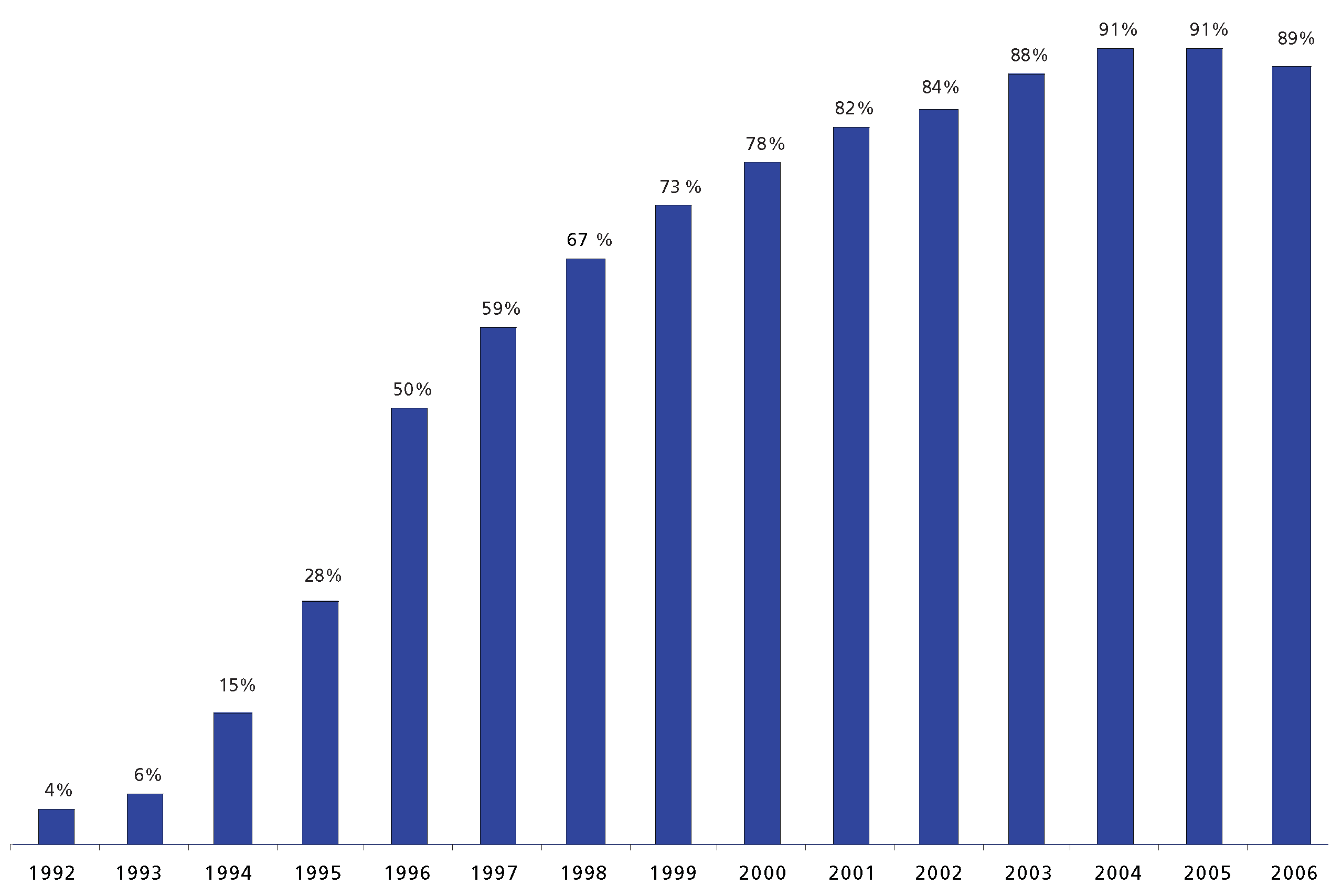
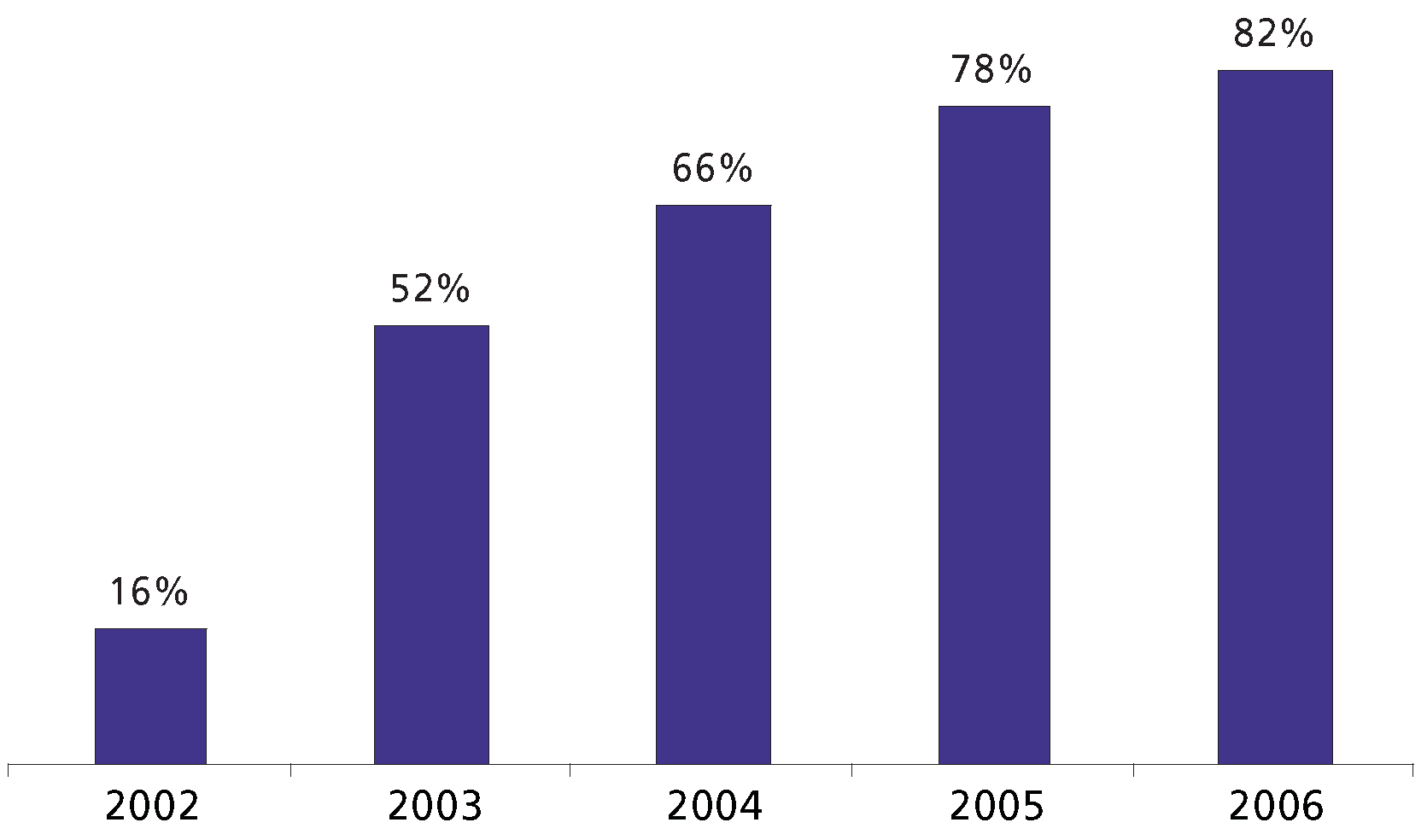
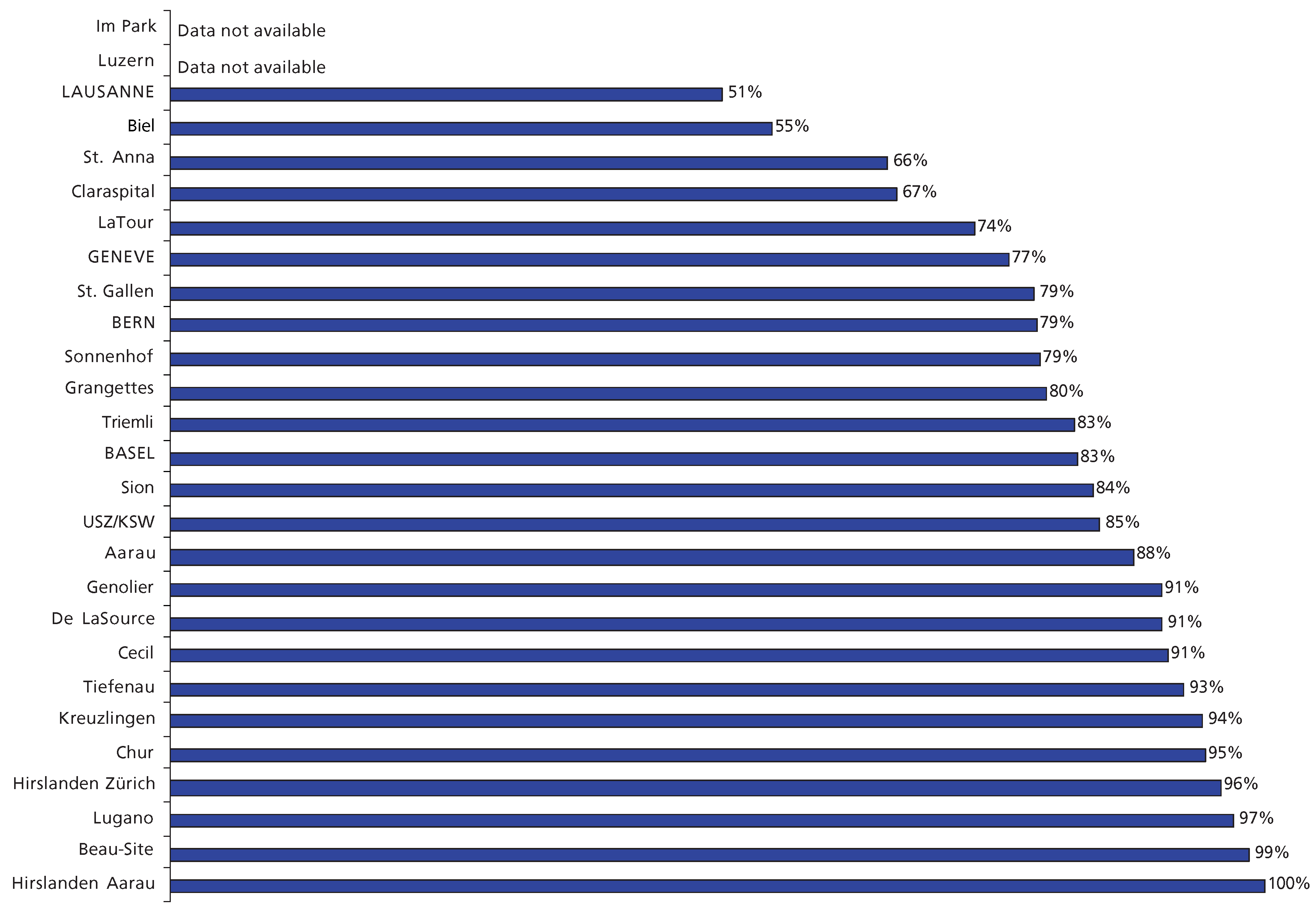
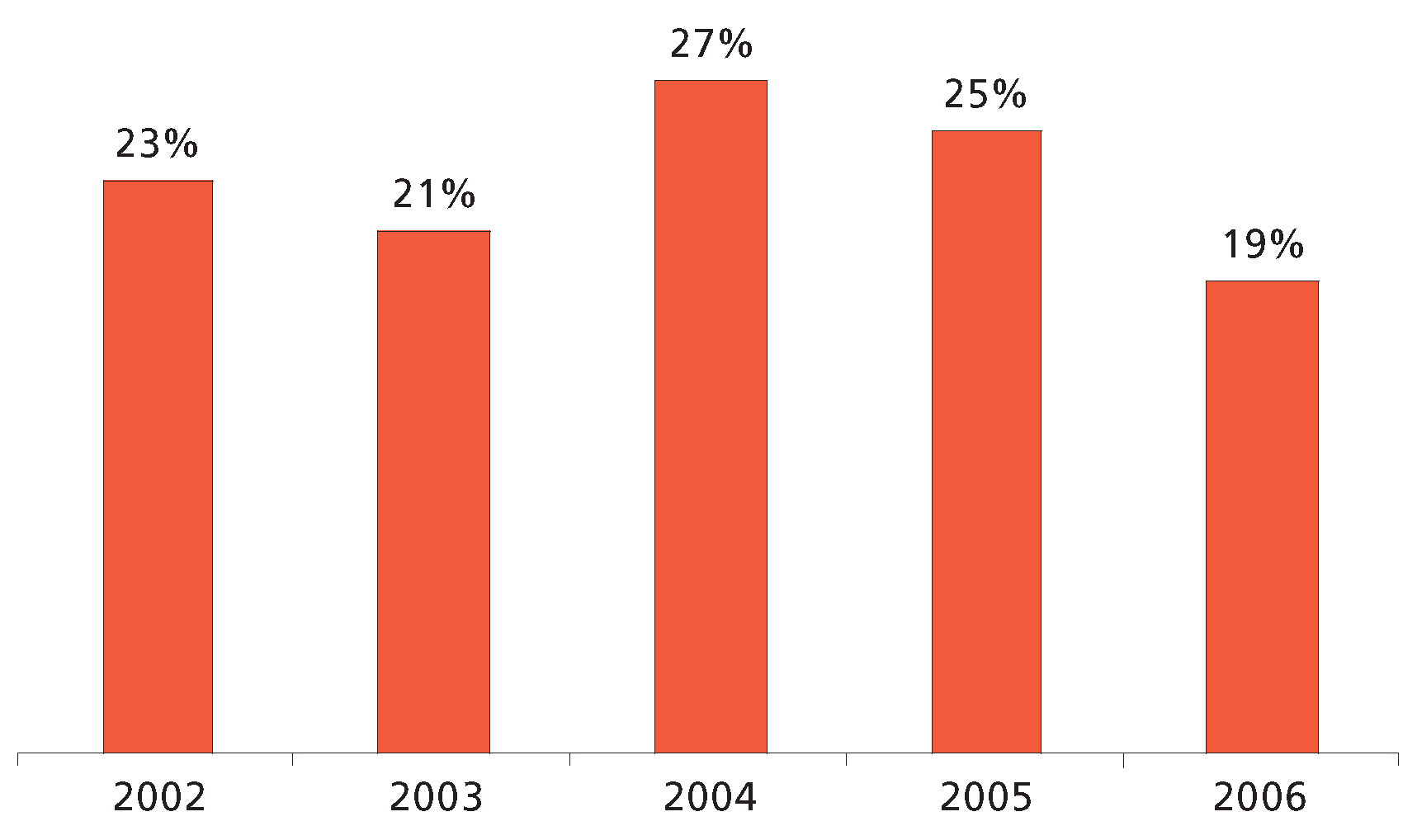
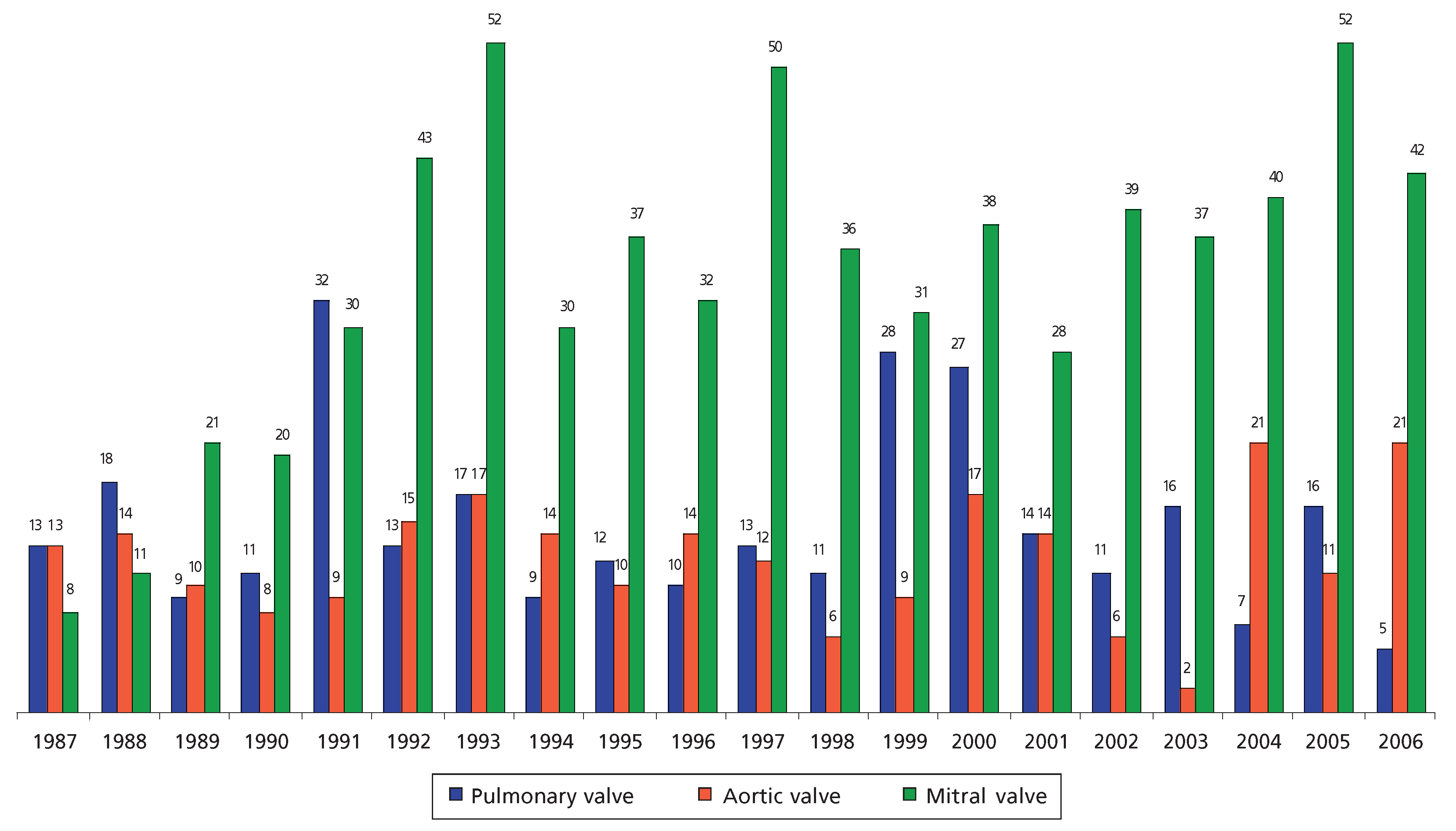
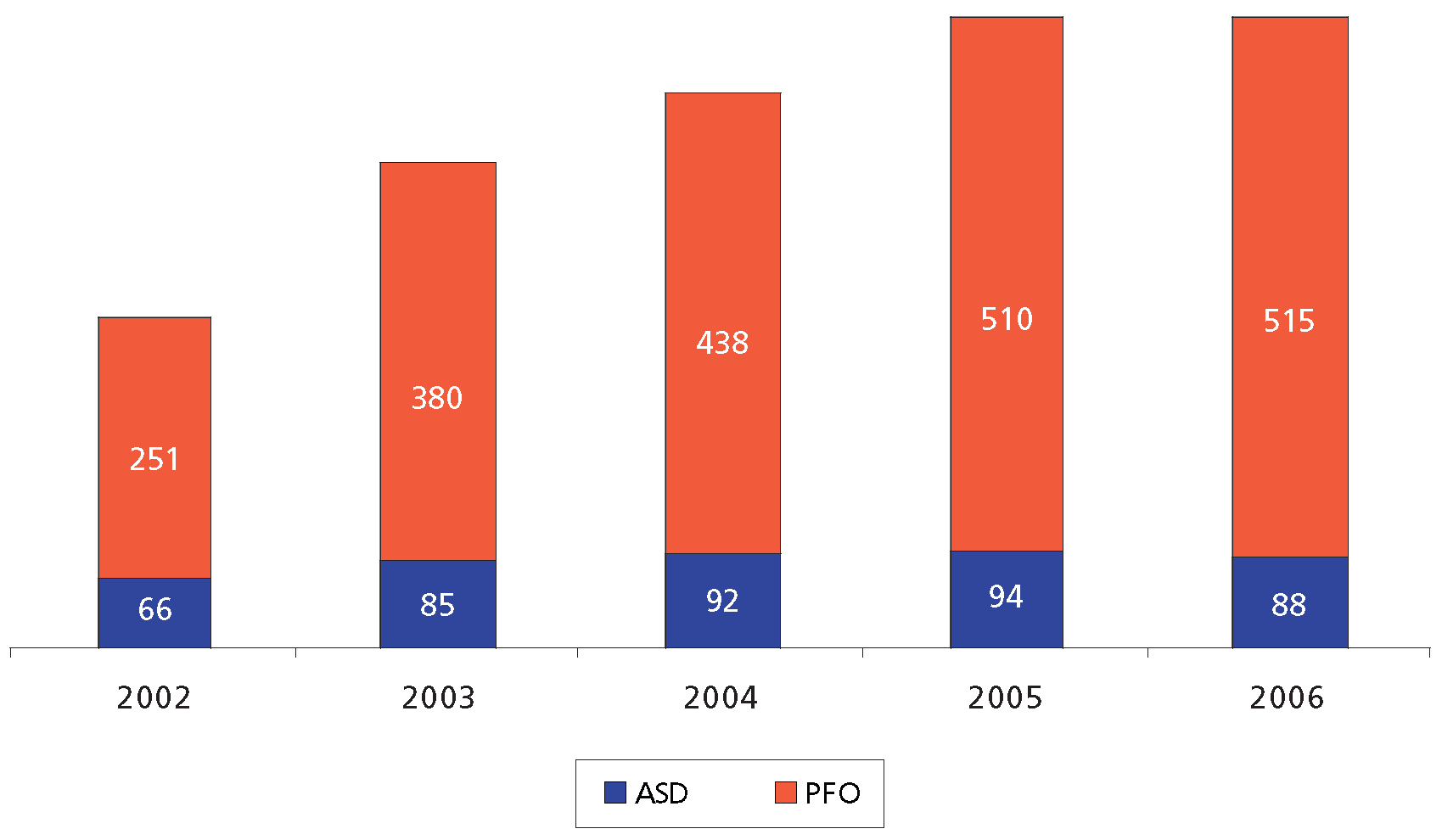
Results
Discussion
Limitations of the study
Conclusions
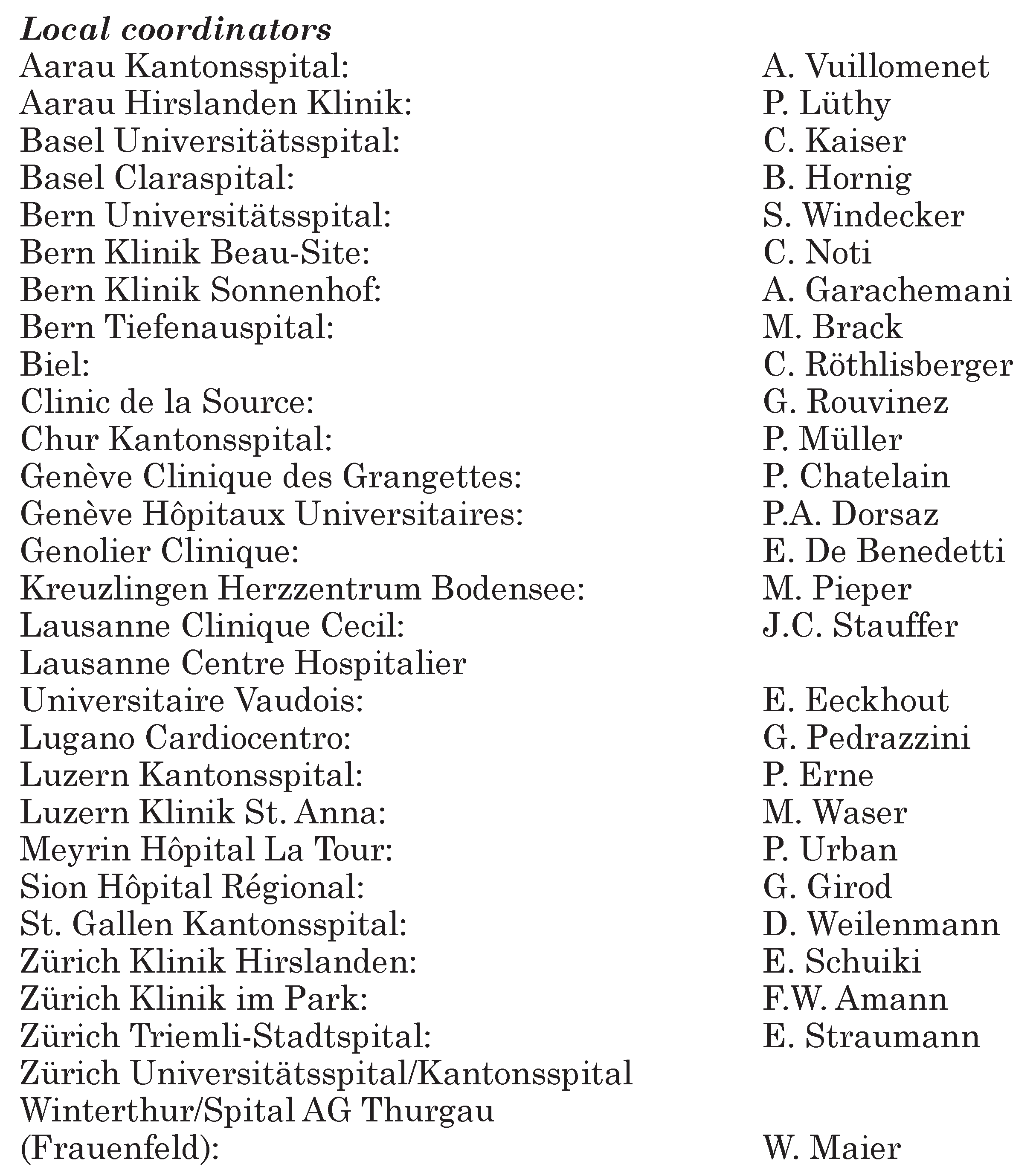
Appendix
References
- Meier, B. Örtliche Entwicklung der Koronarangioplastie. Schweiz Med Wochenschr. 1989, 119, 1033–1039. [Google Scholar]
- Meier, B.; Pfisterer, M. Coronarographie, angioplastie percutanee transluminal coronaire et chirurgie coronaire, interventions valvulaires et anti-arrhythmiques et fibrinolyses pour infarctus aigu du myocarde en Suisse. Schweiz Med Wochenschr. 1990, 120, 1559–1564. [Google Scholar]
- Meier, B.; Pfisterer, M.; Bertel, O. Interventions cardiaque en Suisse. Schweiz Med Wochenschr. 1992, 122, 432–440. [Google Scholar]
- Rouvinez, G.; Bertel, O.; Urban, P.; Meier, B. Herzeingriffe in der Schweiz 1992. Schweiz Med Wochenschr. 1994, 124, 1284–1294. [Google Scholar] [PubMed]
- Röthlisberger, C.; Meier, B.; Urban, P. Herzeingriffe in der Schweiz 1993. Schweiz Rundsch Med Prax. 1995, 84, 402–411. [Google Scholar]
- Goerre, S. Herzeingriffe in der Schweiz 1994. Schweiz Rundsch Med Prax. 1996, 85, 1071–1080. [Google Scholar]
- Goerre, S. Herzeingriffe in der Schweiz 1995. Schweiz Rundsch Med Prax. 1997, 86, 425–431. [Google Scholar]
- Pedrazzini, G. Herzeingriffe in der Schweiz 1996. Schweiz Rundsch Med Prax. 1998, 87, 821–831. [Google Scholar]
- Roffi, M. Herzeingriffe in der Schweiz. 1997. Kardiovaskuläre Medizin. 1999, 2, 302–318. [Google Scholar]
- Roffi, M. Herzeingriffe in der Schweiz. 1998. Kardiovaskuläre Medizin. 2000, 3, 89–103. [Google Scholar]
- Wahl, A. Herzeingriffe in der Schweiz 1999. Kardiovaskuläre Medizin. 2001, 4, 268–281. [Google Scholar]
- Togni, M.; Meier, B. Herzeingriffe in der Schweiz 2000. Kardiovaskuläre Medizin. 2002, 5, 238–248. [Google Scholar]
- Schlüter, L.; Rickli, H.; Vuillomenet, A.; Chatelain, P.; Eberli, F.; Meier, B.; et al. Interventions cardiaque percutanées en Suisse en 2001. Kardiovaskuläre Medizin. 2004, 7, 61–70. [Google Scholar]
- Reho, I.; Eberli, F. Trends of percutaneous cardiac interventions in Switzerland [abstract]. Kardiovaskuläre Medizin. 2005, 8 (Suppl. 8), S39. [Google Scholar]
- Maeder, M.; Stauffer, J.C.; Windecker, S.; Eberli, F.; Pedrazzini, G.; Vuilliomenet, A.; et al. Interventional cardiology in Switzerland 2004. Kardiovaskuläre Medizin. 2006, 9, 213–226. [Google Scholar]
- Maeder, M.T.; Stauffer, J.C.; Windecker, S.; Pedrazzini, G.; Vuilliomenet, A.; Rickli, H. Interventional cardiology in Switzerland during the year 2005. Kardiovaskuläre Medizin. 2007, 10, 92–100. [Google Scholar]
- Kaiser, C.; Brunner-La Rocca, H.P.; Buser, P.T.; Bonetti, P.O.; Osswald, S.; Linka, A.; et al. BASKET Investigators. Incremental cost-effectiveness of drug-eluting stents compared with a third-generation bare-metal stent in a real-world setting: Randomised Basel Stent Kosten Effektivitaets Trial (BASKET). Lancet. 2005, 366, 921–929. [Google Scholar] [CrossRef]
- Pfisterer, M.; Brunner-LaRocca, H.P.; Buser, P.T.; Rickenbacher, P.; Hunziker, P.; Mueller, C.; et al. for the BASKET investigators. Late thrombotic events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: An observational study of drug-eluting vs. bare-metal stents. J Am Coll Cardiol. 2006, 48, 2584–2591. [Google Scholar] [CrossRef]
- Windecker, S.; Remondino, A.; Eberli, F.; Jüni, P.; Räber, L.; Wenaweser, P.; et al. Sirolimus-eluting and paclitaxel-eluting stents for coronary revascularization. N Engl J Med. 2005, 353, 653–662. [Google Scholar] [CrossRef]
- Daemen, J.; Wenaweser, P.; Tsuchida, K.; Abrecht, L.; Vaina, S.; Morger, C.; et al. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: Data from a large two-institutional cohort study. Lancet. 2007, 369, 667–678. [Google Scholar] [CrossRef]
- Silber, S.; Albertson, P.; Avilés, F.F.; Camici, P.G.; Colombo, A.; Hamm, C.; et al. for the Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur Heart, J. 2005, 26, 804–847. [Google Scholar] [CrossRef]
- Fassa AA, Urban P, Radovanovic D; et al. for the AMIS Plus Investigators. Trends in reperfusion therapy of ST segment elevation myocardial infarction in Switzerland: Six year results from a nationwide registry. Heart. 2005, 91, 882–888. [Google Scholar] [CrossRef]
- Hochman JS, Lamas GA, Buller CE; et al. Occluded Artery Trial Investigators. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med. 2006, 355, 2395–2407. [Google Scholar] [CrossRef]
- Boden WE, O’Rourke RA, Teo KK; et al. COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007, 356, 1503–1516. [Google Scholar] [CrossRef] [PubMed]
- Morice, M.C.; Serruys, P.W.; Sousa, J.E.; Fajadet, J.; Ban Hayashi, E.; Perin, M.; et al. A randomised comparison of a sirolimuseluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002, 346, 1773–1780. [Google Scholar] [CrossRef]
- Stone, G.W.; Ellis, S.G.; Cox, D.A.; Hermiller, J.; O’Shaughnessy, C.; Mann, J.T.; et al. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med. 2004, 350, 221–231. [Google Scholar] [CrossRef]
- Holmes, D.R.; Jr Teirstein, P.; Satler, L.; Sketch, M.; O’Malley, J.; Popma, J.J.; et al. Sirolimus-eluting stents vs vascular brachytherapy for in-stent restenosis within bare-metal stents: The SISR randomized trial. JAMA. 2006, 295, 1264–1273. [Google Scholar] [CrossRef]
- Stone, G.W.; Ellis, S.G.; O’Shaughnessy, C.D.; Martin, S.L.; Satler, L.; McGarry, T.; et al. Paclitaxel-eluting stents vs vascular brachytherapy for in-stent restenosis within bare-metal stents: The TAXUS V ISR randomized trial. JAMA. 2006, 295, 1253–1263. [Google Scholar] [CrossRef]
- Bruckenberger, E. Herzbericht 2005 mit Transplantationschirurgie. 18. Bericht. Hannover: Eigenverlag; 2006. Available online: www.bruckenberger.de.
- Lagerqvist, B.; James, S.K.; Stenestrand, U.; Lindback, J.; Nilsson, T.; Wallentin, L. Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N Engl J Med. 2007, 356, 1009–1019. [Google Scholar] [CrossRef] [PubMed]
- Mauri, L.; Hsieh, W.; Massaro, J.M.; Ho, K.K.L.; D’Agostino, R.; Cutlip, D.E. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007, 356, 1020–1029. [Google Scholar] [CrossRef]
- Brunner-La Rocca, H.P.; Kaiser, C.; Pfisterer, M.; Basket Investigators. Targeted stent use in clinical practice based on evidence from the Basel Stent Cost Effectiveness Trial (BASKET). Eur Heart, J. 2007, 28, 719–725. [Google Scholar][Green Version]
- Smith SCJr Dove, J.T.; Jacobs, A.K.; et al. ACC/AHA guidelines of percutaneous coronary interventions (revision of the 1993 PTCA guidelines)—Executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1993 Guidelines for Percutaneous Transluminal Coronary Angioplasty). J Am Coll Cardiol. 2001, 37, 2215–2239. [Google Scholar][Green Version]
- King SB 3rd, Aversano T, Ballard WL; et al. American College of Cardiology Foundation; American Heart Association; American College of Physicians Task Force on Clinical Competence and Training (writing Committee to update the 1998 Clinical Competence Statement on Recommendations for the Assessment and Maintenance of Proficiency in Coronary Interventional Procedures). ACCF/AHA/SCAI 2007 update of the clinical competence statement on cardiac interventional procedures. A report of the American College of Cardiology Foundation/ American Heart Association/American College of Physicians Task Force on Clinical Competence and Training (writing Committee to update the 1998 Clinical Competence Statement on Recommendations for the Assessment and Maintenance of Proficiency in Coronary Interventional Procedures). J Am Coll Cardiol. 2007, 50, 82–108. [Google Scholar] [PubMed][Green Version]
- Moscucci, M.; Share, D.; Smith, D.; et al. Relationship between operator volume and adverse outcome in contemporary percutaneous coronary intervention practice. An analysis of quality-controlled multicenter percutaneous coronary intervention clinical database. J Am Coll Cardiol. 2005, 46, 625–632. [Google Scholar] [CrossRef]
- Cribier, A.; Eltchaninoff, H.; Tron, C.; et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol. 2004, 43, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Grube, E.; Laborde, J.C.; Gerckens, U.; et al. Percutaneous implantation of the CoreValve self-expanding valve prosthesis in high-risk patients with aortic valve disease: The Siegburg first-in-man study. Circulation. 2006, 114, 616–624. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.G.; Chandavimol, M.; Thompson, C.R.; et al. Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation 2006, 113, 842–850. [Google Scholar] [CrossRef]
- Webb, J.G.; Harnek, J.; Munt, B.I.; et al. Percutaneous transvenous mitral annuloplasty: Initial human experience with device implantation in the coronary sinus. Circulation. 2006, 113, 851–855. [Google Scholar] [CrossRef]
- Kizer, J.R.; Devereux, R.B. Patient foramen ovale in young adults with unexplained stroke. N Engl J Med 2005, 353, 2361–2372. [Google Scholar] [CrossRef]
- Handke, M.; Harloff, A.; Olschewski, M.; Hetzel, A.; Geibel, A. Patent foramen ovale and cryptogenic stroke in older patients. N Engl J Med. 2007, 357, 2262–2268. [Google Scholar] [CrossRef]
© 2008 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maeder, M.T.; Stauffer, J.-C.; Windecker, S.; Pedrazzini, G.; Kaiser, C.A.; Roffi, M.; Rickli, H.; on behalf of the Working Group “Interventional Cardiology and Acute Coronary Syndrome”. Interventional Cardiology in Switzerland 2006. Cardiovasc. Med. 2008, 11, 187. https://doi.org/10.4414/cvm.2008.01338
Maeder MT, Stauffer J-C, Windecker S, Pedrazzini G, Kaiser CA, Roffi M, Rickli H, on behalf of the Working Group “Interventional Cardiology and Acute Coronary Syndrome”. Interventional Cardiology in Switzerland 2006. Cardiovascular Medicine. 2008; 11(6):187. https://doi.org/10.4414/cvm.2008.01338
Chicago/Turabian StyleMaeder, Micha T., Jean-Christoph Stauffer, Stephan Windecker, Giovanni Pedrazzini, Christoph A. Kaiser, Marco Roffi, Hans Rickli, and on behalf of the Working Group “Interventional Cardiology and Acute Coronary Syndrome”. 2008. "Interventional Cardiology in Switzerland 2006" Cardiovascular Medicine 11, no. 6: 187. https://doi.org/10.4414/cvm.2008.01338
APA StyleMaeder, M. T., Stauffer, J.-C., Windecker, S., Pedrazzini, G., Kaiser, C. A., Roffi, M., Rickli, H., & on behalf of the Working Group “Interventional Cardiology and Acute Coronary Syndrome”. (2008). Interventional Cardiology in Switzerland 2006. Cardiovascular Medicine, 11(6), 187. https://doi.org/10.4414/cvm.2008.01338



