Coronary CT Is Overused, Angiography Remains the Standard †
Historical development
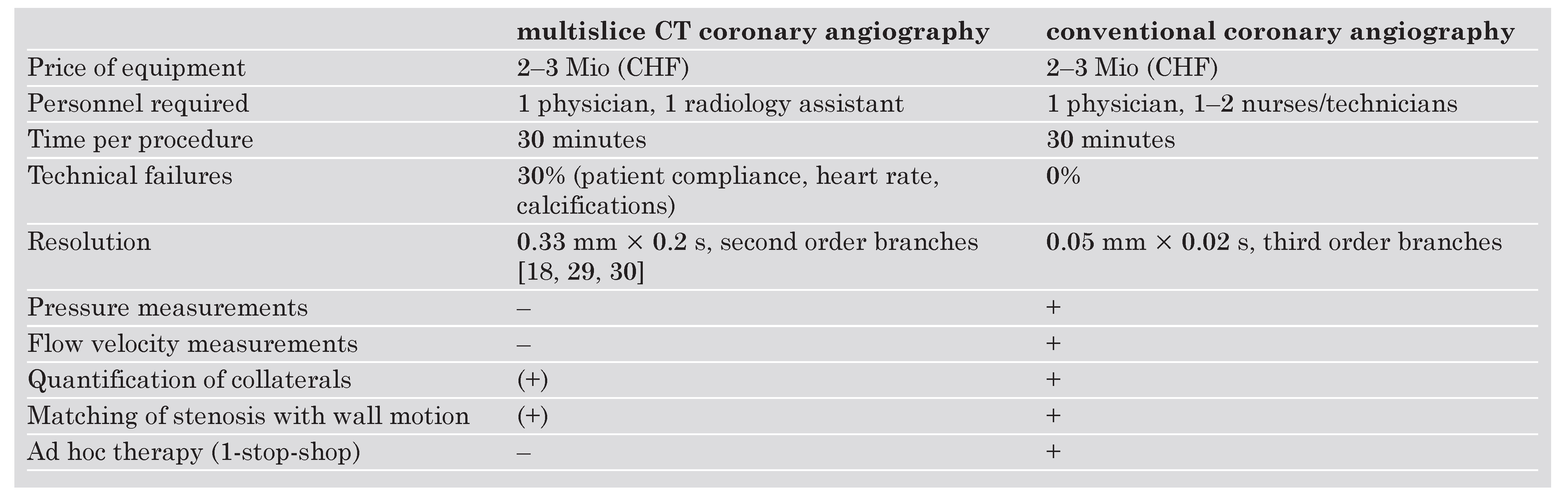
Technicalities
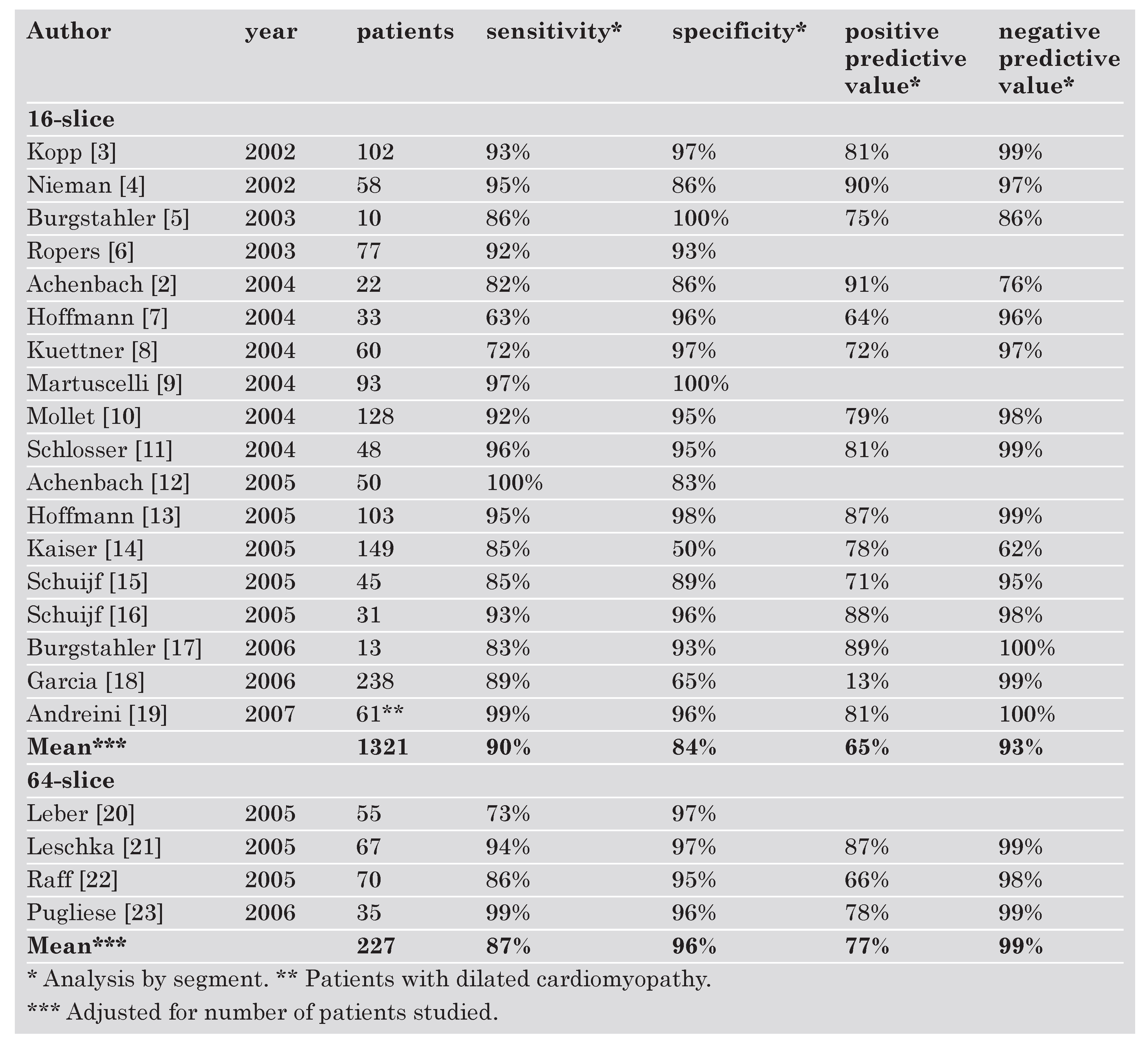
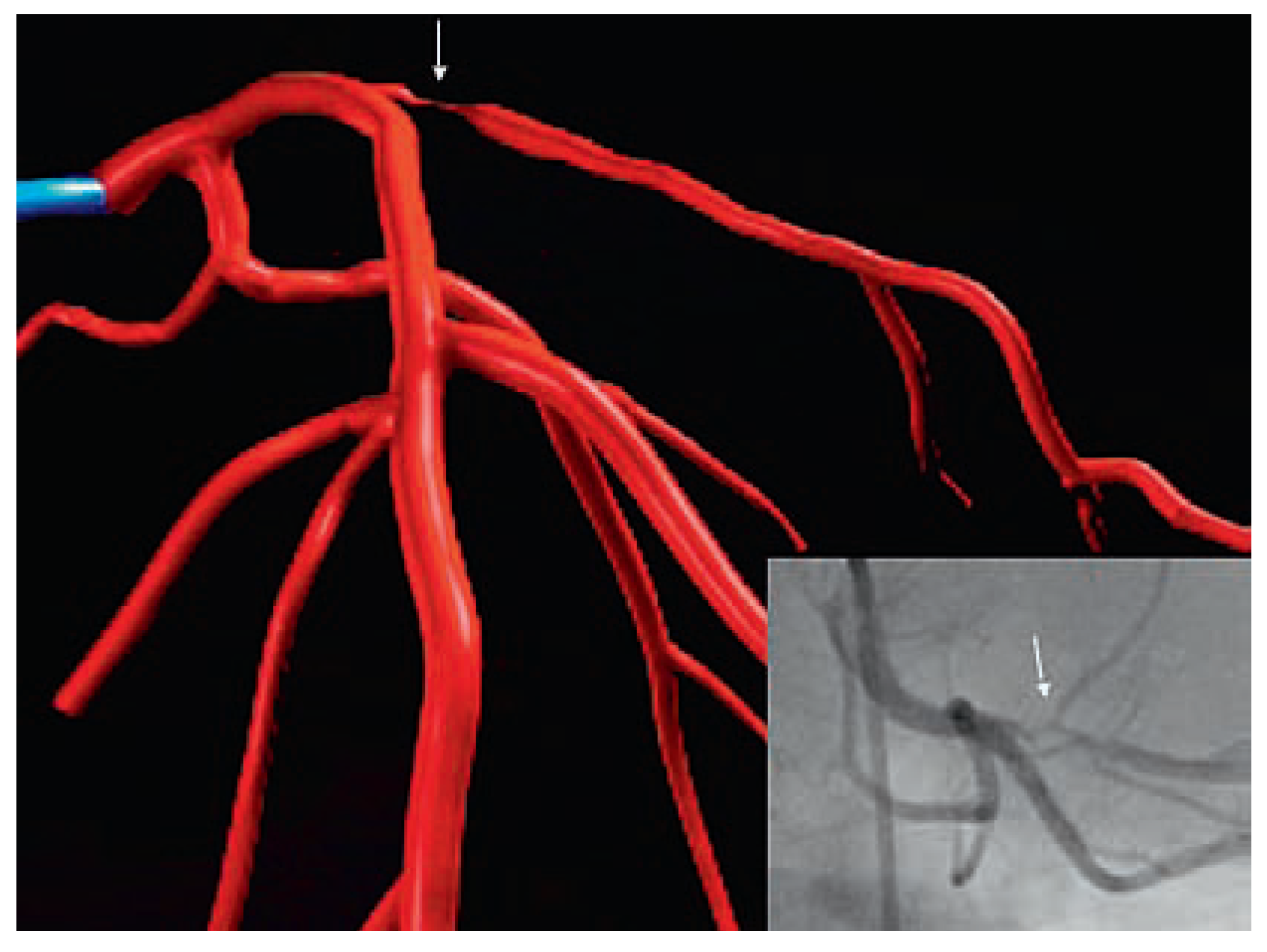
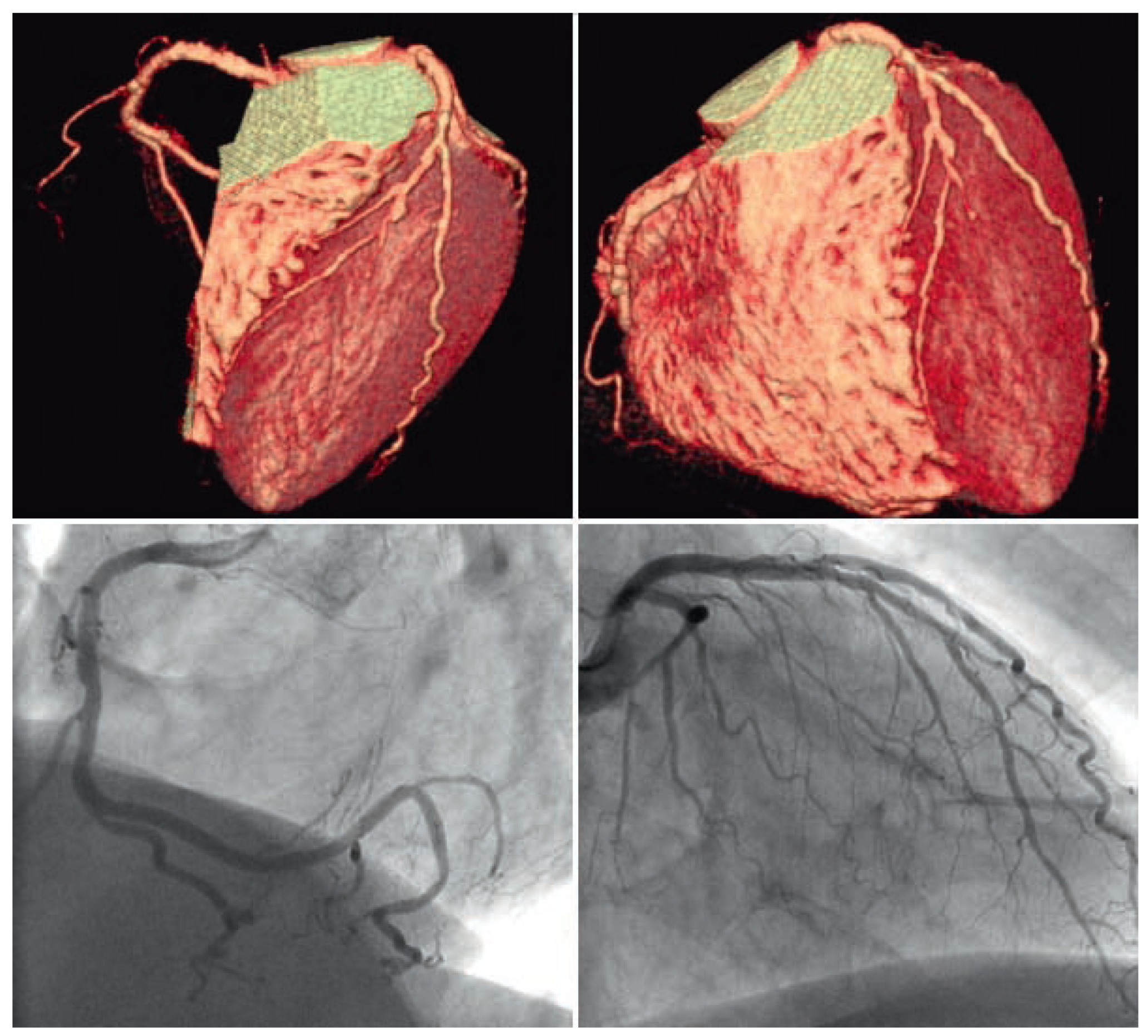
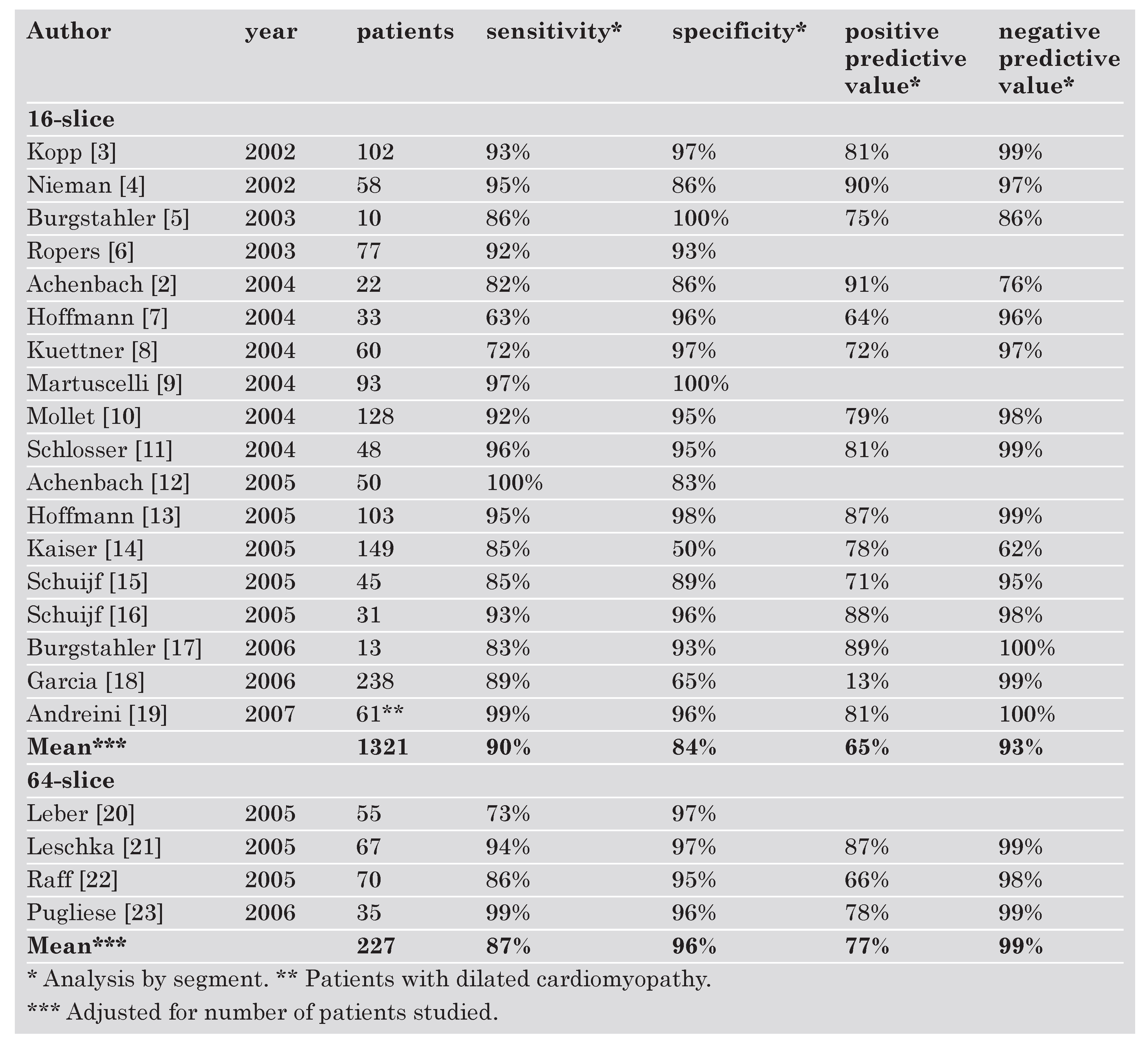
Diagnostic performance
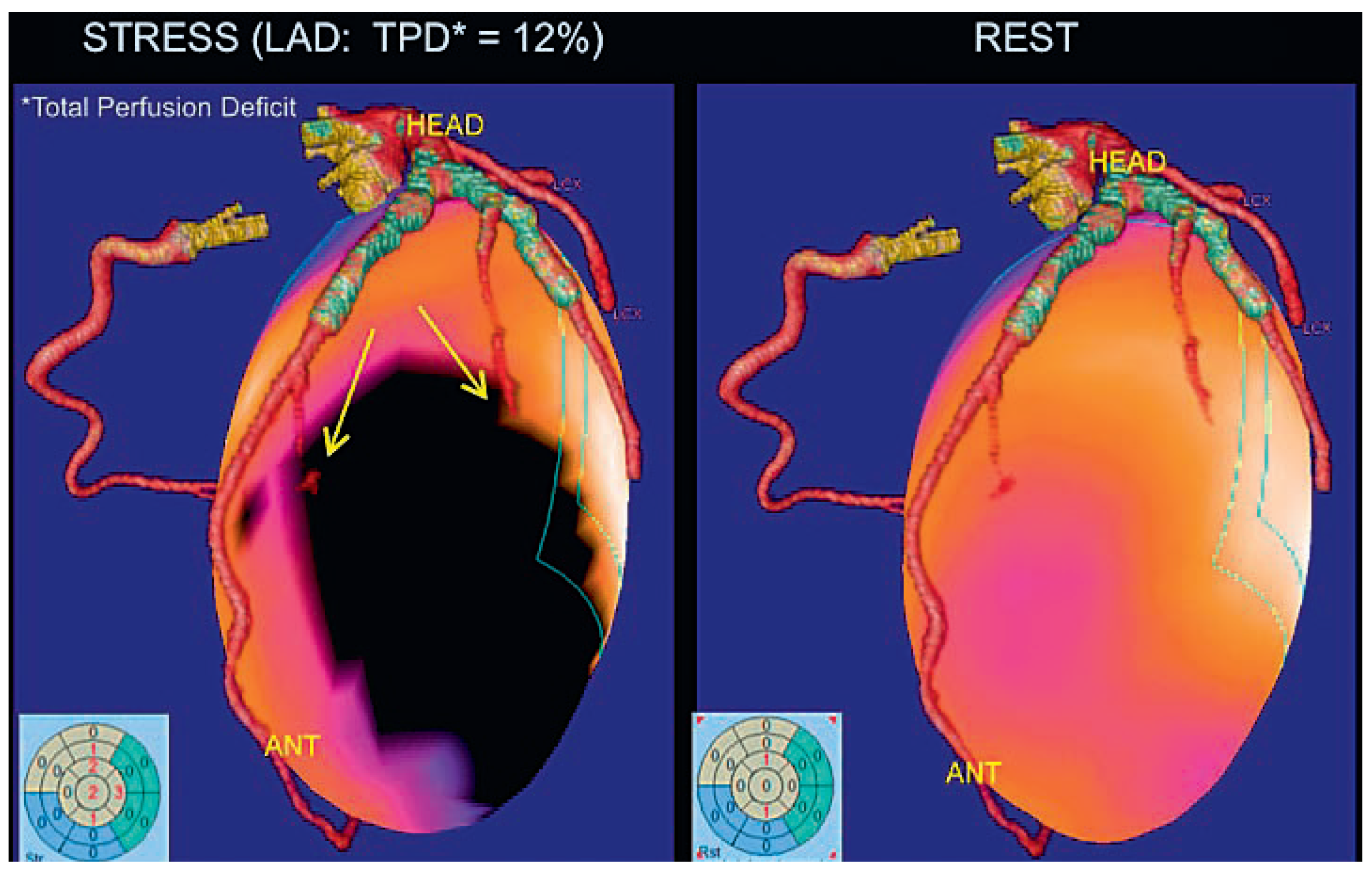
Associated techniques
Hazards and complications
Radiation exposure
Conclusions
References
- Sones, F.M.J.; Shirey, E.K.; Proudfit, W.L.; Westcott, R.N. Cine-coronary arteriography (abstract). Circulation. 1959, 20, 773. [Google Scholar]
- Achenbach, S.; Moshage, W.; Bachmann, K. Coronary angiography by electron beam tomography. Herz. 1996, 21, 106–117. [Google Scholar] [PubMed]
- Kopp, A.F.; Schroeder, S.; Kuettner, A.; Baumbach, A.; Georg, C.; Kuzo, R.; et al. Non-invasive coronary angiography with high resolution multidetector-row computed tomography. Results in 102 patients. Eur Heart J. 2002, 23, 1714–1725. [Google Scholar] [CrossRef] [PubMed]
- Nieman, K.; Cademartiri, F.; Lemos, P.A.; Raaijmakers, R.; Pattynama, P.M.; de Feyter, P.J. Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation. 2002, 106, 2051–2054. [Google Scholar] [CrossRef] [PubMed]
- Burgstahler, C.; Kuettner, A.; Kopp, A.F.; Herdeg, C.; Martensen, J.; Claussen, C.D.; et al. Non-invasive evaluation of coronary artery bypass grafts using multi-slice computed tomography: Initial clinical experience. Int J Cardiol. 2003, 90, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Ropers, D.; Baum, U.; Pohle, K.; Anders, K.; Ulzheimer, S.; Ohnesorge, B.; et al. Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation. 2003, 107, 664–666. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.H.; Shi, H.; Schmid, F.T.; Gelman, H.; Brambs, H.J.; Aschoff, A.J. Noninvasive coronary imaging with MDCT in comparison to invasive conventional coronary angiography: A fast-developing technology. Am J Roentgenol. 2004, 182, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Kuettner, A.; Trabold, T.; Schroeder, S.; Feyer, A.; Beck, T.; Brueckner, A.; et al. Noninvasive detection of coronary lesions using 16–detector multislice spiral computed tomography technology: Initial clinical results. J Am Coll Cardiol. 2004, 44, 1230–1237. [Google Scholar] [PubMed][Green Version]
- Martuscelli, E.; Romagnoli, A.; D’Eliseo, A.; Tomassini, M.; Razzini, C.; Sperandio, M.; et al. Evaluation of venous and arterial conduit patency by 16-slice spiral computed tomography. Circulation. 2004, 110, 3234–3238. [Google Scholar] [CrossRef] [PubMed]
- Mollet, N.R.; Cademartiri, F.; Nieman, K.; Saia, F.; Lemos, P.A.; McFadden, E.P.; et al. Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol. 2004, 43, 2265–2270. [Google Scholar] [CrossRef] [PubMed]
- Schlosser, T.; Konorza, T.; Hunold, P.; Kuhl, H.; Schmermund, A.; Barkhausen, J. Noninvasive visualization of coronary artery bypass grafts using 16–detector row computed tomography. J Am Coll Cardiol. 2004, 44, 1224–1229. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, S.; Ropers, D.; Pohle, F.K.; Raaz, D.; von Erffa, J.; Yilmaz, A.; et al. Detection of coronary artery stenoses using multi-detector CT with 16 ? 0.75 collimation and 375 ms rotation. Eur Heart J. 2005, 26, 1978–1986. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.H.; Shi, H.; Schmitz, B.L.; Schmid, F.T.; Lieberknecht, M.; Schulze, R.; et al. Noninvasive coronary angiography with multislice computed tomography. JAMA. 2005, 293, 2471–2478. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, C.; Bremerich, J.; Haller, S.; Brunner-La Rocca, H.P.; Bongartz, G.; Pfisterer, M.; et al. Limited diagnostic yield of noninvasive coronary angiography by 16–slice multi-detector spiral computed tomography in routine patients referred for evaluation of coronary artery disease. Eur Heart J. 2005, 26, 1987–1992. [Google Scholar] [CrossRef] [PubMed]
- Schuijf, J.D.; Bax, J.J.; Salm, L.P.; Jukema, J.W.; Lamb, H.J.; van der Wall, E.E.; et al. Noninvasive coronary imaging and assessment of left ventricular function using 16-slice computed tomography. Am J Cardiol. 2005, 95, 571–574. [Google Scholar] [CrossRef] [PubMed]
- Schuijf, J.D.; Bax, J.J.; Jukema, J.W.; Lamb, H.J.; Vliegen, H.W.; van der Wall, E.E.; et al. Noninvasive evaluation of the coronary arteries with multislice computed tomography in hypertensive patients. Hypertension. 2005, 45, 227–232. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Burgstahler, C.; Beck, T.; Kuettner, A.; Drosch, T.; Kopp, A.F.; Heuschmid, M.; et al. Non-invasive evaluation of coronary artery bypass grafts using 16-row multi-slice computed tomography with 188 ms temporal resolution. Int J Cardiol. 2006, 106, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.J.; Lessick, J.; Hoffmann, M.H. Accuracy of 16-row multidetector computed tomography for the assessment of coronary artery stenosis. JAMA. 2006, 296, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Andreini, D.; Pontone, G.; Pepi, M.; Ballerini, G.; Bartorelli, A.L.; Magini, A.; et al. Diagnostic accuracy of multidetector computed tomography coronary angiography in patients with dilated cardiomyopathy. J Am Coll Cardiol. 2007, 49, 2044–2050. [Google Scholar] [CrossRef] [PubMed]
- Leber, A.W.; Knez, A.; von Ziegler, F.; Becker, A.; Nikolaou, K.; Paul, S.; et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: A comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005, 46, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Leschka, S.; Alkadhi, H.; Plass, A.; Desbiolles, L.; Grunenfelder, J.; Marincek, B.; et al. Accuracy of MSCT coronary angiogra- phy with 64-slice technology: First experience. Eur Heart J. 2005, 26, 1482–1487. [Google Scholar] [CrossRef]
- Raff, G.L.; Gallagher, M.J.; O’Neill, W.W.; Goldstein, J.A. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005, 46, 552–557. [Google Scholar] [CrossRef]
- Pugliese, F.; Mollet, N.R.; Runza, G.; van Mieghem, C.; Meijboom, W.B.; Malagutti, P.; et al. Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable an- gina pectoris. Eur Radiol. 2006, 16, 575–582. [Google Scholar] [CrossRef]
- Cademartiri, F.; Schuijf, J.D.; Pugliese, F.; Mollet, N.R.; Jukema, J.W.; Maffei, E.; et al. Usefulness of 64-slice multislice compu- ted tomography coronary angiography to assess in-stent restenosis. J Am Coll Cardiol. 2007, 49, 2204–2210. [Google Scholar] [CrossRef]
- Lüscher, T.F.; Kaufmann, P.; Corti, R.; Trigo-Trindade, P. «Car- diac Imaging»: Die Qual der Wahl? Kardiovaskuläre Medizin. 2007, 10, 121–125. [Google Scholar]
- Johnson, L.W.; Lozner, E.C.; Johnson, S.; Krone, R.; Pichard, A.D.; Vetrovec, G.W.; et al. Coronary arteriography 1984–1987: A re- port of the Registry of the Society for Cardiac Angiography and Interventions. I. Results and complications. Cathet Cardiovasc Diagn. 1989, 17, 5–10. [Google Scholar] [CrossRef]
- Wyman, R.M.; Safian, R.D.; Portway, V.; Skillman, J.J.; McKay, R.G.; Baim, D.S. Current complications of diagnostic and therapeu- tic cardiac catheterization. J Am Coll Cardiol. 1988, 12, 1400–1406. [Google Scholar] [CrossRef]
- West, R.; Ellis, G.; Brooks, N. Complications of diagnostic car- diac catheterisation: Results from a confidential inquiry into cardiac catheter complications. Heart. 2006, 92, 810–814. [Google Scholar] [CrossRef]
- Mollet, N.R.; Cademartiri, F.; van Mieghem, C.A.; Runza, G.; McFadden, E.P.; Baks, T.; et al. High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation. 2005, 112, 2318–2323. [Google Scholar] [CrossRef] [PubMed]
- Schwitter, J. Abklärung der Koronaren Herzkrankheit mittels Herz-MR oder Mehrzeilen-CT. Kardiovaskuläre Medizin. 2007, 10, 126–138. [Google Scholar]
- Hunold, P.; Vogt, F.M.; Schmermund, A.; Debatin, J.F.; Kerkhoff, G.; Budde, T.; et al. Radiation exposure during cardiac CT: Ef- fective doses at multi-detector row CT and electron-beam CT. Radiology. 2003, 226, 145–52. [Google Scholar] [CrossRef]
- Budoff, M.J.; Shaw, L.J.; Liu, S.T.; Weinstein, S.R.; Mosler, T.P.; Tseng, P.H.; et al. Long-term prognosis associated with coro- nary calcification: Observations from a registry of 25,253 pa- tients. J Am Coll Cardiol. 2007, 49, 1860–1870. [Google Scholar] [CrossRef]
- Coles, D.R.; Smail, M.A.; Negus, I.S.; Wilde, P.; Oberhoff, M.; Karsch, K.R.; et al. Comparison of radiation doses from multislice computed tomography coronary angiography and conventio- nal diagnostic angiography. J Am Coll Cardiol. 2006, 47, 1840–1845. [Google Scholar] [CrossRef] [PubMed]
- Einstein, A.; Henzlova, M.; Rajagopalan, S. Estimating risk of cancer associated with radiation exposure from 64-slice com- puted tomography coronary angiography. JAMA. 2007, 298, 317–323. [Google Scholar] [CrossRef] [PubMed]
 |
 |
© 2008 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meier, B. Coronary CT Is Overused, Angiography Remains the Standard. Cardiovasc. Med. 2008, 11, 196. https://doi.org/10.4414/cvm.2008.01337
Meier B. Coronary CT Is Overused, Angiography Remains the Standard. Cardiovascular Medicine. 2008; 11(6):196. https://doi.org/10.4414/cvm.2008.01337
Chicago/Turabian StyleMeier, Bernhard. 2008. "Coronary CT Is Overused, Angiography Remains the Standard" Cardiovascular Medicine 11, no. 6: 196. https://doi.org/10.4414/cvm.2008.01337
APA StyleMeier, B. (2008). Coronary CT Is Overused, Angiography Remains the Standard. Cardiovascular Medicine, 11(6), 196. https://doi.org/10.4414/cvm.2008.01337




