Annual Direct Cost and Cost-Drivers of Systemic Lupus Erythematosus: A Multi-Center Cross-Sectional Study from CSTAR Registry
Abstract
1. Introduction
2. Materials and Methods
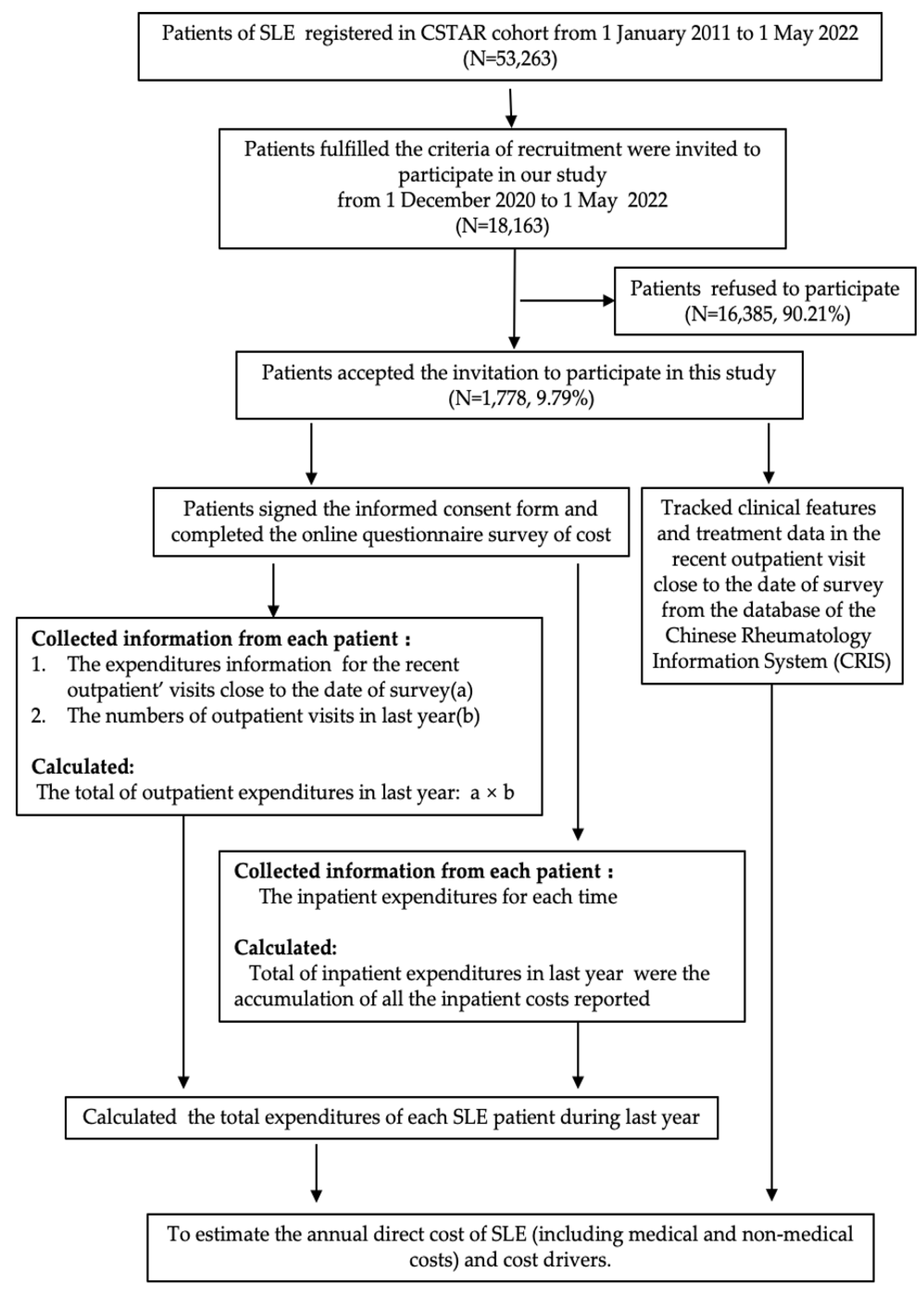
2.1. Study Design
2.2. Data Collection
2.3. Measurements
2.4. Direct Cost Calculation
2.5. Statistical Analysis
3. Results
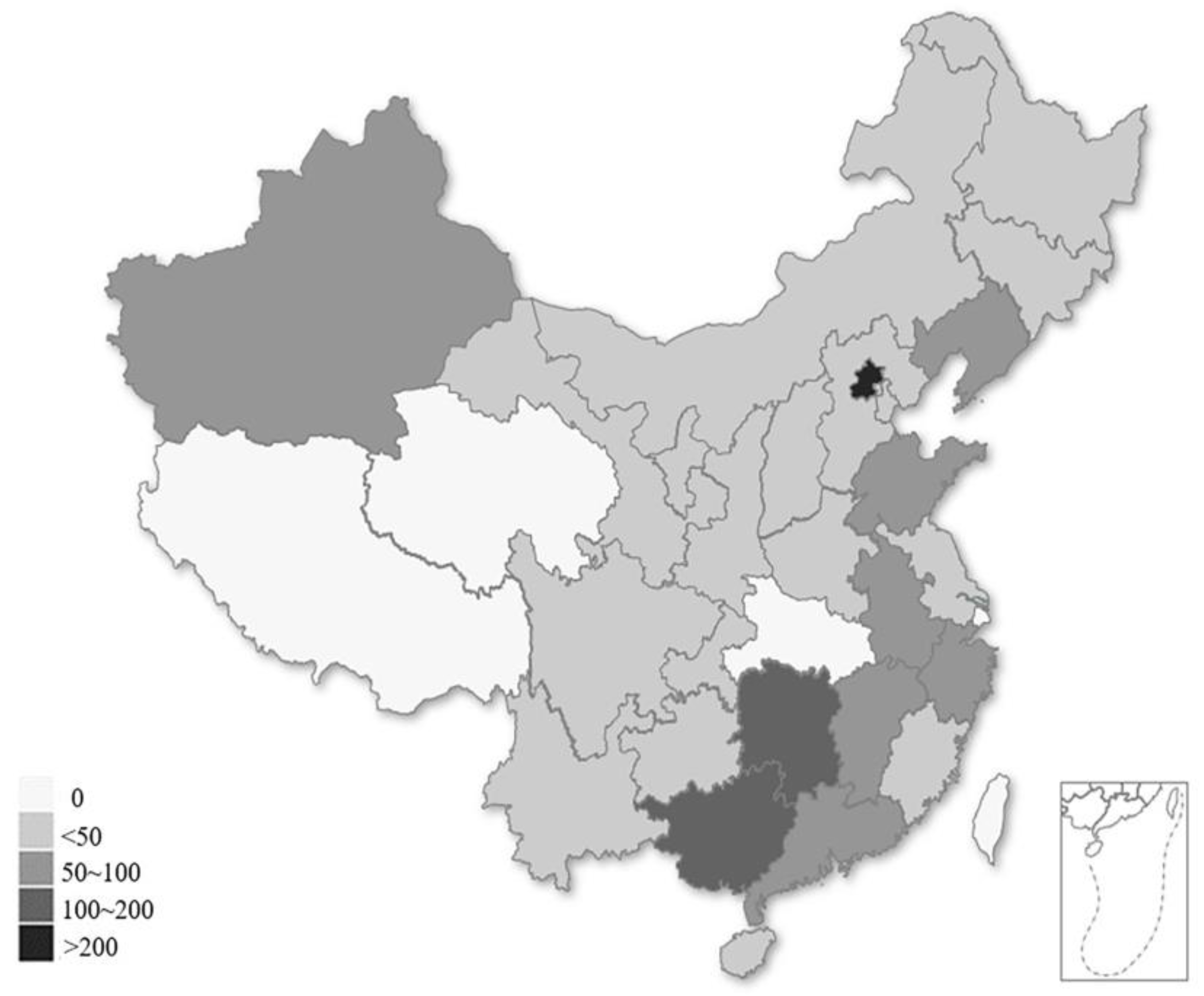
3.1. Socio-Demographic and Clinical Characteristics
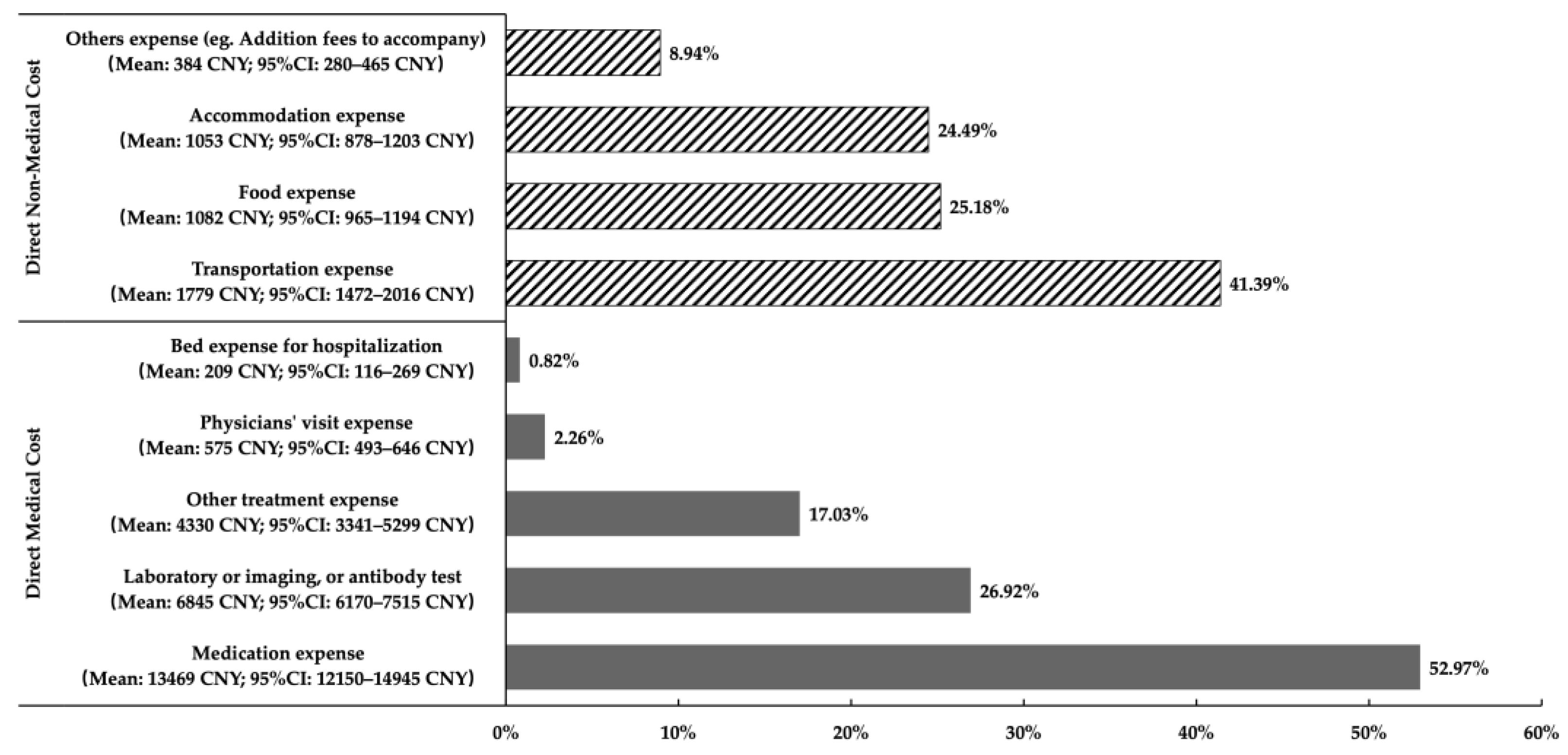
3.2. Direct Cost of SLE Patients
3.3. Cost-Driving Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Segura, B.T. Damage accrual and mortality over long-term follow-up in 300 patients with systemic lupus erythematosus in a multi-ethnic British cohort. Rheumatology 2020, 59, 524–533. [Google Scholar] [CrossRef] [PubMed]
- Chambers, S.A. Damage and mortality in a group of British patients with systemic lupus erythematosus followed up for over 10 years. Rheumatology 2009, 48, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Urowitz, M.B. Evolution of disease burden over five years in a multicenter inception systemic lupus erythematosus cohort. Arthritis Care Res. 2012, 64, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Nusbaum, J.S. Sex Differences in Systemic Lupus Erythematosus: Epidemiology, Clinical Considerations, and Disease Pathogenesis. Mayo. Clin. Proc. 2020, 95, 384–394. [Google Scholar] [CrossRef] [PubMed]
- Grant, E.C. Systemic lupus erythematosus. Lancet 2001, 358, 586. [Google Scholar] [CrossRef]
- Tian, X. The challenges and future perspective for the management of systemic lupus erythematosus in China: A concise annual report of 2020. Rheumatol. Immunol. Res. 2022, 3, 38–44. [Google Scholar] [CrossRef]
- Hodgson, T.A. Cost-of-illness methodology: A guide to current practices and procedures. Milbank Mem. Fund Q. Health. Soc. 1982, 60, 429–462. [Google Scholar] [CrossRef]
- Murimi-Worstell, I.B. Healthcare Utilization and Costs of Systemic Lupus Erythematosus by Disease Severity in the United States. J. Rheumatol. 2021, 48, 385–393. [Google Scholar] [CrossRef]
- Fatoye, F. Direct health system costs for systemic lupus erythematosus patients in Alberta, Canada. PLoS ONE 2021, 16, e0251409. [Google Scholar] [CrossRef]
- Miyazaki, C. Treatment patterns and medical cost of systemic lupus erythematosus patients in Japan: A retrospective claims database study. J. Med. Econ. 2020, 23, 786–799. [Google Scholar] [CrossRef]
- Park, S.Y. Direct medical costs and their predictors in South Korean patients with systemic lupus erythematosus. Rheumatol. Int. 2015, 35, 1809–1815. [Google Scholar] [CrossRef] [PubMed]
- Schwarting, A. The Burden of Systemic Lupus Erythematosus in Germany: Incidence, Prevalence, and Healthcare Resource Utilization. Rheumatol. Ther. 2021, 8, 375–393. [Google Scholar] [CrossRef] [PubMed]
- Samnaliev, M. Health-care utilization and costs in adults with systemic lupus erythematosus in the United Kingdom: A real-world observational retrospective cohort analysis. Rheumatol. Adv. Pract. 2021, 5, rkab071. [Google Scholar] [CrossRef] [PubMed]
- Bertsias, G. Clinical and financial burden of active lupus in Greece: A nationwide study. Lupus 2016, 25, 1385–1394. [Google Scholar] [CrossRef]
- Zhu, T.Y. Systemic lupus erythematosus with neuropsychiatric manifestation incurs high disease costs: A cost-of-illness study in Hong Kong. Rheumatology 2009, 48, 564–568. [Google Scholar] [CrossRef]
- Chiu, Y.M. Medical costs incurred by organ damage caused by active disease, comorbidities and side effect of treatments in systemic lupus erythematosus patients: A Taiwan nationwide population-based study. Rheumatol. Int. 2016, 36, 1507–1514. [Google Scholar] [CrossRef]
- Zhu, T.Y. Cost-of-illness studies in systemic lupus erythematosus: A systematic review. Arthritis Care Res. 2011, 63, 751–760. [Google Scholar] [CrossRef]
- Kim, H. An increased disease burden of autoimmune inflammatory rheumatic diseases in Korea. Semin. Arthritis Rheum. 2020, 50, 526–533. [Google Scholar] [CrossRef]
- Akobundu, E. Cost-of-illness studies: A review of current methods. Pharmacoeconomics 2006, 24, 869–890. [Google Scholar] [CrossRef]
- Yeo, A.L. Lupus Low Disease Activity State and Reduced Direct Health Care Costs in Patients With Systemic Lupus Ery-thematosus. Arthritis Care Res. 2020, 72, 1289–1295. [Google Scholar] [CrossRef]
- Bell, C.F. An evaluation of costs associated with overall organ damage in patients with systemic lupus erythematosus in the United States. Lupus 2022, 31, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Doria, A. Clinical profile and direct medical cost of care of adults presenting with systemic lupus erythematosus in Italy. Clin. Exp. Rheumatol. 2015, 33, 375–384. [Google Scholar] [PubMed]
- Jonsen, A. Total cost and cost predictors in systemic lupus erythematosus—8-years follow-up of a Swedish inception cohort. Lupus 2015, 24, 1248–1256. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L. Treatment adherence and disease burden of individuals with rheumatic diseases admitted as outpatients to a large rheumatology center in Shanghai, China. Patient Prefer. Adherence 2017, 11, 1591–1601. [Google Scholar] [CrossRef]
- Huang, Q. Analysis of the annual direct economic burden and influencing factors of patients with systemic lupus erythematosus in Anhui province. J. Bengbu Med. 2020, 45, 536–540. [Google Scholar]
- Desgagne, A. The use of the bootstrap statistical method for the pharmacoeconomic cost analysis of skewed data. Pharmacoeconomics 1998, 13, 487–497. [Google Scholar] [CrossRef]
- Carpenter, J. Bootstrap confidence intervals: When, which, what? A practical guide for medical statisticians. Stat. Med. 2000, 19, 1141–1164. [Google Scholar] [CrossRef]
- National Bureau of Statistics of China. Available online: http://www.stats.gov.cn/tjsj/ndsj/2021/indexch.htm (accessed on 8 October 2022).
- Tanaka, Y. Disease severity and economic burden in Japanese patients with systemic lupus erythematosus: A retrospective, observational study. Int. J. Rheum. Dis. 2018, 21, 1609–1618. [Google Scholar] [CrossRef]
- Carter, E. The global burden of SLE: Prevalence, health disparities and socioeconomic impact. Nat. Rev. Rheumatol. 2016, 12, 605–620. [Google Scholar] [CrossRef]
- Li, M. Chinese SLE Treatment and Research group (CSTAR) registry: I. Major clinical characteristics of Chinese patients with systemic lupus erythematosus. Lupus 2013, 22, 1192–1199. [Google Scholar] [CrossRef]
- Kasitanon, N. Predictors of survival in systemic lupus erythematosus. Medicine 2006, 85, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Alarcon, G.S. Systemic lupus erythematosus in three ethnic groups. XIV. Poverty, wealth, and their influence on disease activity. Arthritis Rheum. 2004, 51, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Pons-Estel, B.A. The GLADEL multinational Latin American prospective inception cohort of 1214 patients with systemic lupus erythematosus: Ethnic and disease heterogeneity among “Hispanics”. Medicine 2004, 83, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Doria, A. Annual direct medical cost of active systemic lupus erythematosus in five European countries. Ann. Rheum. Dis. 2014, 73, 154–160. [Google Scholar] [CrossRef]
- Khamashta, M.A. The cost of care of systemic lupus erythematosus (SLE) in the UK: Annual direct costs for adult SLE patients with active autoantibody-positive disease. Lupus 2014, 23, 273–283. [Google Scholar] [CrossRef]
- Jiang, M. Disease and economic burden increase with systemic lupus erythematosus severity 1 year before and after diagnosis: A real-world cohort study, United States, 2004–2015. Lupus Sci. Med. 2021, 8, e000503. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z. Long-term outcomes of patients with systemic lupus erythematosus: A Multicenter Cohort Study from CSTAR registry. Rheumatol. Immunol. Res. 2021, 2, 195–202. [Google Scholar] [CrossRef]
- Huscher, D. Cost of illness in rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and systemic lupus erythematosus in Germany. Ann. Rheum. Dis. 2006, 65, 1175–1183. [Google Scholar] [CrossRef]
- Panopalis, P. Health care costs and costs associated with changes in work productivity among persons with systemic lupus erythematosus. Arthritis Rheum. 2008, 59, 1788–1795. [Google Scholar] [CrossRef]
- Anghel, L.A. Medication adherence and persistence in patients with autoimmune rheumatic diseases: A narrative review. Patient Prefer. Adherence 2018, 12, 1151–1166. [Google Scholar] [CrossRef]
- Abdul-Sattar, A.B. Determinants of medication non-adherence in Egyptian patients with systemic lupus erythematosus: Sharkia Governorate. Rheumatol. Int. 2015, 35, 1045–1051. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 1778) | |
|---|---|
| Age (years), mean (SD) | 33.8 (10.8) |
| Gender, females, n (%) | 1646 (92.58%) |
| Disease duration (years), median (p25–p75) | 4.9 (1.8–9.5) |
| Newly treated patients, n (%) | 133 (7.48%) |
| Regions | |
| Western | 372 (20.92%) |
| Central | 429 (24.13%) |
| Eastern | 977 (54.95%) |
| Medical insurance, n (%) | 1508 (84.81%) |
| Patients’ incomes during last year (CNY), median (p25–p75) | 27,600 (0–50,000) |
| Numbers of outpatient visits during last year, median (p25–p75) | 5 (3–8) |
| Hospitalization during last year, n (%) | 345 (19.40%) |
| Hospitalization days for inpatients, median (p25–p75) | 11 (7–17) |
| Positive antinuclear antibody (ANA), n (%) | 1691 (95.11%) |
| Positive anti-double-stranded DNA (dsDNA), n (%) | 1359 (76.43%) |
| Abnormal liver function, n (%) | 380 (21.37%) |
| Low complement, n (%) | 511 (28.74%) |
| Physician’s global assessment, median (p25–p75) | 0.80 (0.40–1.10) |
| SLEDAI scores, median (p25–p75) | 2.00 (0–4.00) |
| Severity of the disease, n (%) | |
| Mild (SLEDAI score < 8) | 1600 (89.99%) |
| Moderate to severe (SLEDAI score ≥ 8) | 178 (10.01%) |
| Disease activity state, n (%) | |
| Remission or LLDAS | 643 (36.16%) |
| Active disease | 1135 (63.84%) |
| System involvement, n (%) | |
| Peripheral vascular system | 919 (51.69%) |
| Serositis | 740 (41.62%) |
| Skin system | 1154 (64.90%) |
| Musculoskeletal system | 942 (52.98%) |
| Renal system | 685 (38.53%) |
| Neuropsychiatric system | 115 (6.47%) |
| Gastrointestinal system | 38 (2.14%) |
| Ocular system | 22 (1.24%) |
| Cardiovascular system | 127 (7.14%) |
| Pulmonary system | 17 (0.96%) |
| Number of organs damaged, n (%) | |
| 0 or 1 | 404 (22.72%) |
| 2 or more | 1374 (77.28%) |
| Treatment of biologics, n (%) | 148 (8.32%) |
| Treatment of glucocorticoids, n (%) | 1442 (81.10%) |
| 0 mg/day (none) | 336 (18.90%) |
| ≤7.5mg/day | 533 (29.98%) |
| >7.5 and ≤15 mg/day | 510 (28.68%) |
| >15 mg/day | 399 (22.44%) |
| Annual Direct Medical Cost | Annual Direct Non-Medical Cost | Total Annual Direct Cost | |
|---|---|---|---|
| Mean ± SD | 25,520 ± 49,592 | 4298 ± 10,938 | 29,818 ± 53,389 |
| Median (p25–p75) | 11,698 (4869–25,644) | 1650 (568–4270) | 14,867 (6820–31,180) |
| Arithmetic mean (bootstrap) | 25,429 | 4298 | 29,727 |
| Bootstrap 95% CI | 23,346 to 27,733 | 3745 to 4762 | 27,384 to 32,319 |
| Proportion of total direct cost | 85.5% | 14.5% | 100% |
| Features | N | Arithmetic Mean (Bootstrap) | 95% CI (Bootstrap) | Median (IQR) | p-Value * |
| Gender | 0.81 | ||||
| Male | 132 | 27,225 | 21,270–33,300 | 15,424 (5429–24,578) | |
| Female | 1646 | 29,928 | 27,470–32,730 | 14,833 (6920–30,764) | |
| Age groups | 0.50 | ||||
| <18 years | 55 | 36,347 | 11,533–53,543 | 17,720 (7968–33,000) | |
| 18–39 years | 1268 | 29,417 | 26,473–32,453 | 14,292 (6899–29,717) | |
| ≥40 years | 455 | 29,785 | 25,722–33,671 | 15,275 (6522–35,093) | |
| Disease duration | <0.001 | ||||
| ≤3 years | 651 | 35,064 | 30,794–39,189 | 18,120 (8405–38,090) | |
| 3–8 years | 555 | 26,454 | 21,568–31,057 | 12,276 (5875–26,264) | |
| >8 years | 572 | 26,822 | 23,033–30,352 | 12,836 (6349–30,263) | |
| Newly treated patients | <0.001 | ||||
| Yes | 133 | 37,870 | 29,540–45,038 | 25,162 (9231–48,000) | |
| No | 1645 | 29,071 | 26,578–31,755 | 14,165 (6650–30,223) | |
| Region | 0.24 | ||||
| Western | 372 | 31,075 | 26,530–35,979 | 16,558 (7315–32,999) | |
| Central | 429 | 29,057 | 24,463–33,994 | 14,232 (6772–30,048) | |
| Eastern | 977 | 29,507 | 25,908–32,796 | 13,912 (6724–30,760) | |
| Health insurance | 0.85 | ||||
| No | 270 | 28,369 | 22,106–33,699 | 14,158 (7433–30,223) | |
| Yes | 1508 | 29,972 | 27,317–32,814 | 14,970 (6656–31,496) | |
| Hospitalization during last year | <0.001 | ||||
| Yes | 345 | 64,755 | 56,272–72,590 | 40625 (23,272–71,727) | |
| No | 1433 | 21,289 | 19,089–23,483 | 11,436 (5667–22,384) | |
| ANA | 0.01 | ||||
| Positive | 1691 | 30,301 | 27,838–33,020 | 15,231 (7000–32,100) | |
| Negative | 87 | 18,556 | 12,889–23,761 | 10,401 (5040–24,200) | |
| dsDNA | 0.53 | ||||
| Positive | 1359 | 29,613 | 27,178–32,371 | 14,833 (6950–31,385) | |
| Negative | 419 | 30,093 | 23,515–35,909 | 15,450 (6348–30,280) | |
| Abnormal liver function | 0.04 | ||||
| Yes | 380 | 31,398 | 26,219–36,323 | 16,879 (7473–35,901) | |
| No | 1398 | 29,272 | 26,268–32,177 | 14,072 (6566–30,512) | |
| Low complement | 0.07 | ||||
| Yes | 511 | 33,279 | 28,820–38,023 | 16,379 (6922–34,707) | |
| No | 1267 | 28,299 | 25,529–31,295 | 14,232 (6800–30,312) | |
| Severity of the disease | <0.001 | ||||
| Mild | 1600 | 27,498 | 25,136–30,097 | 13,755 (6576–29,213) | |
| Moderate to severe | 178 | 49,720 | 39,578–59,592 | 27,269 (11,730–55,497) | |
| Disease Activity State | <0.001 | ||||
| Remission or LLDAS | 643 | 21,337 | 18,932–23,841 | 10,600 (5006–23,220) | |
| Active disease | 1135 | 34,492 | 31,095–38,342 | 17,500 (8216–36,454) | |
| System involvement | |||||
| Skin system | 0.67 | ||||
| Normal | 624 | 30,645 | 25,997–35,103 | 15,167 (6872–31,724) | |
| Abnormal | 1154 | 29,231 | 26,454–32,076 | 14,549 (6800–31,040) | |
| Musculoskeletal system | 0.88 | ||||
| Normal | 836 | 30,730 | 26,796–34,904 | 15,264 (6749–31,949) | |
| Abnormal | 942 | 28,839 | 26,029–31,797 | 14,782 (6920–30,428) | |
| Peripheral vascular system | <0.001 | ||||
| Normal | 859 | 24,699 | 22,318–27,395 | 12,511 (6155–26,460) | |
| Abnormal | 919 | 34,432 | 29,980–38,455 | 17,243 (7394–35,712) | |
| Serositis | <0.001 | ||||
| Normal | 1038 | 25,254 | 22,088–28,390 | 12,501 (6150–25,750) | |
| Abnormal | 740 | 35,994 | 32,291–40,338 | 18,350 (7940–40,312) | |
| Renal system | <0.001 | ||||
| Normal | 1093 | 25,864 | 22,770–28,962 | 13,030 (6095–27,114) | |
| Abnormal | 685 | 35,879 | 32,177–40,254 | 17,990 (7980–37,958) | |
| Neuropsychiatric system | 0.47 | ||||
| Normal | 1663 | 29,014 | 26,758–31,551 | 14,743 (6772–31,000) | |
| Abnormal | 115 | 40,069 | 25,188–53,849 | 15,738 (7050–37,958) | |
| Gastrointestinal system | 0.30 | ||||
| Normal | 1740 | 29,344 | 26,945–31,906 | 14,833 (6851–30,900) | |
| Abnormal | 38 | 47,167 | 21,122–67,857 | 17,645 (6520–51,660) | |
| Ocular system | 0.46 | ||||
| Normal | 1756 | 29,649 | 27,211–32,287 | 14,833 (6801–31,080) | |
| Abnormal | 22 | 35,918 | 14,917–53,009 | 17,754 (8000–40,618) | |
| Cardiovascular system | <0.001 | ||||
| Normal | 1651 | 29,069 | 26,664–31,689 | 14,100 (6559–30,428) | |
| Abnormal | 127 | 38,321 | 28,127–46,539 | 19,935 (11,220–43,701) | |
| Pulmonary system | 0.04 | ||||
| Normal | 1761 | 29,499 | 27,153–32,159 | 14,743 (6803–31,120) | |
| Abnormal | 17 | 53,274 | 23,230–79,140 | 26,784 (13,345–98,400) | |
| Number of Organs damaged | <0.001 | ||||
| 0 or 1 | 404 | 23,048 | 17,132–27,992 | 12,105 (5825–23,546) | |
| 2 or more | 1374 | 31,693 | 28,941–34,647 | 15,761 (7196–34,334) | |
| Biologics | <0.001 | ||||
| Yes | 148 | 48,817 | 33,271–60,434 | 26,890 (11,770–55,241) | |
| No | 1630 | 27,996 | 25,868–30,462 | 13,755 (6559–29,500) | |
| Dose of Glucocorticoids | <0.001 | ||||
| 0 mg/day (Unused) | 336 | 23,515 | 19,851–26,974 | 11,884 (5483–26,238) | |
| ≤7.5mg/day | 533 | 18,903 | 16,665–21,050 | 11,050 (5244–20,589) | |
| >7.5mg/d and ≤15mg/day | 510 | 34,280 | 29,092–39,751 | 16,340 (7941–35,712) | |
| >15mg/day | 399 | 43,608 | 35,702–50,329 | 23,270 (10,953–48,216) | |
| Univariate Linear Regression Model | Multiple Linear Regress Model (Method: Full) | Multiple Linear Regress Model (Method: Stepwise) | % of Increments or Decrements (Stepwise) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | p-Value | β | SE | p-Value | β | SE | p-Value | % * | Amount (CNY) # | |
| Intercept | N. A | N. A | N. A | 8.49 | 0.36 | <0.01 | 8.99 | 0.16 | <0.01 | — | 8022 (ref) |
| Female (ref = Male) | 0.06 | 0.11 | 0.56 | 0.12 | 0.09 | 0.21 | |||||
| Age groups (ref: ≥40 years) | |||||||||||
| <18 years | 0.10 | 0.17 | 0.53 | −0.03 | 0.15 | 0.82 | |||||
| 18–39 years | −0.04 | 0.06 | 0.53 | −0.07 | 0.06 | 0.23 | |||||
| Disease duration (ref = ≤3 years) | |||||||||||
| 3–8 years | −0.36 | 0.07 | <0.01 | −0.08 | 0.07 | 0.23 | |||||
| >8 years | −0.31 | 0.07 | <0.01 | −0.10 | 0.07 | 0.15 | |||||
| Region (ref: West) | |||||||||||
| Central | −0.12 | 0.08 | 0.15 | −0.09 | 0.07 | 0.21 | |||||
| Eastern | −0.11 | 0.07 | 0.13 | −0.13 | 0.07 | 0.04 | |||||
| Health insurance (ref: None) | −0.03 | 0.08 | 0.67 | −0.15 | 0.07 | 0.03 | −0.13 | 0.07 | 0.04 | −12.2 | −978 |
| Hospitalization during last year (ref: None) | 1.32 | 0.06 | <0.01 | 1.19 | 0.06 | <0.01 | 1.22 | 0.06 | <0.01 | 238.7 | 19,150 |
| Newly treated patients (ref: Treated patients) | 0.36 | 0.11 | <0.01 | −0.02 | 0.10 | 0.84 | |||||
| ANA positive (ref: Negative) | 0.30 | 0.13 | 0.02 | 0.20 | 0.11 | 0.08 | |||||
| dsDNA positive (ref: Negative) | 0.04 | 0.07 | 0.54 | 0.04 | 0.06 | 0.53 | |||||
| Abnormal liver function (ref: Normal) | 0.13 | 0.07 | 0.06 | 0.05 | 0.06 | 0.43 | |||||
| Low complement (ref: No) | 0.11 | 0.06 | 0.08 | −0.03 | 0.06 | 0.63 | |||||
| Moderate to severe (ref: Mild) | 0.60 | 0.09 | <0.01 | 0.27 | 0.09 | <0.01 | 0.26 | 0.08 | <0.01 | 29.7 | 2382 |
| Active disease State (ref: Remission or LLDAS) | 0.46 | 0.06 | <0.01 | 0.06 | 0.08 | 0.47 | |||||
| System involvement | |||||||||||
| Skin system (ref: Normal) | −0.02 | 0.06 | 0.71 | −0.01 | 0.06 | 0.83 | |||||
| Musculoskeletal system (ref: Normal) | −0.01 | 0.06 | 0.87 | −0.03 | 0.05 | 0.60 | |||||
| Peripheral vascular system (ref: Normal) | 0.22 | 0.06 | <0.01 | 0.12 | 0.05 | 0.02 | 0.13 | 0.05 | <0.01 | 13.9 | 1114 |
| Serositis (ref: Normal) | 0.33 | 0.06 | <0.01 | 0.01 | 0.10 | 0.90 | |||||
| Renal system (ref: Normal) | 0.30 | 0.06 | <0.01 | 0.20 | 0.10 | 0.04 | 0.20 | 0.05 | <0.01 | 22.1 | 1776 |
| Neuropsychiatric system (ref: Normal) | 0.10 | 0.11 | 0.38 | 0.01 | 0.10 | 0.94 | |||||
| Gastrointestinal system (ref: Normal) | 0.26 | 0.19 | 0.17 | 0.13 | 0.17 | 0.45 | |||||
| Ocular system (ref: Normal) | 0.22 | 0.25 | 0.38 | 0.10 | 0.22 | 0.65 | |||||
| Cardiovascular system (ref: Normal) | 0.43 | 0.11 | <0.01 | 0.42 | 0.10 | <0.01 | 0.39 | 0.09 | <0.01 | 47.7 | 3826 |
| Pulmonary system (ref: Normal) | 0.65 | 0.29 | 0.02 | 0.26 | 0.25 | 0.30 | |||||
| 2 or more damaged organs (ref: 0 or 1) | 0.25 | 0.07 | <0.01 | −0.01 | 0.08 | 0.89 | |||||
| Biologics (ref: Unused) | 0.59 | 0.10 | <0.01 | 0.34 | 0.09 | <0.01 | 0.34 | 0.09 | <0.01 | 40.5 | 3248 |
| Glucocorticoids (ref: Unused) | |||||||||||
| ≤7.5mg/day | −0.09 | 0.08 | 0.24 | −0.01 | 0.07 | 0.92 | −0.02 | 0.07 | 0.73 | −2.0 | −159 |
| >7.5mg/d and ≤15mg/day | 0.34 | 0.08 | <0.01 | 0.19 | 0.09 | 0.04 | 0.23 | 0.07 | <0.01 | 25.9 | 2074 |
| >15mg/day | 0.60 | 0.08 | <0.01 | 0.24 | 0.10 | 0.01 | 0.30 | 0.08 | <0.01 | 35.0 | 2807 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Li, M.; Zou, K.; Wang, Y.; Jia, Q.; Wang, L.; Zhao, J.; Wu, C.; Wang, Q.; Tian, X.; et al. Annual Direct Cost and Cost-Drivers of Systemic Lupus Erythematosus: A Multi-Center Cross-Sectional Study from CSTAR Registry. Int. J. Environ. Res. Public Health 2023, 20, 3522. https://doi.org/10.3390/ijerph20043522
Wang H, Li M, Zou K, Wang Y, Jia Q, Wang L, Zhao J, Wu C, Wang Q, Tian X, et al. Annual Direct Cost and Cost-Drivers of Systemic Lupus Erythematosus: A Multi-Center Cross-Sectional Study from CSTAR Registry. International Journal of Environmental Research and Public Health. 2023; 20(4):3522. https://doi.org/10.3390/ijerph20043522
Chicago/Turabian StyleWang, Haiyan, Mengtao Li, Kaiwen Zou, Yilin Wang, Qiaoling Jia, Li Wang, Jiuliang Zhao, Chanyuan Wu, Qian Wang, Xinping Tian, and et al. 2023. "Annual Direct Cost and Cost-Drivers of Systemic Lupus Erythematosus: A Multi-Center Cross-Sectional Study from CSTAR Registry" International Journal of Environmental Research and Public Health 20, no. 4: 3522. https://doi.org/10.3390/ijerph20043522
APA StyleWang, H., Li, M., Zou, K., Wang, Y., Jia, Q., Wang, L., Zhao, J., Wu, C., Wang, Q., Tian, X., Wang, Y., & Zeng, X. (2023). Annual Direct Cost and Cost-Drivers of Systemic Lupus Erythematosus: A Multi-Center Cross-Sectional Study from CSTAR Registry. International Journal of Environmental Research and Public Health, 20(4), 3522. https://doi.org/10.3390/ijerph20043522






