Tango-Therapy Intervention for Older Adults with Cognitive Impairment Living in Nursing Homes: Effects on Quality of Life, Physical Abilities and Gait
Abstract
1. Introduction
2. Materials and Methods
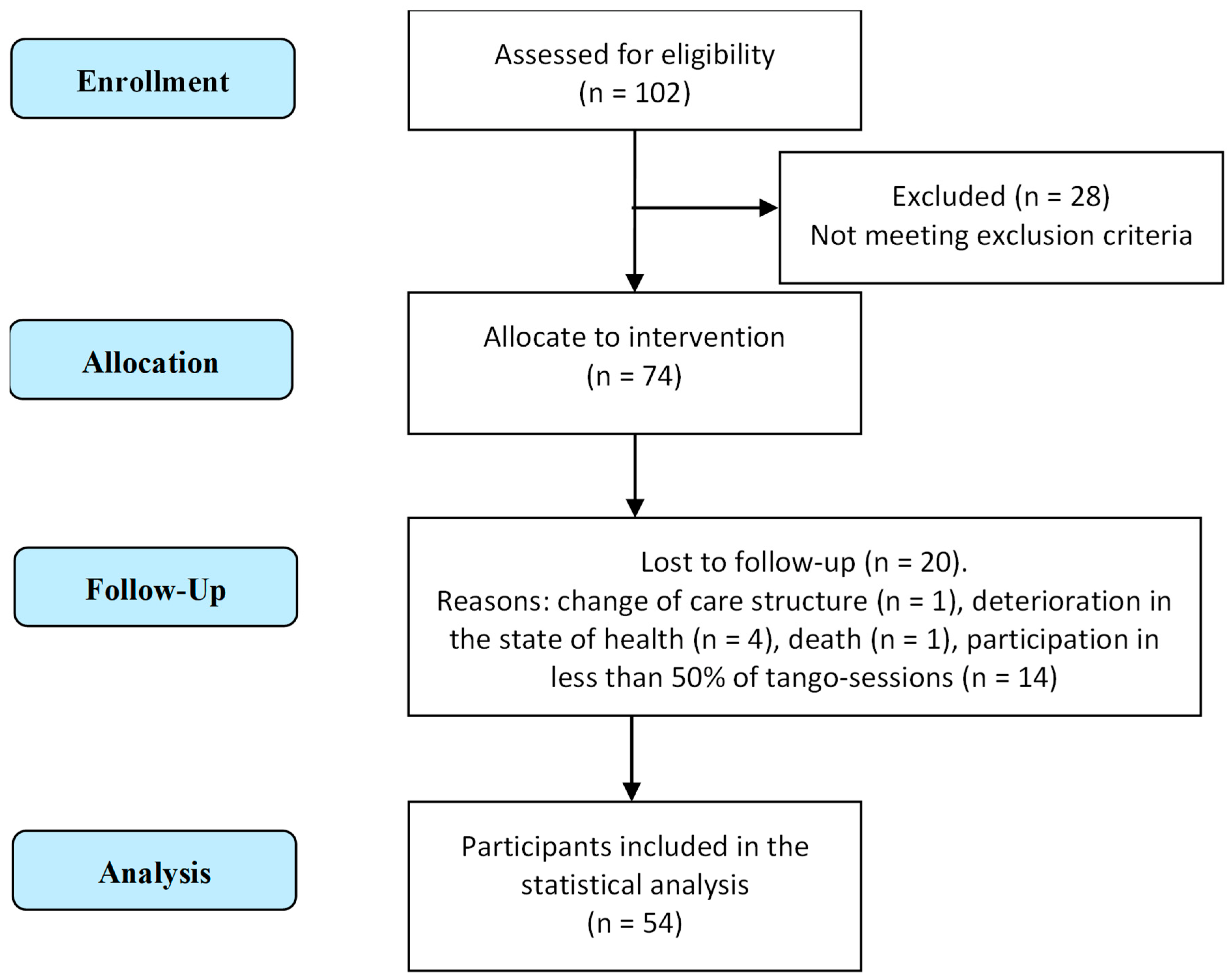
2.1. Participants
2.2. Ethics
2.3. Intervention
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Feasibility
3.3. Outcomes
3.3.1. Intergroup Comparison
3.3.2. Intragroup Comparison
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Taylor, M.E.; Close, J.C.T. Dementia. Handb. Clin. Neurol. 2018, 159, 303–321. [Google Scholar] [CrossRef] [PubMed]
- De Medeiros, M.M.D.; Carletti, T.M.; Magno, M.B.; Maia, L.C.; Cavalcanti, Y.W.; Rodrigues-Garcia, R.C.M. Does the institutionalization influence elderly’s quality of life? A systematic review and meta-analysis. BMC Geriatr. 2020, 20, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Manckoundia, P.; Mourey, F.; Pfitzenmeyer, P. Marche et démences. Ann. Réadaptation Médecine Phys. 2008, 51, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Carapellotti, A.M.; Stevenson, R.; Doumas, M. The efficacy of dance for improving motor impairments, non-motor symptoms, and quality of life in Parkinson’s disease: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0236820. [Google Scholar] [CrossRef]
- Patterson, K.K.; Wong, J.S.; Prout, E.C.; Brooks, D. Dance for the rehabilitation of balance and gait in adults with neurological conditions other than Parkinson’s disease: A systematic review. Heliyon 2018, 4, e00584. [Google Scholar] [CrossRef]
- Koch, S.C.; Mergheim, K.; Raeke, J.; Machado, C.B.; Riegner, E.; Nolden, J.; Diermayr, G.; von Moreau, D.; Hillecke, T.K. The Embodied Self in Parkinson’s Disease: Feasibility of a Single Tango Intervention for Assessing Changes in Psychological Health Outcomes and Aesthetic Experience. Front. Neurosci. 2016, 10, 287. [Google Scholar] [CrossRef]
- Goldstein-Levitas, N. Dance/Movement Therapy and Sensory Stimulation: A Holistic Approach to Dementia Care. Am. J. Danc. Ther. 2016, 38, 429–436. [Google Scholar] [CrossRef]
- Hackney, M.E.; Byers, C.; Butler, G.; Sweeney, M.; Rossbach, L.; Bozzorg, A. Adapted Tango Improves Mobility, Motor-Cognitive Function, and Gait but Not Cognition in Older Adults in Independent Living. J. Am. Geriatr. Soc. 2015, 63, 2105–2113. [Google Scholar] [CrossRef]
- Lötzke, D.; Ostermann, T.; Büssing, A. Argentine Tango in Parkinson Disease—A Systematic Review and Meta-Analysis. BMC Neurol. 2015, 15, 226. [Google Scholar] [CrossRef]
- Hackney, M.E.; Earhart, G.M. Recommendations for implementing tango classes for persons with Parkinson disease. Phys. Ther. Fac. Publ. 2010, 6, 41–52. [Google Scholar] [CrossRef]
- McKee, K.E.; Hackney, M.E. The Effects of Adapted Tango on Spatial Cognition and Disease Severity in Parkinson’s Disease. J. Mot. Behav. 2013, 45, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Hackney, M.E.; Earhart, G.M. Effects of Dance on Gait and Balance in Parkinson’s Disease: A Comparison of Partnered and Nonpartnered Dance Movement. Neurorehabil. Neural Repair 2010, 24, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Duncan, R.P.; Earhart, G.M. Randomized Controlled Trial of Community-Based Dancing to Modify Disease Progression in Parkinson Disease. Neurorehabil. Neural Repair 2012, 26, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Joyal, F. Tango, Corps à Corps Culturel: Danser en Tandem Pour Mieux Vivre; Collection Santé et Societé; Presses de l’Université de Québec: Québec, QC, Canada, 2009; ISBN 978-2-7605-2392-0. [Google Scholar]
- Koh, Y.; Hur, Y.; Kim, I.S.; Ha, C.W.; Noh, G. Tango Gait for Tango Therapy: Functional Anatomical Characteristics of Tango Gait (‘Tango Gaitology’). J. Tango 2019, 1, 33–47. [Google Scholar] [CrossRef]
- Koh, Y.; Kim, I.C.S.; Noh, G. Tango Therapy: Current Status and the Next Perspective. J. Clin. Rev. Case Rep. 2018, 3, 1–6. [Google Scholar] [CrossRef]
- McKinley, P.; Jacobson, A.; Leroux, A.; Bednarczyk, V.; Rossignol, M.; Fung, J. Effect of a Community-Based Argentine Tango Dance Program on Functional Balance and Confidence in Older Adults. J. Aging Phys. Act. 2008, 16, 435–453. [Google Scholar] [CrossRef]
- Bracco, L.; Poirier, G.; Pinto-Carral, A.; Mourey, F. Effect of Dance Therapy on the Physical Abilities of Older Adults with Dementia: A Systematic Review. Eur. J. Geriatr. Gerontol. 2021, 3, 134–142. [Google Scholar] [CrossRef]
- Karkou, V.; Meekums, B. Dance Movement Therapy for Dementia. Cochrane Database Syst. Rev. 2017, 2017, CD011022. [Google Scholar] [CrossRef]
- Nicotra, A. In Contatto con la Realtà. Tango et Danza Movimento Terapia; Ephemeria Editrice: Macerata, Italy, 2018. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Perneczky, R.; Wagenpfeil, S.; Komossa, K.; Grimmer, T.; Diehl, J.; Kurz, A. Mapping Scores Onto Stages: Mini-Mental State Examination and Clinical Dementia Rating. Am. J. Geriatr. Psychiatry 2006, 14, 139–144. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Delphin-Combe, F.; Dauphinot, V.; Denormandie, P.; Sanchez, S.; Hay, P.-E.; Moutet, C.; Krolak-Salmon, P. The Scale of instantaneous wellbeing: Validity in a population with major neurocognitive disorders. Gériatrie Psychol. Neuropsychiatr. Du Viellissement 2018, 16, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Treacy, D.; Hassett, L. The Short Physical Performance Battery. J. Physiother. 2018, 64, 61. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association With Self-Reported Disability and Prediction of Mortality and Nursing Home Admission Energetic cost of walking in older adults View project IOM committee on cognitive agi. J. Gerontol. 1994, 49, 85–94. [Google Scholar] [CrossRef] [PubMed]
- The Staff of The Benjamin Rose Hospital. Multidisciplinary study of illness in aged persons. I. Methods and preliminary results. J. Chronic Dis. 1958, 7, 332–345. [Google Scholar] [CrossRef]
- Cousi, C.; Igier, V.; Quintard, B. French cross-cultural adaptation and validation of the Quality of Life-Alzheimer’s Disease scale in Nursing Homes (QOL-AD NH). Health Qual. Life Outcomes 2021, 19, 219. [Google Scholar] [CrossRef] [PubMed]
- Wolak, A.; Novella, J.-L.; Drame, M.; Guillemin, F.; Di Pollina, L.; Ankri, J.; Aquino, J.-P.; Morrone, I.; Blanchard, F.; Jolly, D. Transcultural adaptation and psychometric validation of a French-language version of the QoL-AD. Aging Ment. Health 2009, 13, 593–600. [Google Scholar] [CrossRef]
- Hoe, J.; Katona, C.; Roch, B.; Livingston, G. Use of the QOL-AD for measuring quality of life in people with severe dementia—The LASER-AD study. Age Ageing 2005, 34, 130–135. [Google Scholar] [CrossRef]
- O’Caoimh, R.; O’Donovan, M.R.; Monahan, M.P.; Dalton O’Connor, C.; Buckley, C.; Kilty, C.; Fitzgerald, S.; Hartigan, I.; Cornally, N. Psychosocial Impact of COVID-19 Nursing Home Restrictions on Visitors of Residents With Cognitive Impairment: A Cross-Sectional Study as Part of the Engaging Remotely in Care (ERiC) Project. Front. Psychiatry 2020, 11, 585373. [Google Scholar] [CrossRef]
- Handing, E.P.; Leng, X.I.; Kritchevsky, S.B.; Craft, S. Association between physical performance and cognitive function in older adults across multiple studies: A pooled analysis study. Innov. Aging 2020, 4, igaa050. [Google Scholar] [CrossRef]
- Logsdon, R.G.; Gibbons, L.E.; McCurry, S.M.; Teri, L. Assessing quality of life in older adults with cognitive impairment. Psychosom. Med. 2002, 64, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Conde-Sala, J.L.; Garre-Olmo, J.; Turró-Garriga, O.; López-Pousa, S.; Vilalta-Franch, J. Factors related to perceived quality of life in patients with Alzheimer’s disease: The patient’s perception compared with that of caregivers. Int. J. Geriatr. Psychiatry 2009, 24, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Baud Mermoud, V.; Morin, D. Regards croisés entre l’évaluation de la qualité de vie perçue par le résident hébergé en établissement médico-social et par le soignant référent. Rech. Soins Infirm. 2016, 126, 38–50. [Google Scholar] [CrossRef]
- Guzmán-García, A.; Hughes, J.C.; James, I.A.; Rochester, L.; Guzman-Garcia, A.; Hughes, J.C.; James, I.A.; Rochester, L. Dancing as a Psychosocial Intervention in Care Homes: A Systematic Review of the Literature. Int. J. Geriatr. Psychiatry 2013, 28, 914–924. [Google Scholar] [CrossRef]
- Duignan, D.; Hedley, L.; Milverton, R. Exploring Dance as a Therapy for Symptoms and Social Interaction in a Dementia Care Unit. Nurs. Times 2009, 105, 19–22. [Google Scholar]
- Koh, W.L.E.; Low, F.; Kam, J.W.; Rahim, S.; Ng, W.F.; Ng, L.L. Person-Centred Creative Dance Intervention for Persons with Dementia Living in the Community in Singapore. Dementia 2020, 19, 2430–2443. [Google Scholar] [CrossRef]
- Hameed, S.; Shah, J.M.; Ting, S.; Gabriel, C.; Tay, S.Y.; Chotphoksap, U.; Liong, A. Improving the Quality of Life in Persons with Dementia through a Pilot Study of a Creative Dance Movement Programme in an Asian Setting. Int. J. Neurorehabil. 2018, 5, 1–4. [Google Scholar] [CrossRef]
- Müller, P.; Rehfeld, K.; Schmicker, M.; Hökelmann, A.; Dordevic, M.; Lessmann, V.; Brigadski, T.; Kaufmann, J.; Müller, N.G. Evolution of Neuroplasticity in Response to Physical Activity in Old Age: The Case for Dancing. Front. Aging Neurosci. 2017, 9, 56. [Google Scholar] [CrossRef]
- Teixeira-Machado, L.; Arida, R.M.; de Mari, J.J.M. Dance for neuroplasticity: A descriptive systematic review. Neurosci. Biobehav. Rev. 2019, 96, 232–240. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J. Nonpharmacologic Interventions for Inappropriate Behaviors in Dementia: A Review, Summary, and Critique. Am. J. Geriatr. Psychiatry 2001, 9, 361–381. [Google Scholar] [CrossRef]
- Murphy, K.; Shea, E.O.; Cooney, A. Quality of life for older people living in long-stay settings in Ireland. J. Clin. Nurs. 2007, 16, 2167–2177. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Rodríguez, P.; Díaz de Bustamante, M.; Aparicio Mollá, S.; Arenas, M.C.; Jiménez-Armero, S.; Lacosta Esclapez, P.; González-Espinoza, L.; Bermejo Boixareu, C. Functional, cognitive, and nutritional decline in 435 elderly nursing home residents after the first wave of the COVID-19 Pandemic. Eur. Geriatr. Med. 2021, 12, 1137–1145. [Google Scholar] [CrossRef] [PubMed]
- Hokkanen, L.; Rantala, L.; Remes, A.M.; Harkonen, B.; Viramo, P.; Winblad, I. Dance/Movement Therapeutic Methods in Management of Dementia. J. Am. Geriatr. Soc. 2008, 56, 771–772. [Google Scholar] [CrossRef] [PubMed]
- Machacova, K.; Vankova, H.; Volicer, L.; Veleta, P.; Holmerova, I. Dance as Prevention of Late Life Functional Decline Among Nursing Home Residents. J. Appl. Gerontol. 2017, 36, 1453–1470. [Google Scholar] [CrossRef]
- Wildes, T.M. Make time for gait speed: Vital to staging the aging. Blood 2019, 134, 334–336. [Google Scholar] [CrossRef] [PubMed]
- Fontanesi, C.; DeSouza, J.F.X. Beauty That Moves: Dance for Parkinson’s Effects on Affect, Self-Efficacy, Gait Symmetry, and Dual Task Performance. Front. Psychol. 2021, 11, 600440. [Google Scholar] [CrossRef]
- Rios Romenets, S.; Anang, J.; Fereshtehnejad, S.-M.; Pelletier, A.; Postuma, R. Tango for treatment of motor and non-motor manifestations in Parkinson’s disease: A randomized control study. Complement. Ther. Med. 2015, 23, 175–184. [Google Scholar] [CrossRef]
- Sacco, K.; Cauda, F.; Cerliani, L.; Mate, D.; Duca, S.; Geminiani, G.C. Motor imagery of walking following training in locomotor attention. The effect of ‘the tango lesson’. Neuroimage 2006, 32, 1441–1449. [Google Scholar] [CrossRef]
- Koh, Y.; Hur, Y.; Noh, G. Basic tango elements for tango therapy. J. Tango 2019, 1, 1–5. [Google Scholar] [CrossRef]
- Studenski, S. Challenges in Clinical Aging Research: Building the Evidence Base for Care of the Older Adult. J. Am. Geriatr. Soc. 2008, 56, 2351–2352. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2010. [Google Scholar]
| Session Components | Activities |
|---|---|
| Pre-warm-up | Organizing the seating arrangement in the room, greeting the participants, engaging in small talk. |
| Warm-up | Seated exercises to mobilize lower and upper limbs, head and trunk as well as singing to warm-up the voice and foster social connection. |
| Main part | Different aspects of tango therapy were practiced. This could include technical aspects, such as forward and backward walking, side-step, square, rectangle, as well as improvisation via spontaneous expression. The physical connection via ‘Abrazo’ (embrace) or other interactions were also an important aspect of the intervention. |
| Cool-down | Seated rituals, such as singing and breathing exercises. |
| Social exchange | The sessions were frequently followed by coffee and cake, or participants stayed to talk with each other and facilitators. |
| Song Title | Artist |
|---|---|
| Le plus beau tango du monde | Tino Rossi |
| Paloma | Tino Rossi |
| Mon Amant de Saint Jean | Lucienne Delyle |
| Voulez-Vous Danser Grand’mère | Lina Margy |
| Vous Permettez Monsieur | Salvatore Adamo |
| Variables | Total (n = 54) | SMCI (n = 41) | MNCI (n = 13) |
|---|---|---|---|
| Sex, females, n (%) | 42 (78) | 32 (78) | 10 (77) |
| Age (years), M ± SD | 84.9 ± 6.7 | 84.9 ± 6.8 | 84.9 ± 6.9 |
| Charlson Index, M ± SD | 5.6 ± 1.6 | 5.4 ± 1.2 | 6.4 ± 2.6 |
| MMSE, score (range 0–30) M ± SD | 14.5 ± 7.4 | 11.3 ± 5.1 | 24.5 ± 2.5 |
| Katz Index, score (range 0–6) M ± SD | 4.5 ± 1.3 | 4.3 ± 1.3 | 5.4± 0.8 |
| Variables | Pre-Test M ± SD | Post-Test M ± SD | p-Value | |
|---|---|---|---|---|
| SPPB | Balance subscore (0–4) | 2.1 ± 0.9 | 2.3 ± 1 | 0.221 |
| Gait speed subscore (0–4) | 2 ± 1 | 2 ± 1.1 | 0.725 | |
| Sit to stand subscore (0–4) | 1.2 ± 1.2 | 1.2 ± 1.2 | 0.862 | |
| Total score (0–12 | 5.3 ± 2.4 | 5.4 ± 2.6 | 0.876 | |
| Katz Index, score (range 0–6) M ± SD | 4.5 ± 1.3 | 4.3 ± 1.2 | 0.253 | |
| QoL-AD, score (range 13–52) | Participant | 33.8 ± 5.4 | 34.3 ± 5.7 | 0.172 |
| Caregiver | 31.9 ± 4.5 | 33 ± 4.2 | 0.103 | |
| Weighted composite score | 33.1 ± 4.6 | 34 ± 4.5 | 0.030 * | |
| Variables | SMCI (n = 41) | MNCI (n = 13) | Intergroup Comparison | Intragroup Comparison | |||||
|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1/T1 | T2/T2 | SMCI | MNCI | ||
| SPPB | Balance (0–4) | 2.05 ± 0.8 | 2.2 ± 0.9 | 2.4 ± 1.2 | 2.7 ± 1.2 | 0.426 | 0.075 | 0.422 | 0.305 |
| Gait speed (0–4) | 1.9 ± 0.9 | 1.7 ± 0.9 | 2.5 ± 1.4 | 2.7 ± 1.3 | 0.171 | 0.020 * | 0.486 | 0.527 | |
| Sit to stand (0–4) | 1 ± 0.9 | 1 ± 1 | 2 ± 1.6 | 1.9 ± 1.4 | 0.042 * | 0.026 * | 0.966 | 0.725 | |
| Total (0–12) | 4.9 ± 1.8 | 4.8 ± 1.9 | 6.8 ± 3.5 | 7.2 ± 3.6 | 0.09 | 0.025 * | 0728 | 0.751 | |
| Katz Index | 4.3 ± 1.3 | 4 ± 1.2 | 5.4 ± 0.8 | 5.3 ± 0.9 | 0.003 * | 0.001 * | 0.25 | 0.914 | |
| QoL-AD (13–52) | Participant | 33.3 ± 5.1 | 34 ± 4.9 | 35 ± 6.1 | 35.2 ± 7.4 | 0.472 | 0.776 | 0.122 | 0.858 |
| Caregiver | 31.4 ± 4.2 | 32.4 ± 4.2 | 33.3 ± 5 | 34.7 ± 3.9 | 0.238 | 0.203 | 0.205 | 0.441 | |
| Composite score | 32.4 ± 4.2 | 33.6 ± 4 | 34.4 ± 5.1 | 35 ± 5.7 | 0.368 | 0.434 | 0.038 * | 0.552 | |
| Intervention Attendance | 7.8 ± 1.7 | 8.7 ± 1.6 | 0.084 | ||||||
| EVIBE | 4.5 ± 0.5 | 4.7 ± 0.4 | 0.087 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bracco, L.; Cornaro, C.; Pinto-Carral, A.; Koch, S.C.; Mourey, F. Tango-Therapy Intervention for Older Adults with Cognitive Impairment Living in Nursing Homes: Effects on Quality of Life, Physical Abilities and Gait. Int. J. Environ. Res. Public Health 2023, 20, 3521. https://doi.org/10.3390/ijerph20043521
Bracco L, Cornaro C, Pinto-Carral A, Koch SC, Mourey F. Tango-Therapy Intervention for Older Adults with Cognitive Impairment Living in Nursing Homes: Effects on Quality of Life, Physical Abilities and Gait. International Journal of Environmental Research and Public Health. 2023; 20(4):3521. https://doi.org/10.3390/ijerph20043521
Chicago/Turabian StyleBracco, Lucía, Clara Cornaro, Arrate Pinto-Carral, Sabine C. Koch, and France Mourey. 2023. "Tango-Therapy Intervention for Older Adults with Cognitive Impairment Living in Nursing Homes: Effects on Quality of Life, Physical Abilities and Gait" International Journal of Environmental Research and Public Health 20, no. 4: 3521. https://doi.org/10.3390/ijerph20043521
APA StyleBracco, L., Cornaro, C., Pinto-Carral, A., Koch, S. C., & Mourey, F. (2023). Tango-Therapy Intervention for Older Adults with Cognitive Impairment Living in Nursing Homes: Effects on Quality of Life, Physical Abilities and Gait. International Journal of Environmental Research and Public Health, 20(4), 3521. https://doi.org/10.3390/ijerph20043521







