Summary
Coronary CT angiography (CTA) is emerging as a highly effective alternative imaging technique for the assessment of coronary artery disease (CAD). The rapid evolution of multidetector CT scanners has lead to major improvement in temporal resolution of image acquisition allowing high-resolution images of coronary arteries to be acquired even in patients with fast and irregular heart rate. So far the clinical value of coronary CTA was mainly enforced by its high negative predictive value allowing to exclude coronary disease with high degree of accuracy in patients with low probability for CAD. With the ability of CTA to provide anatomical and functional information of the heart and great vessels, there are numerous additional applications of CTAfor evaluating cardiac function, valvular disease, calcifications, and characterisation of vascular plaques. With the advent of dual energy imaging and hybrid scanners, combining PET and CT imaging modalities, additional potential applications of CTA in cardiology are predictable. The main limiting factor for broader adoption of CTA in clinical practice is the lag between conclusive clinical trials and the rapid advancement of technology that render clinical trials performed with earlier generation of machines obsolete even before the trials are completed.
Introduction
The rapid development of multi-detector CT scanners in the past decade has lead to faster acquisition capabilities at higher resolution allowing for gated images of the heart to be acquired at a rate sufficiently fast for obtaining still images at different phases of the heart cycle. This technology was rapidly adopted to generate high-resolution contrast-enhanced angiograms of the heart and coronary arteries [
1,
2,
3,
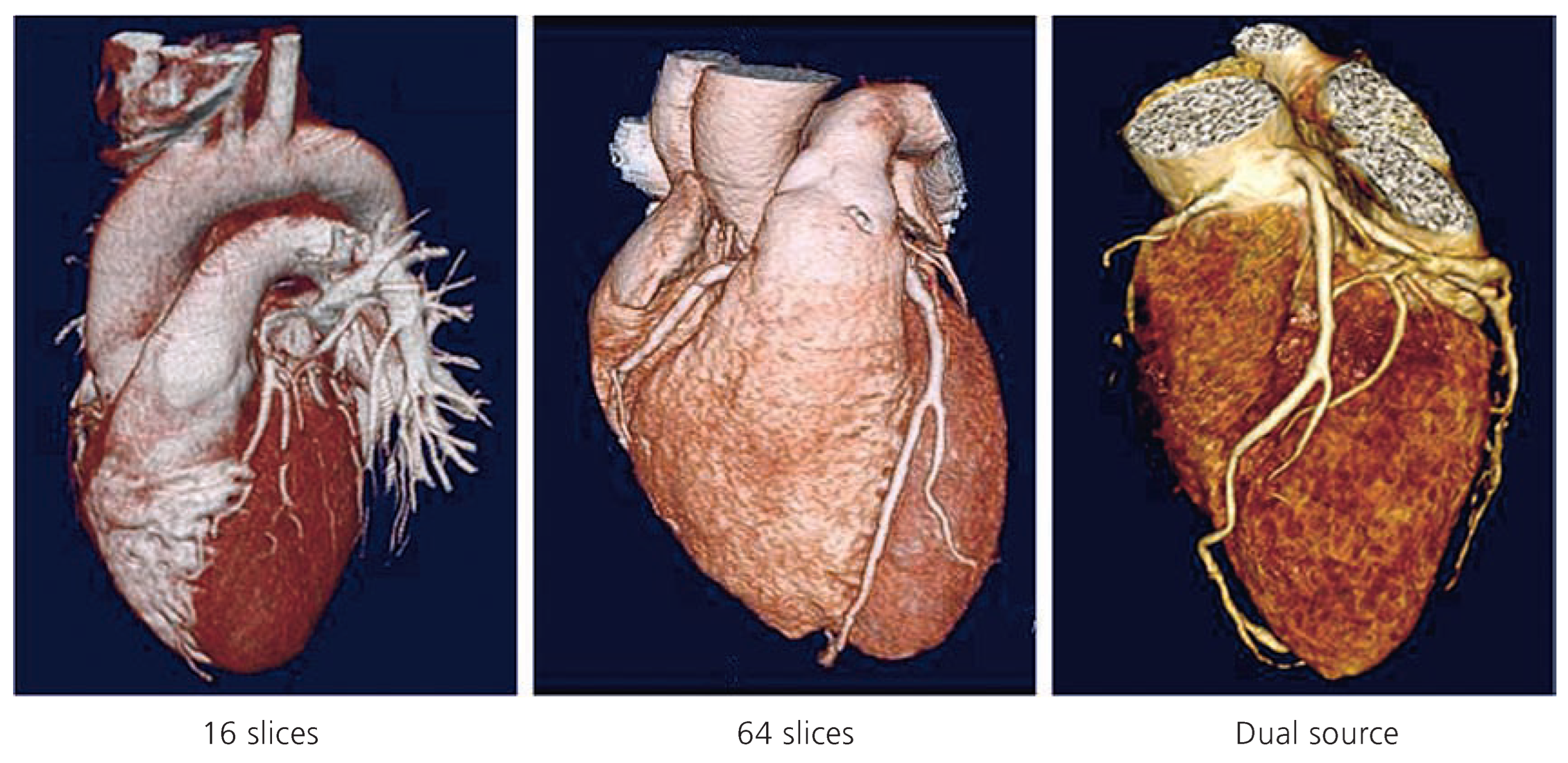
4]. While the first generation of scanners equipped with 12 and 16 rows of detectors were barely sufficient to obtain adequate images, they often failed to generate clinically interpretable images in a large proportion of patients with fast or irregular heart rate (
Figure 1). With the increasing performance obtained by higher number of detectors (64 to 256 detectors) as well as the advent of scanners equipped with dual X-ray beams that can reduce acquisition time by half, the accuracy and performance of the scanners to properly visualise coronary arteries even in presence of fast and irregular heart rate have become a reality. Recent publications [
5] have shown that dual source scanners can generate reliable and diagnostic-quality CT coronary angiograms even in patients with fast heart rates without beta blockade. More recent scanners using large detectors arrays allow nowadays to acquire the whole heart in a single heart beat, allowing for adequate image quality even in presence of irregular heart rate or atrial fibrillation [
6].
This new modality has triggered major controversies regarding its value in the workup of coronary artery disease patients and its potential role in replacing more invasive coronary angiography. The emergence of this controversy is also fuelled by recent studies that challenge the established belief that traditional coronary angiography offers the advantage of performing therapeutic interventions such as angioplasty and stenting of lesions that are identified during the same diagnostic procedure. Recent outcome analysis studies have shown however that stenting anatomically significant coronary lesions in patients with stable CAD may not have any impact on patient outcome in absence of proof of myocardial ischaemia and assessment of the haemodynamic significance of the coronary stenosis [
7,
8,
9]. These studies suggest that therapeutic interventions should only be applied to patients that have proven haemodynamically significant alterations induced by a given vascular stenosis, and therefore such interventions should not be performed based only on morphological assessment of the vessel lumen. That challenges the concept that every significant lesion identified on the coronary angiogram should undergo percutaneous dilatation and stenting in the same session. De-coupling the diagnostic from the therapeutic procedures to allow for adequate assessment of the haemodynamic significance of coronary lesions will then lead to alternative clinical pathways that include less invasive procedures such as coronary CTA to be applicable in selected categories of patients.
The role of coronary CTA
Coronary CTA can play a significant role in diagnosis of coronary artery disease particularly in patients with low probability of CAD with unspecific symptoms and/or non-conclusive functional tests such as exercise, stress echocardiography or scintigraphy [
10,
11]. The strength of coronary CTA early in the diagnostic workup is its negative predictive value that can exclude with high degree of confidence patients that do not have CAD. Non-invasive assessment of coronary arteries and cardio-thoracic structures with CTA in patients with acute chest pain is highly recommended in patients with intermediate probability for CAD and no enzyme or ECG changes. It is also applicable in patients with typical or atypical chest pain and intermediate probability for CAD where more traditional tests remain equivocal or in patients unable to exercise or undergo a stress test (
Figure 3).
Coronary CTA is also highly recommended for follow-up evaluation of coronary bypass grafts. Unlike invasive coronary angiograms it does not require accurate localisation of ostia of venous grafts for selective contrast injections. CTA was shown to be accurate and reliable test for detection of bypass grafts stenosis as well as patency of surgical anastomosis with native coronary arteries. With appropriate imaging protocols, both arterial grafts from mammary arteries and venous grafts can be visualised and evaluated within a single acquisition with a single bolus of contrast agent. With volume rendering of the 3D data acquired by CTA, the topology and localisation of grafts is more accurate than traditional 2D coronary angiograms. Also, the same data acquired for evaluating the bypass grafts allow simultaneous evaluation of the native coronary arteries and assessment of their segmental lesions proximal or distal to the site of graft anastomosis.
With the ability to clearly identify vascular calcifications, coronary CTA provides additional valuable information on plaque characterisation. Detection and quantification of coronary calcium score have been well established as reliable criteria for evaluating risk factors of coronary artery disease. The latest generations of CT scanners also provide images that allow differentiating between different types of vascular plaques based on their tissue density ranging from lipid to fibrous to calcified plaques. While extreme calcifications of the coronary arteries may alter the accuracy of quantitative analysis of the degree of vascular stenosis it remains indicative of the severity of coronary disease.
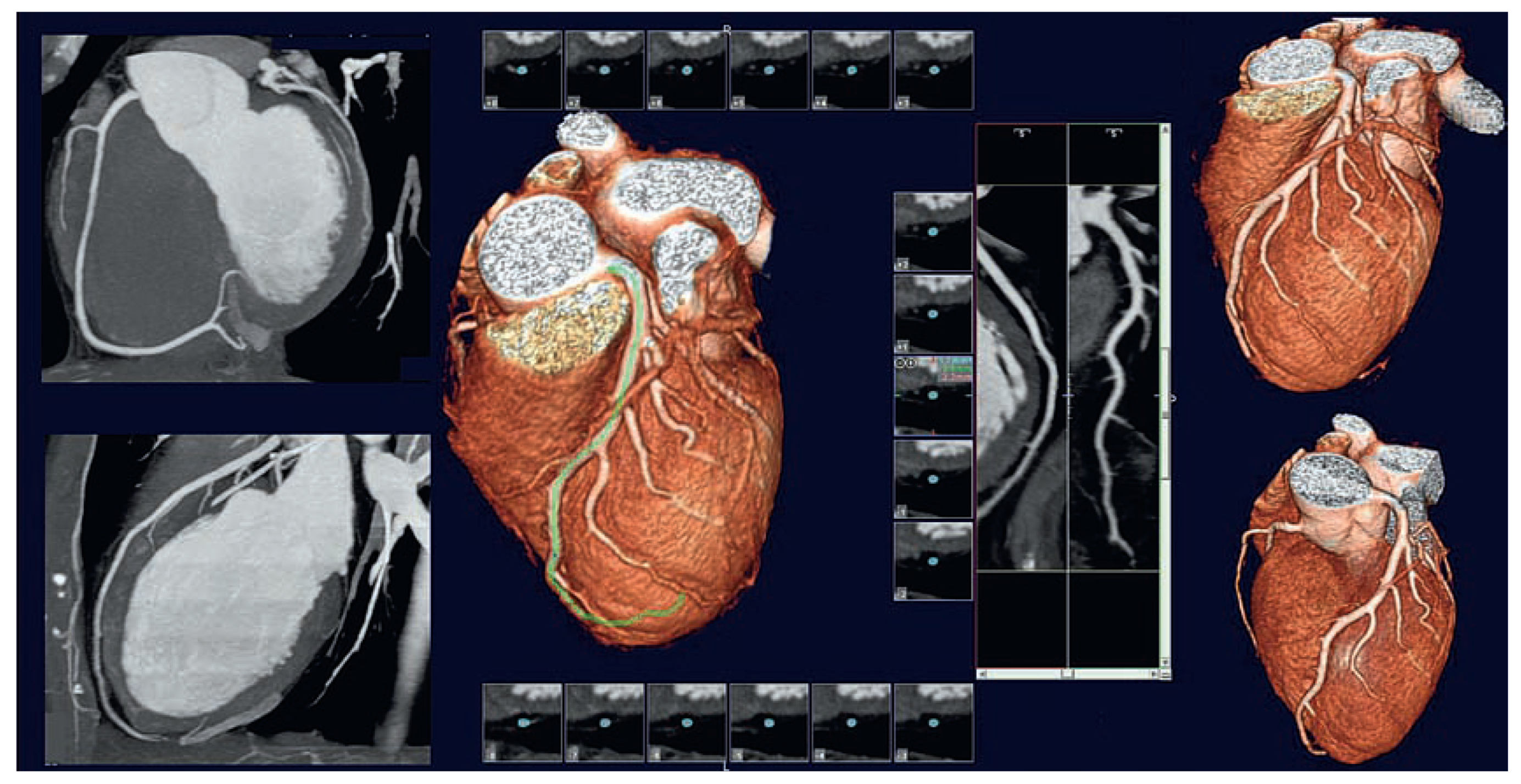
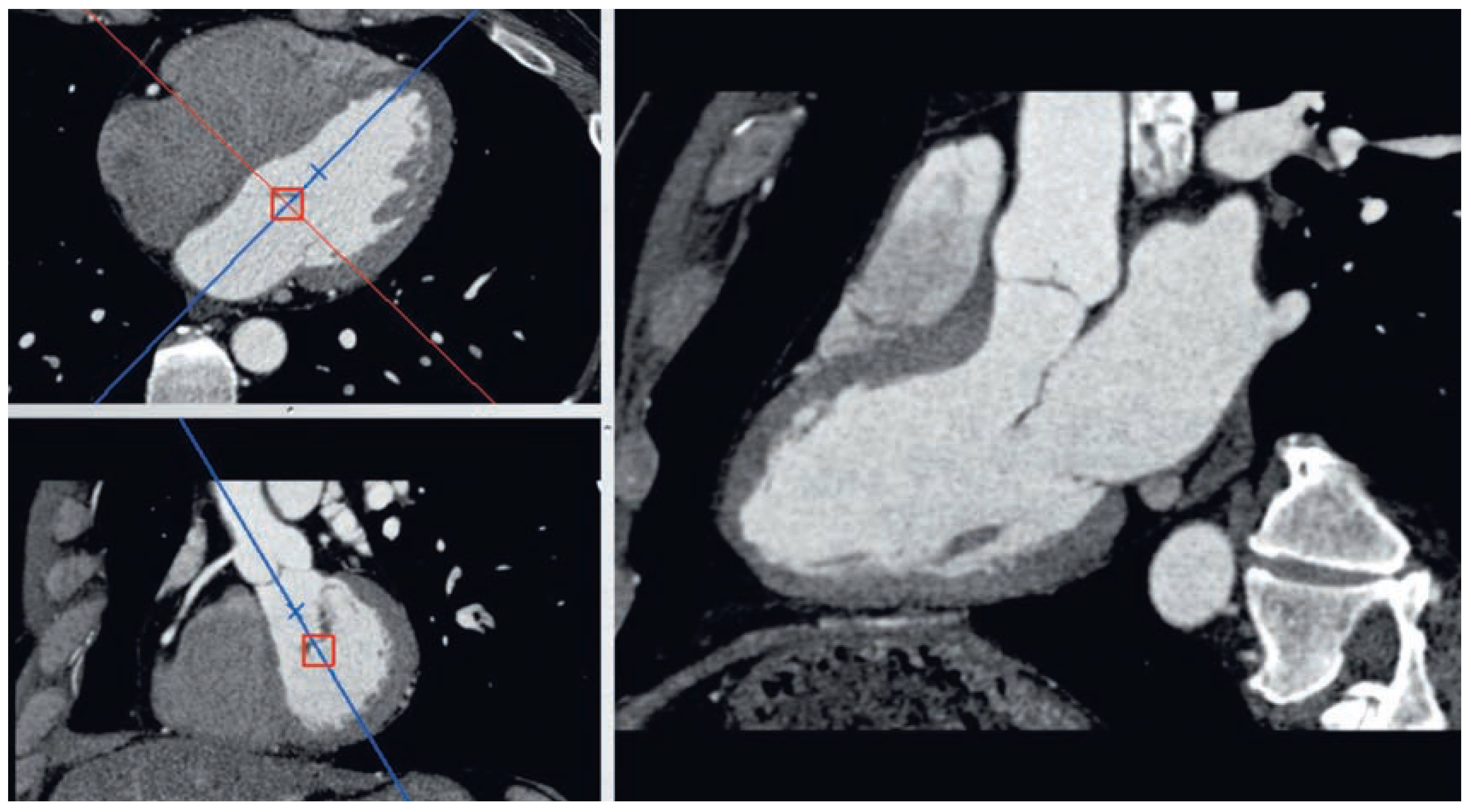
All coronary CTA studies are acquired in ECG-gated dynamic mode where different image sets are obtained at different times in the cardiac cycle. While individual time windows of end-systolic and end-diastolic phases are usually used for adequate visualisation of the coronary arteries at times where they present minimal velocity, it is also possible to reconstruct the data for all phases of the cardiac cycle from the same original dataset. It is thereby possible to generate dynamic cine sequences of the whole heart and to select oblique reformatted planes along standard anatomical axis of the heart (
Figure 4). These reconstructed data provide high quality images for the assessment of heart anatomy and ventricular function. Ventricular volumes and ejection fraction as well as regional wall motion and wall thickening parameters can be measured quantitatively with high degree of accuracy due to the high spatial resolution of the images [
12,
13,
14].
Evolution of coronary CTA technology
Early publication on coronary CTA were performed on scanners with limited number of detectors and resulted in relatively poor results, mostly when the number of coronary segments that could be visualised were considered. The limitation in temporal resolution of the early scanners prevented this technique to be reliably applicable in patients with high heart rate or with irregular rates. Up to the generation of scanners with 16 slice detectors, the ratio of non-conclusive studies was still in the range of 20 to 30% of the patients who had at least one coronary segment that could not be adequately evaluated despite the use of beta blockers in all patients for reduction of their heart rate during the study.
The recent advent of 64 slice scanners followed by new dual beam and 256 slice scanners have led to a quantum leap in temporal and spatial resolution with much higher performance allowing imaging patients with fast and irregular heart rates. Dual beam scanners essentially double the speed of acquisition while maintaining the same spatial resolution of a 64-slice scanner [
5,
15,
16]. With two X-ray beams and detectors rotating simultaneously on the same gantry, the double amount of data are acquired on each rotation. Furthermore, the ability of having each individual generator set to a different energy with different tissue penetration opens new perspectives in better tissue characterisation that would potentially allow a better assessment of composition of vascular plaques. It is also possible using dual energy imaging to separate calcifications from contrast agent to generate images of the vascular lumens without interference from calcified plaques. Dual energy imaging has already been explored in peripheral vessels both for generating better calcium-free angiograms as well as assessing the tissue characteristics of vascular plaques. These techniques may in the future be also applicable to coronary arteries.
Today’s latest generation of scanners have matured to provide reliable and reproducible coronary angiograms in all categories of patients at any heart rate [
17,
18]. While the ability of this technique to exclude coronary artery disease due to its high negative predictive value is well established, the accuracy of identifying and measuring coronary stenosis compared to conventional coronary angiograms has not been well document with this generation of scanners yet. The latest generation of dual beam and 256 slice scanners have only appeared on the market recently and were not available long enough to allow sufficient clinical studies to be performed. Studies performed on earlier generations of scanners cannot be extrapolated to the new scanners due to the significant change in image quality that the latest generation provides.
While the major limitation of coronary CTA is its radiation exposure dose, a significant effort was invested in the recent years to develop techniques that can dramatically reduce the effective dose to the patient. With higher number of detectors, images can be generated with higher exposure rate if full spatial and temporal resolution over the complete heart cycle is pursued. At full dose over the whole chest area, a 64 slice scanner can easily deliver between 15 and 20 mSv. Full CTA dose average the double of conventional coronary angiogram averaging between 9 and 12 mSv However most clinical CTA protocols used today apply prospective or retrospective gating with pulsed radiation synchronous to the ECG that delivers lower radiation dose outside a selected window in diastolic phase. A prospective gate window of 20% over diastole in patients with a heart rate around 60 bpm can reduce the total dose to the patient by 80%. At higher heart rates the reduction of dose may be less and still achieve 55 to 60% of dose reduction. Furthermore, the area covered for a coronary CTA can be reduced to the heart only instead of covering the whole chest further reducing the exposure by half or more. Recent publications have shown that by using prospective gating and proper imaging protocol, accurate images of the coronary arteries can be obtained at doses as low as 1 or 2 mSV [
19,
20]. With 256 detectors and higher, scanners can acquire full 3D images of the whole heart in a single rotation avoiding spiral averaging of multiple heart cycles. This can significantly reduce the dose down to 2.8 mSv with pulsed exposure over diastole and about 5 mSv for full dynamic assessment of LV function over the whole heart cycle [
6,
21]. These recent technical advances and use of appropriate protocols have significantly reduced the exposure dose of coronary CTA way below the dose of a conventional coronary angiogram.
Alternative clinical pathways
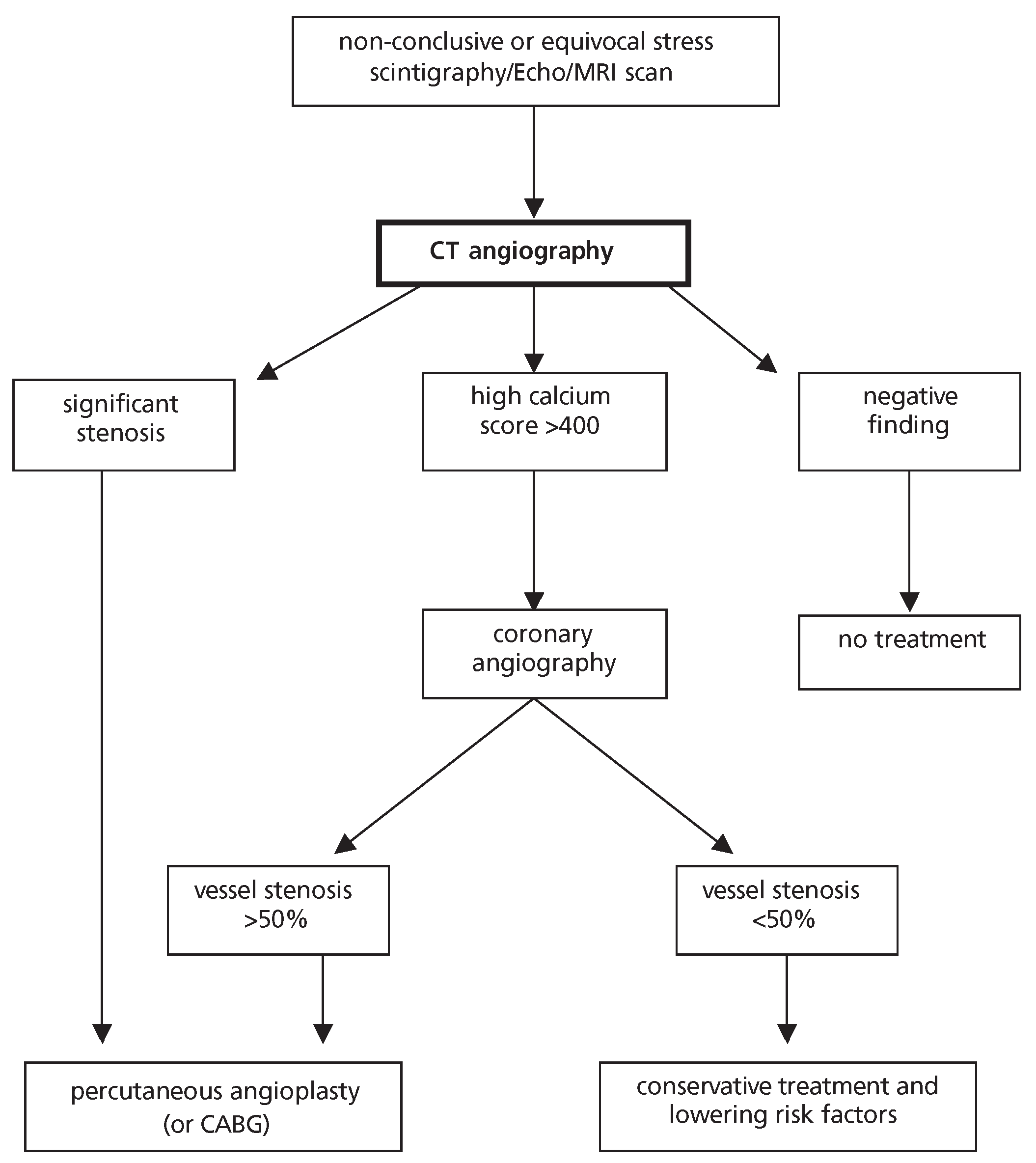
The ability to determine non-invasively with high degree of accuracy the presence of coronary disease with CTA introduces a new paradigm in clinical decision pathways [
11]. Its high negative predictive value makes it an ideal alternative to invasive coronary angiograms in patients with low or medium probability for coronary artery disease. Its use in those patients should lead to a significant reduction of normal coronary angiograms. Recent statistics still show that in most cardiac centres between 30% and 40% of coronary angiograms performed show normal coronary arteries [
10]. This means that in these cases one patient out of three undergoes unnecessary risks and side effects of invasive procedure that could be replaced advantageously by non-invasive coronary CTA with the same accuracy for excluding significant coronary artery disease. To get the best risk-benefit ratio of coronary CTA versus conventional coronary angiograms it is important to establish appropriate selection criteria of patients that have the lowest probability of getting a second coronary angiogram following the diagnostic coronary CTA examination. Thereby one could maximize the number of patients that benefit from CTA while minimising the number of patients that will have positive findings on CTA and would require additional coronary angiogram (
Figure 2). It is also important to apply this technique in cases where CT images can provide additional information that conventional angiograms cannot provide. CT angiogram can provide anatomical and functional information about the heart and great vessels as well as the assessments of calcifications of the valves and thoracic vessels that can otherwise not be seen on conventional contrast angiograms (
Figure 3).
CT angiograms of the heart and thoracic vessels can also be applicable to other clinical indications besides evaluating coronary arteries. According to the appropriateness criteria recently established by the American College of Cardiology [
22], the use of cardiac CTAis appropriate (with a score between 7 and 9 on a scale of 1 to 9) in the following conditions:
- (1.)
Detection of CAD in patient with chest pain with:
- –
intermediate pre-test probability of CAD
- –
ECG uninterpretable or unable to exercise
- (2.)
Evaluation of suspected coronary anomalies
- (3.)
Evaluation of acute chest pain syndrome in patient with:
- –
intermediate pre-test probability of CAD
- –
no ECG changes and serial enzyme negative
- (4.)
Detection of CAD in patients with chest pain syndrome with:
- –
uninterpretable or equivocal stress test (exercise, perfusion or stress echo)
- (5.)
Evaluation of cardiac morphology, structure and function:
- –
assessment of complex congenital heart disease
- –
valuation of coronary arteries in onset of heart failure to assess aetiology
- –
evaluation of cardiac masses in patient with limited echo, MRI or TEE
- –
evaluation of pericardium in patient with limited echo, MRI or TEE
- –
arterial mapping including internal mammary arteries prior to repeat cardiac surgical revascularisation
- –
evaluation of pulmonary veins prior to radiofrequency ablation
- –
coronary vein mapping for placement of biventricular pacemaker
- (6.)
Evaluation of aortic and pulmonary disease
- –
evaluation of suspected aortic dissection
- –
evaluation of suspected pulmonary embolism
Several multicentric clinical trials are underway to establish the true clinical benefits and advantages of coronary and cardiovascular CTA in clinical practice. Alternative pathways in patient management and clinical decisionmaking are foreseen with a major role assigned to cardiac CTA.
The advent of hybrid imaging
A new generation of hybrid scanners combining multidetector CT scanners with positron emission tomography (PET) scanners were recently introduced by different manufacturers. This new generation of combined PET/CT modalities allow for acquiring simultaneous anatomical images from CT and metabolic images from PET scans [
23,
24,
25]. PET imaging has evolved to become the reference technique for measurement of tissue viability and myocardial blood flow with short-lived radionuclides labelled with positron emitting isotopes. The use of fluorodeoxyglucose (FDG) labelled with 18F, an analog of glucose, has been well documented as a tracer of myocardial viability allowing to identify myocardial infarcts and differentiate scar tissue from viable or hibernating myocardium (
Figure 4). PET scans performed with FDG have become the method of choice for identifying the extent of residual viable myocardium that can benefit from revascularisation and interventions following acute myocardial infarcts. Quantitative analysis of the extent of viable myocardium was shown to be a good predictor of the effect of coronary revascularisation on myocardial contractility and ventricular function recovery after myocardial infarction. Furthermore, using other tracers to evaluate myocardial perfusion such as 13N labelled ammonia and 86Rb rubidium with PET imaging provide improved quantitative techniques for evaluation of regional myocardial blood flow more accurately than traditional scintigraphy techniques. With these tracers, PET scans can be performed at rest and after stress or exercise to detect stressinduced myocardial ischaemia and determine the severity of coronary artery disease [
24].
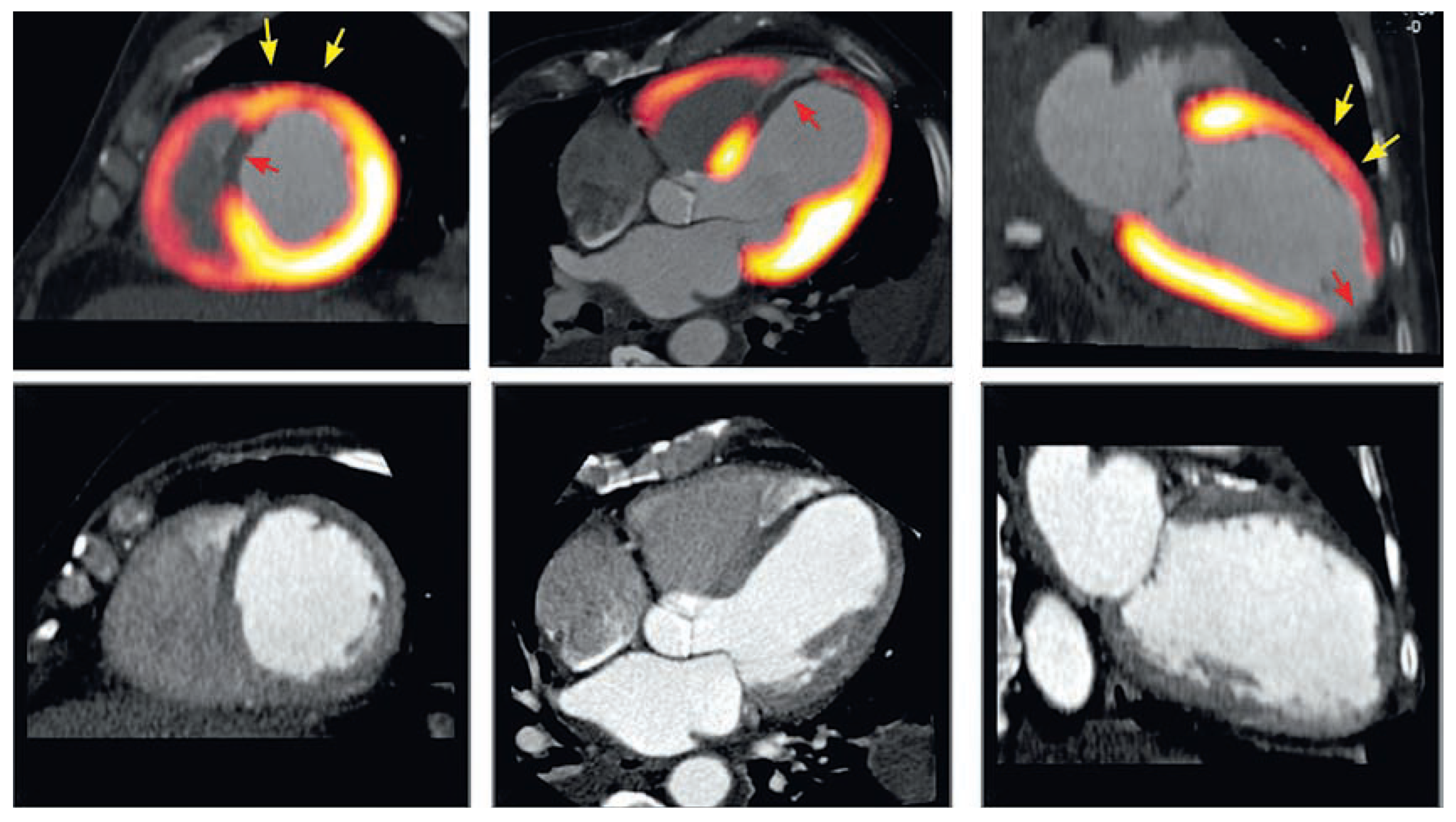
Figure 5.
Hybrid PET/CT images of the heart provide additional information on myocardial viability allowing differentiating segments with residual viable tissue (yellow arrows) from non-viable scar tissue (read arrow) in areas of myocardial infarction identified on CT images with significant wall thinning and hypokinesis (bottom row).
Figure 5.
Hybrid PET/CT images of the heart provide additional information on myocardial viability allowing differentiating segments with residual viable tissue (yellow arrows) from non-viable scar tissue (read arrow) in areas of myocardial infarction identified on CT images with significant wall thinning and hypokinesis (bottom row).
While extensive research over the past decades has shown the advantages of PET imaging over other diagnostic techniques, its widespread clinical use was limited by the limited availability of PET scanners and their relatively high cost. With the advent of hybrid scanners combining multidetector CT and PET scanners in one single machine, it is possible today to combine the anatomical information of coronary CT angiography with myocardial metabolism and perfusion from PET images in a single examination. These combined imaging devices open new perspectives on alternative clinical pathways for evaluating patients with CAD.
Awider adoption of these new hybrid scanners in the market due to their ability to perform different types of examinations is leading to a wider availability of the PET imaging techniques as well. It is anticipated that in the future a wider adoption of combined PET/CT techniques in cardiology will lead to better assessment of the severity and haemodynamic significance of coronary artery lesions prior to therapeutic interventions.
Discussion and conclusion
With the emergence of every new diagnostic tool comes the controversy of challenging the established methods and techniques. Coronary CTA is one among a constellation of new imaging modalities that will reshape clinical practice in cardiology and offer alternative pathways for diagnosis of coronary artery disease. The rapid evolution of the technology has exceeded the most optimistic predictions and has taken the whole medical community by surprise.
Coronary CTA adoption is rapidly growing while clinical evidences gathered from controlled studies lag behind the rapid evolution of the technology [
26,
27,
28]. In most cases, while clinical trials are undertaken, by the time sufficient results are obtained, the technology has already undergone a quantum leap in performance that renders the data obsolete. Sufficient data, however, have been published showing that the technique has reached a level of performance that establishes its value as a reliable alternative to coronary angiograms for diagnosis of coronary artery lesions. Further technical improvement of imaging devices can only improve its accuracy and help address remaining drawbacks such as radiation dose and irregular heart rates.
There is no doubt however that coronary CTA will have a significant impact on reducing the number of unnecessary invasive coronary arteriograms in patients with normal or nonsignificant coronary artery lesions [
4,
11,
12]. With the growing clinical evidence that not all coronary stenoses require therapeutic interventions and outcome studies showing that conservative treatment of significant lesions with minimal haemodynamic effect has the same outcome as invasive therapeutic interventions [
9,
29], coronary CTA will play an increasing role in clinical decision making [
27,
30].